Hemoglobin A1c in Patients with Diabetes Predict Long-Term Mortality Following Coronary Artery Surgery
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Measurement of HbA1c
2.3. Diabetes Mellitus Status
2.4. Study Outcomes
2.5. Post-Operative Glycemic Control
2.6. Statistical Analysis
3. Results
3.1. Population
3.2. Clinical Outcomes
Early Outcomes
3.3. Late Outcomes
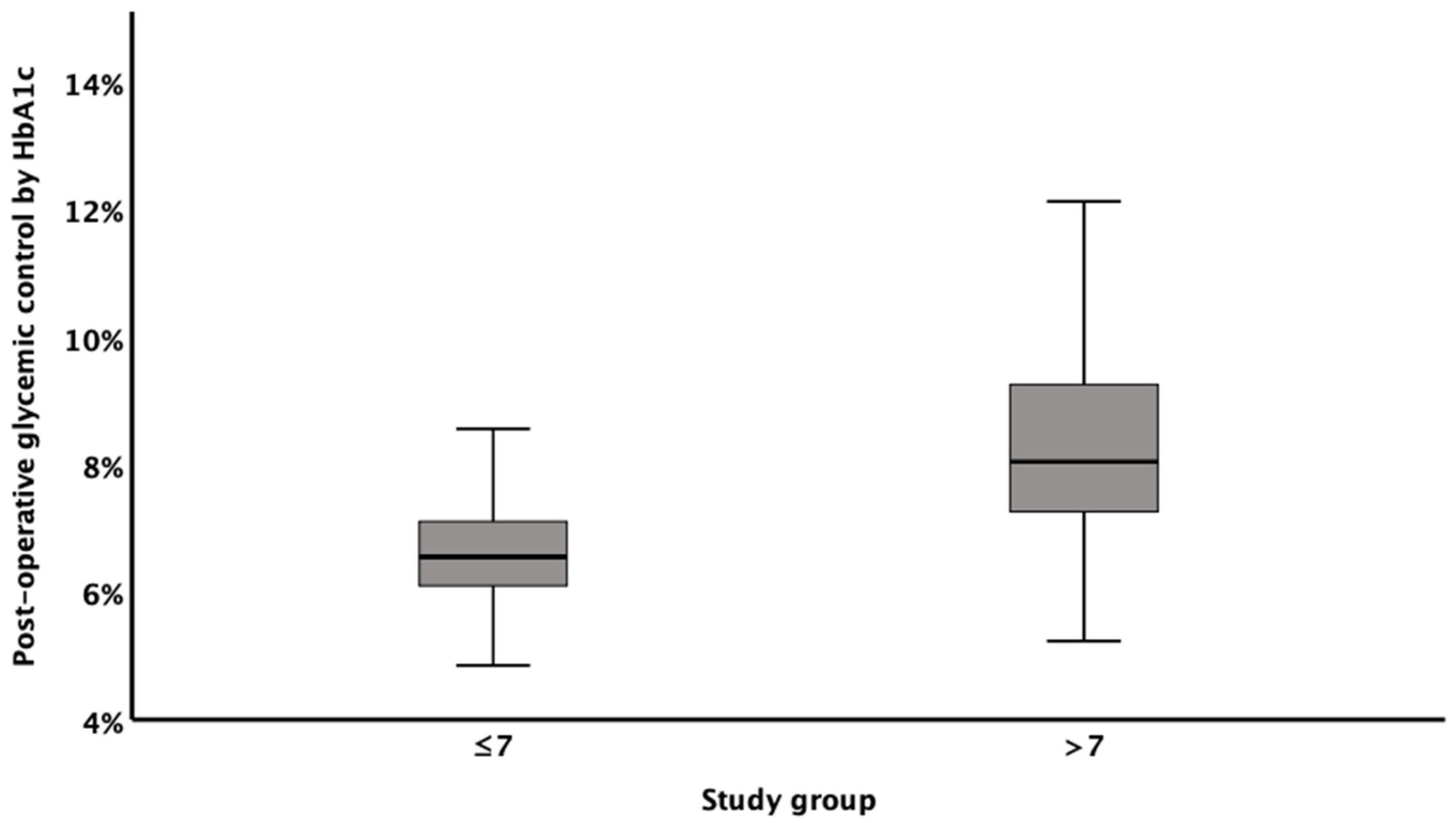
3.4. Post-Operative Glycemic Control
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jortveit, J.; Kaldal, A.; Tonstad, S. Prevalence of diabetes before and after first diagnosis of coronary artery disease. Tidsskr. Nor. Legeforening 2018, 138. [Google Scholar] [CrossRef]
- Raza, S.; Sabik, J.F.; Ainkaran, P.; Blackstone, E.H. Coronary artery bypass grafting in diabetics: A growing health care cost crisis. J. Thorac. Cardiovasc. Surg. 2015, 150, 304–312.e2. [Google Scholar] [CrossRef] [Green Version]
- Robich, M.P.; Iribarne, A.; Leavitt, B.J.; Malenka, D.J.; Quinn, R.D.; Olmstead, E.M.; Ross, C.S.; Sawyer, D.B.; Klemperer, J.D.; Clough, R.A.; et al. Intensity of Glycemic Control Affects Long-Term Survival After Coronary Artery Bypass Graft Surgery. Ann. Thorac. Surg. 2019, 107, 477–484. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grant, P.J.; Cosentino, F. The 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: New features and the ‘Ten Commandments’ of the 2019 Guidelines are discussed by Professor Peter, J. Grant and Professor Francesco Cosentino, the Task Force chairmen. Eur. Heart J. 2019, 40, 3215–3217. [Google Scholar] [PubMed]
- Fox, C.S.; Golden, S.H.; Anderson, C.; Bray, G.A.; Burke, L.E.; De Boer, I.H.; Deedwania, P.; Eckel, R.H.; Ershow, A.G.; Fradkin, J.; et al. Update on Prevention of Cardiovascular Disease in Adults With Type 2 Diabetes Mellitus in Light of Recent Evidence: A Scientific Statement From the American Heart Association and the American Diabetes Association. Circulation 2015, 132, 691–718. [Google Scholar] [CrossRef] [PubMed]
- Bartnik, M.; Rydén, L.; Malmberg, K.; Öhrvik, J.; Pyörälä, K.; Standl, E.; Ferrari, R.; Simoons, M.; Soler-Soler, J. Oral glucose tolerance test is needed for appropriate classification of glucose regulation in patients with coronary artery disease: A report from the Euro Heart Survey on Diabetes and the Heart. Heart 2007, 93, 72–77. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clement, K.C.; Suarez-Pierre, A.; Sebestyen, K.; Alejo, D.; DiNatale, J.; Whitman, G.J.; Matthew, T.L.; Lawton, J.S. Increased Glucose Variability Is Associated With Major Adverse Events After Coronary Artery Bypass. Ann. Thorac. Surg. 2019, 108, 1307–1313. [Google Scholar] [CrossRef] [PubMed]
- Tennyson, C.; Lee, R.; Attia, R. Is there a role for HbA1c in predicting mortality and morbidity outcomes after coronary artery bypass graft surgery? Interact. Cardiovasc. Thorac. Surg. 2013, 17, 1000–1008. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moridani, M.Y.; Verjee, Z.; Allen, L.C. Analytical evaluation of hemoglobin A(1c) dual kit assay on Bio-Rad Variant II: An automated HPLC hemoglobin analyzer for the management of diabetic patients. Clin. Biochem. 2003, 36, 317–320. [Google Scholar] [CrossRef]
- Carson, J.L.; Scholz, P.M.; Chen, A.Y.; Peterson, E.D.; Gold, J.; Schneider, S.H. Diabetes mellitus increases short-term mortality and morbidity in patients undergoing coronary artery bypass graft surgery. J. Am. Coll. Cardiol. 2002, 40, 418–423. [Google Scholar] [CrossRef] [Green Version]
- Halkos, M.E.; Puskas, J.D.; Lattouf, O.M.; Kilgo, P.; Kerendi, F.; Song, H.K.; Guyton, R.A.; Thourani, V.H. Elevated preoperative hemoglobin A1c level is predictive of adverse events after coronary artery bypass surgery. J. Thorac. Cardiovasc. Surg. 2008, 136, 631–640. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuhl, J.; Sartipy, U.; Eliasson, B.; Nyström, T.; Holzmann, M.J. Relationship between preoperative hemoglobin A1c levels and long-term mortality after coronary artery bypass grafting in patients with type 2 diabetes mellitus. Int. J. Cardiol. 2016, 202, 291–296. [Google Scholar] [CrossRef] [PubMed]
- Engoren, M.; Schwann, T.A.; Habib, R.H. Elevated hemoglobin A1c is associated with readmission but not complications. Asian Cardiovasc. Thorac. Ann. 2014, 22, 800–806. [Google Scholar] [CrossRef] [PubMed]
- Alserius, T.; Hammar, N.; Nordqvist, T.; Ivert, T. Risk of death or acute myocardial infarction 10 years after coronary artery bypass surgery in relation to type of diabetes. Am. Heart J. 2006, 152, 599–605. [Google Scholar] [CrossRef] [PubMed]
- Tsuruta, R.; Miyauchi, K.; Yamamoto, T.; Dohi, S.; Tambara, K.; Dohi, T.; Inaba, H.; Kuwaki, K.; Daida, H.; Amano, A. Effect of preoperative hemoglobin A1c levels on long-term outcomes for diabetic patients after off-pump coronary artery bypass grafting. J. Cardiol. 2011, 57, 181–186. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kinoshita, T.; Asai, T.; Suzuki, T.; Kambara, A.; Matsubayashi, K. Preoperative hemoglobin A1c predicts atrial fibrillation after off-pump coronary bypass surgery. Eur. J. Cardiothorac. Surg. 2012, 41, 102–107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moodahadu, L.S.; Dhall, R.; Zargar, A.H.; Bangera, S.; Ramani, L.; Katipally, R. Tight glycemic control and cardiovascular effects in type 2 diabetic patients. Heart Views Off. J. Gulf Heart Assoc. 2014, 15, 111–120. [Google Scholar] [CrossRef] [PubMed]
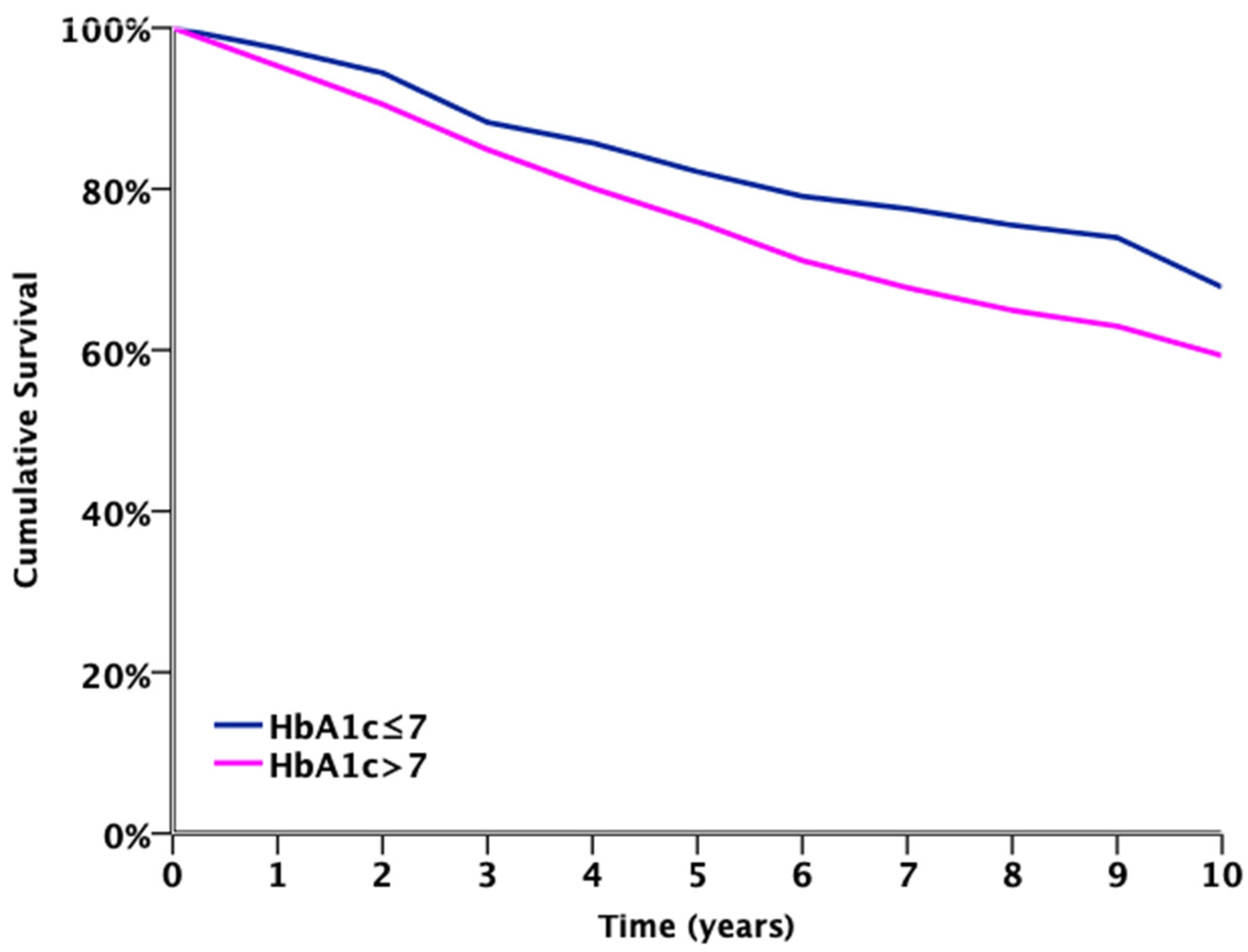
| Number Exposed to Risk | |||||||||||
| HbA1c ≤ 7 | 198 | 196 | 189 | 181 | 172 | 166 | 159 | 153 | 150 | 146 | 76 |
| HbA1c > 7 | 362 | 355 | 336 | 318 | 299 | 282 | 267 | 251 | 240 | 229 | 116 |
| Years | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| Characteristics | HbA1c ≤ 7% | HbA1c > 7% | p Value |
|---|---|---|---|
| n = 206 | n = 373 | ||
| Age Mean ± SD | 67 ± 9 | 63 ± 9 | <0.001 |
| Male | 159 (77.2) | 268 (71.2) | 0.16 |
| HTN | 144 (69.9) | 258 (69.2) | 0.85 |
| CHF | 9 (4.4) | 16 (4.3) | 0.96 |
| CRF | 11 (5.3) | 17 (4.6) | 0.67 |
| COPD | 8 (3.9) | 25 (6.7) | 0.16 |
| History of MI | 56 (27.2) | 88 (23.6) | 0.34 |
| Smoking | 63 (30.6) | 135 (36.2) | 0.17 |
| Characteristics | HbA1c ≤ 7% | HbA1c > 7% | All | p Value |
|---|---|---|---|---|
| n = 206 | n = 373 | |||
| MACCE | 15 (7.3) | 18 (4.8) | 33 (5.7) | 0.22 |
| Mortality | 8 (3.9) | 11 (2.9) | 19 (3.3) | 0.55 |
| PCI | 0 (0) | 0 (0) | 0 (0) | --- |
| Stroke | 2 (1.0) | 2 (0.5) | 4 (0.7) | 0.56 |
| AMI | 6 (2.9) | 7 (1.9) | 13 (2.2) | 0.42 |
| STEMI | 1 (0.5) | 2 (0.5) | 3 (0.5) | 0.94 |
| NSTEMI | 6 (2.9) | 6 (1.6) | 12 (2.1) | 0.29 |
| Atrial fibrillation | 36 (17.5) | 38 (10.2) | 74 (12.8) | 0.01 |
| Wound infections | 11 (5.3) | 30 (8.0) | 41 (7.1) | 0.23 |
| Acute renal failure | 28 (13.6) | 41 (11.0) | 69 (11.9) | 0.35 |
| Cardiogenic shock | 1 (0.5) | 5 (1.3) | 6 (1.0) | 0.33 |
| Re-surgery due to post-operative bleeding | 7 (3.4) | 11 (2.9) | 18 (3.1) | 0.76 |
| Pneumonia | 4 (1.9) | 10 (2.7) | 14 (2.4) | 0.58 |
| ACS | 7 (3.4) | 8 (2.1) | 15 (2.6) | 0.36 |
| Median length of stay (IQR) | 6 (4; 8) | 6 (4; 8) | 6 (4; 8) | 0.58 |
| Characteristics | HbA1c ≤ 7% | HbA1c > 7% | All | p Value |
|---|---|---|---|---|
| n = 206 | n = 373 | |||
| MACCE | 71 (34.5) | 155 (41.6) | 226 (39.0) | 0.04 |
| Mortality | 42 (20.4) | 107 (28.7) | 149 (25.7) | 0.01 |
| AMI | 26 (12.6) | 46 (12.3) | 72 (12.4) | 0.76 |
| -STEMI ^ | 2 (1.0) | 3 (0.8) | 5 (0.9) | 0.09 |
| -NSTEMI ^ | 25 (12.1) | 44 (11.8) | 69 (11.9) | 0.78 |
| PCI | 24 (11.7) | 40 (10.7) | 64 (11.1) | 0.97 |
| Stroke | 10 (4.9) | 29 (7.8) | 39 (6.7) | 0.13 |
| CHF hospitalization | 4 (1.9) | 6 (1.6) | 10 (1.7) | 0.89 |
| Glycemic control by HbA1c% Median (IQR) | 6.5 (6.1; 7.1) | 8.1 (7.3; 9.2) | 7.5 (6.6; 8.5) | <0.001 |
| Characteristics | Hazard Ratio | p Value | 95% Confidence Interval | |
|---|---|---|---|---|
| Lower | Upper | |||
| Age (Years) | 1.04 | 0.01 | 1.01 | 1.06 |
| Old MI | 1.87 | 0.01 | 1.19 | 2.92 |
| History of CHF | 2.20 | 0.06 | 0.96 | 4.93 |
| CRF | 4.49 | <0.001 | 2.11 | 9.54 |
| COPD | 2.60 | 0.01 | 1.28 | 5.28 |
| HbA1c > 7% | 2.67 | 0.001 | 1.52 | 4.68 |
| Glycemic control | 1.003 | 0.97 | 0.86 | 1.18 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abu Tailakh, M.; Ishay, S.-y.; Awesat, J.; Poupko, L.; Sahar, G.; Novack, V. Hemoglobin A1c in Patients with Diabetes Predict Long-Term Mortality Following Coronary Artery Surgery. J. Clin. Med. 2021, 10, 2739. https://doi.org/10.3390/jcm10122739
Abu Tailakh M, Ishay S-y, Awesat J, Poupko L, Sahar G, Novack V. Hemoglobin A1c in Patients with Diabetes Predict Long-Term Mortality Following Coronary Artery Surgery. Journal of Clinical Medicine. 2021; 10(12):2739. https://doi.org/10.3390/jcm10122739
Chicago/Turabian StyleAbu Tailakh, Muhammad, Shlomo-yaron Ishay, Jenan Awesat, Liat Poupko, Gidon Sahar, and Victor Novack. 2021. "Hemoglobin A1c in Patients with Diabetes Predict Long-Term Mortality Following Coronary Artery Surgery" Journal of Clinical Medicine 10, no. 12: 2739. https://doi.org/10.3390/jcm10122739
APA StyleAbu Tailakh, M., Ishay, S.-y., Awesat, J., Poupko, L., Sahar, G., & Novack, V. (2021). Hemoglobin A1c in Patients with Diabetes Predict Long-Term Mortality Following Coronary Artery Surgery. Journal of Clinical Medicine, 10(12), 2739. https://doi.org/10.3390/jcm10122739






