Balloon Enteroscopy-Assisted Endoscopic Retrograde Cholangiopancreatography for the Treatment of Common Bile Duct Stones in Patients with Roux-en-Y Gastrectomy: Outcomes and Factors Affecting Complete Stone Extraction
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Patients
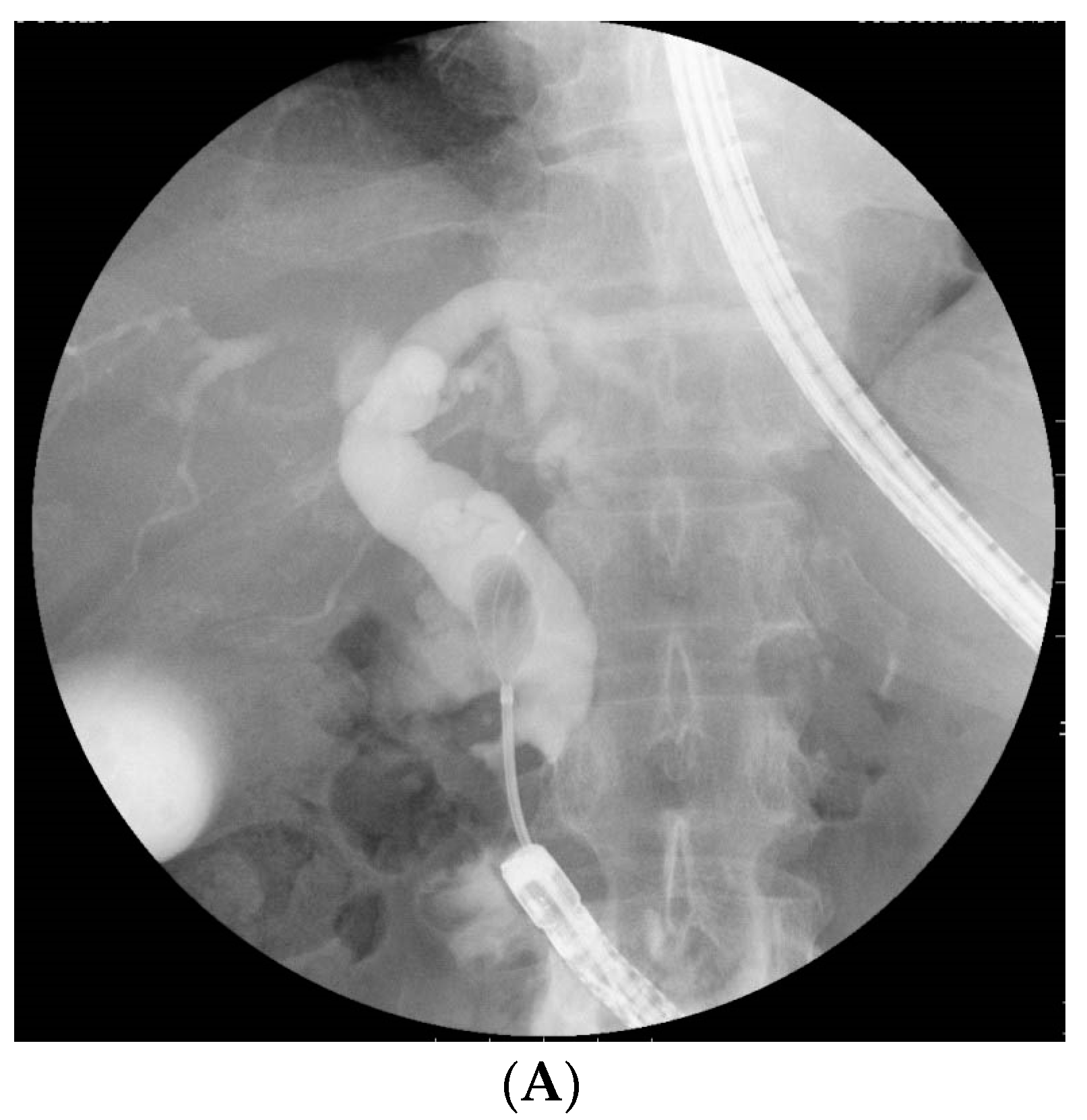
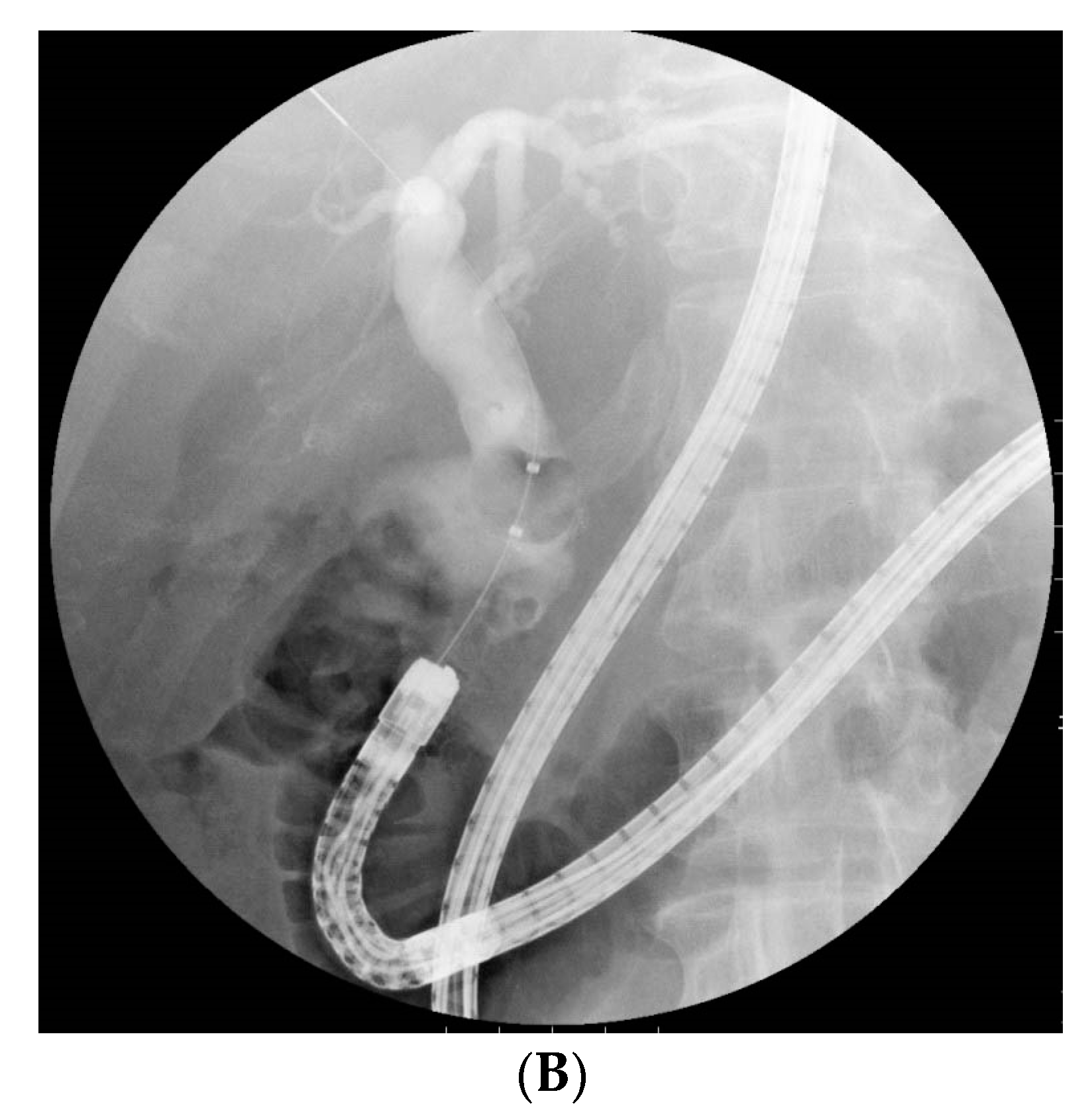
2.3. BE-ERCP Procedure
2.4. Definitions
2.5. Statistical Analyses
3. Results
3.1. Patients’ Characteristics
3.2. Scope Insertion and Biliary Cannulation in an Initial BE-ERCP
3.3. Ampullary Procedure for Stone Extraction at Initial BE-ERCP
3.4. Biliary Intervention and Complete CBD Stone Extraction in an Initial BE-ERCP
3.5. Potential Factors Affecting Complete CBD Stone Extraction
3.6. Adverse Events
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hauters, P.; de Roden, A.d.N.; Pourbaix, A.; Aupaix, F.; Coumans, P.; Therasse, G. Cholelithiasis: A serious complication after total gastrectomy. Br. J. Surg. 1988, 75, 899–900. [Google Scholar] [CrossRef]
- Inoue, K.; Fuchigami, A.; Higashide, S.; Sumi, S.; Kogire, M.; Suzuki, T.; Tobe, T. Gallbladder sludge and stone formation in relation to contractile function after gastrectomy. A prospective study. Ann. Surg. 1992, 215, 19–26. [Google Scholar] [CrossRef]
- Pezzolla, F.; Lantone, G.; Guerra, V.; Misciagna, G.; Prete, F.; Giorgio, I.; Lorusso, D. Influence of the method of digestive tract reconstruction on gallstone development after total gastrectomy for gastric cancer. Am. J. Surg. 1993, 166, 6–10. [Google Scholar] [CrossRef]
- Manes, G.; Paspatis, G.; Aabakken, L.; Anderloni, A.; Arvanitakis, M.; Ah-Soune, P.; Barthet, M.; Domagk, D.; Dumonceau, J.M.; Gigot, J.F.; et al. Endoscopic management of common bile duct stones: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy 2019, 51, 472–491. [Google Scholar] [CrossRef] [Green Version]
- Mukai, S.; Itoi, T.; Baron, T.H.; Takada, T.; Strasberg, S.M.; Pitt, H.A.; Ukai, T.; Shikata, S.; Teoh, A.Y.B.; Kim, M.H.; et al. Indications and techniques of biliary drainage for acute cholangitis in updated Tokyo Guidelines 2018. J. Hepatobiliary Pancreat Sci. 2017, 24, 537–549. [Google Scholar] [CrossRef]
- Hintze, R.E.; Adler, A.; Veltzke, W.; Abou-Rebyeh, H. Endoscopic access to the papilla of Vater for endoscopic retrograde cholangiopancreatography in patients with Billroth II or roux-en-Y gastrojejunostomy. Endoscopy 1997, 29, 69–73. [Google Scholar] [CrossRef]
- Wright, B.E.; Cass, O.W.; Freeman, M.L. ERCP in patients with long-limb Roux-en-Y gastrojejunostomy and intact papilla. Gastrointest. Endosc. 2002, 56, 225–232. [Google Scholar] [CrossRef]
- Gostout, C.J.; Bender, C.E. Cholangiopancreatography, sphincterotomy, and common duct stone removal via Roux-en-Y limb enteroscopy. Gastroenterology 1988, 95, 156–163. [Google Scholar] [CrossRef]
- Nakaji, S.; Hirata, N.; Yamauchi, K.; Shiratori, T.; Kobayashi, M.; Fujii, H.; Ishii, E. Endoscopic retrograde cholangiopancreatography using a cap-assisted highly flexible colonoscope in patients with Roux-en-Y anastomosis. Endoscopy 2014, 46, 529–532. [Google Scholar] [CrossRef] [PubMed]
- Uchida, D.; Tsutsumi, K.; Kato, H.; Matsumi, A.; Saragai, Y.; Tomoda, T.; Matsumoto, K.; Horiguchi, S.; Okada, H. Potential Factors Affecting Results of Short-Type Double-Balloon Endoscope-Assisted Endoscopic Retrograde Cholangiopancreatography. Dig. Dis. Sci. 2020, 65, 1460–1470. [Google Scholar] [CrossRef] [PubMed]
- Clouse, M.; Stokes, K.; Lee, R.; Falchuk, K. Bile duct stones: Percutaneous transhepatic removal. Radiology 1986, 160, 525–529. [Google Scholar] [CrossRef]
- van der Velden, J.J.; Berger, M.Y.; Bonjer, H.J.; Brakel, K.; Laméris, J.S. Percutaneous treatment of bile duct stones in patients treated unsuccessfully with endoscopic retrograde procedures. Gastrointest. Endosc. 2000, 51, 418–422. [Google Scholar] [CrossRef]
- Jeong, E.J.; Kang, D.H.; Kim, D.U.; Choi, C.W.; Eum, J.S.; Jung, W.J.; Kim, P.J.; Kim, Y.W.; Jung, K.S.; Bae, Y.M.; et al. Percutaneous transhepatic choledochoscopic lithotomy as a rescue therapy for removal of bile duct stones in Billroth II gastrectomy patients who are difficult to perform ERCP. Eur. J. Gastroenterol. Hepatol. 2009, 21, 1358–1362. [Google Scholar] [CrossRef] [PubMed]
- Tsutsumi, K.; Kato, H.; Yabe, S.; Mizukawa, S.; Seki, H.; Akimoto, Y.; Uchida, D.; Matsumoto, K.; Tomoda, T.; Yamamoto, N.; et al. A comparative evaluation of treatment methods for bile duct stones after hepaticojejunostomy between percutaneous transhepatic cholangioscopy and peroral, short double-balloon enteroscopy. Therap. Adv. Gastroenterol. 2017, 10, 54–67. [Google Scholar] [CrossRef]
- Shimatani, M.; Matsushita, M.; Takaoka, M.; Koyabu, M.; Ikeura, T.; Kato, K.; Fukui, T.; Uchida, K.; Okazaki, K. Effective “short” double-balloon enteroscope for diagnostic and therapeutic ERCP in patients with altered gastrointestinal anatomy: A large case series. Endoscopy 2009, 41, 849–854. [Google Scholar] [CrossRef]
- Oana, S.; Shibata, S.; Matsuda, N.; Matsumoto, T. Efficacy and safety of double-balloon endoscopy-assisted endoscopic papillary large-balloon dilatation for common bile duct stone removal. Dig. Liver Dis. 2015, 47, 401–404. [Google Scholar] [CrossRef] [PubMed]
- Itoi, T.; Ishii, K.; Sofuni, A.; Itokawa, F.; Kurihara, T.; Tsuchiya, T.; Tsuji, S.; Ikeuchi, N.; Umeda, J.; Tanaka, R.; et al. Large balloon dilatation following endoscopic sphincterotomy using a balloon enteroscope for the bile duct stone extractions in patients with Roux-en-Y anastomosis. Dig. Liver Dis. 2011, 43, 237–241. [Google Scholar] [CrossRef]
- Yamauchi, H.; Kida, M.; Okuwaki, K.; Miyazawa, S.; Iwai, T.; Takezawa, M.; Kikuchi, H.; Watanabe, M.; Imaizumi, H.; Koizumi, W. Short-type single balloon enteroscope for endoscopic retrograde cholangiopancreatography with altered gastrointestinal anatomy. World J. Gastroenterol. 2013, 19, 1728–1735. [Google Scholar] [CrossRef] [PubMed]
- Osoegawa, T.; Motomura, Y.; Akahoshi, K.; Higuchi, N.; Tanaka, Y.; Hisano, T.; Itaba, S.; Gibo, J.; Yamada, M.; Kubokawa, M.; et al. Improved techniques for double-balloon-enteroscopy-assisted endoscopic retrograde cholangiopancreatography. World J. Gastroenterol. 2012, 18, 6843–6849. [Google Scholar] [CrossRef] [PubMed]
- Ishii, K.; Itoi, T.; Tonozuka, R.; Itokawa, F.; Sofuni, A.; Tsuchiya, T.; Tsuji, S.; Ikeuchi, N.; Kamada, K.; Umeda, J.; et al. Balloon enteroscopy-assisted ERCP in patients with Roux-en-Y gastrectomy and intact papillae (with videos). Gastrointest. Endosc. 2016, 83, 377–386. [Google Scholar] [CrossRef]
- Shimatani, M.; Hatanaka, H.; Kogure, H.; Tsutsumi, K.; Kawashima, H.; Hanada, K.; Matsuda, T.; Fujita, T.; Takaoka, M.; Yano, T.; et al. Diagnostic and Therapeutic Endoscopic Retrograde Cholangiography Using a Short-Type Double-Balloon Endoscope in Patients With Altered Gastrointestinal Anatomy: A Multicenter Prospective Study in Japan. Am. J. Gastroenterol. 2016, 111, 1750–1758. [Google Scholar] [CrossRef]
- Tanisaka, Y.; Ryozawa, S.; Mizuide, M.; Fujita, A.; Ogawa, T.; Harada, M.; Noguchi, T.; Suzuki, M.; Araki, R. Biliary Cannulation in Patients with Roux-en-Y Gastrectomy: An Analysis of the Factors Associated with Successful Cannulation. Intern. Med. 2020, 59, 1687–1693. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anvari, S.; Lee, Y.; Patro, N.; Soon, M.S.; Doumouras, A.G.; Hong, D. Double-balloon enteroscopy for diagnostic and therapeutic ERCP in patients with surgically altered gastrointestinal anatomy: A systematic review and meta-analysis. Surg. Endosc. 2021, 35, 18–36. [Google Scholar] [CrossRef]
- Tsutsumi, K.; Kato, H.; Okada, H. Side-to-side jejunojejunostomy is favorable for scope insertion during endoscopic retrograde cholangiopancreatography in patients with Roux-en-Y hepaticojejunostomy. Dig. Endosc. 2015, 27, 708. [Google Scholar] [CrossRef]
- Kim, G.H.; Kang, D.H.; Song, G.A.; Heo, J.; Park, C.H.; Ha, T.I.; Kim, K.Y.; Lee, H.J.; Kim, I.D.; Choi, S.H.; et al. Endoscopic removal of bile-duct stones by using a rotatable papillotome and a large-balloon dilator in patients with a Billroth II gastrectomy (with video). Gastrointest. Endosc. 2008, 67, 1134–1138. [Google Scholar] [CrossRef]
- Itoi, T.; Ishii, K.; Itokawa, F.; Kurihara, T.; Sofuni, A. Large balloon papillary dilation for removal of bile duct stones in patients who have undergone a billroth II gastrectomy. Dig. Endosc. 2010, 22, S98–S102. [Google Scholar] [CrossRef] [PubMed]
- Jang, H.W.; Lee, K.J.; Jung, M.J.; Jung, J.W.; Park, J.Y.; Park, S.W.; Song, S.Y.; Chung, J.B.; Bang, S. Endoscopic papillary large balloon dilatation alone is safe and effective for the treatment of difficult choledocholithiasis in cases of Billroth II gastrectomy: A single center experience. Dig. Dis. Sci. 2013, 58, 1737–1743. [Google Scholar] [CrossRef]
- Kim, T.H.; Kim, J.H.; Seo, D.W.; Lee, D.K.; Reddy, N.D.; Rerknimitr, R.; Ratanachu-Ek, T.; Khor, C.J.; Itoi, T.; Yasuda, I.; et al. International consensus guidelines for endoscopic papillary large-balloon dilation. Gastrointest. Endosc. 2016, 83, 37–47. [Google Scholar] [CrossRef] [Green Version]
- Itoi, T.; Ryozawa, S.; Katanuma, A.; Okabe, Y.; Kato, H.; Horaguchi, J.; Tsuchiya, T.; Gotoda, T.; Fujita, N.; Yasuda, K.; et al. Japan Gastroenterological Endoscopy Society guidelines for endoscopic papillary large balloon dilation. Dig. Endosc. 2018, 30, 293–309. [Google Scholar] [CrossRef]
- Iwashita, T.; Nakai, Y.; Hara, K.; Isayama, H.; Itoi, T.; Park, D.H. Endoscopic ultrasound-guided antegrade treatment of bile duct stone in patients with surgically altered anatomy: A multicenter retrospective cohort study. J. Hepatobiliary Pancreat Sci. 2016, 23, 227–233. [Google Scholar] [CrossRef]
- James, T.W.; Fan, Y.C.; Baron, T.H. EUS-guided hepaticoenterostomy as a portal to allow definitive antegrade treatment of benign biliary diseases in patients with surgically altered anatomy. Gastrointest. Endosc. 2018, 88, 547–554. [Google Scholar] [CrossRef]
- Hosmer, A.; Abdelfatah, M.M.; Law, R.; Baron, T.H. Endoscopic ultrasound-guided hepaticogastrostomy and antegrade clearance of biliary lithiasis in patients with surgically-altered anatomy. Endosc. Int. Open 2018, 6, E127–E130. [Google Scholar] [CrossRef] [Green Version]
- Mukai, S.; Itoi, T.; Sofuni, A.; Tsuchiya, T.; Tanaka, R.; Tonozuka, R.; Honjo, M.; Fujita, M.; Yamamoto, K.; Nagakawa, Y. EUS-guided antegrade intervention for benign biliary diseases in patients with surgically altered anatomy (with videos). Gastrointest. Endosc. 2019, 89, 399–407. [Google Scholar] [CrossRef] [PubMed]
- Cotton, P.B.; Eisen, G.M.; Aabakken, L.; Baron, T.H.; Hutter, M.M.; Jacobson, B.C.; Mergener, K.; Nemcek, A., Jr.; Petersen, B.T.; Petrini, J.L.; et al. A lexicon for endoscopic adverse events: Report of an ASGE workshop. Gastrointest. Endosc. 2010, 71, 446–454. [Google Scholar] [CrossRef]
- Testoni, P.A.; Mariani, A.; Aabakken, L.; Arvanitakis, M.; Bories, E.; Costamagna, G.; Devière, J.; Dinis-Ribeiro, M.; Dumonceau, J.M.; Giovannini, M.; et al. Papillary cannulation and sphincterotomy techniques at ERCP: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 2016, 48, 657–683. [Google Scholar] [CrossRef] [PubMed]
- Park, J.S.; Jeong, S.; Lee, D.K.; Jang, S.I.; Lee, T.H.; Park, S.H.; Hwang, J.C.; Kim, J.H.; Yoo, B.M.; Park, S.G.; et al. Comparison of endoscopic papillary large balloon dilation with or without endoscopic sphincterotomy for the treatment of large bile duct stones. Endoscopy 2019, 51, 125–132. [Google Scholar] [CrossRef]
- Kogure, H.; Kawahata, S.; Mukai, T.; Doi, S.; Iwashita, T.; Ban, T.; Ito, Y.; Kawakami, H.; Hayashi, T.; Sasahira, N.; et al. Multicenter randomized trial of endoscopic papillary large balloon dilation without sphincterotomy versus endoscopic sphincterotomy for removal of bile duct stones: MARVELOUS trial. Endoscopy 2020, 52, 736–744. [Google Scholar] [CrossRef]
- Binmoeller, K.; Brückner, M.; Thonke, F.; Soehendra, N. Treatment of difficult bile duct stones using mechanical, electrohydraulic and extracorporeal shock wave lithotripsy. Endoscopy 1993, 25, 201–206. [Google Scholar] [CrossRef]
- Veld, J.V.; van Huijgevoort, N.C.M.; Boermeester, M.A.; Besselink, M.G.; van Delden, O.M.; Fockens, P.; van Hooft, J.E. A systematic review of advanced endoscopy-assisted lithotripsy for retained biliary tract stones: Laser, electrohydraulic or extracorporeal shock wave. Endoscopy 2018, 50, 896–909. [Google Scholar] [CrossRef]
- Tonozuka, R.; Itoi, T.; Sofuni, A.; Tsuchiya, T.; Ishii, K.; Tanaka, R.; Honjo, M.; Mukai, S.; Yamamoto, K.; Fujita, M.; et al. Novel peroral direct digital cholangioscopy-assisted lithotripsy using a monorail technique through the overtube in patients with surgically altered anatomy (with video). Dig. Endosc. 2019, 31, 203–208. [Google Scholar] [CrossRef]
- Holm, A.N.; Gerke, H. What should be done with a dilated bile duct? Curr. Gastroenterol. Rep. 2010, 12, 150–156. [Google Scholar] [CrossRef]
- Li, J.S.; Zou, D.W.; Jin, Z.D.; Shi, X.G.; Chen, J.; Li, Z.S.; Liu, F. Predictive factors for extraction of common bile duct stones during endoscopic retrograde cholangiopancreatography in Billroth II anatomy patients. Surg. Endosc. 2020, 34, 2454–2459. [Google Scholar] [CrossRef]
- Lee, S.H.; Park, J.K.; Yoon, W.J.; Lee, J.K.; Ryu, J.K.; Kim, Y.T.; Yoon, Y.B. How to predict the outcome of endoscopic mechanical lithotripsy in patients with difficult bile duct stones? Scand. J. Gastroenterol. 2007, 42, 1006–1010. [Google Scholar] [CrossRef]
- Hakuta, R.; Kogure, H.; Nakai, Y.; Hamada, T.; Sato, T.; Suzuki, Y.; Inokuma, A.; Kanai, S.; Nakamura, T.; Noguchi, K.; et al. Feasibility of balloon endoscope-assisted endoscopic retrograde cholangiopancreatography for the elderly. Endosc. Int. Open 2020, 8, E1202–E1211. [Google Scholar] [CrossRef]
- Tokuhara, M.; Shimatani, M.; Mitsuyama, T.; Masuda, M.; Ito, T.; Miyamoto, S.; Fukata, N.; Miyoshi, H.; Ikeura, T.; Takaoka, M.; et al. Evaluation of complications after endoscopic retrograde cholangiopancreatography using a short type double balloon endoscope in patients with altered gastrointestinal anatomy: A single-center retrospective study of 1,576 procedures. J. Gastroenterol. Hepatol. 2020, 35, 1387–1396. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Yang, M.J.; Hwang, J.C.; Yoo, B.M. Endoscopic papillary large balloon dilation for the removal of bile duct stones. World J. Gastroenterol. 2013, 19, 8580–8594. [Google Scholar] [CrossRef]
- Bergman, J.J.; Rauws, E.A.; Tijssen, J.G.; Tytgat, G.N.; Huibregtse, K. Biliary endoprostheses in elderly patients with endoscopically irretrievable common bile duct stones: Report on 117 patients. Gastrointest. Endosc. 1995, 42, 195–201. [Google Scholar] [CrossRef]
| Patients/sessions, n | 79/90 |
| Age, years, median (IQR) | 79 (73–84) |
| Sex, male/female, n | 62/17 |
| ASA-PS, 2/3/4, n | 57/19/3 |
| Reasons for gastrectomy, n (%) | |
| Gastric cancer | 72 (91) |
| Esophageal cancer | 1 (1) |
| Malignant lymphoma | 1 (1) |
| Gastric ulcer | 2 (3) |
| Unknown | 3 (4) |
| Diameter of the largest CBD, mm, median (IQR) | 14 (11–16) |
| Size of the largest CBD stone, mm, median (IQR) | 10 (6–14) |
| Number of CBD stones, n (%) | |
| Debris | 2 (3) |
| 1 | 40 (51) |
| 2 | 15 (19) |
| ≥3 | 22 (28) |
| Reaching the papilla of Vatar, n (%) | 73 (92) | |
| Successful biliary cannulation, n (%) | 64 (81) | |
| Detection of stones by cholangiogram, n (%) | 63 (80) | |
| Overall procedure success, n (%) | 62 (78) | |
| Complete stone extraction, n (%) | 42 (53) | |
| Biliary stenting, n (%) | 20 (25) | |
| Time to reaching the papilla, min, median (IQR) | 25 (11–40) | |
| Time to biliary cannulation, min, median (IQR) | 25 (6–33) | |
| Total procedural time, min, median (IQR) | 90 (67–120) | |
| Adverse events, n (%) | 4 (5) | |
| Perforation | moderate/severe | 1/1 (3) |
| Pancreatitis | mild | 1 (1) |
| Hypoxia | mild | 1 (1) |
| Ampullary Procedure | n (%) |
| Precut alone | 4 (6) |
| EST alone | 6 (10) |
| EPBD alone | 9 (14) |
| EPLBD alone | 5 (8) |
| Precut + EPBD | 12 (19) |
| Precut + EPLBD | 5 (8) |
| EST + EPBD | 12 (19) |
| EST + EPLBD | 5 (8) |
| None | 5 (8) |
| Biliary Intervention | n(%) |
| Balloon catheter | 46 (73) |
| Basket catheter | 21 (29) |
| ML | 22 (30) |
| Plastic stent | 20 (27) |
| ENBD | 2 (3) |
| Variable | Complete Stone Extraction | Univariate | Multivariates | |||
|---|---|---|---|---|---|---|
| n | % | OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Age > 78 years old | 28/34 | 82 | 1.56 (0.47–5.12) | 0.55 | ||
| Male | 46/57 | 81 | 2.09 (0.45–9.67) | 0.39 | ||
| ASA-PS 3 or 4 | 13/16 | 81 | 1.22 (0.30–5.07) | >0.99 | ||
| Initial BE-ERCP | 40/50 | 80 | 1.33 (0.35–5.03) | 0.73 | ||
| Largest CBD diameter ≥ 14 mm | 23/36 | 64 | 0.06 (0.01–0.50) | 0.002 | 0.04 (0.003–0.58) | 0.018 |
| Retroflex position | 26/29 | 90 | 3.67 (0.92–14.69) | 0.073 | 6.43 (1.12–36.81) | 0.037 |
| Largest CBD stone size ≥ 10 mm | 27/39 | 69 | 0.18 (0.04–0.89) | 0.031 | 0.94 (0.11–8.15) | 0.96 |
| Number of CBD stones ≥ 3 | 13/19 | 68 | 0.44 (0.13–1.52) | 0.20 | ||
| EST/Precut | 36/43 | 84 | 2.25 (0.68–7.48) | 0.21 | ||
| EPBD/EPLBD | 46/59 | 78 | 0.59 (0.07–5.35) | >0.99 | ||
| Time from RYG to BE-ERCP > 4.9 years | 26/33 | 79 | 1.00 (0.31–3.26) | >0.99 | ||
| Variable | Complete Stone Extraction | Univariate | ||
|---|---|---|---|---|
| n | % | OR (95% CI) | p Value | |
| Age > 78 years old | 9/15 | 60 | 0.75 (0.19–2.97) | 0.74 |
| Male | 21/31 | 68 | 3.15 (0.45–21.95) | 0.33 |
| ASA-PS 3 or 4 | 4/7 | 57 | 0.70 (0.13–3.77) | 0.69 |
| Initial BE-ERCP | 18/27 | 67 | 1.60 (0.34–7.46) | 0.69 |
| Retroflex position | 15/18 | 83 | 6.25 (1.33–29.43) | 0.035 |
| Largest CBD stone size ≥ 10 mm | 16/28 | 57 | 0.24 (0.03–2.22) | 0.21 |
| Number of CBD stones ≥ 3 | 10/16 | 63 | 0.90 (0.23–3.52) | >0.99 |
| EST/Precut | 16/22 | 73 | 2.67 (0.65–10.88) | 0.29 |
| EPBD/EPLBD | 20/32 | 63 | 0.56 (0.05–5.97) | >0.99 |
| Time from RYG to BE-ERCP > 4.9 years | 14/21 | 67 | 1.33 (0.34–5.27) | 0.74 |
| Variable | Complete Stone Extraction | Univariate | ||
|---|---|---|---|---|
| n | % | OR (95% CI) | p Value | |
| Age > 78 years old | 14/20 | 70 | 1.08 (0.28–4.20) | >0.99 |
| Male | 24/33 | 73 | 2.67 (0.45–15.72) | 0.35 |
| ASA-PS 3 or 4 | 8/11 | 73 | 1.26 (0.27–5.93) | >0.99 |
| Initial BE-ERCP | 20/28 | 71 | 1.43 (0.33–6.26) | 0.71 |
| Largest CBD diameter ≥ 14 mm | 16/28 | 57 | N.A. | 0.017 |
| Retroflex position | 15/17 | 88 | 6.25 (1.15–34.12) | 0.037 |
| Number of CBD stones ≥ 3 | 9/15 | 60 | 0.50 (0.13–2.00) | 0.48 |
| EST/Precut | 19/25 | 76 | 2.38 (0.59–9.64) | 0.29 |
| EPBD/EPLBD | 25/36 | 69 | 1.14 (0.09–13.89) | >0.99 |
| Time from RYG to BE-ERCP > 4.9 years | 14/21 | 67 | 0.89 (0.23–3.54) | 0.74 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Obata, T.; Tsutsumi, K.; Kato, H.; Ueki, T.; Miyamoto, K.; Yamazaki, T.; Matsumi, A.; Fujii, Y.; Matsumoto, K.; Horiguchi, S.; et al. Balloon Enteroscopy-Assisted Endoscopic Retrograde Cholangiopancreatography for the Treatment of Common Bile Duct Stones in Patients with Roux-en-Y Gastrectomy: Outcomes and Factors Affecting Complete Stone Extraction. J. Clin. Med. 2021, 10, 3314. https://doi.org/10.3390/jcm10153314
Obata T, Tsutsumi K, Kato H, Ueki T, Miyamoto K, Yamazaki T, Matsumi A, Fujii Y, Matsumoto K, Horiguchi S, et al. Balloon Enteroscopy-Assisted Endoscopic Retrograde Cholangiopancreatography for the Treatment of Common Bile Duct Stones in Patients with Roux-en-Y Gastrectomy: Outcomes and Factors Affecting Complete Stone Extraction. Journal of Clinical Medicine. 2021; 10(15):3314. https://doi.org/10.3390/jcm10153314
Chicago/Turabian StyleObata, Taisuke, Koichiro Tsutsumi, Hironari Kato, Toru Ueki, Kazuya Miyamoto, Tatsuhiro Yamazaki, Akihiro Matsumi, Yuki Fujii, Kazuyuki Matsumoto, Shigeru Horiguchi, and et al. 2021. "Balloon Enteroscopy-Assisted Endoscopic Retrograde Cholangiopancreatography for the Treatment of Common Bile Duct Stones in Patients with Roux-en-Y Gastrectomy: Outcomes and Factors Affecting Complete Stone Extraction" Journal of Clinical Medicine 10, no. 15: 3314. https://doi.org/10.3390/jcm10153314
APA StyleObata, T., Tsutsumi, K., Kato, H., Ueki, T., Miyamoto, K., Yamazaki, T., Matsumi, A., Fujii, Y., Matsumoto, K., Horiguchi, S., Yasugi, K., Ogawa, T., Takenaka, R., & Okada, H. (2021). Balloon Enteroscopy-Assisted Endoscopic Retrograde Cholangiopancreatography for the Treatment of Common Bile Duct Stones in Patients with Roux-en-Y Gastrectomy: Outcomes and Factors Affecting Complete Stone Extraction. Journal of Clinical Medicine, 10(15), 3314. https://doi.org/10.3390/jcm10153314






