Role of Annual Influenza Vaccination against Lung Cancer in Type 2 Diabetic Patients from a Population-Based Cohort Study
Abstract
1. Introduction
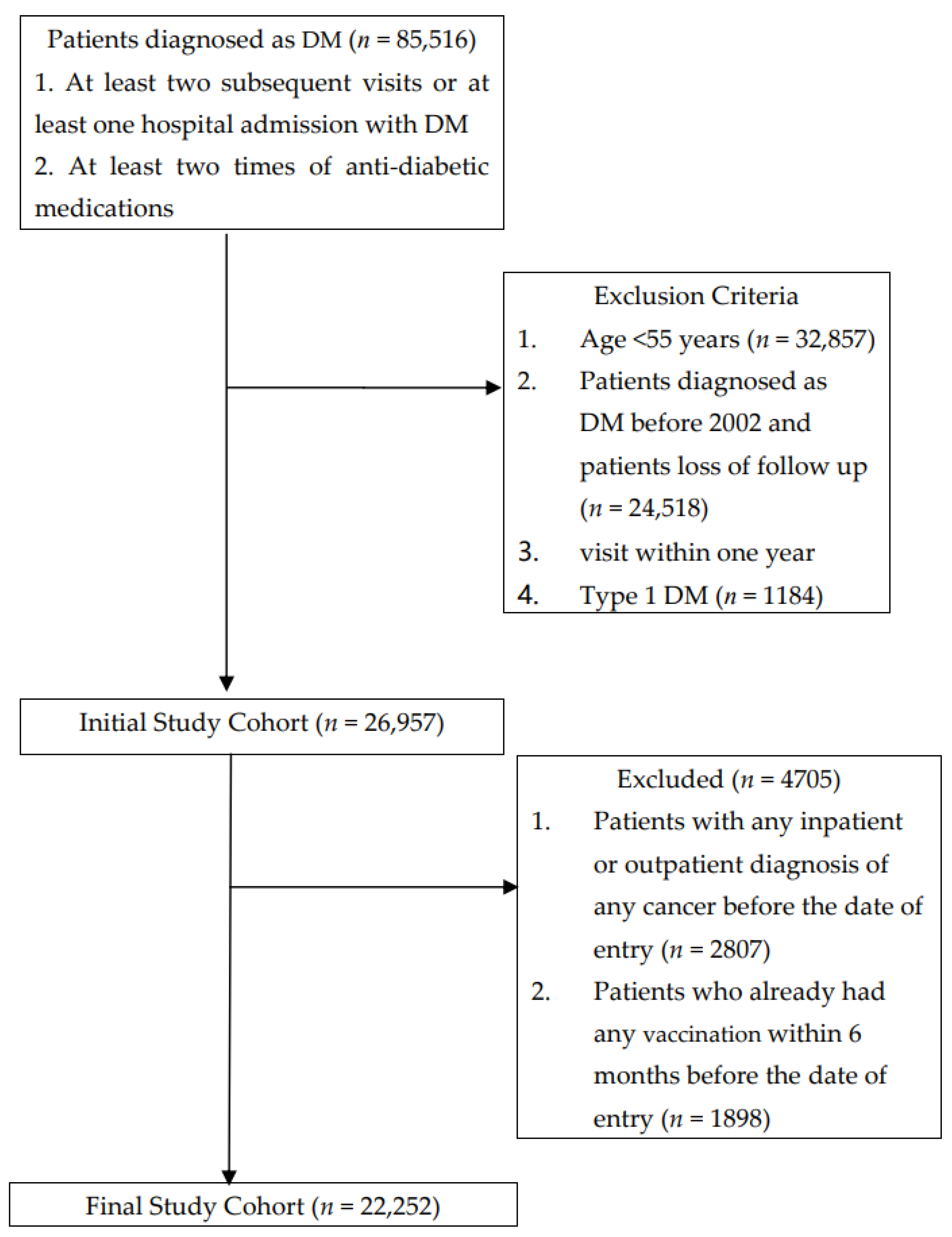
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Song, S.; Wang, B.; Zhang, X.; Hao, L.; Hu, X.; Li, Z.; Sun, S. Long-Term Diabetes Mellitus Is Associated with an Increased Risk of Pancreatic Cancer: A Meta-Analysis. PLoS ONE 2015, 10, e0134321. [Google Scholar] [CrossRef] [PubMed]
- Sasazuki, S.; Charvat, H.; Hara, A.; Wakai, K.; Nagata, C.; Nakamura, K.; Tsuji, I.; Sugawara, Y.; Tamakoshi, A.; Matsuo, K.; et al. Diabetes mellitus and cancer risk: Pooled analysis of eight cohort studies in Japan. Cancer Sci. 2013, 104, 1499–1507. [Google Scholar] [CrossRef]
- Hope, C.; Robertshaw, A.; Cheung, K.L.; Idris, I.; English, E. Relationship between HbA1c and cancer in people with or without diabetes: A systematic review. Diabet. Med. 2016, 33, 1013–1025. [Google Scholar] [CrossRef] [PubMed]
- Agache, A.; Mustatea, P.; Mihalache, O.; Bobirca, F.T.; Georgescu, D.E.; Jauca, C.M.; Birligea, A.; Doran, H.; Patrascu, T. Diabetes Mellitus as a Risk-factor for Colorectal Cancer Literature Review-Current Situation and Future Perspectives. Chirurgia 2018, 113, 603–610. [Google Scholar] [CrossRef]
- Kuriki, K.; Hirose, K.; Tajima, K. Diabetes and cancer risk for all and specific sites among Japanese men and women. Eur. J. Cancer Prev. 2007, 16, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Luo, J.; Chlebowski, R.; Wactawski-Wende, J.; Schlecht, N.F.; Tinker, L.; Margolis, K.L. Diabetes and lung cancer among postmenopausal women. Diabet. Care 2012, 35, 1485–1491. [Google Scholar] [CrossRef]
- Jee, S.H.; Ohrr, H.; Sull, J.W.; Yun, J.E.; Ji, M.; Samet, J.M. Fasting serum glucose level and cancer risk in Korean men and women. JAMA 2005, 293, 194–202. [Google Scholar] [CrossRef] [PubMed]
- Pallis, A.G.; Syrigos, K.N. Lung cancer in never smokers: Disease characteristics and risk factors. Crit. Rev. Oncol. Hematol. 2013, 88, 494–503. [Google Scholar] [CrossRef] [PubMed]
- Argiles, J.M.; Lopez-Soriano, F.J. Insulin and cancer (Review). Int. J. Oncol. 2001, 18, 683–687. [Google Scholar] [CrossRef]
- Strickler, H.D.; Wylie-Rosett, J.; Rohan, T.; Hoover, D.R.; Smoller, S.; Burk, R.D.; Yu, H. The relation of type 2 diabetes and cancer. Diabetes. Technol. Ther. 2001, 3, 263–274. [Google Scholar] [CrossRef] [PubMed]
- Forgiarini, L.A., Jr.; Kretzmann, N.A.; Porawski, M.; Dias, A.S.; Marroni, N.A. Experimental diabetes mellitus: Oxidative stress and changes in lung structure. J. Bras. Pneumol. 2009, 35, 788–791. [Google Scholar] [CrossRef]
- Lee, G.; Walser, T.C.; Dubinett, S.M. Chronic inflammation, chronic obstructive pulmonary disease, and lung cancer. Curr. Opin. Pulm. Med. 2009, 15, 303–307. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.Y.; Jeon, I.; Lee, J.M.; Yoon, J.M.; Park, S.M. Diabetes mellitus as an independent risk factor for lung cancer: A meta-analysis of observational studies. Eur. J. Cancer 2013, 49, 2411–2423. [Google Scholar] [CrossRef]
- Zhu, L.; Cao, H.; Zhang, T.; Shen, H.; Dong, W.; Wang, L.; Du, J. The Effect of Diabetes Mellitus on Lung Cancer Prognosis: A PRISMA-compliant Meta-analysis of Cohort Studies. Medicine 2016, 95, e3528. [Google Scholar] [CrossRef]
- Chan, T.C.; Fu, Y.C.; Wang, D.W.; Chuang, J.H. Determinants of receiving the pandemic (H1N1) 2009 vaccine and intention to receive the seasonal influenza vaccine in Taiwan. PLoS ONE 2014, 9, e101083. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.Y.; Wu, S.M.; Liu, J.C.; Lee, K.Y. Effect of annual influenza vaccination on reducing lung cancer in patients with chronic obstructive pulmonary disease from a population-based cohort study. Medicine 2019, 98, e18035. [Google Scholar] [CrossRef] [PubMed]
- D’Agostino, R.B., Jr. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat. Med. 1998, 17, 2265–2281. [Google Scholar] [CrossRef]
- Allard, R.; Leclerc, P.; Tremblay, C.; Tannenbaum, T.N. Diabetes and the severity of pandemic influenza A (H1N1) infection. Diabetes Care 2010, 33, 1491–1493. [Google Scholar] [CrossRef] [PubMed]
- Wilking, H.; Buda, S.; von der Lippe, E.; Altmann, D.; Krause, G.; Eckmanns, T.; Haas, W. Mortality of 2009 pandemic influenza A(H1N1) in Germany. Euro. Surveill. 2010, 15, 19741. [Google Scholar] [CrossRef]
- Nojima, I.; Eikawa, S.; Tomonobu, N.; Hada, Y.; Kajitani, N.; Teshigawara, S.; Miyamoto, S.; Tone, A.; Uchida, H.A.; Nakatsuka, A.; et al. Dysfunction of CD8 + PD-1 + T cells in type 2 diabetes caused by the impairment of metabolism-immune axis. Sci. Rep. 2020, 10, 14928. [Google Scholar] [CrossRef]
- Sheridan, P.A.; Paich, H.A.; Handy, J.; Karlsson, E.A.; Schultz-Cherry, S.; Hudgens, M.; Weir, S.; Noah, T.; Beck, M.A. The antibody response to influenza vaccination is not impaired in type 2 diabetics. Vaccine 2015, 33, 3306–3313. [Google Scholar] [CrossRef] [PubMed]
- Seo, Y.B.; Baek, J.H.; Lee, J.; Song, J.Y.; Lee, J.S.; Cheong, H.J.; Kim, W.J. Long-Term Immunogenicity and Safety of a Conventional Influenza Vaccine in Patients with Type 2 Diabetes. Clin. Vaccine Immunol. 2015, 22, 1160–1165. [Google Scholar] [CrossRef] [PubMed]
- McElhaney, J.E.; Garneau, H.; Camous, X.; Dupuis, G.; Pawelec, G.; Baehl, S.; Tessier, D.; Frost, E.H.; Frasca, D.; Larbi, A.; et al. Predictors of the antibody response to influenza vaccination in older adults with type 2 diabetes. BMJ Open. Diabetes Res. Care 2015, 3, e000140. [Google Scholar] [CrossRef]
- Newman, J.H.; Chesson, C.B.; Herzog, N.L.; Bommareddy, P.K.; Aspromonte, S.M.; Pepe, R.; Estupinian, R.; Aboelatta, M.M.; Buddhadev, S.; Tarabichi, S.; et al. Intratumoral injection of the seasonal flu shot converts immunologically cold tumors to hot and serves as an immunotherapy for cancer. Proc. Natl. Acad. Sci. USA 2020, 117, 1119–1128. [Google Scholar] [CrossRef] [PubMed]
- Chang, F.C.; Sung, H.Y.; Zhu, S.H.; Chiou, S.T. Impact of the 2009 Taiwan tobacco hazards prevention act on smoking cessation. Addiction 2014, 109, 140–146. [Google Scholar] [CrossRef]
- Ozlu, T.; Bulbul, Y. Smoking and lung cancer. Tuberk. Toraks 2005, 53, 200–209. [Google Scholar] [PubMed]
- Murin, S.; Bilello, K.S. Respiratory tract infections: Another reason not to smoke. Cleve Clin. J. Med. 2005, 72, 916–920. [Google Scholar] [CrossRef]
- Feng, Y.; Kong, Y.; Barnes, P.F.; Huang, F.F.; Klucar, P.; Wang, X.; Samten, B.; Sengupta, M.; Machona, B.; Donis, R.; et al. Exposure to cigarette smoke inhibits the pulmonary T-cell response to influenza virus and Mycobacterium tuberculosis. Infect. Immun. 2011, 79, 229–237. [Google Scholar] [CrossRef]
- Epstein, M.A.; Reynaldo, S.; El-Amin, A.N. Is smoking a risk factor for influenza hospitalization and death? J. Infect. Dis. 2010, 201, 794–795. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Almirall, J.; Bolibar, I.; Serra-Prat, M.; Roig, J.; Hospital, I.; Carandell, E.; Agusti, M.; Ayuso, P.; Estela, A.; Torres, A.; et al. New evidence of risk factors for community-acquired pneumonia: A population-based study. Eur. Respir. J. 2008, 31, 1274–1284. [Google Scholar] [CrossRef] [PubMed]
- Godoy, P.; Castilla, J.; Soldevila, N.; Mayoral, J.M.; Toledo, D.; Martin, V.; Astray, J.; Egurrola, M.; Morales-Suarez-Varela, M.; Dominguez, A.; et al. Smoking may increase the risk of influenza hospitalization and reduce influenza vaccine effectiveness in the elderly. Eur J. Public Health 2018, 28, 150–155. [Google Scholar] [CrossRef] [PubMed]
- Chambers, C.; Skowronski, D.M.; Rose, C.; Serres, G.; Winter, A.L.; Dickinson, J.A.; Jassem, A.; Gubbay, J.B.; Fonseca, K.; Drews, S.J.; et al. Should Sex Be Considered an Effect Modifier in the Evaluation of Influenza Vaccine Effectiveness? Open. Forum. Infect. Dis. 2018, 5, ofy211. [Google Scholar] [CrossRef] [PubMed]
- Klein, S.L.; Pekosz, A. Sex-based biology and the rational design of influenza vaccination strategies. J. Infect. Dis. 2014, 209, S114–S119. [Google Scholar] [CrossRef]
- Gabriel, G.; Arck, P.C. Sex, immunity and influenza. J. Infect. Dis. 2014, 209, S93–S99. [Google Scholar] [CrossRef] [PubMed]
- Weng, C.F.; Chen, L.J.; Lin, C.W.; Chen, H.M.; Lee, H.H.; Ling, T.Y.; Hsiao, F.Y. Association between the risk of lung cancer and influenza: A population-based nested case-control study. Int. J. Infect. Dis. 2019, 88, 8–13. [Google Scholar] [CrossRef] [PubMed]
| Whole Cohort (n = 22,252) | Unvaccinated (n = 14,392) | Vaccinated (n = 7860) | p | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Age, years (Mean ± SD) | 66.48 (8.70) | 64.64 (8.74) | 69.85 (7.54) | <0.001 | |||
| 55–64 | 11,464 | 51.52 | 9111 | 63.31 | 2353 | 29.94 | <0.001 |
| 65–74 | 6749 | 30.33 | 3202 | 22.25 | 3547 | 45.13 | |
| ≥75 | 4039 | 18.15 | 2079 | 14.45 | 1960 | 24.94 | |
| Gender | |||||||
| Female | 11,248 | 50.55 | 7032 | 48.86 | 4216 | 53.64 | <0.001 |
| Male | 11,004 | 49.45 | 7360 | 51.14 | 3644 | 46.36 | |
| CCI Index | |||||||
| 0 | 6821 | 30.65 | 4743 | 32.96 | 2078 | 26.44 | <0.001 |
| 1 | 5959 | 26.78 | 3881 | 26.97 | 2078 | 26.44 | |
| 2 | 4322 | 19.42 | 2689 | 18.68 | 1633 | 20.78 | |
| ≥3 | 5150 | 23.14 | 3079 | 21.39 | 2071 | 26.35 | |
| Hypertension | |||||||
| No | 7775 | 34.94 | 5389 | 37.44 | 2386 | 30.36 | <0.001 |
| Yes | 14,477 | 65.06 | 9003 | 62.56 | 5474 | 69.64 | |
| Dyslipidemia | |||||||
| No | 14,300 | 64.26 | 9263 | 64.36 | 5037 | 64.08 | 0.679 |
| Yes | 7952 | 35.74 | 5129 | 35.64 | 2823 | 35.92 | |
| Hypoglycemic medications | |||||||
| Insulin and analogues | 3788 | 17.02 | 2242 | 15.58 | 1546 | 19.67 | <0.001 |
| Biguanides | 16,711 | 75.10 | 10,813 | 75.13 | 5898 | 75.04 | 0.877 |
| Sulfonamides, urea derivatives | 14,330 | 64.40 | 8980 | 62.40 | 5350 | 68.07 | <0.001 |
| Alpha glucosidase inhibitors | 3889 | 17.48 | 2325 | 16.15 | 1564 | 19.90 | <0.001 |
| Thiazolidinediones | 2949 | 13.25 | 1770 | 12.30 | 1179 | 15.00 | <0.001 |
| Dipeptidyl peptidase 4 (DPP-4) | 3089 | 13.88 | 1975 | 13.72 | 1114 | 14.17 | 0.353 |
| Oral blood glucose lowering | 2808 | 12.62 | 1843 | 12.81 | 965 | 12.28 | 0.257 |
| Other blood glucose lowering drugs | 2917 | 13.11 | 1700 | 11.81 | 1217 | 15.48 | <0.001 |
| Number of hypoglycemic medications | |||||||
| 0–1 | 6652 | 29.89 | 4522 | 31.42 | 2130 | 27.10 | <0.001 |
| 2-3 | 9987 | 44.88 | 6587 | 45.77 | 3400 | 43.26 | |
| >3 | 5613 | 25.22 | 3283 | 22.81 | 2330 | 29.64 | |
| Combined medications | |||||||
| Statins | |||||||
| <28 days | 11,051 | 49.66 | 7428 | 51.61 | 3623 | 46.09 | <0.001 |
| 28–365 days | 5150 | 23.14 | 3418 | 23.75 | 1732 | 22.04 | |
| >365 days | 6051 | 27.19 | 3546 | 24.64 | 2505 | 31.87 | |
| Aspirin | |||||||
| <28 days | 12,296 | 55.26 | 8908 | 61.90 | 3388 | 43.10 | <0.001 |
| 28–365 days | 4192 | 18.84 | 2535 | 17.61 | 1657 | 21.08 | |
| >365 days | 5764 | 25.90 | 2949 | 20.49 | 2815 | 35.81 | |
| ACEI and ARB | |||||||
| <28 days | 8138 | 36.57 | 6026 | 41.87 | 2112 | 26.87 | <0.001 |
| 28–365 days | 4765 | 21.41 | 3174 | 22.05 | 1591 | 20.24 | |
| >365 days | 9349 | 42.01 | 5192 | 36.08 | 4157 | 52.89 | |
| Level of Urbanization | |||||||
| Urban | 15,587 | 70.05 | 10,619 | 73.78 | 4968 | 63.21 | <0.001 |
| Suburban | 4432 | 19.92 | 2626 | 18.25 | 1806 | 22.98 | |
| Rural | 2233 | 10.04 | 1147 | 7.97 | 1086 | 13.82 | |
| Monthly income (NT$) | |||||||
| 0 | 2016 | 9.06 | 1129 | 7.84 | 887 | 11.28 | <0.001 |
| 1–19,200 | 6212 | 27.92 | 3687 | 25.62 | 2525 | 32.12 | |
| 19,200–25,000 | 6746 | 30.32 | 3896 | 27.07 | 2850 | 36.26 | |
| ≥25,001 | 7278 | 32.71 | 5680 | 39.47 | 1598 | 20.33 | |
| All Group (n = 22,252) | Unvaccinated (Total Follow-Up 59,866.2 Person-Years) | Vaccinated (Total Follow-Up 51,033.7 Person-Years) | Adjusted HR † (95% C.I.) | ||
|---|---|---|---|---|---|
| No. of Patients With Cancer | Incidence Rate (per 105 Person-Years) (95% C.I.) | No. of Patients With Cancer | Incidence Rate (per 105 Person-Years) (95% C.I.) | ||
| Whole cohort | 244 | 407.6 (356.4, 458.7) | 165 | 323.3 (274.0, 372.6) | 0.77 (0.62, 0.95) * |
| Age (years) | |||||
| 55–64 a | 112 | 268.9 (219.1, 318.7) | 28 | 151.9 (95.6, 208.2) | 0.61 (0.40, 0.94) * |
| 65–74 b | 74 | 600.0 (463.3, 736.8) | 87 | 386.1 (305.0, 467.3) | 0.74 (0.54, 1.03) |
| ≥75 c | 58 | 986.4 (732.5, 1240.2) | 50 | 496.5 (358.9, 634.1) | 0.63 (0.42, 0.92) * |
| Sex | |||||
| Female d | 77 | 254.3 (197.5, 311.1) | 64 | 226.4 (170.9, 281.8) | 0.85 (0.60, 1.22) |
| Male e | 167 | 564.4 (478.8, 650.0) | 101 | 443.7 (357.2, 530.2) | 0.72 (0.55, 0.94) * |
| Unvaccinated | Vaccinated | p for Trend | |||
|---|---|---|---|---|---|
| 1 | 2–3 | ≥4 | |||
| Adjusted HR (95% C.I.) | Adjusted HR (95% C.I.) | Adjusted HR (95% C.I.) | Adjusted HR (95% C.I.) | ||
| Main model † | 1.00 | 0.95(0.72, 1.26) | 0.88(0.67, 1.16) | 0.42(0.29, 0.61) *** | <0.001 |
| Subgroup effects | |||||
| Age, years | |||||
| 55–64 | 1.00 | 0.60(0.32, 1.11) | 0.66(0.35, 1.24) | 0.56(0.24, 1.28) | 0.041 |
| 65–74 | 1.00 | 1.08(0.71, 1.64) | 0.90(0.60, 1.36) | 0.37(0.23, 0.62) *** | <0.001 |
| ≥75 | 1.00 | 0.82(0.49, 1.37) | 0.68(0.41, 1.12) | 0.31(0.15, 0.66) ** | 0.002 |
| Sex | |||||
| Female | 1.00 | 1.01(0.63, 1.63) | 0.97(0.61, 1.53) | 0.53(0.30, 0.95) * | 0.076 |
| Male | 1.00 | 0.93(0.65, 1.32) | 0.84(0.59, 1.20) | 0.35(0.21, 0.57) *** | <0.001 |
| CCI Index | |||||
| 0 | 1.00 | 0.97(0.58, 1.62) | 0.72(0.41, 1.26) | 0.35(0.17, 0.75) ** | 0.006 |
| 1 | 1.00 | 0.71(0.37, 1.34) | 1.08(0.63, 1.86) | 0.50(0.25, 0.99) * | 0.130 |
| 2 | 1.00 | 1.20(0.66, 2.17) | 1.03(0.57, 1.86) | 0.40(0.16, 0.97) * | 0.124 |
| ≥3 | 1.00 | 0.89(0.52, 1.52) | 0.70(0.40, 1.21) | 0.38(0.18, 0.80) * | 0.009 |
| Hypertension | |||||
| No | 1.00 | 1.11(0.70, 1.76) | 1.14(0.72, 1.81) | 0.56(0.31, 1.01) | 0.196 |
| Yes | 1.00 | 0.86(0.60, 1.24) | 0.77(0.54, 1.09) | 0.35(0.22, 0.57) *** | <0.001 |
| Dyslipidemia | |||||
| No | 1.00 | 0.90(0.63, 1.27) | 0.98(0.70, 1.36) | 0.39(0.24, 0.62) *** | 0.001 |
| Yes | 1.00 | 1.06(0.65, 1.72) | 0.69(0.41, 1.16) | 0.46(0.24, 0.85) * | 0.010 |
| Insulins and analogues | |||||
| No (<28 days) | 1.00 | 0.93(0.69, 1.26) | 0.84(0.62, 1.13) | 0.36(0.23, 0.54) *** | <0.001 |
| Yes (≥28 days) | 1.00 | 1.07(0.49, 2.33) | 1.12(0.54, 2.34) | 0.75(0.32, 1.75) | 0.666 |
| Biguanides | |||||
| No (<28 days) | 1.00 | 0.73(0.47, 1.13) | 0.67(0.43, 1.04) | 0.30(0.15, 0.59) *** | <0.001 |
| Yes (≥28 days) | 1.00 | 1.09(0.75, 1.58) | 1.02(0.71, 1.46) | 0.49(0.31, 0.77) ** | 0.013 |
| Sulfonamides, urea derivatives | |||||
| No (<28 days) | 1.00 | 0.81(0.53, 1.25) | 0.59(0.37, 0.94) * | 0.35(0.19, 0.65) *** | <0.001 |
| Yes (≥28 days) | 1.00 | 1.04(0.72, 1.52) | 1.08(0.76, 1.54) | 0.45(0.28, 0.72) *** | 0.011 |
| Alpha glucosidase inhibitors | |||||
| No (<28 days) | 1.00 | 0.86(0.63, 1.17) | 0.85(0.63, 1.15) | 0.41(0.27, 0.62) *** | <0.001 |
| Yes (≥28 days) | 1.00 | 1.63(0.78, 3.40) | 1.04(0.47, 2.32) | 0.45(0.16, 1.24) | 0.197 |
| Thiazolidinediones | |||||
| No (<28 days) | 1.00 | 0.94(0.70, 1.26) | 0.81(0.60, 1.09) | 0.37(0.25, 0.55) *** | <0.001 |
| Yes (≥28 days) | 1.00 | 0.96(0.35, 2.60) | 1.57(0.69, 3.62) | 0.88(0.31, 2.54) | 0.783 |
| Dipeptidyl peptidase 4 (DPP-4) | |||||
| No (<28 days) | 1.00 | 0.93(0.70, 1.24) | 0.85(0.64, 1.12) | 0.40(0.28, 0.59) *** | <0.001 |
| Yes (≥28 days) | 1.00 | 0.61(0.07, 5.21) | 1.50(0.35, 6.34) | 0.46(0.05, 4.30) | 0.782 |
| Oral blood glucose lowering | |||||
| No (< 28 days) | 1.00 | 0.98(0.73, 1.31) | 0.88(0.66, 1.18) | 0.43(0.29, 0.63) *** | <0.001 |
| Yes (≥28 days) | 1.00 | 0.44(0.10, 1.96) | 0.72(0.22, 2.31) | 0.14(0.02, 1.15) | 0.062 |
| Other hypoglycemic medications | |||||
| No (<28 days) | 1.00 | 0.99(0.74, 1.32) | 0.80(0.59, 1.08) | 0.39(0.26, 0.59) *** | <0.001 |
| Yes (≥28 days) | 1.00 | 0.38(0.09, 1.66) | 1.66(0.75, 3.65) | 0.54(0.17, 1.69) | 0.822 |
| Number of hypoglycemic medications | |||||
| 0–1 | 1.00 | 0.70(0.45, 1.10) | 0.55(0.34, 0.87) * | 0.32(0.17, 0.59) *** | <0.001 |
| 2–3 | 1.00 | 1.34(0.89, 2.03) | 1.02(0.66, 1.57) | 0.42(0.23, 0.76) ** | 0.022 |
| >3 | 1.00 | 0.66(0.29, 1.51) | 1.30(0.69, 2.44) | 0.53(0.23, 1.21) | 0.387 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zheng, J.-Q.; Lin, C.-H.; Chen, C.-C.; Lin, Y.-F.; Chiu, C.-C.; Yang, T.Y.; Hsu, M.-H.; Fang, Y.-A.; Hao, W.-R.; Liu, J.-C.; et al. Role of Annual Influenza Vaccination against Lung Cancer in Type 2 Diabetic Patients from a Population-Based Cohort Study. J. Clin. Med. 2021, 10, 3434. https://doi.org/10.3390/jcm10153434
Zheng J-Q, Lin C-H, Chen C-C, Lin Y-F, Chiu C-C, Yang TY, Hsu M-H, Fang Y-A, Hao W-R, Liu J-C, et al. Role of Annual Influenza Vaccination against Lung Cancer in Type 2 Diabetic Patients from a Population-Based Cohort Study. Journal of Clinical Medicine. 2021; 10(15):3434. https://doi.org/10.3390/jcm10153434
Chicago/Turabian StyleZheng, Jing-Quan, Cheng-Hsin Lin, Chun-Chao Chen, Yuan-Feng Lin, Chun-Chih Chiu, Tsung Yeh Yang, Min-Huei Hsu, Yu-Ann Fang, Wen-Rui Hao, Ju-Chi Liu, and et al. 2021. "Role of Annual Influenza Vaccination against Lung Cancer in Type 2 Diabetic Patients from a Population-Based Cohort Study" Journal of Clinical Medicine 10, no. 15: 3434. https://doi.org/10.3390/jcm10153434
APA StyleZheng, J.-Q., Lin, C.-H., Chen, C.-C., Lin, Y.-F., Chiu, C.-C., Yang, T. Y., Hsu, M.-H., Fang, Y.-A., Hao, W.-R., Liu, J.-C., & Lee, K.-Y. (2021). Role of Annual Influenza Vaccination against Lung Cancer in Type 2 Diabetic Patients from a Population-Based Cohort Study. Journal of Clinical Medicine, 10(15), 3434. https://doi.org/10.3390/jcm10153434









