Early vs. Late Tracheostomy in Patients with Traumatic Brain Injury: Systematic Review and Meta-Analysis
Abstract
1. Introduction
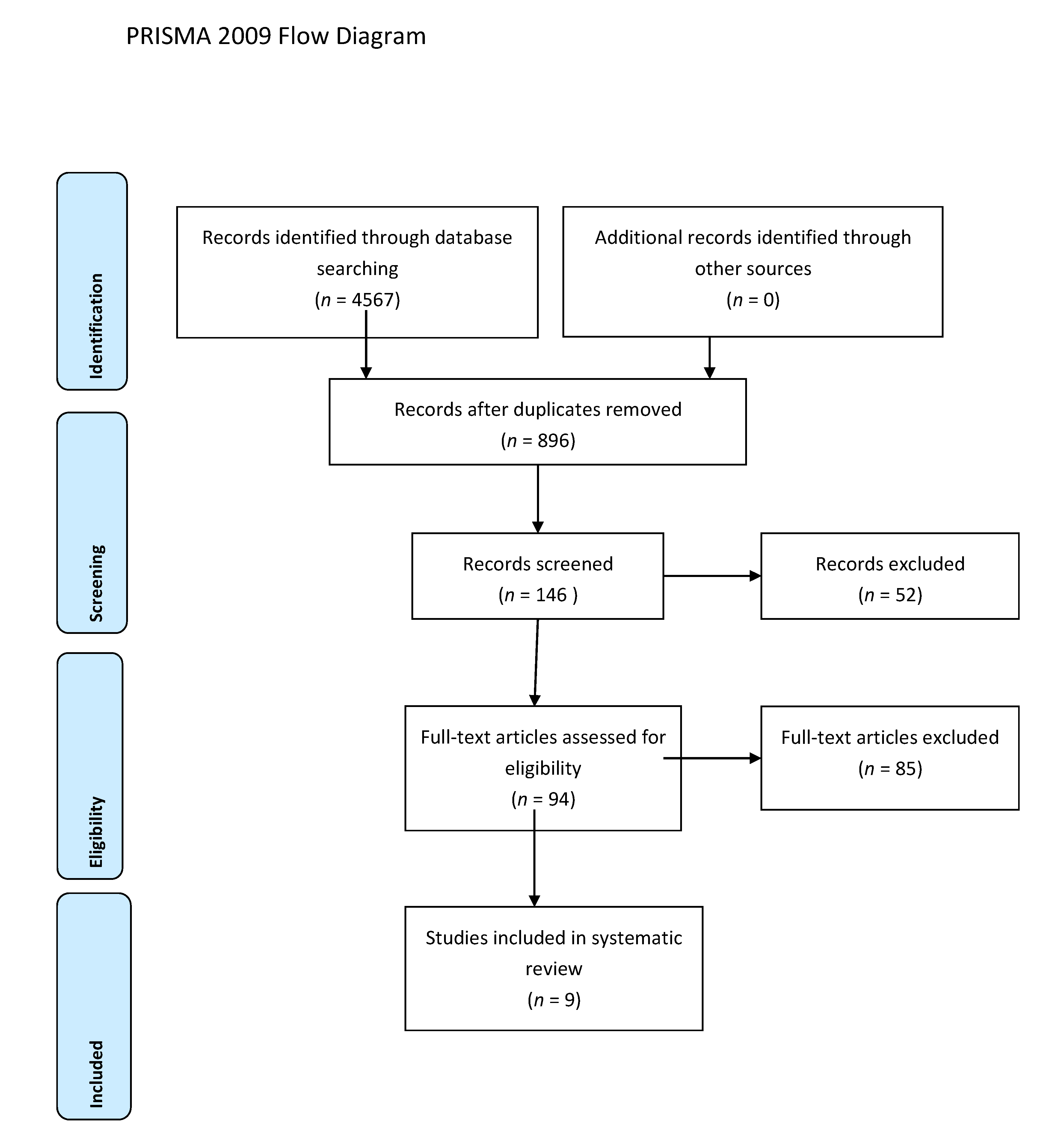
2. Materials and Methods
3. Data Extraction
4. Risk of Bias
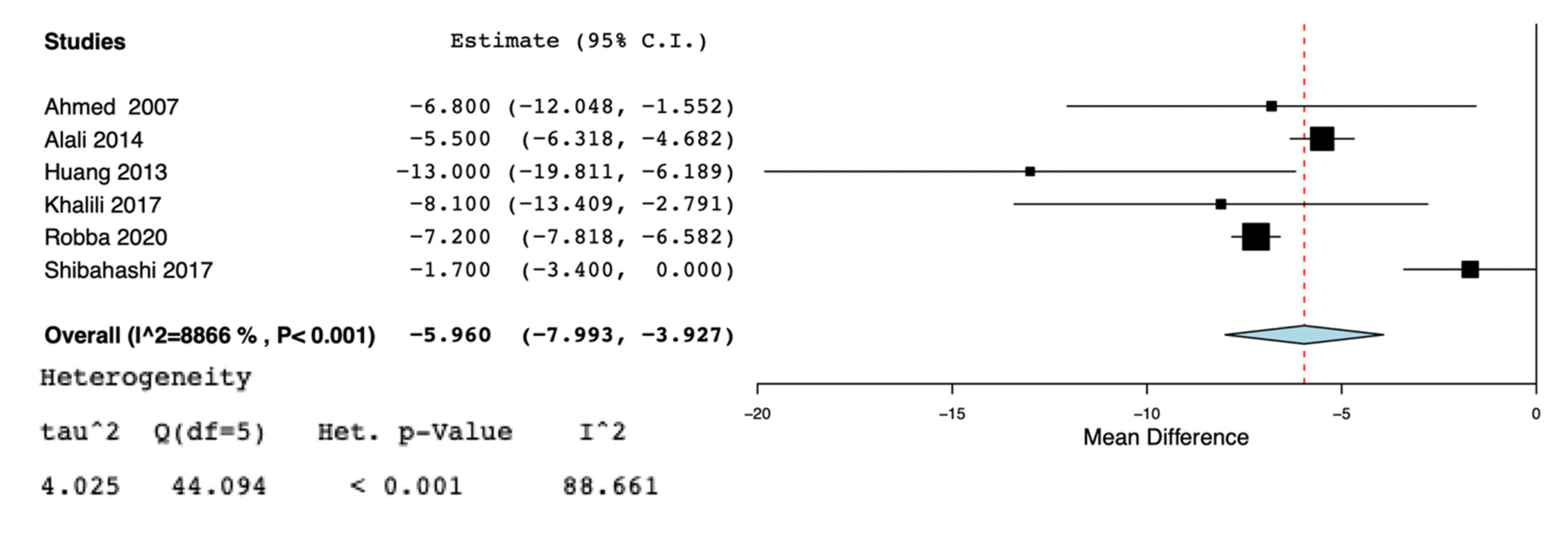
5. Data Synthesis and Analysis
6. Results
7. Discussion
8. Conclusions and Future Perspectives
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- De Franca, S.A.; Tavares, W.M.; Salinet, A.S.M.; Paiva, W.; Teixeira, M.J. Early Tracheostomy in Severe Traumatic Brain Injury Patients: A meta-analysis and comparison with late tracheostomy. Crit. Care Med. 2020, 48, e325–e331. [Google Scholar] [CrossRef]
- Dewan, M.C.; Rattani, A.; Gupta, S.; Baticulon, R.; Hung, Y.-C.; Punchak, M.; Agrawal, A.; Adeleye, A.O.; Shrime, M.G.; Rubiano, A.M.; et al. Estimating the global incidence of traumatic brain injury. J. Neurosurg. 2019, 130, 1080–1097. [Google Scholar] [CrossRef]
- Lu, Q.; Xie, Y.; Qi, X.; Li, X.; Yang, S.; Wang, Y. Is Early Tracheostomy Better for Severe Traumatic Brain Injury? A Meta-Analysis. World Neurosurg. 2018, 112, e324–e330. [Google Scholar] [CrossRef]
- Rumbak, M.J.; Newton, M.; Truncale, T.; Schwartz, S.W.; Adams, J.W.; Hazard, P.B. A prospective, randomized, study comparing early percutaneous dilational tracheotomy to prolonged translaryngeal intubation (delayed tracheotomy) in critically ill medical patients. Crit. Care Med. 2004, 32, 1689–1694. [Google Scholar] [CrossRef]
- Robba, C.; The CENTER-TBI ICU Participants and Investigators; Galimberti, S.; Graziano, F.; Wiegers, E.J.A.; Lingsma, H.F.; Iaquaniello, C.; Stocchetti, N.; Menon, D.; Citerio, G. Tracheostomy practice and timing in traumatic brain-injured patients: A CENTER-TBI study. Intensiv. Care Med. 2020, 46, 983–994. [Google Scholar] [CrossRef] [PubMed]
- Raimondi, N.; Vial, M.R.; Calleja, J.; Quintero, A.; Cortés, A.; Celis, E.; Pacheco, C.; Ugarte, S.; Añón, J.M.; Hernández, G.; et al. Evidence-based guidelines for the use of tracheostomy in critically ill patients. J. Crit. Care 2017, 38, 304–318. [Google Scholar] [CrossRef] [PubMed]
- Lazaridis, C.; DeSantis, S.M.; McLawhorn, M.; Krishna, V. Liberation of neurosurgical patients from mechanical ventilation and tracheostomy in neurocritical care. J. Crit. Care 2012, 27, 417.e1–417.e8. [Google Scholar] [CrossRef] [PubMed]
- Siempos, I.I.; Ntaidou, T.K.; Filippidis, F.; Choi, A.M.K. Effect of early versus late or no tracheostomy on mortality and pneumonia of critically ill patients receiving mechanical ventilation: A systematic review and meta-analysis. Lancet Respir. Med. 2015, 3, 150–158. [Google Scholar] [CrossRef]
- Andriolo, B.N.G.; Andriolo, R.B.; Saconato, H.; Atallah, Á.N.; Valente, O. Early versus late tracheostomy for critically ill patients. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef] [PubMed]
- Szakmany, T.; Russell, P.; Wilkes, A.R.; Hall, J.E. Effect of early tracheostomy on resource utilization and clinical outcomes in critically ill patients: Meta-analysis of randomized controlled trials. Br. J. Anaesth. 2015, 114, 396–405. [Google Scholar] [CrossRef]
- Alali, A.S.; Scales, D.C.; Fowler, R.A.; Mainprize, T.G.; Ray, J.G.; Kiss, A.; de Mestral, C.; Nathens, A.B. Tracheostomy timing in traumatic brain injury. J. Trauma Acute Care Surg. 2014, 76, 70–78. [Google Scholar] [CrossRef]
- Pinheiro, B.D.V.; Tostes, R.D.O.; Brum, C.I.; Carvalho, E.V.; Pinto, S.P.S.; De Oliveira, J.C.A. Early versus late tracheostomy in patients with acute severe brain injury. J. Bras. Pneumol. 2010, 36, 84–91. [Google Scholar] [CrossRef]
- Wang, H.-K.; Lu, K.; Liliang, P.-C.; Wang, K.-W.; Chen, H.-J.; Chen, T.-B.; Liang, C.-L. The impact of tracheostomy timing in patients with severe head injury: An observational cohort study. Injury 2012, 43, 1432–1436. [Google Scholar] [CrossRef]
- Rizk, E.B.; Patel, A.S.; Stetter, C.M.; Chinchilli, V.M.; Cockroft, K.M. Impact of Tracheostomy Timing on Outcome After Severe Head Injury. Neurocritical Care 2011, 15, 481–489. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandom-Ised Studies in Meta-Analyses; Ottawa Hospital Research Institute: Ottawa, ON, USA, 2000. [Google Scholar]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials revisited. Contemp. Clin. Trials 2015, 45, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Hozo, S.P.; Djulbegovic, B.; Hozo, I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med. Res. Methodol. 2005, 5, 13. [Google Scholar] [CrossRef]
- Dunham, C.M.; Cutrona, A.F.; Gruber, B.S.; Calderon, J.E.; Ransom, K.J.; Flowers, L.L. Early tracheostomy in severe traumatic brain injury: Evidence for decreased mechanical ventilation and increased hospital mortality. Int. J. Burn. Trauma 2014, 4, 14–24. [Google Scholar]
- Huang, Y.-H.; Lee, T.-C.; Liao, C.-C.; Deng, Y.-H.; Kwan, A.-L. Tracheostomy in craniectomised survivors after traumatic brain injury: A cross-sectional analytical study. Injury 2013, 44, 1226–1231. [Google Scholar] [CrossRef]
- Khalili, H.; Paydar, S.; Safari, R.; Arasteh, P.; Niakan, A.; Foroughi, A.A. Experience with Traumatic Brain Injury: Is Early Tracheostomy Associated with Better Prognosis? World Neurosurg. 2017, 103, 88–93. [Google Scholar] [CrossRef] [PubMed]
- Shibahashi, K.; Sugiyama, K.; Houda, H.; Takasu, Y.; Hamabe, Y.; Morita, A. The effect of tracheostomy performed within 72 h after traumatic brain injury. Br. J. Neurosurg. 2017, 31, 564–568. [Google Scholar] [CrossRef]
- Bouderka, M.A.; Fakhir, B.; Bouaggad, A.; Hmamouchi, B.; Hamoudi, D.; Harti, A. Early Tracheostomy versus Prolonged Endotracheal Intubation in Severe Head Injury. J. Trauma Inj. Infect. Crit. Care 2004, 57, 251–254. [Google Scholar] [CrossRef] [PubMed]
- Sugerman, H.J.; Wolfe, L.; Pasquale, M.D.; Rogers, F.B.; O’Malley, K.F.; Knudson, M.; Dinardo, L.; Gordon, M.; Schaffer, S. Multicenter, Randomized, Prospective Trial of Early Tracheostomy. J. Trauma Inj. Infect. Crit. Care 1997, 43, 741–747. [Google Scholar] [CrossRef] [PubMed]
- Sabelnikovs, O.; The LUNG-SAFE Investigators and the ESICM Trials Group; Madotto, F.; Pham, T.; Nagata, I.; Uchida, M.; Tamiya, N.; Kurahashi, K.; Bellani, G.; Laffey, J.G. Epidemiology and patterns of tracheostomy practice in patients with acute respiratory distress syndrome in ICUs across 50 countries. Crit. Care 2018, 22, 195. [Google Scholar] [CrossRef]
- Mehta, A.B.; Syeda, S.N.; Bajpayee, L.; Cooke, C.R.; Walkey, A.; Wiener, R. Trends in Tracheostomy for Mechanically Ventilated Patients in the United States, 1993–2012. Am. J. Respir. Crit. Care Med. 2015, 192, 446–454. [Google Scholar] [CrossRef]
- Vargas, M.; Pelosi, P.; Servillo, G. Percutaneous tracheostomy: It’s time for a shared approach! Crit. Care 2014, 18, 448. [Google Scholar] [CrossRef]
- Vargas, M.; Sutherasan, Y.; Antonelli, M.; Brunetti, I.; Corcione, A.; Laffey, J.G.; Putensen, C.; Servillo, G.; Pelosi, P. Tracheostomy procedures in the intensive care unit: An international survey. Crit. Care 2015, 19, 362. [Google Scholar] [CrossRef] [PubMed]
- Durbin, C.G. Indications for and timing of tracheostomy. Respir. Care 2005, 50, 483–487. [Google Scholar]
- Vargas, M.; Servillo, G.; Antonelli, M.; Brunetti, I.; De Stefano, F.; Putensen, C.; Pelosi, P. Informed consent for tracheostomy procedures in Intensive Care Unit: An Italian national survey. Minerva Anestesiol 2013, 79, 741–749. [Google Scholar]
- Frutos-Vivar, F.; Esteban, A.; Apezteguía, C.; Anzueto, A.; Nightingale, P.; González, M.; Soto, L.; Rodrigo, C.; Raad, J.; David, C.M.; et al. Outcome of mechanically ventilated patients who require a tracheostomy. Crit. Care Med. 2005, 33, 290–298. [Google Scholar] [CrossRef]
- Wang, Y.; Guo, Z.; Fan, D.; Lu, H.; Xie, D.; Zhang, D.; Jiang, Y.; Li, P.; Teng, H. A Meta-Analysis of the Influencing Factors for Tracheostomy after Cervical Spinal Cord Injury. BioMed Res. Int. 2018, 2018, 5895830. [Google Scholar] [CrossRef]
- Bösel, J.; Schiller, P.; Hook, Y.; Andes, M.; Neumann, J.-O.; Poli, S.; Amiri, H.; Schönenberger, S.; Peng, Z.; Unterberg, A.; et al. Stroke-Related Early Tracheostomy Versus Prolonged Orotracheal Intubation in Neurocritical Care Trial (SETPOINT). Stroke 2013, 44, 21–28. [Google Scholar] [CrossRef] [PubMed]
- MacIntyre, N. Discontinuing Mechanical Ventilatory Support. Chest 2007, 132, 1049–1056. [Google Scholar] [CrossRef] [PubMed]
- Blot, F.; Similowski, T.; Trouillet, J.-L.; Chardon, P.; Korach, J.-M.; Costa, M.-A.; Journois, D.; Thiéry, G.; Fartoukh, M.; Pipien, I.; et al. Early tracheotomy versus prolonged endotracheal intubation in unselected severely ill ICU patients. Intensive care Med. 2008, 34, 1779–1787. [Google Scholar] [CrossRef] [PubMed]
- Chastre, J.; Fagon, J. State of the Art Ventilator-associated Pneumonia. Am. J. Respir. Crit. Care Med. 2002. [Google Scholar] [CrossRef] [PubMed]
- Combes, A.; Figliolini, C.; Trouillet, J.-L.; Kassis, N.; Wolff, M.; Gibert, C.; Chastre, J. Incidence and outcome of polymicrobial ventilator-associated pneumonia. Chest 2002, 121, 1618–1623. [Google Scholar] [CrossRef]
- Hui, X.; Haider, A.H.; Hashmi, Z.G.; Rushing, A.P.; Dhiman, N.; Scott, V.K.; Selvarajah, S.; Haut, E.; Efron, D.T.; Schneider, E.B. Increased risk of pneumonia among ventilated patients with traumatic brain injury: Every day counts! J. Surg. Res. 2013, 184, 438–443. [Google Scholar] [CrossRef]
- McCredie, V.A.; Alali, A.S.; Scales, D.C.; Adhikari, N.K.J.; Rubenfeld, G.D.; Cuthbertson, B.H.; Nathens, A.B. Effect of Early versus Late Tracheostomy or Prolonged Intubation in Critically Ill Patients with Acute Brain Injury: A Systematic Review and Meta-Analysis. Neurocritical Care 2017, 26, 14–25. [Google Scholar] [CrossRef]
- Romero, J.; Vari, A.; Gambarrutta, C.; Oliviero, A. Tracheostomy timing in traumatic spinal cord injury. Eur. Spine J. 2009, 18, 1452–1457. [Google Scholar] [CrossRef]
- Brook, A.; Sherman, G.; Malen, J.; Kollef, M. Early versus late tracheostomy in patients who require prolonged mechanical ventilation. Am. J. Crit. Care 2000, 9, 352–359. [Google Scholar] [CrossRef]
- Jeon, Y.-T.; Hwang, J.-W.; Lim, Y.-J.; Lee, S.-Y.; Woo, K.-I.; Park, H.-P. Effect of Tracheostomy Timing on Clinical Outcome in Neurosurgical Patients. J. Neurosurg. Anesthesiol. 2014, 26, 22–26. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, J.; Barber, V.S.; Morgan, L.; Young, J.D. Systematic review and meta-analysis of studies of the timing of tracheostomy in adult patients undergoing artificial ventilation. BMJ 2005, 330, 1243. [Google Scholar] [CrossRef]
- Vargas, M.; Sutherasan, Y.; Brunetti, I.; Micalizzi, C.; Insorsi, A.; Ball, L.; Folentino, M.; Sileo, R.; De Lucia, A.; Cerana, M.; et al. Mortality and long-term quality of life after percutaneous tracheotomy in Intensive Care Unit: A prospective observational study. Minerva Anestesiol. 2018, 84, 1024–1031. [Google Scholar] [CrossRef] [PubMed]
- Cheung, N.H.; Napolitano, L.M. Tracheostomy: Epidemiology, Indications, Timing, Technique, and Outcomes. Respir. Care 2014, 59, 895–919. [Google Scholar] [CrossRef] [PubMed]
- Cox, C.E.; Carson, S.S.; Holmes, G.M.; Howard, A.; Carey, T.S. Increase in tracheostomy for prolonged mechanical ventilation in North Carolina, 1993–2002. Crit. Care Med. 2004, 32, 2219–2226. [Google Scholar] [CrossRef]




| Authors | Study Design | Age (Years) in ET vs. LT Groups | Sex (Male) in ET vs. LT Groups | GCS Score Information ET vs. LT Groups | How Early Tracheostomy Was Defined by the Studies |
|---|---|---|---|---|---|
| Alali et al. [12] | Retrospective cohort | 49 (30–64) vs. 53 (35–68) | 75.6% vs. 73% | 4 (3–7) vs. 7 (3–13) | ≤8 days |
| Bouderka et al. [23] | Retrospective cohort | NA | NA | NA | <7 days |
| Dunham et al. [19] | Randomized controlled trial | NA | NA | NA | 3–5 days of endotracheal tube |
| Huang et al. [20] | Cross-sectional study | NA | NA | NA | ≤10 days after decompressive tracheotomy |
| Khalili et al. [21] | Observational cohort | 41.6 vs. 37.8 | 50% vs. 86% | 6.15 vs. 5.70 | ≤6 days |
| Robba et al. [6] | Prospective observational | 48.5 (31–67) vs. 44 (28–59 | 77.2% vs. 76.7% | 5.5 (3–10 vs. 5 (3–9) | ≤7 days |
| Shibahashi et al. [22] | Retrospective cohort | 68 (62–74) vs. 68 (53–74) | 33 vs. 33 | 6 (3–7) vs. 6 (6–9) | ≤3 days |
| Surgeman et al. [24] | Randomized controlled trial | NA | NA | NA | 3–5 days |
| Wang et al. [14] | Observational cohort | 55.3 (19–80) vs. 57.5 (18–85) | 87.5% vs. 66% | 5.9 (3–8) vs. 5.7 83–8) | ≤10 days |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marra, A.; Vargas, M.; Buonanno, P.; Iacovazzo, C.; Coviello, A.; Servillo, G. Early vs. Late Tracheostomy in Patients with Traumatic Brain Injury: Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 3319. https://doi.org/10.3390/jcm10153319
Marra A, Vargas M, Buonanno P, Iacovazzo C, Coviello A, Servillo G. Early vs. Late Tracheostomy in Patients with Traumatic Brain Injury: Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2021; 10(15):3319. https://doi.org/10.3390/jcm10153319
Chicago/Turabian StyleMarra, Annachiara, Maria Vargas, Pasquale Buonanno, Carmine Iacovazzo, Antonio Coviello, and Giuseppe Servillo. 2021. "Early vs. Late Tracheostomy in Patients with Traumatic Brain Injury: Systematic Review and Meta-Analysis" Journal of Clinical Medicine 10, no. 15: 3319. https://doi.org/10.3390/jcm10153319
APA StyleMarra, A., Vargas, M., Buonanno, P., Iacovazzo, C., Coviello, A., & Servillo, G. (2021). Early vs. Late Tracheostomy in Patients with Traumatic Brain Injury: Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 10(15), 3319. https://doi.org/10.3390/jcm10153319





