The Potential of Non-Invasive Biomarkers for Early Diagnosis of Asymptomatic Patients with Endometriosis
Abstract
1. Introduction
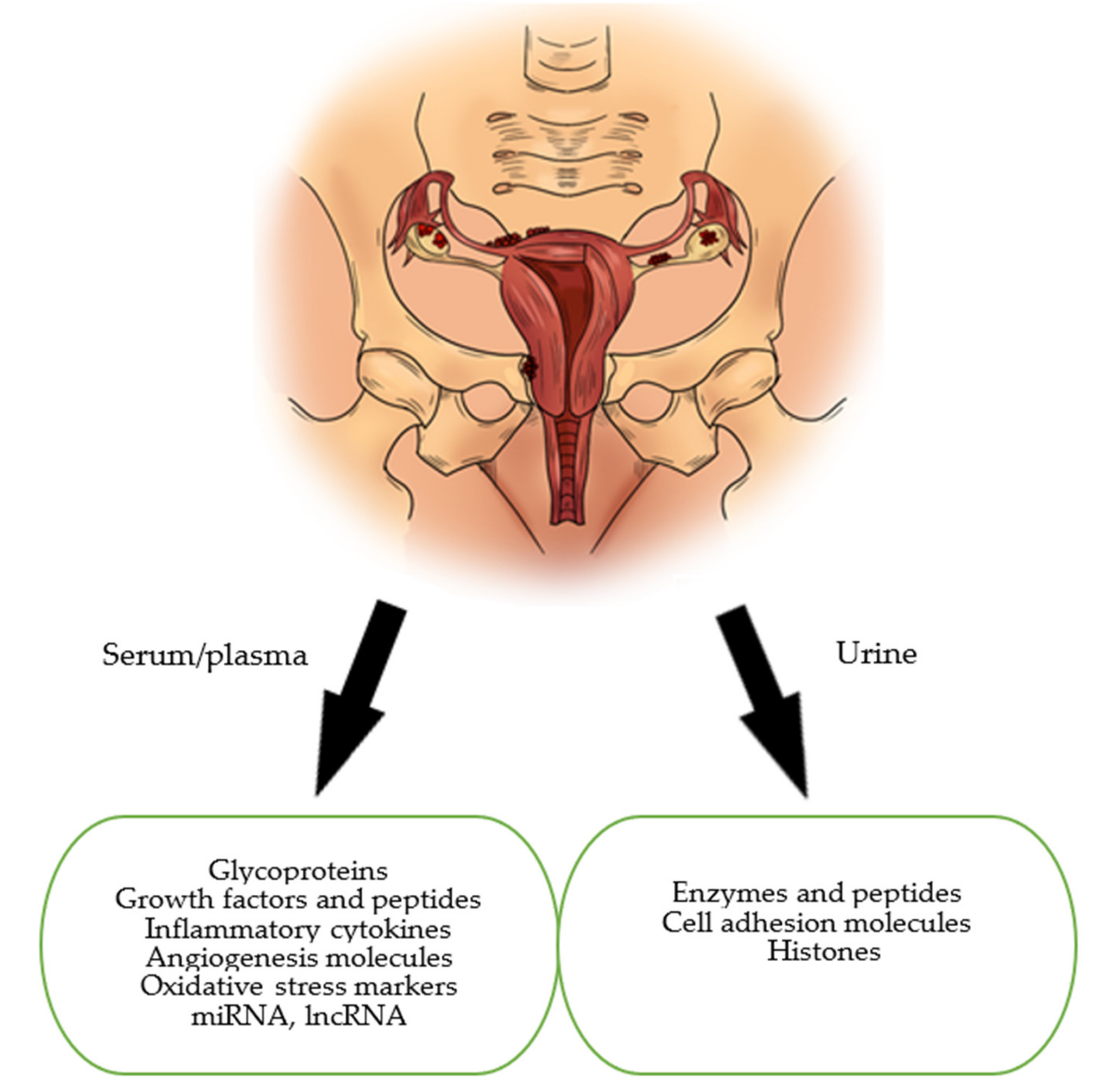
- The samples of biomarkers could be collected from serum, plasma, whole blood, tissue, urine
- Randomized clinical trials, systemic reviews, meta-analyses
- Animal, human, in vitro studies.
- Case reports, conference summaries, comments
- Insufficient data
- Not accessible as a full-text article for review
- Language other than English
- Studies conducted on non-mammalian species.
2. Glycoproteins
3. Growth Factors and Peptides: Urocortin, Activin, Follistatin
4. Immunological Markers
5. Oxidative Stress Markers
6. MiRNAs and lncRNAs
7. Urinary Biomarkers in Endometriosis
8. Perspectives
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Laganà, A.S.; Garzon, S.; Götte, M.; Viganò, P.; Franchi, M.; Ghezzi, F.; Martin, D.C. The Pathogenesis of Endometriosis: Molecular and Cell Biology Insights. Int. J. Mol. Sci. 2019, 20, 5615. [Google Scholar] [CrossRef]
- De Fáveri, C.; Fermino, P.M.P.; Piovezan, A.P.; Volpato, L.K. The Inflammatory Role of Pro-Resolving Mediators in Endometriosis: An Integrative Review. Int. J. Mol. Sci. 2021, 22, 4370. [Google Scholar] [CrossRef]
- Machairiotis, N.; Vasilakaki, S.; Thomakos, N. Inflammatory Mediators and Pain in Endometriosis: A Systematic Review. Biomedicines 2021, 9, 54. [Google Scholar] [CrossRef]
- Samimi, M.; Pourhanifeh, M.H.; Mehdizadehkashi, A.; Eftekhar, T.; Asemi, Z. The role of inflammation, oxidative stress, angiogenesis, and apoptosis in the pathophysiology of endometriosis: Basic science and new insights based on gene expression. J. Cell Physiol. 2019, 234, 19384–19392. [Google Scholar] [CrossRef] [PubMed]
- Symons, L.K.; Miller, J.E.; Kay, V.R.; Marks, R.M.; Liblik, K.; Koti, M.; Tayade, C. The Immunopathophysiology of Endometriosis. Trends Mol. Med. 2018, 24, 748–762. [Google Scholar] [CrossRef] [PubMed]
- Jiang, L.; Yan, Y.; Liu, Z.; Wang, Y. Inflammation and endometriosis. Front. Biosci. 2016, 21, 941–948. [Google Scholar]
- Koninckx, P.R.; Ussia, A.; Adamyan, L.; Wattiez, A.; Gomel, V.; Martin, D.C. Pathogenesis of endometriosis: The genetic/epigenetic theory. Fertil. Steril. 2019, 111, 327–340. [Google Scholar] [CrossRef] [PubMed]
- Gordts, S.; Koninckx, P.; Brosens, I. Pathogenesis of deep endometriosis. Fertil. Steril. 2017, 108, 872.e1–885.e1. [Google Scholar] [CrossRef] [PubMed]
- Hickey, M.; Ballard, K.; Farquhar, C. Endometriosis. BMJ 2014, 348, 29–34. [Google Scholar] [CrossRef]
- Falcone, T.; Flyckt, R. Clinical Management of Endometriosis. Obstet. Gynecol. 2018, 131, 557–571. [Google Scholar] [CrossRef]
- Basta, A.; Brucka, A.; Górski, J.; Kotarski, J.; Kulig, B.; Oszukowski, P.; Poreba, R.; Radowicki, S.; Radwan, J.; Sikora, J.; et al. The statement of Polish Society’s Experts Group concerning diagnostics and methods of endometriosis treatment. Ginekol. Pol. 2012, 83, 871–876. [Google Scholar]
- Giudice, L.C. Clinical practice. Endometriosis. N. Engl. J. Med. 2010, 362, 2389–2398. [Google Scholar] [CrossRef]
- May, K.E.; Conduit-Hulbert, S.A.; Villar, J.; Kirtley, S.; Kennedy, S.H.; Becker, C.M. Peripheral biomarkers of endometriosis: A systematic review. Hum. Reprod. Update 2010, 16, 651–674. [Google Scholar] [CrossRef] [PubMed]
- Kiesel, L.; Sourouni, M. Diagnosis of endometriosis in the 21st century. Climacteric 2019, 22, 296–302. [Google Scholar] [CrossRef]
- Bourdel, N.; Chauvet, P.; Billone, V.; Douridas, G.; Fauconnier, A.; Gerbaud, L.; Canis, M. Systematic review of quality of life measures in patients with endometriosis. PLoS ONE 2019, 14, e0208464. [Google Scholar] [CrossRef]
- Luisi, S.; Pinzauti, S.; Regini, C.; Petraglia, F. Serum markers for the noninvasive diagnosis of endometriosis. Womens Health 2015, 11, 603–610. [Google Scholar] [CrossRef]
- Coutinho, L.M.; Ferreira, M.C.; Rocha, A.L.L.; Carneiro, M.M.; Reis, F.M. New biomarkers in endometriosis. Adv. Clin. Chem. 2019, 89, 59–77. [Google Scholar]
- Fassbender, A.; Burney, R.O.; Dorien, F.O.; D’Hooghe, T.; Giudice, L. Update on Biomarkers for the Detection of Endometriosis. BioMed Res. Int. 2015, 2015, 130854. [Google Scholar] [CrossRef]
- Das, S.; Batra, S.K. Understanding the Unique Attributes of MUC16 (CA125): Potential Implications in Targeted Therapy. Cancer Res. 2015, 75, 4669–4674. [Google Scholar] [CrossRef] [PubMed]
- Bafna, S.; Kaur, S.; Batra, S.K. Membrane-bound mucins: The mechanistic basis for alterations in the growth and survival of cancer cells. Oncogene 2010, 29, 2893–2904. [Google Scholar] [CrossRef] [PubMed]
- Gipson, I.K.; Blalock, T.; Tisdale, A.; Spurr-Michaud, S.; Allcorn, S.; Stavreus-Evers, A.; Gemzell, K. MUC16 is lost from the uterodome (pinopode) surface of the receptive human endometrium: In vitro evidence that MUC16 is a barrier to trophoblast adherence. Biol. Reprod. 2008, 78, 134–142. [Google Scholar] [CrossRef]
- Haridas, D.; Ponnusamy, M.P.; Chugh, S.; Lakshmanan, I.; Seshacharyulu, P.; Batra, S.K. MUC16: Molecular analysis and its functional implications in benign and malignant conditions. FASEB J. 2014, 28, 4183–4199. [Google Scholar] [CrossRef]
- Felder, M.; Kapur, A.; Gonzalez-Bosquet, J.; Horibata, S.; Heintz, J.; Albrecht, R.; Fass, L.; Kaur, J.; Hu, K.; Shojaei, H.; et al. MUC16 (CA125): Tumor biomarker to cancer therapy, a work in progress. Mol. Cancer 2014, 13, 129. [Google Scholar] [CrossRef]
- Jacobs, I. Screening for ovarian cancer by CA-125 measurement. Lancet 1988, 1, 889. [Google Scholar] [CrossRef]
- Oliveira, M.A.P.; Raymundo, T.S.; Soares, L.C.; Pereira, T.R.D.; Demôro, A.V.E. How to Use CA-125 More Effectively in the Diagnosis of Deep Endometriosis. BioMed Res. Int. 2017, 2017, 9857196. [Google Scholar] [CrossRef] [PubMed]
- Mol, B.W.J.; Bayram, N.; Lijmer, J.G.; Wiegerinck, M.A.; Bongers, M.Y.; Van der Veen, F.; Bossuyt, P.M. The performance of CA-125 measurement in the detection of endometriosis: A meta-analysis. Fertil. Steril. 1998, 70, 1101–1108. [Google Scholar] [CrossRef]
- Karimi-Zarchi, M.; Dehshiri-Zadeh, N.; Sekhavat, L.; Nosouhi, F. Correlation of CA-125 serum level and clinico-pathological characteristic of patients with endometriosis. Int. J. Reprod. Biomed. 2016, 14, 713–718. [Google Scholar] [CrossRef] [PubMed]
- Moretuzzo, R.W.; DiLauro, S.; Jenison, E.; Chen, S.L.; Reindollar, R.H.; McDonough, P.G. Serum and peritoneal lavage fluid CA-125 levels in endometriosis. Fertil. Steril. 1994, 61, 438–442. [Google Scholar] [CrossRef]
- Franchi, M.; Beretta, P.; Zanaboni, F.; Donadello, N.; Ghezzi, F. Use of serum CA125 measurement in patients with endometriosis. Ital. J. Gynaecol. Obstet. 1993, 5, 149–153. [Google Scholar]
- Hirsch, M.; Duffy, J.M.; Deguara, C.S.; Davis, C.J.; Khan, K.S. Diagnostic accuracy of Cancer Antigen 125 (CA125) for endometriosis in symptomatic women: A multi-center study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2016, 210, 102–107. [Google Scholar] [CrossRef]
- Tian, Z.; Chang, X.H.; Zhao, Y.; Zhu, H.L. Current biomarkers for the detection of endometriosis. Chin. Med. J. 2020, 133, 2346–2352. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, M.; Duffy, J.M.N.; Davis, C.J.; Nieves Plana, M.; Khan, K.S. Diagnostic accuracy of cancer antigen 125 for endometriosis: A systematic review and meta—Analysis. BJOG 2016, 123, 1761–1768. [Google Scholar] [CrossRef] [PubMed]
- Kafali, H.; Artuc, H.; Demir, N. Use of CA-125 fluctuation during the menstrual cycle as a tool in the clinical diagnosis of endometriosis. J. Obstet. Gynecol. Reprod. Biol. 2004, 116, 85–88. [Google Scholar] [CrossRef]
- Vodolazkaia, A.; El-Aalamat, Y.; Popovic, D.; Mihalyi, A.; Bossuyt, X.; Kyama, C.M.; Fassbender, A.; Bokor, A.; Schols, D.; Huskens, D.; et al. Evaluation of a panel of 28 biomarkers for the non-invasive diagnosis of endometriosis. Hum. Reprod. 2012, 27, 2698–2711. [Google Scholar] [CrossRef] [PubMed]
- Dorien, F.O.; Fassbender, A.; Van Bree, R.; Laenen, A.; Peterse, D.P.; Vanhie, A.; Waelkens, E.; D’Hooghe, T.M. Technical Verification and Assessment of Independent Validation of Biomarker Models for Endometriosis. BioMed Res. Int. 2019, 2019, 367306. [Google Scholar]
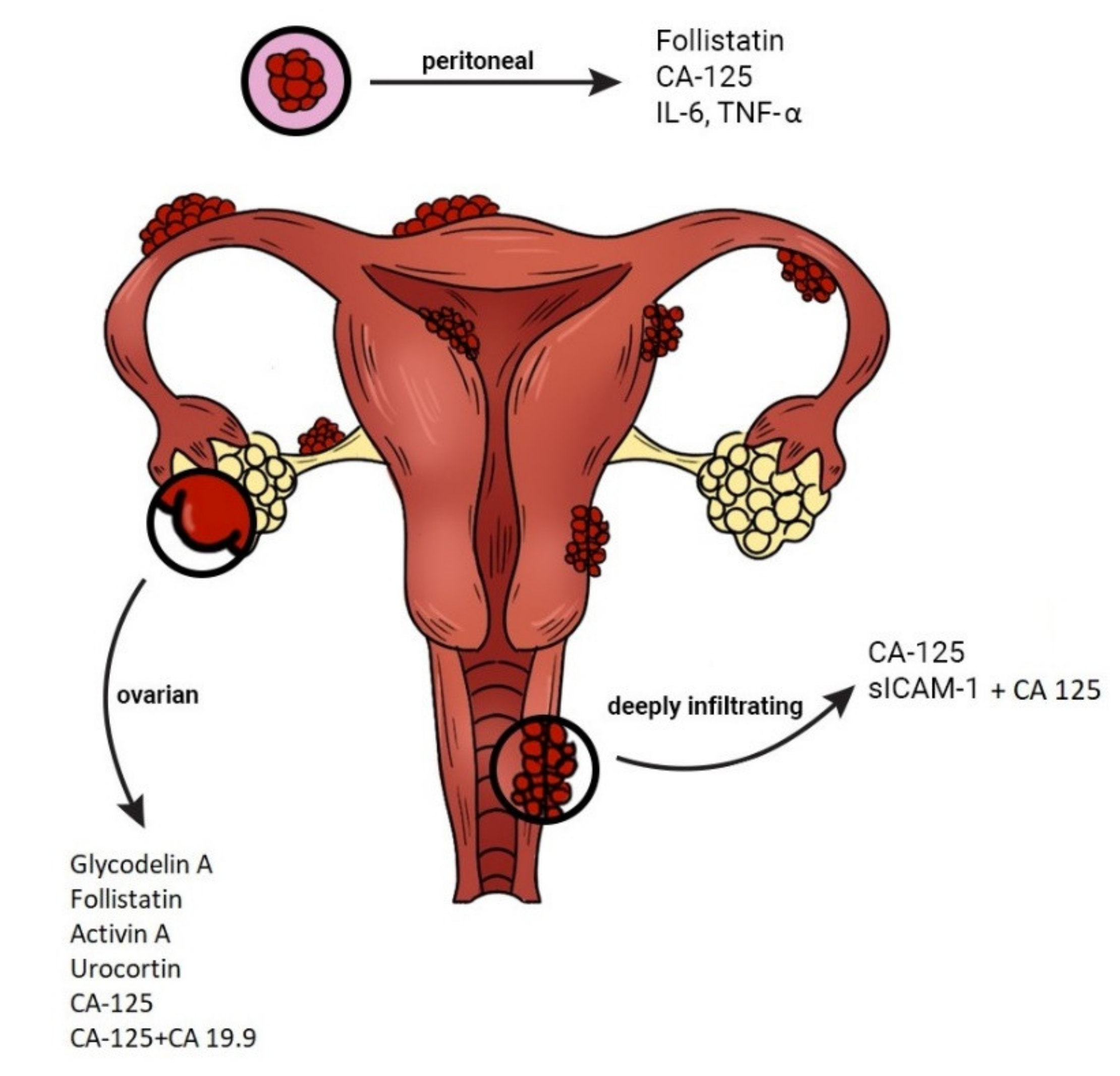
- Mihalyi, A.; Gevaert, O.; Kyama, C.M.; Simsa, P.; Pochet, N.; De Smet, F.; De Moor, B.; Meuleman, C.; Billen, J.; Blanckaert, N.; et al. Non-invasive diagnosis of endometriosis based on a combined analysis of six plasma biomarkers. Hum. Reprod. 2010, 25, 654–664. [Google Scholar] [CrossRef]
- Irungu, S.; Mavrelos, D.; Worthington, J.; Blyuss, O.; Saridogan, E.; Timms, J.F. Discovery of non-invasive biomarkers for the diagnosis of endometriosis. Clin. Proteom. 2019, 16, 14. [Google Scholar] [CrossRef]
- Somigliana, E.; Viganö, P.; Tirelli, A.S. Use of the concomitant serum dosage of CA-125, CA 19–19 and interleukin-6 to detect the presence of endometriosis. Results from a series of reproductive age women undergoing laparoscopic surgery for benign gynaecological conditions. Hum. Reprod. 2004, 19, 1871–1876. [Google Scholar] [CrossRef]
- Kurdoglu, Z.; Gursoy, R.; Kurdoglu, M.; Erdem, M.; Erdem, O.; Erdem, A. Comparison of the clinical value of CA 19-9 versus CA 125 for the diagnosis of endometriosis. Fertil. Steril. 2009, 92, 1761–1763. [Google Scholar] [CrossRef]
- Anastasiu, C.V.; Moga, M.A.; Elena Neculau, A.; Bălan, A.; Scârneciu, I.; Dragomir, R.M.; Dull, A.M.; Chicea, L.M. Biomarkers for the Noninvasive Diagnosis of Endometriosis: State of the Art and Future Perspectives. Int. J. Mol. Sci. 2020, 21, 1750. [Google Scholar] [CrossRef]
- Kocbek, V.; Vouk, K.; Mueller, M.D.; Rižner, T.L.; Bersinger, N.A. Elevated glycodelin-A concentrations in serum and peritoneal fluid of women with ovarian endometriosis. Gynecol. Endocrinol. 2013, 29, 454–459. [Google Scholar] [CrossRef]
- Mosbah, A.; Nabiel, Y.; Khashaba, E. Interleukin-6, intracellular adhesion molecule-1, and glycodelin A levels in serum and peritoneal fluid as biomarkers for endometriosis. Obstet. Gynecol. 2016, 134, 247–251. [Google Scholar] [CrossRef] [PubMed]
- Kalyani, T.; Nanda, A.; Jana, S.K. Detection of a novel glycodelin biomarker using electrochemical immunosensor for endometriosis. Anal. Chim. Acta 2021, 1146, 146–154. [Google Scholar] [CrossRef] [PubMed]
- Novembri, R.; Borges, L.E.; Carrarelli, P.; Rocha, A.L.; De Pascalis, F.; Florio, P.; Petraglia, F. Impaired CRH and urocortin expression and function in eutopic endometrium of women with endometriosis. J. Clin. Endocrinol. Metab. 2011, 96, 1145–1450. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yalcin, S.E.; Ocal, I.; Yalcin, Y.; Selim, H.S.; Caltekin, M.D.; Aydogmus, H.; Kelekci, S. Evaluation of the Ki-67 proliferation index and urocortin expression in women with ovarian endometriomas. Eurasian J. Med. 2017, 49, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Liew, H.K.; Huang, L.C.; Yang, H.I.; Peng, H.F.; Li, K.W.; Tsai, A.P.; Chen, S.Y.; Kuo, J.S.; Pang, C.Y. Therapeutic effects of human urocortin-1, -2 and -3 in intracerebral hemorrhage of rats. Neuropeptides 2015, 52, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Maia, L.M.; Rocha, A.L.; Del Puerto, H.L.; Petraglia, F.; Reis, F.M. Plasma urocortin-1 as a preoperative marker of endometriosis in symptomatisc women. Gynecol. Endocrinol. 2018, 34, 202–205. [Google Scholar] [CrossRef] [PubMed]
- Florio, P.; Reis, F.M.; Torres, P.B.; Calonaci, F.; Toti, P.; Bocchi, C.; Linton, E.A.; Petraglia, F. Plasma urocortin levels in the diagnosis of ovarian endometriosis. Obstet. Gynecol. 2007, 110, 594–600. [Google Scholar] [CrossRef]
- Chmaj-Wierzchowska, K.; Kampioni, M.; Wilczak, M.; Sajdak, S.; Opala, T. Novel markers in the diagnostics of endometriomas: Urocortin, ghrelin, and leptin or leukocytes, fibrinogen, and CA-125? Taiwan J. Obstet. Gynecol. 2015, 54, 126–130. [Google Scholar] [CrossRef] [PubMed]
- Tokmak, A.; Ugur, M.; Tonguc, E.; Var, T.; Moraloğlu, O.; Ozaksit, G. The value of urocortin and Ca-125 in the diagnosis of endometrioma. Arch. Gynecol. Obstet. 2011, 283, 1075–1079. [Google Scholar] [CrossRef]
- Rocha, A.L.; Carrarelli, P.; Novembri, R.; Sabbioni, L.; Luisi, S.; Reis, F.M.; Petraglia, F. Altered expression of activin, cripto, and follistatin in the endometrium of women with endometrioma. Fertil. Steril. 2011, 95, 2241–2246. [Google Scholar] [CrossRef] [PubMed]
- Reis, F.M.; Luisi, S.; Abrão, M.S.; Rocha, A.L.; Viganò, P.; Rezende, C.P.; Florio, P.; Petraglia, F. Diagnostic value of serum activin A and follistatin levels in women with peritoneal, ovarian and deep infiltrating endometriosis. Hum. Reprod. 2012, 27, 1445–1450. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Torres, P.B.; Florio, P.; Ferreira, M.C.; Torricelli, M.; Reis, F.M.; Petraglia, F. Deranged expression of follistatin and follistatin-like protein in women with ovarian endometriosis. Fertil. Steril. 2007, 88, 200–205. [Google Scholar] [CrossRef]
- Aznaurova, Y.B.; Zhumataev, M.B.; Roberts, T.K.; Aliper, A.M.; Zhavoronkov, A.A. Molecular aspects of development and regulation of endometriosis. Reprod. Biol. Endocrino. 2014, 12, 50. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.J.; Lai, M.D.; Lei, H.Y.; Wing, L.Y. Neutrophils and macrophages promote angiogenesis in the early stage of endometriosis in a mouse model. Endocrinology 2006, 147, 1278–1286. [Google Scholar] [CrossRef]
- Xavier, P.; Belo, L.; Beires, J.; Rebelo, I.; Martinez-de-Oliveira, J.; Lunet, N.; Barros, H. Serum levels of VEGF and TNF-alpha and their association with C-reactive protein in patients with endometriosis. Arch. Gynecol. Obstet. 2006, 273, 227–231. [Google Scholar] [CrossRef] [PubMed]
- Herrmann Lavoie, C.; Fraser, D.; Therriault, M.J.; Akoum, A. Interleukin-1 Stimulates Macrophage Migration Inhibitory Factor Secretion in Ectopic Endometrial Cells of Women with Endometriosis. Am. J. Reprod. Immunol. 2007, 58, 505–513. [Google Scholar] [CrossRef]
- Morin, M.; Bellehumeur, C.; Therriault, M.J.; Metz, C.; Maheux, R.; Akoum, A. Elevated levels of macrophage migration inhibitory factor in the peripheral blood of women with endometriosis. Fertil. Steril. 2005, 83, 865–872. [Google Scholar] [CrossRef]
- Eisenberg, V.H.; Zolti, M.; Soriano, D. Is there an association between autoimmunity and endometriosis? Autoimmun. Rev. 2012, 11, 806–814. [Google Scholar] [CrossRef]
- Itoh, H.; Sashihara, T.; Hosono, A.; Kaminogawa, S.; Uchida, M. Interleukin-12 inhibits development of ectopic endometriotic tissues in peritoneal cavity via activation of NK cells in a murine endometriosis model. Cytotechnology 2011, 63, 133–141. [Google Scholar] [CrossRef]
- Matalliotakis, I.M.; Goumenou, A.G.; Koumantakis, G.E.; Athanassakis, I.; Dionyssopoulou, E.; Neonaki, M.A.; Vassiliadis, S. Expression of Serum Human Leukocyte Antigen and Growth Factor Levels in a Greek Family With Familial Endometriosis. J. Soc. Gynecol. Investig. 2003, 3, 81–89. [Google Scholar]
- Matalliotakis, I.M.; Vassiliadis, S.; Goumenou, A.G.; Athanassakis, I.; Koumantakis, G.E.; Neonaki, M.A.; Koumantakis, E.E. Soluble ICAM-1 levels in the serum of endometriotic patients appear to be independent of medical treatment. J. Reprod. Immunol. 2001, 51, 9–19. [Google Scholar] [CrossRef]
- Kuessel, L.; Wenzl, R.; Proestling, K.; Balendran, S.; Pateisky, P.; Yotova, S.; Yerlikaya, G.; Streubel, B.; Husslein, H. Soluble VCAM-1/soluble ICAM-1 ratio is a promising biomarker for diagnosing endometriosis. Hum. Reprod. 2017, 32, 770–779. [Google Scholar] [CrossRef]
- Cho, S.; Cho, H.; Nam, A.; Kim, H.Y.; Choi, Y.S.; Park, K.H.; Cho, D.J.; Lee, B.S. Neutrophil-to-lymphocyte ratio as an adjunct to CA-125 for the diagnosis of endometriosis. Fertil. Steril. 2008, 90, 2073–2079. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, L.F.; Samadder, A.N.; Agarwal, A.; Fernandes, L.F.; Abrão, M.S. Oxidative stress biomarkers in patients with endometriosis: A systemic review. Arch. Gynecol. Obstet. 2012, 286, 1033–1040. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, M.; Davis, C.J. Preoperative assessment and diagnosis of endometriosis: Are we any closer? Curr. Opin. Obstet. Gynecol. 2015, 27, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Nisenblat, V.; Bossuyt, P.M.; Shaikh, R.; Farquhar, C.; Jordan, V.; Scheffers, C.S.; Mol, B.W.; Johnson, N.; Hull, M.L. Blood biomarkers for the non-invasive diagnosis of endometriosis. Cochrane Database Syst. Rev. 2016, 5, CD012179. [Google Scholar] [CrossRef]
- Amreen, S.; Kumar, P.; Gupta, P.; Rao, P. Evaluation of Oxidative Stress and Severity of Endometriosis. J. Hum. Reprod. Sci. 2019, 12, 40–46. [Google Scholar]
- Thézénas, M.L.; De Leo, B.; Laux-Biehlmann, A.; Bafligil, C.; Elger, B.; Tapmeier, T.; Morten, K.; Rahmioglu, N.; Dakin, S.G.; Charles, P.; et al. Amine oxidase 3 is a novel pro-inflammatory marker of oxidative stress in peritoneal endometriosis lesions. Sci. Rep. 2020, 10, 56–65. [Google Scholar]
- Wei, S.H.; Xu, H.; Kuang, Y. Systematic enrichment analysis of microRNA expression profiling studies in endometriosis. Iran J. Basic Med. Sci. 2015, 18, 423–429. [Google Scholar]
- Goulielmosa, G.N.; Matalliotakisa, M.; Matalliotaki, C.; Eliopoulos, E.; Matalliotakis, I.; Zervou, M.I. Endometriosis research in the -omics era. Gene 2020, 741, 144545. [Google Scholar] [CrossRef]
- Zhang, L.; Li, H.; Yuan, M.; Li, D.; Sun, C.; Wang, G. Serum Exosomal MicroRNAs as Potential Circulating. Dis. Markers 2020, 2456340. [Google Scholar]
- Cosar, E.; Mamillapalli, R.; Ersoy, G.S.; Cho, S.; Seifer, B.; Taylor, H.S. Serum microRNAs as diagnostic markers of endometriosis: A comprehensive array-based analysis. Fertil. Steril. 2016, 106, 402–409. [Google Scholar] [CrossRef]
- Bjorkman, S.; Taylor, H.S. microRNAs in endometriosis: Biological function and emerging biomarker candidates. Biol. Reprod. 2019, 100, 1135–1146. [Google Scholar] [CrossRef] [PubMed]
- Moustafa, S.; Burn, M.; Mamillapalli, R.; Nematian, S.; Flores, V.; Taylor, H.S. Accurate diagnosis of endometriosis using serummicroRNAs. Am. J. Obstet. Gynecol. 2020, 557, 1–11. [Google Scholar]
- Hudson, Q.J.; Perricos, A.; Wenzl, R.; Yotova, I. Challenges in uncovering non-invasive biomarkers of endometriosis. Exp. Biol. Med. 2020, 245, 437–447. [Google Scholar] [CrossRef] [PubMed]
- Moga, M.A.; Bălan, A.; Dimienescu, O.G.; Burtea, V.; Dragomir, R.M.; Anastasiu, C.V. Circulating miRNAs as Biomarkers for Endometriosis and Endometriosis-Related Ovarian Cancer—An Overview. J. Clin. Med. 2019, 8, 735. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Chen, Y.; Gao, J.; Shankar, S.; Zhang, G. Diagnostic Value of Circulating MicroRNAs for Endometriosis: A Meta-analysis. Reprod. Sci. 2020, 27, 793–805. [Google Scholar] [CrossRef]
- Ahn, S.H.; Singh, V.; Tayade, C. Biomarkers in endometriosis: Challenges and opportunities. Fertil. Steril. 2017, 107, 524–532. [Google Scholar] [CrossRef]
- Yun, B.H.; Lee, Y.S.; Chon, S.J.; Jung, Y.S.; Yim, S.Y.; Kim, H.Y.; Park, J.H.; Seo, S.K.; Cho, S.; Choi, Y.S.; et al. Evaluation of elevated urinary enolase I levels in patients with endometriosis. Biomarkers 2014, 19, 16–21. [Google Scholar] [CrossRef]
- Liu, E.; Nisenblat, V.; Farquhar, C.; Fraser, I.; Bossuyt, P.M.; Johnson, N.; Hull, M.L. Urinary biomarkers for the non-invasive diagnosis of endometriosis. Cochrane Database Syst. Rev. 2015, 12, CD012019. [Google Scholar] [CrossRef]
- Cho, S.; Choi, Y.S.; Yim, S.Y.; Yang, H.I.; Jeon, Y.E.; Lee, K.E.; Kim, H.Y.; Seo, S.K.; Lee, B.S. Urinary vitamin D-binding protein is elevated in patients with endometriosis. Hum. Reprod. 2012, 27, 515–522. [Google Scholar] [CrossRef] [PubMed]
- El-Kasti, M.M.; Wright, C.; Fye, H.K.S.; Roseman, F.; Kessler, B.M.; Becker, C.M. Urinary peptide profiling identifies a panel of putative biomarkers for diagnosing and staging endometriosis. Fertil. Steril. 2011, 95, 1261–1266. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Liu, H.Y.; Shi, H.H.; Lang, J.H.; Sun, W. Urine peptide patterns for non-invasive diagnosis of endometriosis: A preliminary prospective study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014, 177, 23–28. [Google Scholar]
- Kuessel, C.; Jaeger-Lamsky, A.; Pateisky, P.; Rossberg, N.; Schulz, A.; Schmitz, A.A.P.; Staudigl, C.; Wenzl, R. Cytokeratin-19 as a biomarker in urine and in serum for the diagnosis of endometriosis—A prospective study. Gynecol. Endocrinol. 2014, 30, 38–41. [Google Scholar] [CrossRef] [PubMed]
- Lessey, B.A.; Savaris, R.F.; Ali, S.; Brophy, S.; Tomazic-Allen, S.; Chwalisz, K. Diagnostic accuracy of urinary cytokeratin 19 fragment for endometriosis. Reprod. Sci. 2015, 22, 551–555. [Google Scholar] [CrossRef] [PubMed]
- Tokushige, N.; Markham, R.; Crossett, B.; Ahn, S.B.; Nelaturi, V.L.; Khan, A.; Fraser, I.S. Discovery of a novel biomarker in the urine in women with endometriosis. Fertil. Steril. 2011, 95, 46–49. [Google Scholar] [CrossRef]
- Proestling, K.; Wenzl, R.; Yotova, I.; Hauser, C.; Husslein, H.; Kuessel, L. Investigating selected adhesion molecules as urinary biomarkers for diagnosing endometriosis. Reprod. Biomed. Online 2020, 40, 555–558. [Google Scholar] [CrossRef]
- Chen, X.; Liu, H.; Sun, W.; Guo, Z.; Lang, J. Elevated urine histone 4 levels in women with ovarian endometriosis revealed by discovery and parallel reaction monitoring proteomics. J. Proteom. 2019, 204, 103398. [Google Scholar] [CrossRef]
- Nisenblat, V.; Prentice, L.; Bossuyt, P.M.; Farquhar, C.; Hull, M.L.; Johnson, N. Combination of the non-invasive tests for the diagnosis of endometriosis. Cochrane Database Syst. Rev. 2016, 7, CD012281. [Google Scholar] [CrossRef]
- Gupta, D.; Hull, M.L.; Fraser, I.; Miller, L.; Bossuyt, P.M.; Johnson, N.; Nisenblat, V. Endometrial biomarkers for the non-invasive diagnosis of endometriosis. Cochrane Database Syst. Rev. 2016, 4, CD012165. [Google Scholar] [CrossRef] [PubMed]
- Falcone, T.; Mascha, E. The elusive diagnostic test for endometriosis. Fertil. Steril. 2003, 80, 886–888. [Google Scholar] [CrossRef]
- Hartzes, A.M.; Morgan, C.J. Meta-analysis for diagnostic tests. J. Nucl. Cardiol. 2019, 26, 68–71. [Google Scholar] [CrossRef] [PubMed]
- Florkowski, C.M. Sensitivity, specificity, receiver-operating characteristic (ROC) curves and likelihood ratios: Communicating the performance of diagnostic tests. Clin. Biochem. Rev. 2008, 29 (Suppl. 1), S83–S87. [Google Scholar] [PubMed]
- Bedaiwy, M.A.; Falcone, T.; Sharma, R.K.; Goldberg, J.M.; Attaran, M.; Nelson, D.R.; Agarwal, A. Prediction of endometriosis with serum and peritoneal fluid markers: A prospective controlled trial. Hum. Reprod. 2002, 17, 426–431. [Google Scholar] [CrossRef] [PubMed]
| Biomarkers | Molecules | References |
|---|---|---|
| Glycoproteins | CA-125, CA 19.9, CA 15.3, CA 72, AFP, CEA, Glycodelin A | [18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44] |
| Growth factors | Urocortin, Activin A, Follistatin | [44,45,46,47,48,49,50,51,52,53] |
| Immunological markers | VEGF, TNF-α, IL-6, NK, slCAM-1, sVCAM-1, MCP-1 | [16,54,55,56,57,58,59,60,61,62,63,64] |
| Oxidative stress markers | ROS | [17,65,66,67,68,69] |
| miRNA, lncRNA | miR-134-5p, miR-197-5p, miR-22-3p, miR-320a, miR-494-3p, miR-939-5p, NR_038395, NR_038452, ENST00000482343, ENST00000544649, and ENST00000393610, TC0101441 | [40,70,71,72,73,74,75,76,77,78,79] |
| Urinary biomarkers | NNE-Cr, VDBP-Cr, CK-19, sVCAM-1, sICAM-1, E-selectin, P-selectin, Histone 4 | [80,81,82,83,84,85,86,87,88,89] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kimber-Trojnar, Ż.; Pilszyk, A.; Niebrzydowska, M.; Pilszyk, Z.; Ruszała, M.; Leszczyńska-Gorzelak, B. The Potential of Non-Invasive Biomarkers for Early Diagnosis of Asymptomatic Patients with Endometriosis. J. Clin. Med. 2021, 10, 2762. https://doi.org/10.3390/jcm10132762
Kimber-Trojnar Ż, Pilszyk A, Niebrzydowska M, Pilszyk Z, Ruszała M, Leszczyńska-Gorzelak B. The Potential of Non-Invasive Biomarkers for Early Diagnosis of Asymptomatic Patients with Endometriosis. Journal of Clinical Medicine. 2021; 10(13):2762. https://doi.org/10.3390/jcm10132762
Chicago/Turabian StyleKimber-Trojnar, Żaneta, Aleksandra Pilszyk, Magdalena Niebrzydowska, Zuzanna Pilszyk, Monika Ruszała, and Bożena Leszczyńska-Gorzelak. 2021. "The Potential of Non-Invasive Biomarkers for Early Diagnosis of Asymptomatic Patients with Endometriosis" Journal of Clinical Medicine 10, no. 13: 2762. https://doi.org/10.3390/jcm10132762
APA StyleKimber-Trojnar, Ż., Pilszyk, A., Niebrzydowska, M., Pilszyk, Z., Ruszała, M., & Leszczyńska-Gorzelak, B. (2021). The Potential of Non-Invasive Biomarkers for Early Diagnosis of Asymptomatic Patients with Endometriosis. Journal of Clinical Medicine, 10(13), 2762. https://doi.org/10.3390/jcm10132762







