Feasibility and Safety of the Left Distal Radial Approach in Percutaneous Coronary Intervention for Bifurcation Lesions
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects and Study Design
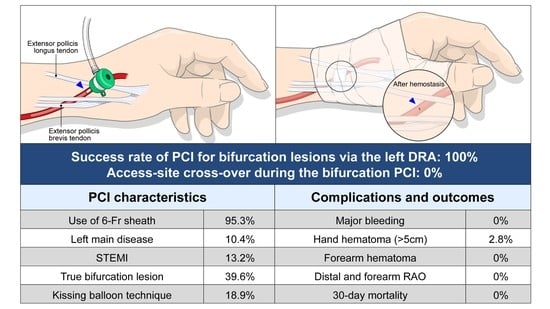
2.2. Preparation for the Left Distal Radial Approach
2.3. Procedural Details of Percutaneous Coronary Intervention for Bifurcation Lesions
2.4. Definition and Study Endpoints
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2018, 39, 119–177. [Google Scholar] [PubMed] [Green Version]
- Neumann, F.-J.; Sousa-Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.-P.; Falk, V.; Head, S.J.; et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. Heart J. 2019, 40, 87–165. [Google Scholar] [CrossRef] [PubMed]
- Kolkailah, A.A.; Alreshq, R.S.; Muhammed, A.M.; Zahran, M.E.; El-Wegoud, M.A.; Nabhan, A.F. Transradial versus transfemoral approach for diagnostic coronary angiography and percutaneous coronary intervention in people with coronary artery disease. Cochrane Database Syst. Rev. 2018, 4, CD012318. [Google Scholar] [CrossRef] [PubMed]
- Rashid, M.; Lawson, C.; Potts, J.; Kontopantelis, E.; Kwok, C.S.; Bertrand, O.F.; Shoaib, A.; Ludman, P.; Kinnaird, T.; de Belder, M.; et al. Incidence, determinants, and outcomes of left and right radial access use in patients undergoing percutaneous coronary intervention in the United Kingdom: A national perspective using the BCIS dataset. JACC Cardiovasc. Interv. 2018, 11, 1021–1033. [Google Scholar] [CrossRef]
- Kiemeneij, F. Left distal transradial access in the anatomical snuffbox for coronary angiography (ldTRA) and interventions (ldTRI). EuroIntervention 2017, 13, 851–857. [Google Scholar] [CrossRef]
- Sgueglia, G.A.; Di Giorgio, A.; Gaspardone, A.; Babunashvili, A. Anatomic basis and physiological rationale of distal radial artery access for percutaneous coronary and endovascular procedures. JACC Cardiovasc. Interv. 2018, 11, 2113–2119. [Google Scholar] [CrossRef]
- Sgueglia, G.A.; Lee, B.K.; Cho, B.R.; Babunashvili, A.; Lee, J.B.; Lee, J.W.; Schenke, K.; Lee, S.Y.; Harb, S. Distal radial access: Consensus report of the first Korea-Europe transradial intervention meeting. JACC Cardiovasc. Interv. 2021, 14, 892–906. [Google Scholar] [CrossRef] [PubMed]
- Sawaya, F.J.; Lefèvre, T.; Chevalier, B.; Garot, P.; Hovasse, T.; Morice, M.-C.; Rab, T.; Louvard, Y. Contemporary approach to coronary bifurcation lesion treatment. JACC Cardiovasc. Interv. 2016, 9, 1861–1878. [Google Scholar] [CrossRef]
- Chung, S.; Her, S.-H.; Song, P.S.; Song, Y.B.; Hahn, J.-Y.; Choi, J.-H.; Lee, S.H.; Jang, Y.; Yoon, J.H.; Tahk, S.-J.; et al. Trans-radial versus trans-femoral intervention for the treatment of coronary bifurcations: Results from coronary bifurcation stenting registry. J. Korean Med. Sci. 2013, 28, 388. [Google Scholar] [CrossRef] [Green Version]
- Chung, S.; Yang, J.H.; Choi, S.-H.; Song, Y.B.; Hahn, J.-Y.; Choi, J.-H.; Lee, S.H.; Jang, Y.; Yoon, J.H.; Tahk, S.-J.; et al. Transradial versus transfemoral intervention for the treatment of left main coronary bifurcations: Results from the COBIS (coronary bifurcation stenting) II registry. J. Invasive Cardiol. 2015, 27, 35–40. [Google Scholar]
- Medina, A.; Suárez de Lezo, J.; Pan, M. A new classification of coronary bifurcation lesions. Rev. Esp. Cardiol. 2006, 59, 183. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soydan, E.; Akın, M. Coronary angiography using the left distal radial approach-an alternative site to conventional radial coronary angiography. Anatol. J. Cardiol. 2018, 19, 243. [Google Scholar] [CrossRef] [PubMed]
- Al-Azizi, K.M.; Grewal, V.; Gobeil, K.; Maqsood, K.; Haider, A.; Mohani, A.; Giugliano, G.; Lotfi, A.S. The left distal transradial artery access for coronary angiography and interventions: A US experience. Cardiovasc. Revasc. Med. 2019, 20, 786–789. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Ahn, Y.; Kim, I.; Lee, D.H.; Kim, M.C.; Sim, D.S.; Hong, Y.J.; Kim, J.H.; Jeong, M.H. Feasibility of coronary angiography and percutaneous coronary intervention via left snuffbox approach. Korean Circ. J. 2018, 48, 1120. [Google Scholar] [CrossRef]
- Gasparini, G.L.; Garbo, R.; Gagnor, A.; Oreglia, J.; Mazzarotto, P. First prospective multicentre experience with left distal transradial approach for coronary chronic total occlusion interventions using a 7 Fr Glidesheath Slender. EuroIntervention 2019, 15, 126–128. [Google Scholar] [CrossRef]
- Lee, J.-W.; Park, S.W.; Son, J.-W.; Ahn, S.-G.; Lee, S.-H. Real-world experience of the left distal transradial approach for coronary angiography and percutaneous coronary intervention: A prospective observational study (LeDRA). EuroIntervention 2018, 14, e995–e1003. [Google Scholar] [CrossRef] [Green Version]
- Sciahbasi, A.; Romagnoli, E.; Burzotta, F.; Trani, C.; Sarandrea, A.; Summaria, F.; Pendenza, G.; Tommasino, A.; Patrizi, R.; Mazzari, M.; et al. Transradial approach (left vs right) and procedural times during percutaneous coronary procedures: TALENT study. Am. Heart J. 2011, 161, 172–179. [Google Scholar] [CrossRef]
- Park, J.Y.; Rha, S.-W.; Choi, B.G.; Oh, D.J.; Choi, C.U.; Youn, Y.-J.; Yoon, J. Comparison of clinical outcomes between the right and left radial artery approaches from the Korean transradial coronary intervention registry. Yonsei Med. J. 2017, 58, 521. [Google Scholar] [CrossRef] [Green Version]
- Biondi-Zoccai, G.; Sciahbasi, A.; Bodí, V.; Fernández-Portales, J.; Kanei, Y.; Romagnoli, E.; Agostoni, P.; Sangiorgi, G.; Lotrionte, M.; Modena, M.G. Right versus left radial artery access for coronary procedures: An international collaborative systematic review and meta-analysis including 5 randomized trials and 3210 patients. Int. J. Cardiol. 2013, 166, 621–626. [Google Scholar] [CrossRef] [Green Version]
- Kado, H.; Patel, A.M.; Suryadevara, S.; Zenni, M.M.; Box, L.C.; Angiolillo, D.J.; Bass, T.A.; Guzman, L.A. Operator radiation exposure and physical discomfort during a right versus left radial approach for coronary interventions: A randomized evaluation. JACC Cardiovasc. Interv. 2014, 7, 810–816. [Google Scholar] [CrossRef] [Green Version]
- Colletti, G.; Auslender, J.; Antoine De Meester, M.; Aminian, A.; Kayaert, P.; Ungureanu, C. Feasibility and safety of performing complex coronary interventions by distal radial artery using the railway sheathless vascular system. J. Invasive Cardiol. 2020, 32, 459–462. [Google Scholar]
- Youn, Y.J.; Yoon, J.; Han, S.W.; Lee, J.-W.; Sung, J.K.; Ahn, S.-G.; Kim, J.-Y.; Yoo, B.-S.; Lee, S.-H.; Choe, K.-H. Feasibility of transradial coronary intervention using a sheathless guiding catheter in patients with small radial artery. Korean Circ. J. 2011, 41, 143–148. [Google Scholar] [CrossRef] [Green Version]
- Aminian, A.; Iglesias, J.F.; Van Mieghem, C.; Zuffi, A.; Ferrara, A.; Manih, R.; Dolatabadi, D.; Lalmand, J.; Saito, S. First prospective multicenter experience with the 7 French Glidesheath slender for complex transradial coronary interventions. Catheter. Cardiovasc. Interv. 2017, 89, 1014–1020. [Google Scholar] [CrossRef]


| Characteristic | Value |
|---|---|
| Age (years) | 63.3 ± 11.1 |
| Male sex | 84 (79.2%) |
| Height (cm) | 167.5 (160, 172) |
| Weight (kg) | 69.0 ± 11.1 |
| Body mass index (kg/m2) | 25.0 ± 2.9 |
| Hypertension | 64 (60.4%) |
| Diabetes mellitus | 33 (31.1%) |
| Dyslipidemia | 54 (50.9%) |
| Current smoker | 29 (27.4%) |
| Chronic kidney disease, ≥stage 3 | 15 (14.2%) |
| Clinical presentation | |
| Stable angina | 11 (10.4%) |
| Unstable angina | 54 (50.9%) |
| NSTEMI | 27 (25.5%) |
| STEMI | 14 (13.2%) |
| LVEF (%) | 61.3 ± 11.0 |
| Periprocedural medication | |
| DAPT | 106 (100%) |
| Aspirin | 106 (100%) |
| P2Y12 inhibitor | |
| Clopidogrel | 77 (72.6%) |
| Ticagrelor | 13 (12.3%) |
| Prasugrel | 16 (15.1%) |
| Oral anticoagulation | 3 (2.8%) |
| Glycoprotein IIb/IIIa inhibitors | 5 (4.7%) |
| Characteristic | Value |
|---|---|
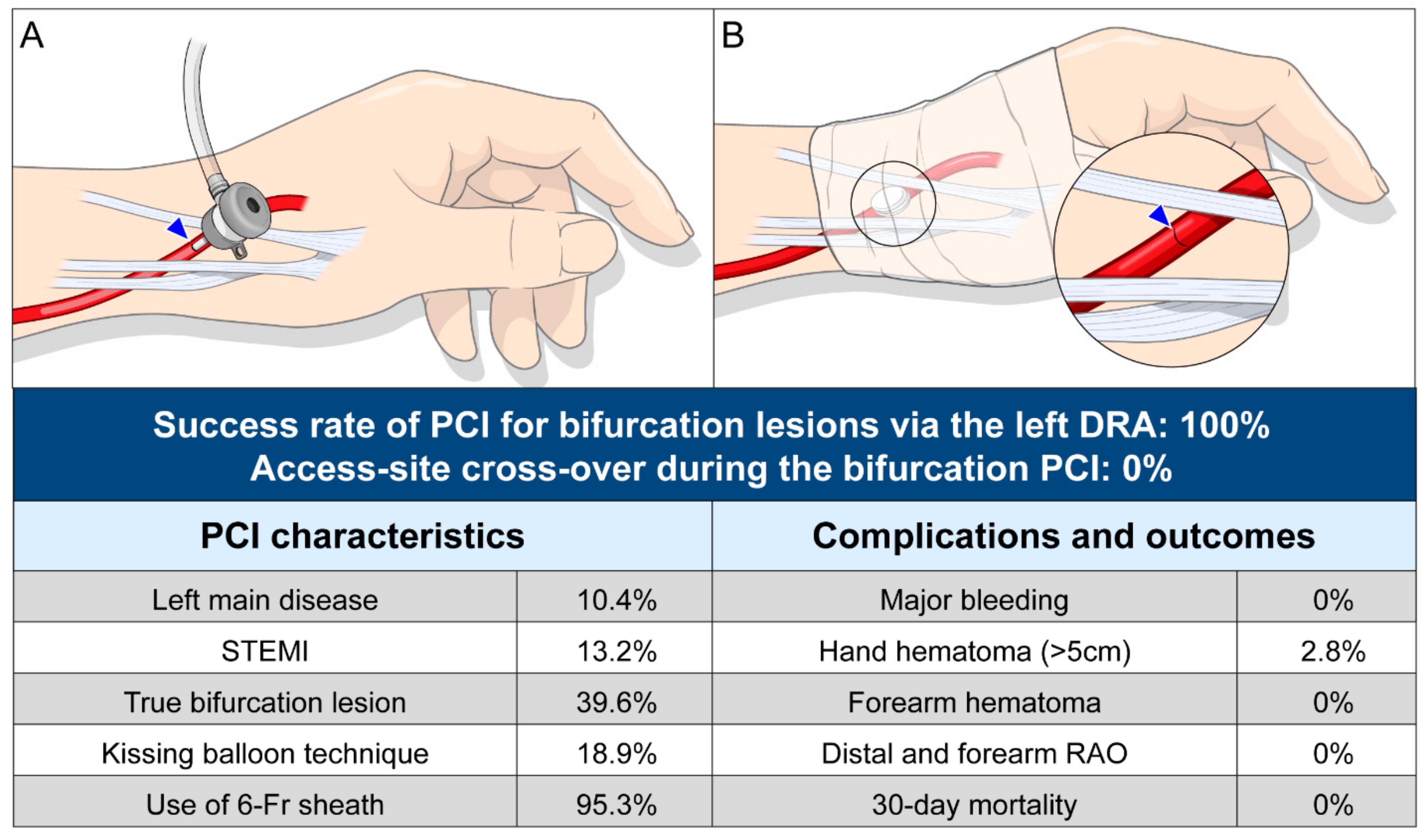
| Successful bifurcation PCI via the left DRA | 106 (100%) |
| Cross-over to another vascular approach | 0 (0) |
| Characteristics of the left DRA | |
| Puncture time (min) | |
| Mean ± SD | 2.4 ± 1.6 |
| Median (IQR) | 1.8 (1.3, 3.4) |
| Puncture time <3 min | 76 (71.7%) |
| Puncture time <5 min | 99 (93.4%) |
| Lesion characteristics | |
| Target lesion | |
| Left main coronary artery | 11 (10.4%) |
| Left anterior descending artery | 61 (57.5%) |
| Left circumflex artery | 18 (17.0%) |
| Right coronary artery | 16 (15.1%) |
| Medina classification | |
| 0, 0, 1 | 2 (1.9%) |
| 0, 1, 0 | 21 (19.8%) |
| 0, 1, 1 | 9 (8.5%) |
| 1, 0, 0 | 16 (15.1%) |
| 1, 0, 1 | 9 (8.5%) |
| 1, 1, 0 | 25 (23.6%) |
| 1, 1, 1 | 24 (22.6%) |
| True bifurcation | 42 (39.6%) |
| ACC/AHA type B2/C lesion | 57 (53.8%) |
| Procedural characteristics | |
| Treatment of the side branch | |
| Plain balloon angioplasty | 26 (24.5%) |
| Stenting (two-stent technique) | 4 (3.8%) |
| Kissing balloon technique | 20 (18.9%) |
| Intravascular imaging-guided PCI | 25 (23.6%) |
| IVUS guidance | 10 (9.4%) |
| OCT guidance | 15 (14.2%) |
| Multi-vessel PCI | 12 (11.3%) |
| Total no. of implanted stents | 1.26 ± 0.54 |
| Cases with implantation of ≥2 stents | 23 (21.7%) |
| Stent diameter in the main vessel (mm) | 2.98 ± 0.38 |
| Total stent length in the main vessel (mm) | 31.8 ± 14.3 |
| Left guiding catheter (n = 96) | |
| EBU type catheter | 71 (74.0%) |
| Judkins left type catheter | 25 (26.0%) |
| Right guiding catheter (n = 18) | |
| Judkins right type catheter | 4 (22.2%) |
| Amplatz type catheter | 14 (77.8%) |
| Guiding catheter size | |
| 5-Fr | 3 (2.8%) |
| 6-Fr | 101 (95.3%) |
| 7-Fr | 2 (1.9%) |
| Variable | Total Patients (n = 106) |
|---|---|
| 30-day mortality | 0 |
| Any bleeding complication requiring surgery or transfusion | 0 |
| Access-site complication | |
| Distal radial artery occlusion | 0 |
| Forearm radial artery occlusion | 0 |
| Hand hematoma | 5 (4.7%) |
| ≤5 cm in diameter | 2 (1.9%) |
| >5 cm in diameter | 3 (2.8%) |
| Forearm hematoma | 0 |
| Study, Author Name (y of Publication) | No. of Patients | Mean Age (y) | Male Sex | Left DRA | Success Rate of the Puncture Site | PCI | Bifurcation | Success Rate of PCI | Cross-over in PCI | Distal RAO | Major Bleeding Requiring Transfusion or Surgery |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Kiemeneji et al. (2017) [5] | 70 | 68 ± 11 | 55 (79%) | 100% | 89% | 25 (36%) | N/A | N/A | 1 | 1 (1.5%) | 0 |
| Kim et al. (2018) [14] | 150 | 66 ± 13 | 94 (71%) | 100% | 88% | 42 (28%) | N/A | 97.6% | 1 | N/A | 0 |
| Lee et al. (2018) [16] | 200 | 66 ± 12 | 132 (66%) | 100% | 95.5% | 87 (44%) | 28/87 (32.2%) | 98.9% | 0 | 0 | 0 |
| Soydan et al. (2018) [12] | 54 | 59 ± 12 | 43 (80%) | 100% | 100% | 20 (37%) | N/A | N/A | 2 | 0 | 0 |
| Al-Azizi et al. (2018) [13] | 61 | 70 | 46 (75%) | 100% | 98.4 | 34 (56%) | N/A | N/A | 0 | 0 | 0 |
| Gasparini et al. (2019) [15] | 41 | 68 ± 5 | 31 (76%) | 100% | 82.9% | 100% | N/A | 78.1% | N/A | 1 (4.3%) | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, O.-H.; Roh, J.W.; Im, E.; Cho, D.-K.; Jeong, M.H.; Choi, D.; Kim, Y. Feasibility and Safety of the Left Distal Radial Approach in Percutaneous Coronary Intervention for Bifurcation Lesions. J. Clin. Med. 2021, 10, 2204. https://doi.org/10.3390/jcm10102204
Lee O-H, Roh JW, Im E, Cho D-K, Jeong MH, Choi D, Kim Y. Feasibility and Safety of the Left Distal Radial Approach in Percutaneous Coronary Intervention for Bifurcation Lesions. Journal of Clinical Medicine. 2021; 10(10):2204. https://doi.org/10.3390/jcm10102204
Chicago/Turabian StyleLee, Oh-Hyun, Ji Woong Roh, Eui Im, Deok-Kyu Cho, Myung Ho Jeong, Donghoon Choi, and Yongcheol Kim. 2021. "Feasibility and Safety of the Left Distal Radial Approach in Percutaneous Coronary Intervention for Bifurcation Lesions" Journal of Clinical Medicine 10, no. 10: 2204. https://doi.org/10.3390/jcm10102204
APA StyleLee, O.-H., Roh, J. W., Im, E., Cho, D.-K., Jeong, M. H., Choi, D., & Kim, Y. (2021). Feasibility and Safety of the Left Distal Radial Approach in Percutaneous Coronary Intervention for Bifurcation Lesions. Journal of Clinical Medicine, 10(10), 2204. https://doi.org/10.3390/jcm10102204