Application of a Lifestyle-Based Score to Predict Cardiovascular Risk in African Americans: The Jackson Heart Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Healthy Heart Score
2.3. Assessment of Cardiovascular Disease
2.4. Statistical Analysis
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rosamond, W.; Flegal, K.; Furie, K.; Go, A.; Greenlund, K.; Haase, N.; Hailpern, S.M.; Ho, M.; Howard, V. Heart Disease and Stroke Statistics—2008 Update. Circulation 2008, 117, e25–e146. [Google Scholar] [CrossRef]
- Carnethon, M.R.; Pu, J.; Howard, G.; Albert, M.A.; Anderson, C.A.; Bertoni, A.G.; Mujahid, M.S.; Palaniappan, L.; Taylor, H.A.; Willis, M.; et al. Cardiovascular Health in African Americans: A Scientific Statement from the American Heart Association. Circulation 2017, 136, e393–e423. [Google Scholar] [CrossRef]
- Benjamin, E.J.; Blaha, M.J.; Chiuve, S.E.; Cushman, M.; Das, S.R.; de Ferranti, S.D.; Floyd, J.; Fornage, M.; Gillespie, C.; Isasi, C.R.; et al. Heart disease and stroke statistics—2017 update a report from the American heart association. Circulation 2017, 135, e146–e603. [Google Scholar] [CrossRef]
- Joseph, J.J.; Echouffo-Tcheugui, J.B.; Talegawkar, S.A.; Effoe, V.S.; Okhomina, V.; Carnethon, M.R.; Hsueh, W.A.; Golden, S.H. Modifiable Lifestyle Risk Factors and Incident Diabetes in African Americans. Am. J. Prev. Med. 2017, 53, e165–e174. [Google Scholar] [CrossRef]
- Fox, E.R.; Samdarshi, T.E.; Musani, S.K.; Pencina, M.J.; Sung, J.H.; Bertoni, A.G.; Xanthakis, V.; Balfour, P.C.; Shreenivas, S.S.; Covington, C.; et al. Development and Validation of Risk Prediction Models for Cardiovascular Events in Black Adults. JAMA Cardiol. 2016, 1, 15–25. [Google Scholar] [CrossRef] [PubMed]
- D’Agostino, R.B.; Grundy, S.; Sullivan, L.M.; Wilson, P. Validation of the Framingham Coronary Heart Disease Prediction Scores. JAMA 2001, 286, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Pencina, M.J.; D’Agostino, R.B.; Larson, M.G.; Massaro, J.M.; Vasan, R.S. Predicting the 30-Year Risk of Cardiovascular Disease. Circulation 2009, 119, 3078–3084. [Google Scholar] [CrossRef]
- Goff, D.C., Jr.; Lloyd-Jones, D.M.; Bennett, G.; Coady, S.; D’Agostino, R.B.; Gibbons, R.; Greenland, P.; Lackland, D.T.; Levy, D.; O’Donnell, C.J.; et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2014, 63, 2935–2959. [Google Scholar] [CrossRef] [PubMed]
- Hippisley-Cox, J.; Coupland, C.; Vinogradova, Y.; Robson, J.; May, M.; Brindle, P. Derivation and validation of QRISK, a new cardiovascular disease risk score for the United Kingdom: Prospective open cohort study. BMJ 2007, 335, 136. [Google Scholar] [CrossRef] [PubMed]
- Ridker, P.M.; Buring, J.E.; Rifai, N.; Cook, N.R. Development and Validation of Improved Algorithms for the Assessment of Global Cardiovascular Risk in Women. JAMA 2007, 297, 611–619. [Google Scholar] [CrossRef]
- Champagne, C.M.; Bogle, M.L.; McGee, B.B.; Yadrick, K.; Allen, H.; Kramer, T.R.; Simpson, P.; Gossett, J.; Weber, J. Dietary intake in the lower Mississippi delta region: Results from the foods of our delta study. J. Am. Diet. Assoc. 2004, 104, 199–207. [Google Scholar] [CrossRef] [PubMed]
- On Racism: A New Standard for Publishing on Racial Health Inequities. Health Affairs. Available online: https://www.healthaffairs.org/do/10.1377/hblog20200630.939347/full/ (accessed on 9 July 2020).
- Chiuve, S.E.; Cook, N.R.; Shay, C.; Rexrode, K.M.; Albert, C.M.; Manson, J.E.; Willett, W.C.; Rimm, E.B. Lifestyle-Based Prediction Model for the Prevention of CVD: The Healthy Heart Score. J. Am. Heart Assoc. 2014, 3, e000954. [Google Scholar] [CrossRef] [PubMed]
- Gooding, H.C.; Ning, H.; Gillman, M.W.; Shay, C.; Allen, N.; Goff, D.C.; Lloyd-Jones, D.; Chiuve, S. Application of a Lifestyle-Based Tool to Estimate Premature Cardiovascular Disease Events in Young Adults. JAMA Intern. Med. 2017, 177, 1354–1360. [Google Scholar] [CrossRef] [PubMed]
- Fuqua, S.R.; Wyatt, S.B.; Andrew, M.E.; Sarpong, D.F.; Henderson, F.R.; Cunningham, M.F.; Taylor, H.A., Jr. Recruiting African-American research participation in the Jackson Heart Study: Methods, response rates, and sample description. Ethn. Dis. 2005, 15, S6-18–S6-29. [Google Scholar]
- Carithers, T.C.; Talegawkar, S.A.; Rowser, M.L.; Henry, O.R.; Dubbert, P.M.; Bogle, M.L.; Taylor, H.A.; Tucker, K.L. Validity and Calibration of Food Frequency Questionnaires Used with African-American Adults in the Jackson Heart Study. J. Am. Diet. Assoc. 2009, 109, 1184–1193. [Google Scholar] [CrossRef]
- Talegawkar, S.A.; Johnson, E.J.; Carithers, T.C.; Taylor, H.A.; Bogle, M.L.; Tucker, K.L. Serum Carotenoid and Tocopherol Concentrations Vary by Dietary Pattern among African Americans. J. Am. Diet. Assoc. 2008, 108, 2013–2020. [Google Scholar] [CrossRef] [PubMed]
- Talegawkar, S.A.; Johnson, E.J.; Carithers, T.C.; Taylor, H.A.; Bogle, M.L.; Tucker, K.L. Carotenoid intakes, assessed by food-frequency questionnaires (FFQs), are associated with serum carotenoid concentrations in the Jackson Heart Study: Validation of the Jackson Heart Study Delta NIRI Adult FFQs. Public Health Nutr. 2008, 11, 989–997. [Google Scholar] [CrossRef]
- Dubbert, P.M.; Carithers, T.; Ainsworth, B.E.; Taylor, H.A.; Wilson, G.; Wyatt, S.B. Physical activity assessment methods in the Jackson Heart Study. Ethn. Dis. 2005, 15, S6-56–S6-61. [Google Scholar]
- Booth, I.J.N.; Abdalla, M.; Tanner, R.M.; Diaz, K.M.; Bromfield, S.G.; Tajeu, G.S.; Correa, A.; Sims, M.; Ogedegbe, G.; Bress, A.P.; et al. Cardiovascular Health and Incident Hypertension in Blacks. Hypertension 2017, 70, 285–292. [Google Scholar] [CrossRef]
- Keku, E.; Rosamond, W.; Taylor, H.A.; Garrison, R.; Wyatt, S.B.; Richard, M.; Jenkins, B.; Reeves, L.; Sarpong, D. Cardiovascular disease event classification in the Jackson Heart Study: Methods and procedures. Ethn. Dis. 2005, 15, S6-62–S6-70. [Google Scholar]
- Harrell, F.E. Cox Proportional Hazards Regression Model. In Regression Modeling Strategies: With Applications to Linear Models, Logistic and Ordinal Regression, and Survival Analysis; Harrell, F.E., Jr., Ed.; Springer: Cham, Switzerland, 2015; pp. 475–519. [Google Scholar] [CrossRef]
- Effoe, V.S.; Carnethon, M.R.; Echouffo-Tcheugui, J.B.; Chen, H.; Joseph, J.J.; Norwood, A.F.; Bertoni, A.G. The American Heart Association Ideal Cardiovascular Health and Incident Type 2 Diabetes Mellitus Among Blacks: The Jackson Heart Study. J. Am. Heart Assoc. 2017, 6, e005008. [Google Scholar] [CrossRef] [PubMed]
- Joseph, J.J.; Echouffo-Tcheugui, J.B.; Carnethon, M.R.; Bertoni, A.G.; Shay, C.M.; Ahmed, H.M.; Blumenthal, R.S.; Cushman, M.; Golden, S.H. The association of ideal cardiovascular health with incident type 2 diabetes mellitus: The Multi-Ethnic Study of Atherosclerosis. Diabetologia 2016, 59, 1893–1903. [Google Scholar] [CrossRef] [PubMed]
- Booth, J.N.; Allen, N.B.; Calhoun, D.; Carson, A.P.; Deng, L.; Goff, D.C.; Redden, D.T.; Reis, J.P.; Shimbo, D.; Shikany, J.M.; et al. Racial Differences in Maintaining Optimal Health Behaviors into Middle Age. Am. J. Prev. Med. 2019, 56, 368–375. [Google Scholar] [CrossRef] [PubMed]
- Bress, A.P.; Colantonio, L.D.; Booth, J.N.; Spruill, T.M.; Ravenell, J.; Butler, M.; Shallcross, A.J.; Seals, S.R.; Reynolds, K.; Ogedegbe, G.; et al. Modifiable Risk Factors Versus Age on Developing High Predicted Cardiovascular Disease Risk in Blacks. J. Am. Heart Assoc. 2017, 6, e005054. [Google Scholar] [CrossRef]
- Flint, A.C.; Conell, C.; Ren, X.; Banki, N.M.; Chan, S.L.; Rao, V.A.; Melles, R.B.; Bhatt, D.L. Effect of Systolic and Diastolic Blood Pressure on Cardiovascular Outcomes. N. Engl. J. Med. 2019, 381, 243–251. [Google Scholar] [CrossRef]
- Sotos-Prieto, M.; Mattei, J.; Hu, F.B.; Chomistek, A.K.; Rimm, E.B.; Willett, W.C.; Eliassen, A.H.; Chiuve, S.E. Association Between a Healthy Heart Score and the Development of Clinical Cardiovascular Risk Factors Among Women. Circ. Cardiovasc. Qual. Outcomes 2016, 9, S77–S85. [Google Scholar] [CrossRef][Green Version]
- Sotos-Prieto, M.; Mattei, J.; Cook, N.R.; Hu, F.B.; Willett, W.C.; Chiuve, S.E.; Rimm, E.B.; Sesso, H.D. Association Between a 20-Year Cardiovascular Disease Risk Score Based on Modifiable Lifestyles and Total and Cause-Specific Mortality Among US Men and Women. J. Am. Heart Assoc. 2018, 7, e010052. [Google Scholar] [CrossRef]
- Belin, R.J.; Greenland, P.; Allison, M.; Martin, L.W.; Shikany, J.M.; Larson, J.; Tinker, L.; Howard, B.V.; Lloyd-Jones, N.; Van Horn, L. Diet quality and the risk of cardiovascular disease: The Women’s Health Initiative (WHI). Am. J. Clin. Nutr. 2011, 94, 49–57. [Google Scholar] [CrossRef]
- Appel, L.J.; Moore, T.J.; Obarzanek, E.; Vollmer, W.M.; Svetkey, L.P.; Sacks, F.M.; Bray, G.A.; Vogt, T.M.; Cutler, J.A.; Windhauser, M.M.; et al. A Clinical Trial of the Effects of Dietary Patterns on Blood Pressure. N. Engl. J. Med. 1997, 336, 1117–1124. [Google Scholar] [CrossRef]
- Fuchs, F.D.; Chambless, L.E.; Folsom, A.R.; Eigenbrodt, M.L.; Duncan, B.B.; Gilbert, A.; Szklo, M. Association between Alcoholic Beverage Consumption and Incidence of Coronary Heart Disease in Whites and Blacks: The Atherosclerosis Risk in Communities Study. Am. J. Epidemiol. 2004, 160, 466–474. [Google Scholar] [CrossRef]
- Carithers, T.; Dubbert, P.M.; Crook, E.; Davy, B.; Wyatt, S.B.; Bogle, M.L.; Taylor, H.A.; Tucker, K.L. Dietary assessment in African Americans: Methods used in the Jackson Heart Study. Ethn. Dis. 2005, 15, S6-49–S6-55. [Google Scholar]
- Validation of the Jackson Heart Study Physical Activity Survey in African Americans—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/19998858/ (accessed on 12 June 2020).
- Products—Data Briefs—Number 100—July 2012. Available online: https://www.cdc.gov/nchs/products/databriefs/db100.htm (accessed on 15 June 2020).
| Variable | Total (n = 3041) | Female (n = 1917) | Male (n = 1124) |
|---|---|---|---|
| Age, years, mean (SD) | 53.1 (12.7) | 53.5 (12.8) | 52.4 (12.5) |
| Smoker | |||
| Never | 2189 (72%) | 1491 (77.8%) | 698 (62.1%) |
| Past | 492 (16.2%) | 253 (13.2%) | 239 (21.3%) |
| Current | 360 (11.8%) | 173 (9%) | 187 (16.6%) |
| Body mass index, kg/m2 | 30.9 (6.9) | 31.9 (7.3) | 29.4 (5.9) |
| Moderate and vigorous physical activity, hours/week | 0.3 [0, 1.7] | 0.2 [0, 1.5] | 0.5 [0, 1.9] |
| Total alcohol intake, g/day | 0.4 [0.1, 1.8] | 0.3 [0.1, 0.9] | 0.9 [0.1, 7.4] |
| Total Cholesterol, (mg/dL) mean (SD) | 199.9 (38.1) | 200.8 (37.6) | 198.5 (38.9) |
| Low-Density Lipoprotein (mg/dL) mean (SD) | 128.2 (35.8) | 126.6 (34.9) | 131 (37) |
| Estimated Glomerular Filtration Rate, ml/min per 1.73 m2 mean (SD) | 96.6 (19.4) | 97.5 (20.4) | 95.2 (17.6) |
| Blood pressure, mmHg mean (SD) | 125.7 (16.4) | 125 (16.8) | 127 (15.5) |
| Glucose, mg/dl mean (SD) | 90.1 (8.7) | 89.3 (8.7) | 91.4 (8.5) |
| Hemoglobin A1c, % | 5.5 [5.2, 5.8] | 5.5 [5.2, 5.8] | 5.6 [5.2, 5.8] |
| Diet Score Components | |||
| Total fruits and vegetables, serving/day | 5.9 [3.8, 8.8] | 6 [3.9, 9] | 5.7 [3.7, 8.5] |
| Total cereal fiber, g/day | 1.1 [0.4, 2.8] | 1.2 [0.4, 2.9] | 1.1 [0.4, 2.6] |
| Total red and processed meat, serving/day | 1.6 [0.9, 2.8] | 1.4 [0.8, 2.4] | 2.1 [1.2, 3.5] |
| Total nuts, serving/day | 0.2 [0, 0.6] | 0.1 [0, 0.5] | 0.2 [0.1, 0.6] |
| Sweetened beverages, serving/day | 1 [0.3, 2.2] | 0.9 [0.3, 2] | 1.1 [0.5, 2.5] |
| Diet Score, [score range] | −2.5 [−34.9, 15.2] | −1.9 [−34.9, 15.2] | −3.4 [−27.8, 4.3] |
| Heart Healthy Score | |||
| Heart Healthy Score, [score range] | 7.7 [3.4, 13] | 7.4 [3.4, 13] | 8.1 [4.4, 12.4] |
| Events | |||
| Cardiovascular Events | |||
| No | 2852 (93.8%) | 1806 (94.2%) | 1046 (93.1%) |
| Yes | 189 (6.2%) | 111 (5.8%) | 78 (6.9%) |
| Incident Cardiovascular Events | Total (n = 3041) | Men (n = 1124) | Women (n = 1917) |
|---|---|---|---|
| HR (95% CI) Age Alone | 1.07 (1.06, 1.09) | 1.07 (1.05, 1.09) | 1.08 (1.06, 1.1) |
| HR (95% CI) Healthy Heart Score | 1.98 (1.77, 2.23) | 2.07 (1.68, 2.55) | 1.95 (1.7, 2.25) |
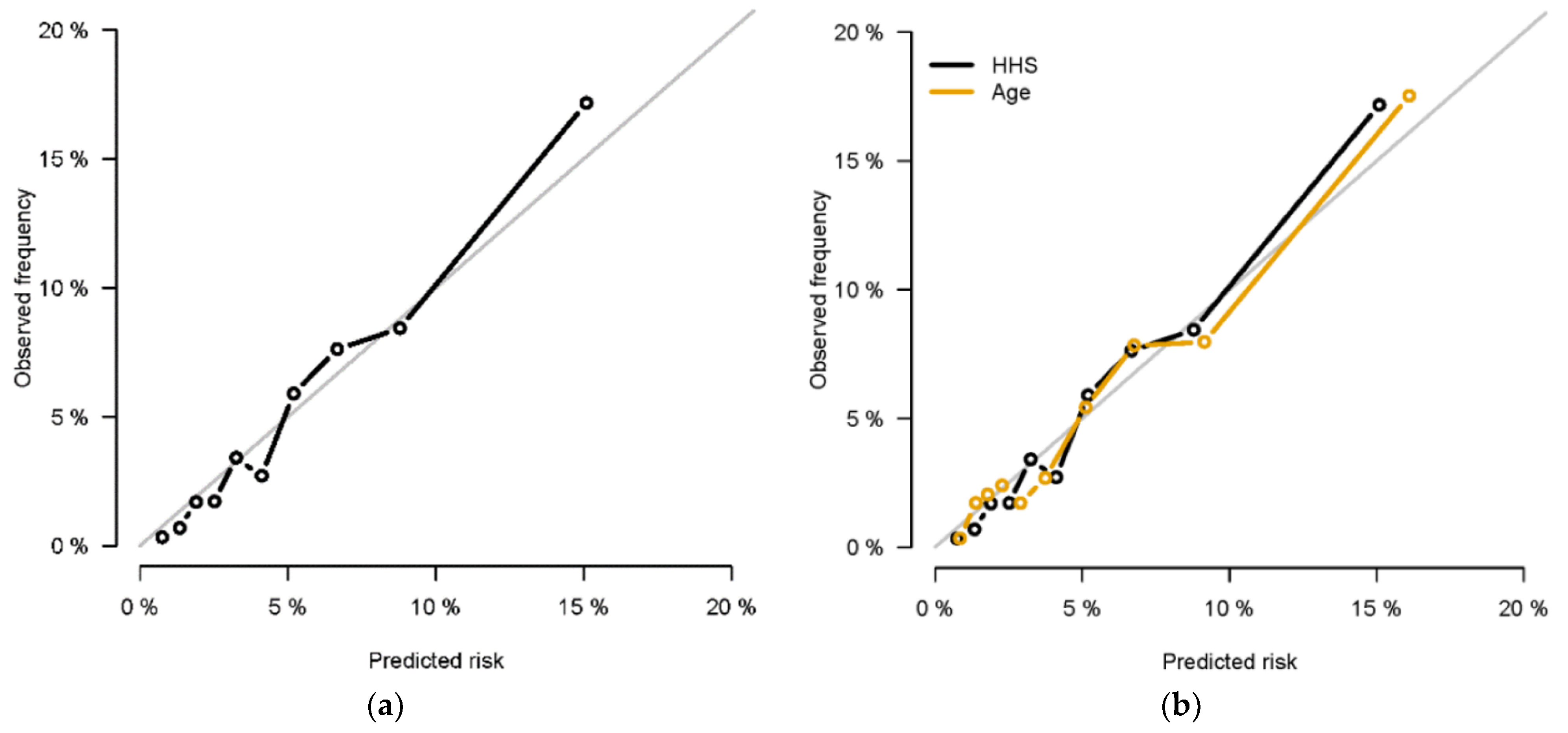
| Harrell’s Concordance Statistic (95% CI)—Age Alone | 0.74 (0.7, 0.77) | 0.73 (0.68, 0.79) | 0.75 (0.7, 0.79) |
| Harrell’s Concordance Statistic—(95% CI) Healthy Heart Score | 0.75 (0.71, 0.78) | 0.73 (0.68, 0.78) | 0.75 (0.71, 0.8) |
| Time Dependent AUC (95% CI)—Age Alone | |||
| 1 year | 0.76 (0.65, 0.88) | 0.81 (0.67, 0.95) | 0.72 (0.54, 0.9) |
| 3 years | 0.76 (0.70, 0.83) | 0.76 (0.65, 0.87) | 0.77 (0.69, 0.84) |
| 5 years | 0.77 (0.72, 0.81) | 0.76 (0.67, 0.84) | 0.78 (0.72, 0.83) |
| Integrated Time-Dependent AUC—Age Alone | 0.76 | 0.77 | 0.76 |
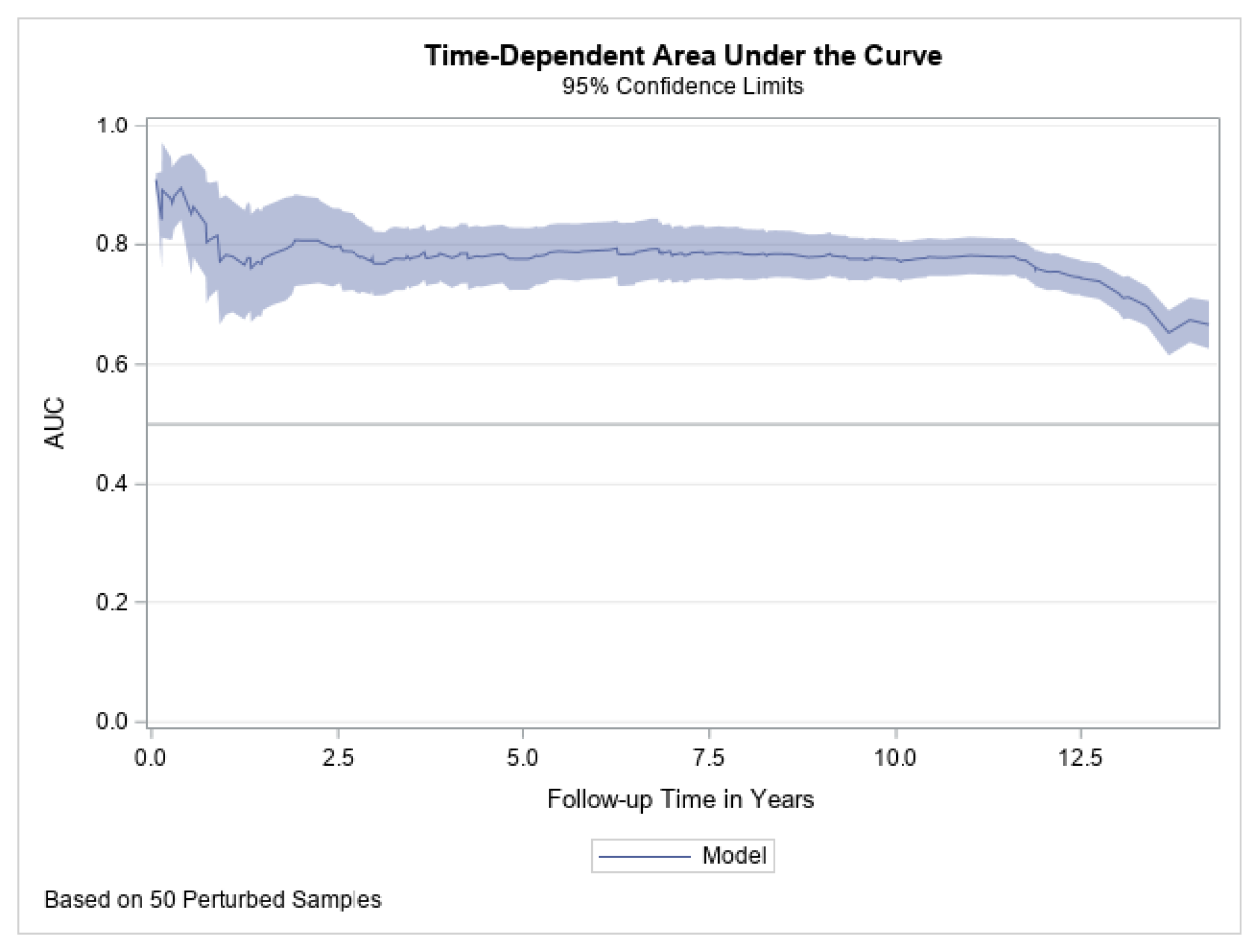
| Time Dependent AUC (95% CI)—Healthy Heart Score | |||
| 1 year | 0.78 (0.68, 0.89) | 0.79 (0.64, 0.94) | 0.76 (0.59, 0.93) |
| 3 years | 0.77 (0.72, 0.83) | 0.78 (0.68, 0.87) | 0.78 (0.7, 0.85) |
| 5 years | 0.78 (0.73, 0.82) | 0.77 (0.69, 0.85) | 0.78 (0.72, 0.84) |
| Integrated Time-Dependent AUC—Healthy Heart Score | 0.77 | 0.77 | 0.77 |
| Incident Cardiovascular Events | Total (n = 3041) | Men (n = 1124) | Women (n = 1917) | |||
|---|---|---|---|---|---|---|
| Age < Median (n = 1520) | Age > = Median (n = 1521) | Age < Median (n = 562) | Age > = Median (n = 562) | Age < Median (n = 958) | Age > = Median (n = 959) | |
| HR (95% CI) Age alone | 1.08 (1.01, 1.14) | 1.07 (1.05, 1.10) | 1.08 (0.99, 1.17) | 1.08 (1.05, 1.11) | 1.09 (0.999, 1.18) | 1.07 (1.05, 1.1) |
| Harrell’s Concordance Statistic—Age alone | 0.61 (0.53, 0.68) | 0.66 (0.62, 0.71) | 0.61 (0.5, 0.73) | 0.68 (0.61, 0.75) | 0.62 (0.52, 0.71) | 0.66 (0.60, 0.72) |
| Integrated Time-Dependent AUC—Age alone | 0.64 | 0.68 | 0.69 | 0.70 | 0.59 | 0.66 |
| HR (95% CI) Healthy Heart Score | 1.6(1.24, 2.05) | 1.97 (1.64, 2.38) | 1.8 (1.08, 3) | 1.87 (1.38, 2.54) | 1.54 (1.05, 2.26) | 1.94 (1.55, 2.44) |
| Harrell’s Concordance Statistic Healthy Heart Score | 0.67 (0.59, 0.75) | 0.67 (0.63, 0.71) | 0.65 (0.54, 0.76) | 0.66 (0.6, 0.73) | 0.65 (0.55, 0.75) | 0.67 (0.61, 0.73) |
| Integrated Time-Dependent AUC Healthy Heart Score | 0.69 | 0.69 | 0.69 | 0.71 | 0.63 | 0.67 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sotos-Prieto, M.; Zhao, S.; Kline, D.; Brock, G.; Gooding, H.; Mattei, J.; Rodriguez-Artalejo, F.; Min, Y.-I.; Rimm, E.B.; Tucker, K.L.; et al. Application of a Lifestyle-Based Score to Predict Cardiovascular Risk in African Americans: The Jackson Heart Study. J. Clin. Med. 2021, 10, 2252. https://doi.org/10.3390/jcm10112252
Sotos-Prieto M, Zhao S, Kline D, Brock G, Gooding H, Mattei J, Rodriguez-Artalejo F, Min Y-I, Rimm EB, Tucker KL, et al. Application of a Lifestyle-Based Score to Predict Cardiovascular Risk in African Americans: The Jackson Heart Study. Journal of Clinical Medicine. 2021; 10(11):2252. https://doi.org/10.3390/jcm10112252
Chicago/Turabian StyleSotos-Prieto, Mercedes, Songzhu Zhao, David Kline, Guy Brock, Holly Gooding, Josiemer Mattei, Fernando Rodriguez-Artalejo, Yuan-I Min, Eric B. Rimm, Katherine L. Tucker, and et al. 2021. "Application of a Lifestyle-Based Score to Predict Cardiovascular Risk in African Americans: The Jackson Heart Study" Journal of Clinical Medicine 10, no. 11: 2252. https://doi.org/10.3390/jcm10112252
APA StyleSotos-Prieto, M., Zhao, S., Kline, D., Brock, G., Gooding, H., Mattei, J., Rodriguez-Artalejo, F., Min, Y.-I., Rimm, E. B., Tucker, K. L., & Joseph, J. J. (2021). Application of a Lifestyle-Based Score to Predict Cardiovascular Risk in African Americans: The Jackson Heart Study. Journal of Clinical Medicine, 10(11), 2252. https://doi.org/10.3390/jcm10112252







