Cardiac Rehabilitation and Physical Performance in Patients after Myocardial Infarction: Preliminary Research
Abstract
1. Introduction
2. Materials and Methods
- test time [min];
- metabolic equivalent of task (MET);
- systolic blood pressure: resting (RR sys. rest.) and maximum (RR sys. max) (measured at the time of maximum workload, at the peak of physical exercise) [mmHg];
- diastolic blood pressure: resting (RR diast. rest.) and maximum (RR diast. max) [mmHg];
- heart rate (HR): resting (HR rest.) and maximum (HR max) [beats/min];
- HR one minute after physical exertion.
3. Results
3.1. Study Group Characteristics
3.2. Cardiac Rehabilitation in the 3rd Month after MI
3.3. Cardiac Rehabilitation in the 6th Month after MI
3.4. Impact of Selected Parameters on the Change: 6MWT, the Exercise Stress Test, MET Test and VO2max (After the Cardiac Rehabilitation in the 6th Month)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Johansson, S.; Rosengren, A.; Young, K.; Jennings, E. Mortality and morbidity trends after the first year in survivors of acute myocardial infarction: A systematic review. BMC Cardiovasc. Disord. 2017, 17, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Boudreau, M.; Genovese, J. Cardiac Rehabilitation: A Comprehensive Program for the Management of Heart Failure. Prog. Cardiovasc. Nurs. 2007, 22, 88–92. [Google Scholar] [CrossRef] [PubMed]
- De Schutter, A.; Kachur, S.; Lavie, C.J.; Menezes, A.; Shum, K.K.; Bangalore, S.; Arena, R.; Milani, R.V. Cardiac rehabilitation fitness changes and subsequent survival. Eur. Hear. J. Qual. Care Clin. Outcomes 2018, 1, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Piepoli, M.F.; Corra, U.; Adamopoulos, S.; Benzer, W.; Bjarnason-Wehrens, B.; Cupples, M.; Dendale, P.; Doherty, P.; Gaita, D.; Höfer, S.; et al. Core components, standards and outcome measures for referral and delivery: A policy statement from the cardiac rehabilitation section of the European Asso-ciation for Cardiovascular Prevention & Rehabilitation. Endorsed by the Committee for Practice Guidelines of the European Society of Cardiology. Eur. J. Prev. Cardiol. 2014, 21, 664–681. [Google Scholar]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.T.; Corrà, U.; Cosyns, B.; Deaton, C.; et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiol-ogy and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 socie-ties and by invited experts)Developed with the special contribution of the European Association for Cardiovascular Preven-tion & Rehabilitation (EACPR). Eur. Heart J. 2016, 37, 2315–2381. [Google Scholar]
- Anderson, L.; Thompson, D.R.; Oldridge, N.; Zwisler, A.-D.; Rees, K.; Martin, N.; Taylor, R.S. Exercise-Based Cardiac Reha-bilitation for Coronary Heart Disease: Cochrane Systematic Review and Meta-Analysis. J. Am. Coll. Cardiol. 2016, 67, 1–12. [Google Scholar] [CrossRef]
- Fornitano, L.D.; Godoy, M.F. Duplo produto elevado corno preditor de ausência de coronariopatia obstrutiva de grau im-portante em pacientes com teste ergométrico positivo [Increased rate-pressure product as predictor for the absence of signifi-cant obstructive coronary artery disease in patients with positive exercise test]. Arq. Bras. Cardiol. 2006, 86, 138–144. [Google Scholar] [CrossRef]
- Lawler, P.R.; Filion, K.B.; Eisenberg, M.J. Efficacy of exercise-based cardiac rehabilitation post-myocardial infarction: A systematic review and meta-analysis of randomized controlled trials. Am. Heart J. 2011, 162, 571–584.e2. [Google Scholar] [CrossRef]
- Fletcher, G.F.; Landolfo, C.; Niebauer, J.; Ozemek, C.; Arena, R.; Lavie, C.J. Promoting Physical Activity and Exercise. J. Am. Coll. Cardiol. 2018, 72, 1622–1639. [Google Scholar] [CrossRef]
- Jolliffe, J.A.; Rees, K.; Taylor, R.S.; Thompson, D.; Oldridge, N.; Ebrahim, S. Exercise-based rehabilitation for coronary heart disease. Cochrane Database Syst. Rev. 2001, 1, CD001800. [Google Scholar] [CrossRef]
- Sendercock, G.R.; Hodges, L.D.; Das, S.K.; Brodie, D.A. The impact of short term supervised and home-based walking pro-grammes on heart rate variability in patients with peripheral arterial disease. J. Sports Sci. Med. 2007, 6, 471–476. [Google Scholar]
- Cwikiel, J.; Seljeflot, I.; Fagerland, M.W.; Wachtell, K.; Arnesen, H.; Berge, E.; Flaa, A. High-sensitive cardiac Troponin T and exercise stress test for evaluation of angiographically significant coronary disease. Int. J. Cardiol. 2019, 287, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Lu, H.; Pan, S.; Lin, Y.; Zhou, K.; Wang, L. 6MWT Performance and its Correlations with VO2 and Handgrip Strength in Home-Dwelling Mid-Aged and Older Chinese. Int. J. Environ. Res. Public Health 2017, 14, 473. [Google Scholar] [CrossRef] [PubMed]
- Polish Society of Cardiology “Recommendations for Comprehensive Cardiological Rehabilitation”; AsteriaMed: Gdańsk, Poland, 2017.
- Bjarnason-Wehrens, B.; McGee, H.; Zwisler, A.-D.; Piepoli, M.F.; Benzer, W.; Schmid, J.-P.; Dendale, P.; Pogosova, G.-N.; Zdrenghea, D.; Niebauer, J.; et al. Cardiac rehabilitation in Europe: Results from the European Cardiac Rehabilitation Inventory Survey. Eur. J. Cardiovasc. Prev. Rehabil. 2010, 17, 410–418. [Google Scholar] [CrossRef] [PubMed]
- Vilela, E.M.; Ladeiras-Lopes, R.; Ruivo, C.; Torres, S.; Braga, J.; Fonseca, M.; Ribeiro, J.; Primo, J.; Fontes-Carvalho, R.; Campos, L.; et al. Different outcomes of a cardiac rehabilitation programme in functional parameters among myocardial infarction survivors according to ejection fraction. Neth. Hear. J. 2019, 27, 347–353. [Google Scholar] [CrossRef]
- Foster, C.; Jackson, A.S.; Pollock, M.L.; Taylor, M.M.; Hare, J.; Sennett, S.M.; Rod, J.L.; Sarwar, M.; Schmidt, D.H. Generalized equations for predicting functional capacity from treadmill performance. Am. Heart J. 1984, 107, 1229–1234. [Google Scholar] [CrossRef]
- Giga, V.; Ostojic, M.; Vujisic-Tesic, B.; Djordjevic-Dikic, A.; Stepanovic, J.; Beleslin, B.; Petrovic, M.; Nedeljkovic, M.; Nedeljkovic, I.; Milic, N. Exercise-induced changes in mitral regurgitation in patients with prior myocardial infarction and left ventricular dysfunction: Relation to mitral deformation and left ventricular function and shape. Eur. Hear. J. 2005, 26, 1860–1865. [Google Scholar] [CrossRef] [PubMed]
- ATS Statement Guidelines for the Six-Minute Walk Test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [CrossRef]
- Glowinski, S.; Łosiński, K.; Kowiański, P.; Waśkow, M.; Bryndal, A.; Grochulska, A. Inertial Sensors as a Tool for Diagnosing Discopathy Lumbosacral Pathologic Gait: A Preliminary Research. Diagnostics 2020, 10, 342. [Google Scholar] [CrossRef]
- Statistica 13.0. Available online: www.statsoft.com (accessed on 20 May 2020).
- Marchionni, N.; Fattirolli, F.; Fumagalli, S.; Oldridge, N.; Del Lungo, F.; Morosi, L.; Burgisser, C.; Masotti, G. Improved Exer-cise tolerance and Quality of live with Cardiac Rehabilitation of Older Patients After Myocardial Infarction: Results of a ran-domized, controlled Trial. Circulation 2003, 107, 2201–2206. [Google Scholar] [CrossRef]
- Humphrey, R.; Guazzi, M.; Niebauer, J. Cardiac Rehabilitation in Europe. Prog. Cardiovasc. Dis. 2014, 56, 551–556. [Google Scholar] [CrossRef]
- Russell, K.L.; Holloway, T.M.; Brum, M.; Caruso, V.; Chessex, C.; Grace, S.L. Cardiac rehabilitation wait times: Effect on enrollment. J. Cardiopulm Rehabil. Prev. 2011, 31, 373–377. [Google Scholar] [CrossRef] [PubMed]
- Ades, P.A.; Keteyian, S.J.; Wright, J.S.; Hamm, L.F.; Lui, K.; Newlin, K.; Shepard, D.S.; Thomas, R.J. Increasing cardiac reha-bilitation participation from 20% to 70%: A road map from the million hearts cardiac rehabilitation collaborative. Mayo Clin. Proc. 2017, 92, 234–242. [Google Scholar] [CrossRef] [PubMed]
- Heldal, M.; Sire, S.; Dale, J. Randomised training after myocardial infarction: Short and long-term effects of exercise training after myocardial infarction in patients on beta-blocker treatment. A randomized, controlled study. Scand. Cardiovasc. J. 2000, 34, 59–64. [Google Scholar] [PubMed]
- Kargarfard, M.; Rouzbehani, R.; Basati, F. Effects of Exercise Rehabilitation on Blood Pressure of Patients after Myocardial Infarction. Int. J. Prev. Med. 2010, 1, 124–130. [Google Scholar] [PubMed]
- Giallauria, F.; Lucci, R.; D’Agostino, M.; Vitelli, A.; Maresca, L.; Mancini, M.; Aurino, M.; Del Forno, D.; Giannuzzi., P.; Vigorito, C. Two-year multicomprehensive secondary prevention program: Favorable effects on cardiovascular functional capacity and coronary risk profile after acute myocardial infarction. J. Cardiovasc. Med. 2009, 10, 772–780. [Google Scholar] [CrossRef]
- Ilarraza, H.; Myers, J.; Kottman, W.; Rickli, H.; Dubach, P. An evaluation of training responses using self-regulation in residential rehabilitation program. J. Cardiopulm Rehabil. 2004, 24, 27–33. [Google Scholar] [CrossRef]
- Hevey, D.; Brown, A.; Cahill, A.; Newton, H.; Kierns, M.; Horgan, J.H. Four-week Multidisciplinary Cardiac Rehabilitation Produces Similar Improvements in Exercise Capacity and Quality of Life to a 10-week Program. J. Cardiopulm. Rehabil. 2003, 23, 17–21. [Google Scholar] [CrossRef]
- Gathright, E.C.; Goldstein, C.M.; Loucks, E.B.; Busch, A.M.; Stabile, L.; Wu, W.-C. Examination of clinical and psychosocial determinants of exercise capacity change in cardiac rehabilitation. Hear. Lung 2019, 48, 13–17. [Google Scholar] [CrossRef]
- Piotrowicz, R.; Wolszakiewicz, J. Cardiac rehabilitation following myocardial infarction. Cardiol. J. 2008, 15, 18810728. [Google Scholar]
- Agarwal, M.; Agrawal, S.; Garg, L.; Mohananey, D.; Garg, A.; Bhatia, N.; Lavie, C.J. National Trends in the Incidence, Management, and Outcomes of Heart Failure Complications in Patients Hospitalized for ST-Segment Elevation Myocardial Infarction. Mayo Clin. Proc. Innov. Qual. Outcomes 2017, 1, 26–36. [Google Scholar] [CrossRef] [PubMed]


| Model | Risk | Exercise Tolerance | Types of Training | Frequency | Total Duration | Intensity |
|---|---|---|---|---|---|---|
| A | Low | Normal ≥7 MET; ≥100 VAT | Continuous type of endurance training on the treadmill | 3–5 days a week | 60–90 min per day | 60–80% heart rate reserve or 50–70% maximum load |
| Resistance training | 2–3 days a week | |||||
| A set of general fitness exercises | 2–3 series 5 days a week | |||||
| B | Medium | Normal and medium ≥5 MET; ≥75 W | Endurance training on the treadmill Continuous type—for patients with good exercise tolerance Interval—for patients with medium exercise tolerance | 3–5 days a week | 45–60 min per day | 50–60% heart rate reserve or 50% maximum load |
| Resistance training | 2–3 days a week | |||||
| A set of general fitness exercises | 1 series 5 days per week | |||||
| C | Medium High | Low 3–5 MET; 50–75 W Normal ≥ 6 MET; >75 W | Interval type of endurance training on the treadmill | 3–5 days a week | 45 min per day | 40–50% heart rate reserve or 40–50% maximum load |
| Continuous type of endurance training on the treadmill (5–10 min) | 2 days per week | |||||
| A set of general fitness exercises | 5 days per week | |||||
| Elements of resistance training (exercises performed alternately once with one limb and once with the other limb) | 2–3 days a week1 series |
| Parameter | BMI | WHR | Waist [cm] | Cholesterol | HDL |
| Mean (SD) Range Me 95% CI | 29.3 (4.1) 20.5–41.0 29.0 [28.5;30.0] | 1.7 (8.0) 0.7–91.0 1.0 [0.3;3.1] | 100.1 (11.8) 69.0–130.0 100.0 [98.0;102.2] | 207.2 (198.9) 25.9–320.0 185.0 [172.2;242.3] | 50.0 (18.6) 28.0–162.0 44.0 [46.7;53.3] |
| Parameter | LDL | TG | LVEF | ||
| Mean (SD) Range Me 95% CI | 123.8 (62.1) 32.0–564.0 114.5 [112.9;134.8] | 164.0 (177.3) 29.0–1421 134.0 [132.8;195.3] | 53.8 (7.9) 35.0–65.0 56.0 [52.4;55.1] |
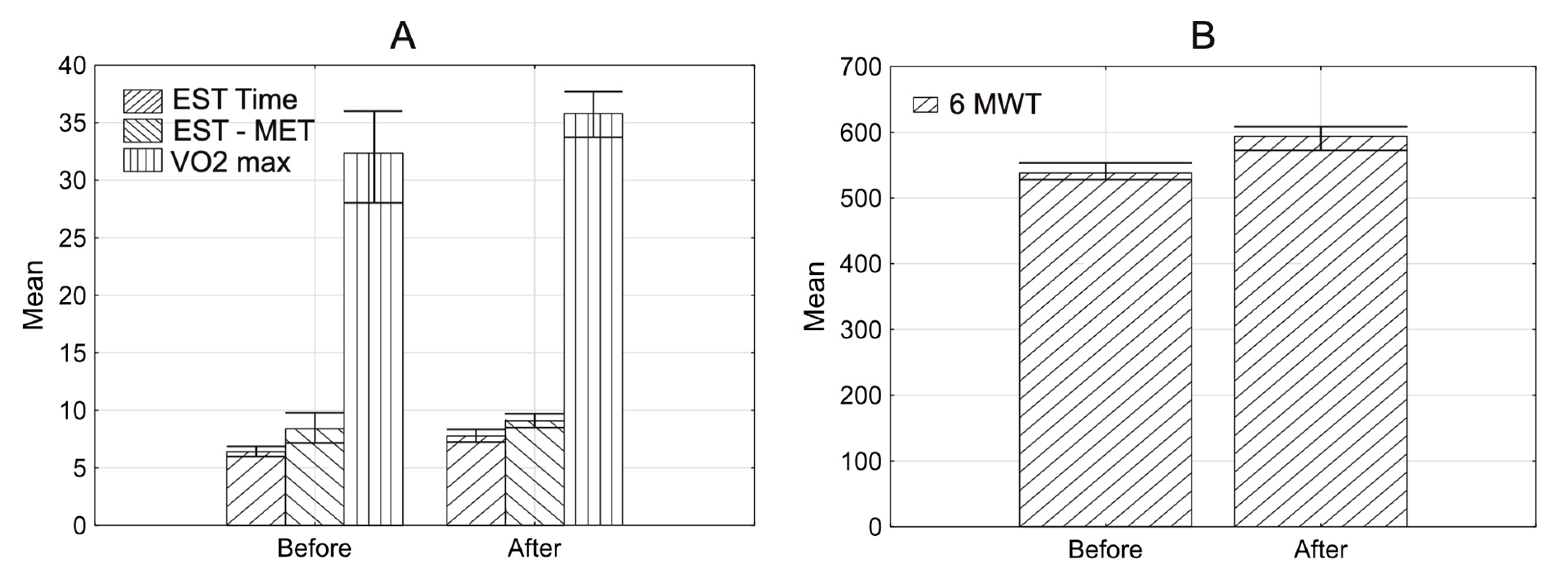
| n = 126 | Parameter | Exercise Stress Test Time [min] | Exercise Stress Test MET | VO2max | DPr | 6MWT [m] |
|---|---|---|---|---|---|---|
| Before rehabilitation | Mean (SD) Range Me 95% CI | 6.4 (2.2) 0.6–14.3 6.4 [6.0;6.8] | 8.4 (7.2) 2.5–85.0 7.8 [7.1;9.6] | 32.3 (25.4) 16.3–302.0 29.2 [27.9;36.8] | 18360.3 (4504.6) 25.0–28400.0 18515.0 [17541.2;19179.4] | 538.0 (80.9) 340.0–820.0 530.0 [523.8;552.3] |
| After rehabilitation | Mean (SD) Range Me 95% CI | 7.8 (2.2) 2.0–13.6 8.2 [7.4;8.2] | 9.1 (2.2) 3.4–14.1 9.4 [8.7;9.5] | 35.8 (9.6) 18.5–61.9 35.4 [34.1;37.5] | 18592.2 (4504.6) 8530.0–28000.0 18270.0 [17798.2;19386.6] | 593.0 (94.3) 186.0–800.0 600.0 [577.3;610.5] |
| p-value | 0.0001 1 | 0.0001 1 | 0.0001 1 | 0.5232 1 | 0.0001 1 |
| Rehabilitation n = 126 | Parameter | Exercise Stress Test Time [min] | Exercise Stress Test MET | VO2max | DPr | 6 MWT |
|---|---|---|---|---|---|---|
| Before rehabilitation | Mean (SD) Range Me 95% CI | 7.3 (2.0) 1.0–12.1 7.3 [6.9;7.6] | 9.1 (5.8) 2.5–70.0 8.7 [8.1;10.1] | 33.5 (8.2) 16.3–60.2 32.9 [32.0;35.0] | 18627.3 (4215.7) 8460.0–27710.0 18660.0 [17884.0;19370.6] | 579.2 (67.9) 340.0–820.0 530.0 [523.8;552.3] |
| After rehabilitation | Mean (SD) Range Me 95% CI | 14.8 (72.5) 2.0–815.0 8.6 [2.0;27.7] | 10.2 (5.2) 3.4–63.0 10.0 [9.2;11.1] | 38.3 (10.3) 18.5–63.9 38.4 [36.4;40.1] | 19466.9 (4251.2) 10370.0–30780.0 19650.0 [18717.4;20216.5] | 628.0 (77.7) 380.0–820.0 640.0 [615.2;642.6] |
| p-value | 0.0001 1 | 0.0001 1 | 0.0001 1 | 0.0031 4 | 0.0001 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grochulska, A.; Glowinski, S.; Bryndal, A. Cardiac Rehabilitation and Physical Performance in Patients after Myocardial Infarction: Preliminary Research. J. Clin. Med. 2021, 10, 2253. https://doi.org/10.3390/jcm10112253
Grochulska A, Glowinski S, Bryndal A. Cardiac Rehabilitation and Physical Performance in Patients after Myocardial Infarction: Preliminary Research. Journal of Clinical Medicine. 2021; 10(11):2253. https://doi.org/10.3390/jcm10112253
Chicago/Turabian StyleGrochulska, Agnieszka, Sebastian Glowinski, and Aleksandra Bryndal. 2021. "Cardiac Rehabilitation and Physical Performance in Patients after Myocardial Infarction: Preliminary Research" Journal of Clinical Medicine 10, no. 11: 2253. https://doi.org/10.3390/jcm10112253
APA StyleGrochulska, A., Glowinski, S., & Bryndal, A. (2021). Cardiac Rehabilitation and Physical Performance in Patients after Myocardial Infarction: Preliminary Research. Journal of Clinical Medicine, 10(11), 2253. https://doi.org/10.3390/jcm10112253







