The Comparison of Breast Reconstruction Using Two Types of Acellular Dermal Matrix after Breast-Conserving Surgery
Abstract
:1. Introduction
2. Patients and Methods
2.1. Patient Selection
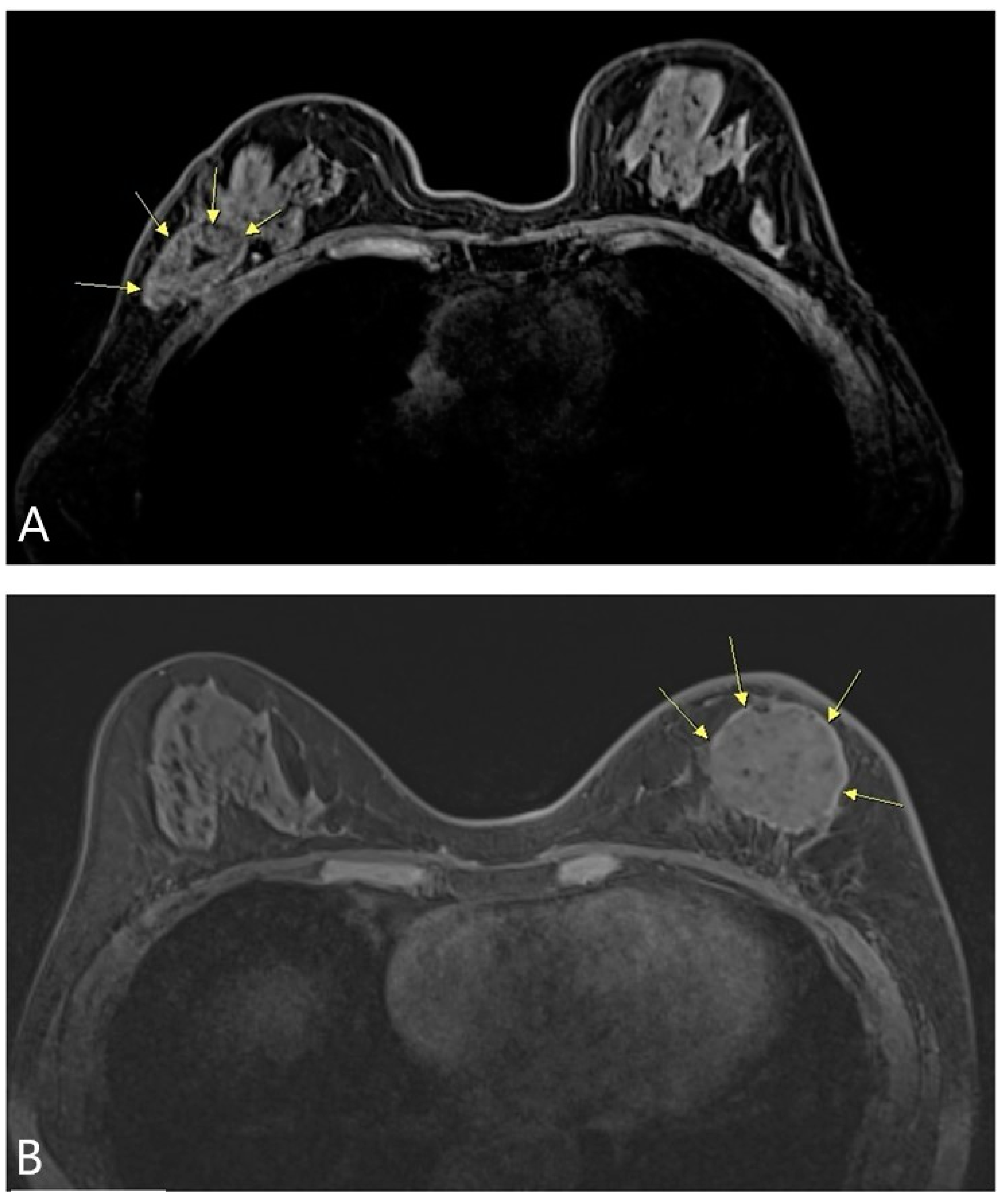
2.2. Surgical Technique
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kang, S.Y.; Lee, S.B.; Kim, Y.S.; Kim, Z.; Kim, H.Y.; Kim, H.J.; Park, S.; Bae, S.Y.; Yoon, K.; Lee, S.K.; et al. Breast Cancer Statistics in Korea, 2018. J. Breast Cancer 2021, 24, 123–137. [Google Scholar] [CrossRef] [PubMed]
- Bertozzi, N.; Pesce, M.; Santi, P.L.; Raposio, E. Oncoplastic breast surgery: Comprehensive review. Eur. Rev. Med. Pharmacol. Sci. 2017, 21, 2572–2585. [Google Scholar]
- Thiessen, F.E.F.; Tjalma, W.A.A.; Tondu, T. Breast reconstruction after breast conservation therapy for breast cancer. Eur. J. Obstet. Gynecol. Reprod. Biol. 2018, 230, 233–238. [Google Scholar] [CrossRef]
- Hallberg, H.; Rafnsdottir, S.; Selvaggi, G.; Strandell, A.; Samuelsson, O.; Stadig, I.; Svanberg, T.; Hansson, E.; Lewin, R. Benefits and risks with acellular dermal matrix (ADM) and mesh support in immediate breast reconstruction: A systematic review and meta-analysis. J. Plast. Surg. Hand Surg. 2018, 52, 130–147. [Google Scholar] [CrossRef]
- Gravina, P.R.; Pettit, R.W.; Davis, M.J.; Winocour, S.J.; Selber, J.C. Evidence for the use of acellular dermal matrix in implant-based breast reconstruction. Semin. Plast. Surg. 2019, 33, 229–235. [Google Scholar] [CrossRef] [PubMed]
- Wazir, U.; Mokbel, K. The evolving role of pre-pectoral ADM-assisted implant-based immediate breast reconstruction following skin-sparing mastectomy. Am. J. Surg. 2018, 216, 639–640. [Google Scholar] [CrossRef]
- Cabalag, M.S.; Rostek, M.; Miller, G.S.; Chae, M.P.; Quinn, T.; Rozen, W.M.; Hunter-Smith, D.J. Alloplastic adjuncts in breast reconstruction. Gland Surg. 2016, 5, 158–173. [Google Scholar] [CrossRef] [PubMed]
- Sorkin, M.; Qi, J.; Kim, H.M.; Hamill, J.B.; Kozlow, J.H.; Pusic, A.L.; Wilkins, E.G. Acellular dermal matrix in immediate expander/implant breast reconstruction: A multicenter assessment of risks and benefits. Plast. Reconstr. Surg. 2017, 140, 1091–1100. [Google Scholar] [CrossRef] [PubMed]
- Clavien, P.A.; Barkun, J.; de Oliveira, M.L.; Vauthey, J.N.; Dindo, D.; Schulick, R.D.; de Santibañes, E.; Pekolj, J.; Slankamenac, K.; Bassi, C.; et al. The Clavien-Dindo classification of surgical complications: Five-year experience. Ann. Surg. 2009, 250, 187–196. [Google Scholar] [CrossRef] [Green Version]
- Meattini, I.; Becherini, C.; Bernini, M.; Bonzano, E.; Criscitiello, C.; De Rose, F.; De Santis, M.C.; Fontana, A.; Franco, P.; Gentilini, O.D.; et al. Breast reconstruction and radiation therapy: An Italian expert Delphi consensus statements and critical review. Cancer Treat. Rev. 2021, 99, 102236. [Google Scholar] [CrossRef]
- Von Smitten, K. Surgical management of breast cancer in the future. Acta Oncol. 2000, 39, 437–439. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, H.N.; Hardman, M.J. Wound healing: Cellular mechanisms and pathological outcomes. Open Biol. 2020, 10, 200223. [Google Scholar] [CrossRef]
- Versey, Z.; da Cruz Nizer, W.S.; Russell, E.; Zigic, S.; DeZeeuw, K.G.; Marek, J.E.; Overhage, J.; Cassol, E. Biofilm-Innate Immune Interface: Contribution to Chronic Wound Formation. Front. Immunol. 2021, 12, 648554. [Google Scholar] [CrossRef]
- Franceschini, G.; Masetti, R. Acellular dermal matrix as filler in breast-conserving surgery: Warnings for a careful use. World J. Surg. Oncol. 2021, 19, 1. [Google Scholar] [CrossRef] [PubMed]
- Sethi, D.; Sen, R.; Parshad, S.; Khetarpal, S.; Garg, M.; Sen, J. Histopathologic changes following neoadjuvant chemotherapy in various malignancies. Int. J. Appl. Basic Med. Res. 2012, 2, 111–116. [Google Scholar] [CrossRef] [Green Version]
- Ridker, P.M. Hyperlipidemia as an instigator of inflammation: Inaugurating new approaches to vascular prevention. J. Am. Heart Assoc. 2012, 1, 3–5. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Yang, J.D.; Lee, J.W.; Li, J.; Jung, J.H.; Kim, W.W.; Park, C.S.; Lee, J.S.; Park, H.Y. Acellular dermal matrix combined with oxidized regenerated cellulose for partial breast reconstruction: Two case reports. Medicine 2020, 99, e21217. [Google Scholar] [CrossRef]
- Rassu, P.C. Observed outcomes on the use of oxidized and regenerated cellulose polymer for breast conserving surgery—A case series. Ann. Med. Surg. 2015, 5, 57–66. [Google Scholar] [CrossRef]
- Langdon, R.C.; Cuono, C.B.; Birchall, N.; Madri, J.A.; Kuklinska, E.; McGuire, J.; Moellmann, G.E. Reconstitution of structure and cell function in human skin grafts derived from cryopreserved allogeneic dermis and autologous cultured keratinocytes. J. Investig. Dermatol. 1988, 91, 478–485. [Google Scholar] [CrossRef] [Green Version]
- Tognetti, L.; Pianigiani, E.; Ierardi, F.; Lorenzini, G.; Casella, D.; Liso, F.G.; De Pascalis, A.; Cinotti, E.; Rubegni, P. The use of human acellular dermal matrices in advanced wound healing and surgical procedures: State of the art. Dermatol. Ther. 2021, e14987. [Google Scholar] [CrossRef]
- Cooper, J.; Mirzayan, R. Acellular Dermal Matrix in Rotator Cuff Surgery. Am. J. Orthop. 2016, 45, 301–305. [Google Scholar] [PubMed]
- Haney, N.M.; Huang, M.M.; Liu, J.L.; Hawksworth, D.J.; Burnett, A.L. Acellular Dermal Matrix tissues in genitourinary reconstructive surgery: A review of the literature and case discussions. Sex. Med. Rev. 2020. [Google Scholar] [CrossRef] [PubMed]
- Gwak, H.; Jeon, Y.W.; Lim, S.T.; Park, S.Y.; Suh, Y.J. Volume replacement with diced acellular dermal matrix in oncoplastic breast-conserving surgery: A prospective single-center experience. World J. Surg. Oncol. 2020, 18, 60. [Google Scholar] [CrossRef]
- Schwartz, J.D. Use of a Bioabsorbable Implant-Acellular Dermal Matrix Construct to Facilitate Oncoplastic Breast-conserving Surgery. Plast. Reconstr. Surg. Glob. Open 2021, 9, e3356. [Google Scholar] [CrossRef]
- Ichinose, Y.; Kosaka, Y.; Saeki, T.; Fujimoto, A.; Nukui, A.; Asano, A.; Shimada, H.; Matsuura, K.; Hasebe, T.; Osaki, A. Granuloma after breast conserving surgery—A report of three cases. J. Surg. Case Rep. 2021, 2021, rjab199. [Google Scholar] [CrossRef] [PubMed]




| Total | Sheet-Type ADM | Pellet-Type ADM | ||
|---|---|---|---|---|
| Age | Mean ± SD (Range) | 51.8 ± 9.3 (27–74) | 52.5 ± 10.8 (31–74) | 51.6 ± 8.8 (27–71) |
| BMI | Mean ± SD (Range) | 23.8 ± 3.8 (16.6–36.8) | 22.7 ± 3.8 (17.2–35.9) | 24.2 ± 3.8 (16.6–36.8) |
| Hight | Mean ± SD (Range) | 158.8 ± 5.3 (143.8–173.1) | 158.5 ± 5.4 (143.8–168) | 158.9 ± 5.3 (146–173.1) |
| Weight | Mean ± SD (Range) | 60.1 ± 10.5 (42.5–97.8) | 57.1 ± 10.9 (43.7–97.8) | 61.1 ± 10.2 (42.5–91.7) |
| Stage | Range | Stage 0–IIIA | Stage 0–IIIA | Stage 0–II |
| Total operation time | Mean ± SD (Range) | 100.4 ± 22.1 (40–200) | 94.9 ± 23.6 (40–150) | 101.7 ± 21.9 (55–200) |
| Category | Patient Number (%) | |
|---|---|---|
| Cases | Sheet-type ADM | 33 (24.63%) |
| Pellet-type ADM | 101 (75.37%) | |
| Complication cases | Sheet-type ADM | 5 (3.73%) |
| Pellet-type ADM | 1 (0.75%) | |
| Classification of complication | Major | 0 |
| Minor | 6 (4.48%) | |
| Types of complication | Hematoma | 1 (0.75%) |
| Infection | 4 (2.99%) | |
| Granuloma | 1 (0.75%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
An, J.; Kwon, H.; Lim, W.; Moon, B.-I.; Paik, N.S. The Comparison of Breast Reconstruction Using Two Types of Acellular Dermal Matrix after Breast-Conserving Surgery. J. Clin. Med. 2021, 10, 3430. https://doi.org/10.3390/jcm10153430
An J, Kwon H, Lim W, Moon B-I, Paik NS. The Comparison of Breast Reconstruction Using Two Types of Acellular Dermal Matrix after Breast-Conserving Surgery. Journal of Clinical Medicine. 2021; 10(15):3430. https://doi.org/10.3390/jcm10153430
Chicago/Turabian StyleAn, Jeongshin, Hyungju Kwon, Woosung Lim, Byung-In Moon, and Nam Sun Paik. 2021. "The Comparison of Breast Reconstruction Using Two Types of Acellular Dermal Matrix after Breast-Conserving Surgery" Journal of Clinical Medicine 10, no. 15: 3430. https://doi.org/10.3390/jcm10153430
APA StyleAn, J., Kwon, H., Lim, W., Moon, B.-I., & Paik, N. S. (2021). The Comparison of Breast Reconstruction Using Two Types of Acellular Dermal Matrix after Breast-Conserving Surgery. Journal of Clinical Medicine, 10(15), 3430. https://doi.org/10.3390/jcm10153430






