Changes in Corneal Epithelial Thickness Induced by Topical Antiglaucoma Medications
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Statistical Analysis
3. Results
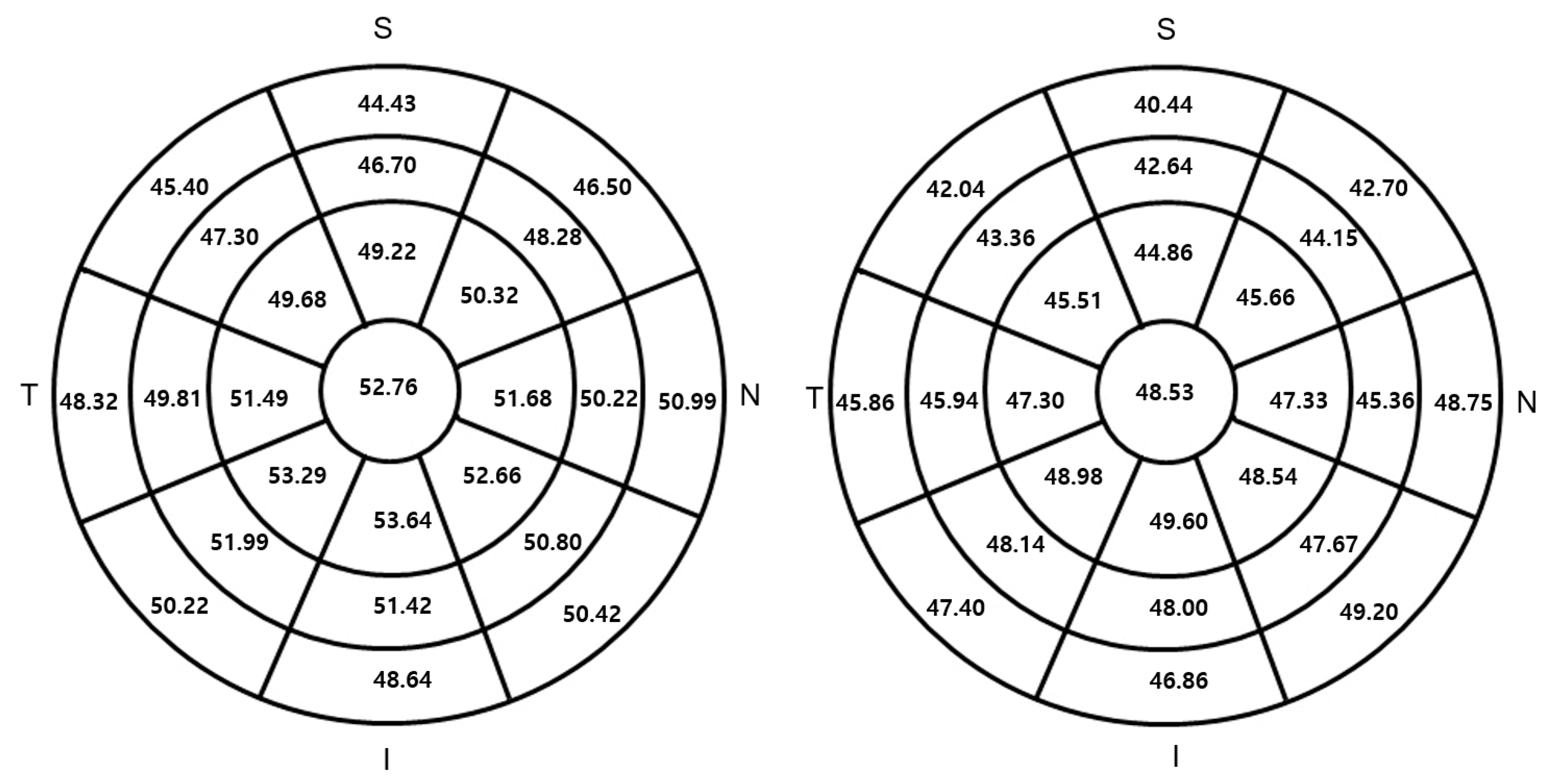
3.1. CET Profiles
3.2. Association between Glaucoma Medication and Corneal Thickness
3.3. Association between Glaucoma Medication and CET in the Monotherapy Medication Group
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Day, A.C.; Machin, D.; Aung, T.; Gazzard, G.; Husain, R.; Chew, P.T.; Khaw, P.T.; Seah, S.K.; Foster, P.J. Central corneal thickness and glaucoma in East Asian people. Investig. Ophthalmol. Vis. Sci. 2011, 52, 8407–8412. [Google Scholar] [CrossRef] [Green Version]
- Grewal, D.S.; Brar, G.S.; Grewal, S.P. Assessment of central corneal thickness in normal, keratoconus, and post-laser in situ keratomileusis eyes using Scheimpflug imaging, spectral domain optical coherence tomography, and ultrasound pachymetry. J. Cataract Refract. Surg. 2010, 36, 954–964. [Google Scholar] [CrossRef] [PubMed]
- Shah, H.; Kniestedt, C.; Bostrom, A.; Stamper, R.; Lin, S. Role of central corneal thickness on baseline parameters and progression of visual fields in open angle glaucoma. Eur. J. Ophthalmol. 2007, 17, 545–549. [Google Scholar] [CrossRef]
- Lee, M.; Ahn, J. Effects of Central Corneal Stromal Thickness and Epithelial Thickness on Intraocular Pressure Using Goldmann Applanation and Non-Contact Tonometers. PLoS ONE 2016, 11, e0151868. [Google Scholar] [CrossRef]
- Ma, Y.; He, X.; Zhu, X.; Lu, L.; Zhu, J.; Zou, H. Corneal Epithelium Thickness Profile in 614 Normal Chinese Children Aged 7–15 Years Old. Sci. Rep. 2016, 6, 23482. [Google Scholar] [CrossRef] [Green Version]
- Kanellopoulos, A.J.; Asimellis, G. In vivo three-dimensional corneal epithelium imaging in normal eyes by anterior-segment optical coherence tomography: A clinical reference study. Cornea 2013, 32, 1493–1498. [Google Scholar] [CrossRef] [PubMed]
- Kim, W.K.; Ryu, I.H.; Yoo, J.; Kim, S.W. Effect of Gender, Age, and Ocular and Growth-Related Factors on Corneal Epithelial and Stromal Thickness in Children. J. Clin. Med. 2020, 9, 3849. [Google Scholar] [CrossRef] [PubMed]
- Kanellopoulos, A.J.; Asimellis, G. In pursuit of objective dry eye screening clinical techniques. Eye Vis. 2016, 3, 1. [Google Scholar] [CrossRef] [Green Version]
- Kanellopoulos, A.J.; Asimellis, G. In vivo 3-dimensional corneal epithelial thickness mapping as an indicator of dry eye: Preliminary clinical assessment. Am. J. Ophthalmol. 2014, 157, 63–68.e2. [Google Scholar] [CrossRef] [PubMed]
- Cui, X.; Hong, J.; Wang, F.; Deng, S.X.; Yang, Y.; Zhu, X.; Wu, D.; Zhao, Y.; Xu, J. Assessment of corneal epithelial thickness in dry eye patients. Optom. Vis. Sci. 2014, 91, 1446–1454. [Google Scholar] [CrossRef] [Green Version]
- Abou Shousha, M.; Wang, J.; Kontadakis, G.; Feuer, W.; Canto, A.P.; Hoffmann, R.; Perez, V.L. Corneal epithelial thickness profile in dry-eye disease. Eye 2020, 34, 915–922. [Google Scholar] [CrossRef]
- Li, Y.; Chamberlain, W.; Tan, O.; Brass, R.; Weiss, J.L.; Huang, D. Subclinical keratoconus detection by pattern analysis of corneal and epithelial thickness maps with optical coherence tomography. J. Cataract Refract. Surg. 2016, 42, 284–295. [Google Scholar] [CrossRef] [Green Version]
- Silverman, R.H.; Urs, R.; RoyChoudhury, A.; Archer, T.J.; Gobbe, M.; Reinstein, D.Z. Combined tomography and epithelial thickness mapping for diagnosis of keratoconus. Eur. J. Ophthalmol. 2017, 27, 129–134. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsai, J.H.; Derby, E.; Holland, E.J.; Khatana, A.K. Incidence and prevalence of glaucoma in severe ocular surface disease. Cornea 2006, 25, 530–532. [Google Scholar] [CrossRef] [PubMed]
- Leung, E.W.; Medeiros, F.A.; Weinreb, R.N. Prevalence of ocular surface disease in glaucoma patients. J. Glaucoma 2008, 17, 350–355. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghosh, S.; O’Hare, F.; Lamoureux, E.; Vajpayee, R.B.; Crowston, J.G. Prevalence of signs and symptoms of ocular surface disease in individuals treated and not treated with glaucoma medication. Clin. Exp. Ophthalmol. 2012, 40, 675–681. [Google Scholar] [CrossRef]
- Doğan, E.; Cakir, B.K.; Aksoy, N.O.; Celik, E.; Erkorkmaz, U. Effects of topical antiglaucomatous medications on central corneal epithelial thickness by anterior segment optical coherence tomography. Eur. J. Ophthalmol. 2020, 30, 1519–1524. [Google Scholar] [CrossRef]
- Batawi, H.; Lollett, I.V.; Maliakal, C.; Wellik, S.R.; Anderson, M.G.; Feuer, W.; Karp, C.L.; Galor, A. A Comparative Study of Central Corneal Epithelial, Stromal, and Total Thickness in Males with and without Primary Open-Angle Glaucoma. Cornea 2018, 37, 712–719. [Google Scholar] [CrossRef]
- Halkiadakis, I.; Vernikou, A.; Tzimis, V.; Markopoulos, I.; Popeskou, K.; Konstadinidou, V. Assessment of Corneal Epithelium Thickness in Glaucomatous Patients Undergoing Medical Treatment. J. Glaucoma 2021, 30, 44–49. [Google Scholar] [CrossRef]
- Aguayo Bonniard, A.; Yeung, J.Y.; Chan, C.C.; Birt, C.M. Ocular surface toxicity from glaucoma topical medications and associated preservatives such as benzalkonium chloride (BAK). Expert Opin. Drug Metab. Toxicol. 2016, 12, 1279–1289. [Google Scholar] [CrossRef]
- Martone, G.; Frezzotti, P.; Tosi, G.M.; Traversi, C.; Mittica, V.; Malandrini, A.; Pichierri, P.; Balestrazzi, A.; Motolese, P.A.; Motolese, I.; et al. An in vivo confocal microscopy analysis of effects of topical antiglaucoma therapy with preservative on corneal innervation and morphology. Am. J. Ophthalmol. 2009, 147, 725–735.e1. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.; Park, M.; Richardson, A.; Tedla, N.; Pandzic, E.; de Paiva, C.S.; Watson, S.; Wakefield, D.; Di Girolamo, N. Dose-dependent benzalkonium chloride toxicity imparts ocular surface epithelial changes with features of dry eye disease. Ocul. Surf. 2020, 18, 158–169. [Google Scholar] [CrossRef]
- Fuentes, E.; Sandali, O.; El Sanharawi, M.; Basli, E.; Hamiche, T.; Goemaere, I.; Borderie, V.; Bouheraoua, N.; Laroche, L. Anatomic Predictive Factors of Acute Corneal Hydrops in Keratoconus: An Optical Coherence Tomography Study. Ophthalmology 2015, 122, 1653–1659. [Google Scholar] [CrossRef]
- Ryu, I.H.; Kim, B.J.; Lee, J.H.; Kim, S.W. Comparison of Corneal Epithelial Remodeling After Femtosecond Laser-Assisted LASIK and Small Incision Lenticule Extraction (SMILE). J. Refract. Surg. 2017, 33, 250–256. [Google Scholar] [CrossRef]
- Kang, D.S.Y.; Kim, S.W. Effect of Corneal Cross-Linking on Epithelial Hyperplasia and Myopia Regression after Transepithelial Photorefractive Keratectomy. J. Refract. Surg. 2019, 35, 354–361. [Google Scholar] [CrossRef]
- Haberman, I.D.; Lang, P.Z.; Broncano, A.F.; Kim, S.W.; Hafezi, F.; Randleman, J.B. Epithelial remodeling after corneal crosslinking using higher fluence and accelerated treatment time. J. Cataract Refract. Surg. 2018, 44, 306–312. [Google Scholar] [CrossRef] [PubMed]
- Kim, W.K.; Kim, B.J.; Ryu, I.H.; Kim, J.K.; Kim, S.W. Corneal epithelial and stromal thickness changes in myopic orthokeratology and their relationship with refractive change. PLoS ONE 2018, 13, e0203652. [Google Scholar] [CrossRef]
- Iovino, C.; Fossarello, M.; Giannaccare, G.; Pellegrini, M.; Braghiroli, M.; Demarinis, G.; Napoli, P.E. Corneal endothelium features in Fuchs’ Endothelial Corneal Dystrophy: A preliminary 3D anterior segment optical coherence tomography study. PLoS ONE 2018, 13, e0207891. [Google Scholar] [CrossRef]
- Napoli, P.E.; Nioi, M.; Iovino, C.; Sanna, R.; d’Aloja, E.; Fossarello, M. Ocular surface and respiratory tract damages from occupational, sub-chronic exposure to fluorspar: Case report and other considerations. Int. Ophthalmol. 2019, 39, 1175–1178. [Google Scholar] [CrossRef]
- Sharma, R.; Dikshit, S.; Hoshing, A.; Vaddavalli, P.K. Effect of timolol on refractive outcomes in eyes with myopic regression after laser in situ keratomileusis: A prospective randomized clinical trial. Am. J. Ophthalmol. 2013, 156, 413–414. [Google Scholar] [CrossRef]
- Ryu, I.H.; Kim, W.K.; Nam, M.S.; Kim, J.K.; Kim, S.W. Reduction of corneal epithelial thickness during medical treatment for myopic regression following FS-LASIK. BMC Ophthalmol. 2020, 20, 296. [Google Scholar] [CrossRef]
- Petounis, A.D.; Akritopoulos, P. Influence of topical and systemic beta-blockers on tear production. Int. Ophthalmol. 1989, 13, 75–80. [Google Scholar] [CrossRef]
- Bonomi, L.; Zavarise, G.; Noya, E.; Michieletto, S. Effects of timolol maleate on tear flow in human eyes. Albrecht Von Graefes Arch. Klin. Exp. Ophthalmol. 1980, 213, 19–22. [Google Scholar] [CrossRef]
- Kuppens, E.V.; Stolwijk, T.R.; de Keizer, R.J.; van Best, J.A. Basal tear turnover and topical timolol in glaucoma patients and healthy controls by fluorophotometry. Investig. Ophthalmol. Vis. Sci. 1992, 33, 3442–3448. [Google Scholar]
- Napoli, P.E.; Nioi, M.; d’Aloja, E.; Fossarello, M. The Bull’s Eye Pattern of the Tear Film in Humans during Visual Fixation on En-Face Optical Coherence Tomography. Sci. Rep. 2019, 9, 1413. [Google Scholar] [CrossRef] [PubMed]
- Brandt, J.D.; Gordon, M.O.; Beiser, J.A.; Lin, S.C.; Alexander, M.Y.; Kass, M.A.; Ocular Hypertension Treatment Study Group. Changes in central corneal thickness over time: The ocular hypertension treatment study. Ophthalmology 2008, 115, 1550–1556.e1. [Google Scholar] [CrossRef]
- Jang, M.; Kang, K.E.; Cho, B.J. Effect of Prostaglandin Analogues on Central Corneal Thickness: 3-Year Follow-Up Results. Korean J. Ophthalmol. 2020, 34, 347–352. [Google Scholar] [CrossRef]
- Bafa, M.; Georgopoulos, G.; Mihas, C.; Stavrakas, P.; Papaconstantinou, D.; Vergados, I. The effect of prostaglandin analogues on central corneal thickness of patients with chronic open-angle glaucoma: A 2-year study on 129 eyes. Acta Ophthalmol. 2011, 89, 448–451. [Google Scholar] [CrossRef]
- Kim, B.J.; Ryu, I.H.; Kim, S.W. Age-related differences in corneal epithelial thickness measurements with anterior segment optical coherence tomography. Jpn J. Ophthalmol. 2016, 60, 357–364. [Google Scholar] [CrossRef]
- King-Smith, P.E.; Kimball, S.H.; Nichols, J.J. Tear film interferometry and corneal surface roughness. Investig. Ophthalmol. Vis. Sci. 2014, 55, 2614–2618. [Google Scholar] [CrossRef] [Green Version]
- Napoli, P.E.; Nioi, M.; Mangoni, L.; Gentile, P.; Braghiroli, M.; d’Aloja, E.; Fossarello, M. Fourier-Domain OCT Imaging of the Ocular Surface and Tear Film Dynamics: A Review of the State of the Art and an Integrative Model of the Tear Behavior During the Inter-Blink Period and Visual Fixation. J. Clin. Med. 2020, 9, 668. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Patient Characteristics | Control (n = 125) | Glaucoma (n = 125) | p Value |
|---|---|---|---|
| Age (years) | 65.1 ± 8.9 | 66.7 ± 11.0 | 0.191 |
| Sex | 62:63 | 68:57 | 0.527 |
| CCT | 525.0 ± 29.6 | 520.7 ± 31.7 | 0.269 |
| CST | 472.2 ± 29.5 | 472.3 ± 29.5 | 0.987 |
| Epithelium (µm) | |||
| Central | 52.8 ± 3.6 | 48.5 ± 3.9 | <0.001 * |
| Paracentral | 51.5 ± 3.4 | 47.2 ± 4.0 | <0.001 * |
| Mid-peripheral | 49.6 ± 3.3 | 45.8 ± 3.8 | <0.001 * |
| Peripheral | 48.1 ± 3.4 | 45.4 ± 4.1 | <0.001 * |
| Thickness variability | 2.9 ± 1.0 | 3.0 ± 1.1 | 0.304 |
| Simple Regression | ||||||
|---|---|---|---|---|---|---|
| B | R | p | B | R | p | |
| Central Epithelium | Central Stroma | |||||
| Age | −0.068 | 0.189 | 0.035 | −0.543 | 0.189 | 0.034 |
| Sex | 0.029 | 0.004 | 0.967 | −0.400 | 0.006 | 0.944 |
| Medication number | −1.874 | 0.402 | <0.001 | −3.682 | 0.099 | 0.271 |
| BAK-containing instillations | −1.413 | 0.428 | <0.001 | −2.085 | 0.079 | 0.379 |
| β-blockers | −3.257 | 0.390 | <0.001 | −4.118 | 0.062 | 0.493 |
| PG | −2.147 | 0.238 | 0.007 | −11.912 | 0.166 | 0.064 |
| CAIs | −2.223 | 0.274 | 0.002 | 1.514 | 0.023 | 0.795 |
| α-agonists | −1.397 | 0.176 | 0.049 | −0.519 | 0.008 | 0.927 |
| VFI | 0.042 | 0.346 | <0.001 | −0.104 | 0.108 | 0.231 |
| Multiple Regression | |||
|---|---|---|---|
| B | R | p | |
| Central epithelium | 0.550 | <0.001 | |
| Age | −0.016 | 0.597 | |
| BAK-containing instillations | −0.777 | 0.016 | |
| β-blockers | −2.449 | 0.038 | |
| PG | −1.690 | 0.024 | |
| CAIs | 0.575 | 0.589 | |
| α-agonists | −0.209 | 0.756 | |
| VFI | 0.017 | 0.117 | |
| Patient Characteristics | Preservative-Containing Medication (n = 37) | Preservative-Free Medication (n = 19) | p Value |
|---|---|---|---|
| Age (years) | 65.9 ± 10.8 | 63.1 ± 11.6 | 0.376 |
| CCT | 529.1 ± 31.4 | 526.6 ± 29.6 | 0.775 |
| CST | 479.0 ± 31.1 | 475.9 ± 29.7 | 0.719 |
| Epithelium (µm) | |||
| Central | 50.1 ± 3.3 | 50.7 ± 3.3 | 0.502 |
| Paracentral | 49.1 ± 3.6 | 49.6 ± 2.9 | 0.565 |
| Mid-peripheral | 47.4 ± 3.6 | 48.1 ± 2.7 | 0.522 |
| Peripheral | 46.7 ± 3.5 | 47.47 ± 3.7 | 0.499 |
| Thickness variability | 2.8 ± 1.1 | 2.8 ± 0.81 | 1.000 |
| Medication | n | CET | CST | CCT | |
|---|---|---|---|---|---|
| β-blockers | Yes | 23 | 49.1 ± 3.1 | 476.8 ± 28.3 | 526.0 ± 28.2 |
| No | 33 | 51.1 ± 3.2 | 478.8 ± 32.2 | 529.8 ± 32.4 | |
| p | 0.029 | 0.818 | 0.646 | ||
| PG | Yes | 29 | 50.3 ± 3.1 | 471.0 ± 29.8 | 521.3 ± 29.6 |
| No | 27 | 50.3 ± 3.5 | 485.4 ± 29.7 | 535.7 ± 30.3 | |
| p | 0.985 | 0.075 | 0.077 | ||
| BAK | Yes | 30 | 49.5 ± 3.0 | 472.4 ± 30.0 | 521.9 ± 29.7 |
| No | 26 | 51.2 ± 3.4 | 484.4 ± 30.1 | 535.5 ± 30.5 | |
| p | 0.059 | 0.143 | 0.096 |
| Simple Regression | ||||||
|---|---|---|---|---|---|---|
| B | R | p | B | R | p | |
| Central Epithelium | Central Stroma | |||||
| Age | −0.068 | 0.189 | 0.279 | −1.220 | 0.443 | 0.001 |
| BAK-containing instillations | −1.196 | 0.288 | 0.031 | −4.855 | 0.126 | 0.353 |
| β-blockers | −1.930 | 0.292 | 0.029 | −1.931 | 0.032 | 0.818 |
| PG | 0.017 | 0.003 | 0.985 | −14.444 | 0.240 | 0.075 |
| CAIs | −0.638 | 0.090 | 0.590 | 6.893 | 0.105 | 0.440 |
| α-agonists | 1.005 | 0.113 | 0.405 | 20.695 | 0.252 | 0.061 |
| VFI | 0.032 | 0.180 | 0.188 | 0.142 | 0.083 | 0.548 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nam, M.; Kim, S.W. Changes in Corneal Epithelial Thickness Induced by Topical Antiglaucoma Medications. J. Clin. Med. 2021, 10, 3464. https://doi.org/10.3390/jcm10163464
Nam M, Kim SW. Changes in Corneal Epithelial Thickness Induced by Topical Antiglaucoma Medications. Journal of Clinical Medicine. 2021; 10(16):3464. https://doi.org/10.3390/jcm10163464
Chicago/Turabian StyleNam, Myungsik, and Sun Woong Kim. 2021. "Changes in Corneal Epithelial Thickness Induced by Topical Antiglaucoma Medications" Journal of Clinical Medicine 10, no. 16: 3464. https://doi.org/10.3390/jcm10163464
APA StyleNam, M., & Kim, S. W. (2021). Changes in Corneal Epithelial Thickness Induced by Topical Antiglaucoma Medications. Journal of Clinical Medicine, 10(16), 3464. https://doi.org/10.3390/jcm10163464






