Direct and Indirect Impact of COVID-19 for Patients with Immune-Mediated Inflammatory Diseases: A Retrospective Cohort Study
Abstract
1. Introduction
2. Methods
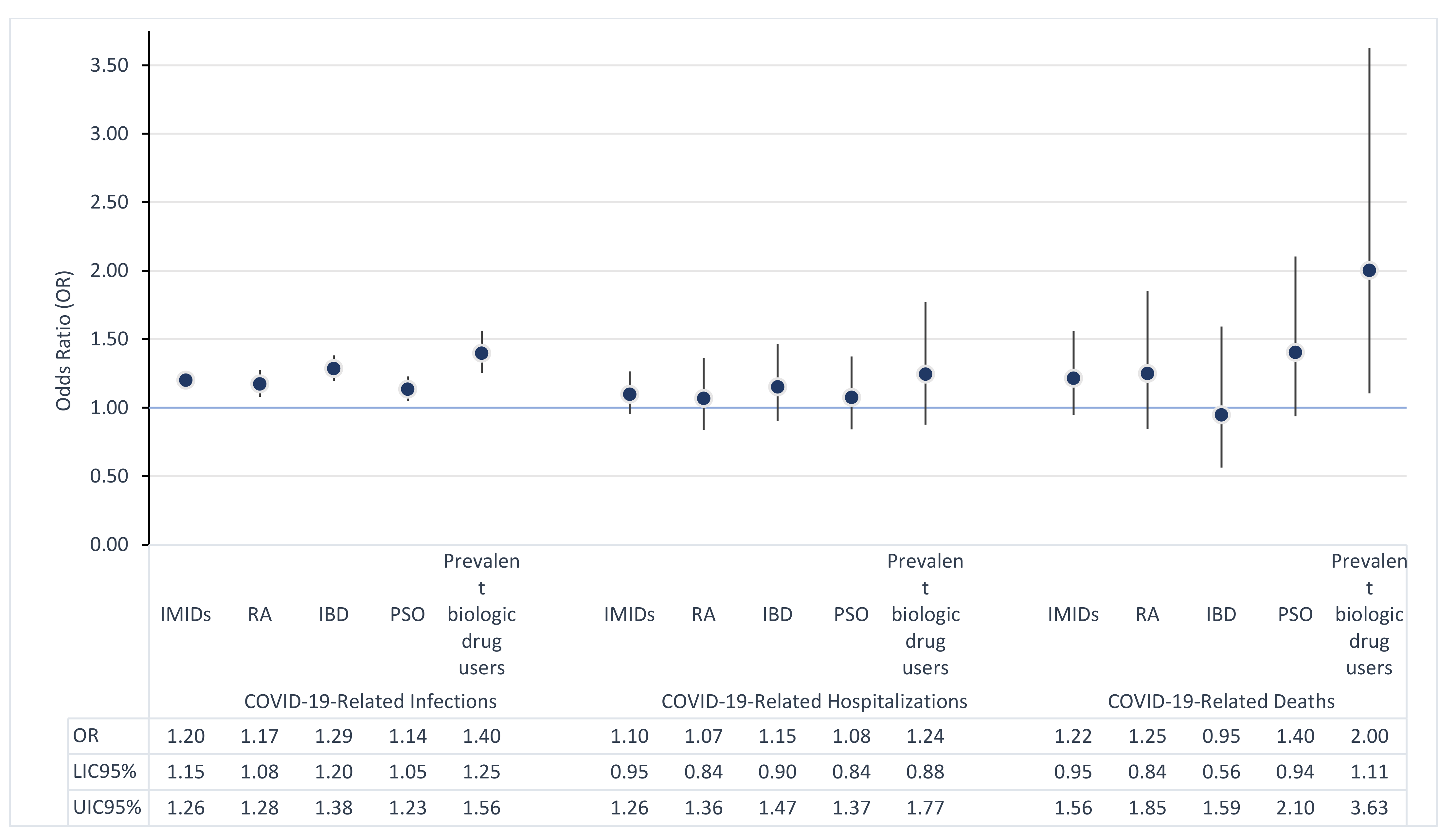
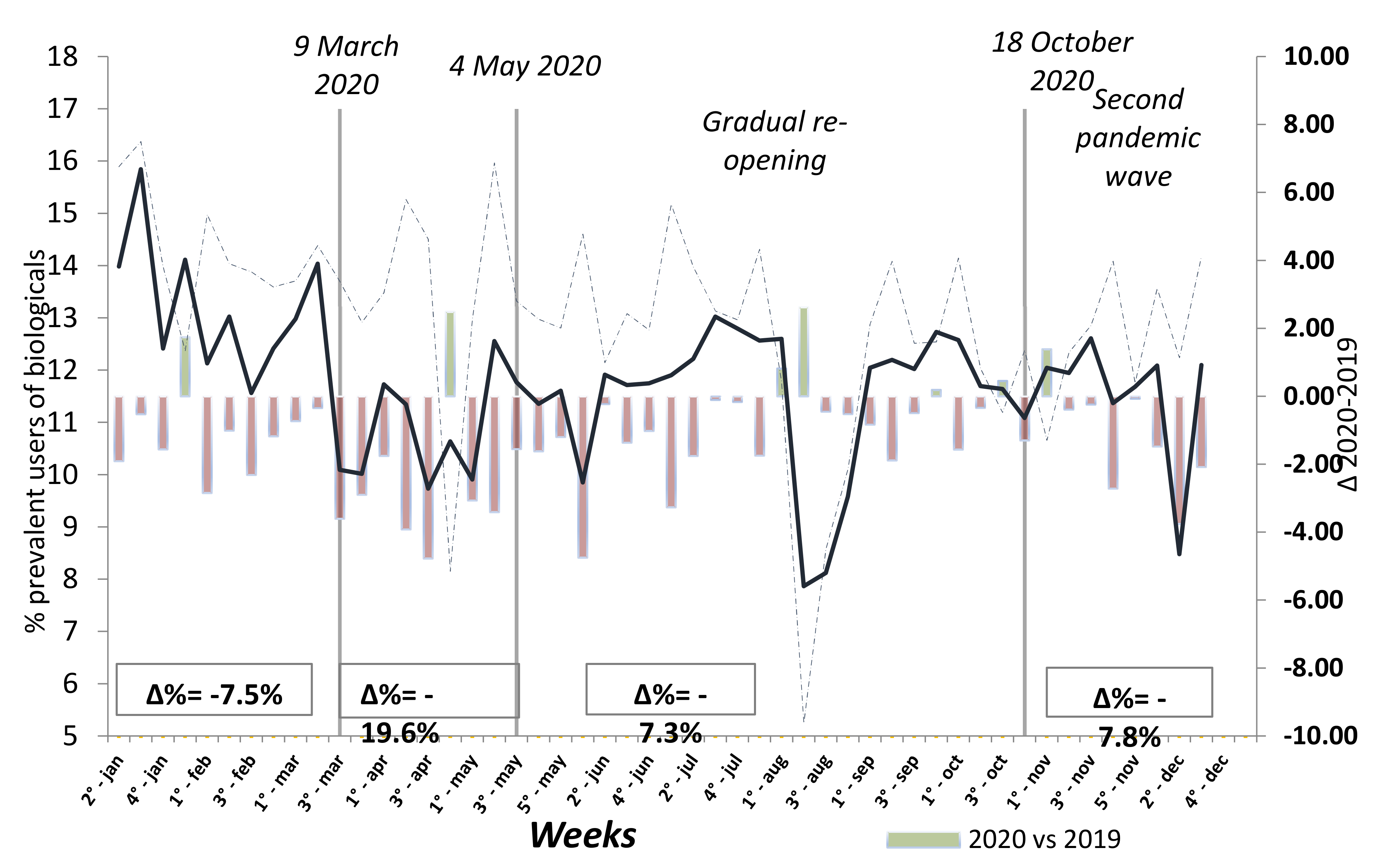
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Akiyama, S.; Hamdeh, S.; Micic, D.; Sakuraba, A. Prevalence and clinical outcomes of COVID-19 in patients with autoimmune diseases: A systematic review and meta-analysis. Ann. Rheum. Dis. 2020. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.; Yi, Z.; Cai, R.; Chen, R.; Thong, B.Y.; Mu, R. Clinical outcomes of COVID-19 in patients with rheumatic diseases: A systematic review and meta-analysis of global data. Autoimmun. Rev. 2021, 20, 102778. [Google Scholar] [CrossRef] [PubMed]
- Ministero della Salute; Presidenza del Consiglio dei Ministri; Istituto Superiore di Sanità; Agenzia Nazionale per i Servizi Sanitari Regionali; Agenzia Italiana del Farmaco. Vaccinazione anti-SARS-CoV-2/COVID-19. Piano Strategico. Available online: http://www.salute.gov.it/imgs/C_17 (accessed on 1 April 2021).
- Department of Health and Social Care. UK COVID-19 Vaccines Delivery Plan. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/951928/uk-covid-19-vaccines-delivery-plan-final.pdf (accessed on 1 April 2021).
- The Centers for Disease Control and Prevention. The COVID-19 Vaccination Program Interim Operational Guidance for Jurisdictions Playbook. Available online: https://www.cdc.gov/vaccines/imz-managers/downloads/COVID-19-Vaccination-ProgramInterim_Playbook.pdf (accessed on 1 April 2021).
- European Centre for Disease Prevention and Control. Overview of COVID-19 Vaccination Strategies and Vaccine Deployment Plans in the EU/EEA and the UK. Available online: https://www.ecdc.europa.eu/en/publications-data/overview-implementation-covid-19-vaccination-strategies-and-vaccine-deployment (accessed on 1 April 2021).
- Diamanti, A.P.; Cattaruzza, M.S.; Di Rosa, R.; Del Porto, F.; Salemi, S.; Sorgi, M.L.; Martin, L.S.M.; Rai, A.; Iacono, D.; Sesti, G.; et al. Psychological Distress in Patients with Autoimmune Arthritis during the COVID-19 Induced Lockdown in Italy. Microorganisms 2020, 8, 1818. [Google Scholar] [CrossRef] [PubMed]
- Quan, H.; Sundararajan, V.; Halfon, P.; Fong, A.; Burnand, B.; Luthi, J.C.; Saunders, L.D.; Beck, C.A.; Feasby, T.E.; Ghali, W.A. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med. Care 2005, 43, 1130–1139. [Google Scholar] [CrossRef] [PubMed]
- Strangfeld, A.; Schäfer, M.; Gianfrancesco, M.A.; Lawson-Tovey, S.; Liew, J.W.; Ljung, L.; Mateus, E.F.; Richez, C.; Santos, M.J.; Schmajuk, G.; et al. Factors associated with COVID-19-related death in people with rheumatic diseases: Results from the COVID-19 Global Rheumatology Alliance physician-reported registry. Ann. Rheum. Dis. 2021. [Google Scholar] [CrossRef] [PubMed]
- Attauabi, M.; Seidelin, J.B.; Felding, O.K.; Wewer, M.D.; Arp, L.K.V.; Sarikaya, M.Z.; Egeberg, A.; Vladimirova, N.; Bendtsen, F.; Burisch, J. Coronavirus disease 2019, immune-mediated inflammatory diseases and immunosuppressive therapies—A Danish population-based cohort study. J. Autoimmun. 2021, 118, 102613. [Google Scholar] [CrossRef] [PubMed]
- Bower, H.; Frisell, T.; Di Giuseppe, D.; Delcoigne, B.; Ahlenius, G.-M.; Baecklund, E.; Chatzidionysiou, K.; Feltelius, N.; Forsblad-D’Elia, H.; Kastbom, A.; et al. Impact of the COVID-19 pandemic on morbidity and mortality in patients with inflammatory joint diseases and in the general population: A nationwide Swedish cohort study. Ann. Rheum. Dis. 2021. [Google Scholar] [CrossRef]
- Hasseli, R.; Mueller-Ladner, U.; Hoyer, B.F.; Krause, A.; Lorenz, H.-M.; Pfeil, A.; Richter, J.; Schäfer, M.; Schmeiser, T.; Strangfeld, A.; et al. Older age, comorbidity, glucocorticoid use and disease activity are risk factors for COVID-19 hospitalisation in patients with inflammatory rheumatic and musculoskeletal diseases. RMD Open 2021, 7, e001464. [Google Scholar] [CrossRef] [PubMed]
- Landewé, R.B.; Machado, P.M.; Kroon, F.; Bijlsma, H.W.; Burmester, G.R.; Carmona, L.; Combe, B.; Galli, M.; Gossec, L.; Iagnocco, A.; et al. EULAR provisional recommendations for the management of rheumatic and musculoskeletal diseases in the context of SARS-CoV-2. Ann. Rheum. Dis. 2020, 79, 851–858. [Google Scholar] [CrossRef] [PubMed]
- Mikuls, T.R.; Johnson, S.R.; Fraenkel, L.; Arasaratnam, R.J.; Baden, L.R.; Bermas, B.L.; Chatham, W.; Cohen, S.; Costenbader, K.; Gravallese, E.M.; et al. American College of Rheumatology Guidance for the Management of Rheumatic Disease in Adult Patients During the COVID-19 Pandemic: Version 3. Arthritis Rheumatol. 2021, 73, e1–e12. [Google Scholar] [CrossRef] [PubMed]
- Mahil, S.K.; Dand, N.; Mason, K.J.; Yiu, Z.Z.; Tsakok, T.; Meynell, F.; Coker, B.; McAteer, H.; Moorhead, L.; MacKenzie, T.; et al. Factors associated with adverse COVID-19 outcomes in patients with psoriasis-insights from a global registry-based study. J. Allergy Clin. Immunol. 2021, 147, 60–71. [Google Scholar] [CrossRef] [PubMed]
- Hyrich, K.L.; Machado, P.M. Rheumatic disease and COVID-19: Epidemiology and outcomes. Nat. Rev. Rheumatol. 2021, 17, 71–72. [Google Scholar] [CrossRef] [PubMed]
- Venerito, V.; Lopalco, G.; Iannone, F. COVID-19, rheumatic diseases and immunosuppressive drugs: An appeal for medication adherence. Rheumatol. Int. 2020, 40, 827–828. [Google Scholar] [CrossRef] [PubMed]
- Minozzi, S.; Bonovas, S.; Lytras, T.; Pecoraro, V.; González-Lorenzo, M.; Bastiampillai, A.J.; Gabrielli, E.M.; Lonati, A.C.; Moja, L.; Cinquini, M.; et al. Risk of infections using anti-TNF agents in rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis: A systematic review and meta-analysis. Expert Opin. Drug Saf. 2016, 15 (Suppl. 1), 11–34. [Google Scholar] [CrossRef] [PubMed]
| IMIDs | RA | IBD | PSO | Prevalent Biologic Drug Users | General Population | |
|---|---|---|---|---|---|---|
| 65,230 | 20,299 | 22,525 | 22,406 | 9176 | 4,702,567 | |
| Sex | ||||||
| Male | 42.4% | 25.2% | 52% | 47.8% | 42.9% | 47.3% |
| Age (years) | ||||||
| <50 | 29.9% | 20.5% | 41.3% | 26.9% | 35.3% | 46.0% |
| 50–60 | 21.3% | 18.6% | 22.1% | 22.9% | 25.4% | 19.3% |
| 60–70 | 21.5% | 23.5% | 17.4% | 23.9% | 23.2% | 14.5% |
| 70–80 | 17.2% | 22.0% | 12.4% | 17.8% | 13.2% | 11.6% |
| >=80 | 10.1% | 15.4% | 6.9% | 8.5% | 3.0% | 8.5% |
| Median [IQR] | 59 (47–71) | 64 (52–75) | 53 (42–66) | 60 (49–70) | 56 (44–65) | 51 (38–66) |
| Charlson comorbidity index | ||||||
| 0 | 80.7% | 69.3% | 87.7% | 84.1% | 83.1% | 92.4% |
| 1–2 | 14.4% | 23.5% | 9.1% | 11.6% | 14.8% | 5.8% |
| 3+ | 4.8% | 7.3% | 3.1% | 4.3% | 2.1% | 1.8% |
| Covid-19 cumulative incidence during 2020 (per 10,000 inhabitants) | 304 | 286 | 337 | 286 | 360 | 266 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Belleudi, V.; Rosa, A.C.; Poggi, F.R.; Armuzzi, A.; Nicastri, E.; Goletti, D.; Diamanti, A.P.; Davoli, M.; Agabiti, N.; Addis, A. Direct and Indirect Impact of COVID-19 for Patients with Immune-Mediated Inflammatory Diseases: A Retrospective Cohort Study. J. Clin. Med. 2021, 10, 2388. https://doi.org/10.3390/jcm10112388
Belleudi V, Rosa AC, Poggi FR, Armuzzi A, Nicastri E, Goletti D, Diamanti AP, Davoli M, Agabiti N, Addis A. Direct and Indirect Impact of COVID-19 for Patients with Immune-Mediated Inflammatory Diseases: A Retrospective Cohort Study. Journal of Clinical Medicine. 2021; 10(11):2388. https://doi.org/10.3390/jcm10112388
Chicago/Turabian StyleBelleudi, Valeria, Alessandro C. Rosa, Francesca R. Poggi, Alessandro Armuzzi, Emanuele Nicastri, Delia Goletti, Andrea Picchianti Diamanti, Marina Davoli, Nera Agabiti, and Antonio Addis. 2021. "Direct and Indirect Impact of COVID-19 for Patients with Immune-Mediated Inflammatory Diseases: A Retrospective Cohort Study" Journal of Clinical Medicine 10, no. 11: 2388. https://doi.org/10.3390/jcm10112388
APA StyleBelleudi, V., Rosa, A. C., Poggi, F. R., Armuzzi, A., Nicastri, E., Goletti, D., Diamanti, A. P., Davoli, M., Agabiti, N., & Addis, A. (2021). Direct and Indirect Impact of COVID-19 for Patients with Immune-Mediated Inflammatory Diseases: A Retrospective Cohort Study. Journal of Clinical Medicine, 10(11), 2388. https://doi.org/10.3390/jcm10112388







