The Radiological Assessment of Root Features and Periodontal Structures in Endodontically Treated Teeth Subjected to Forces Generated by Fixed Orthodontic Appliances. A Prospective, Clinical Cohort Study
Abstract
:1. Introduction
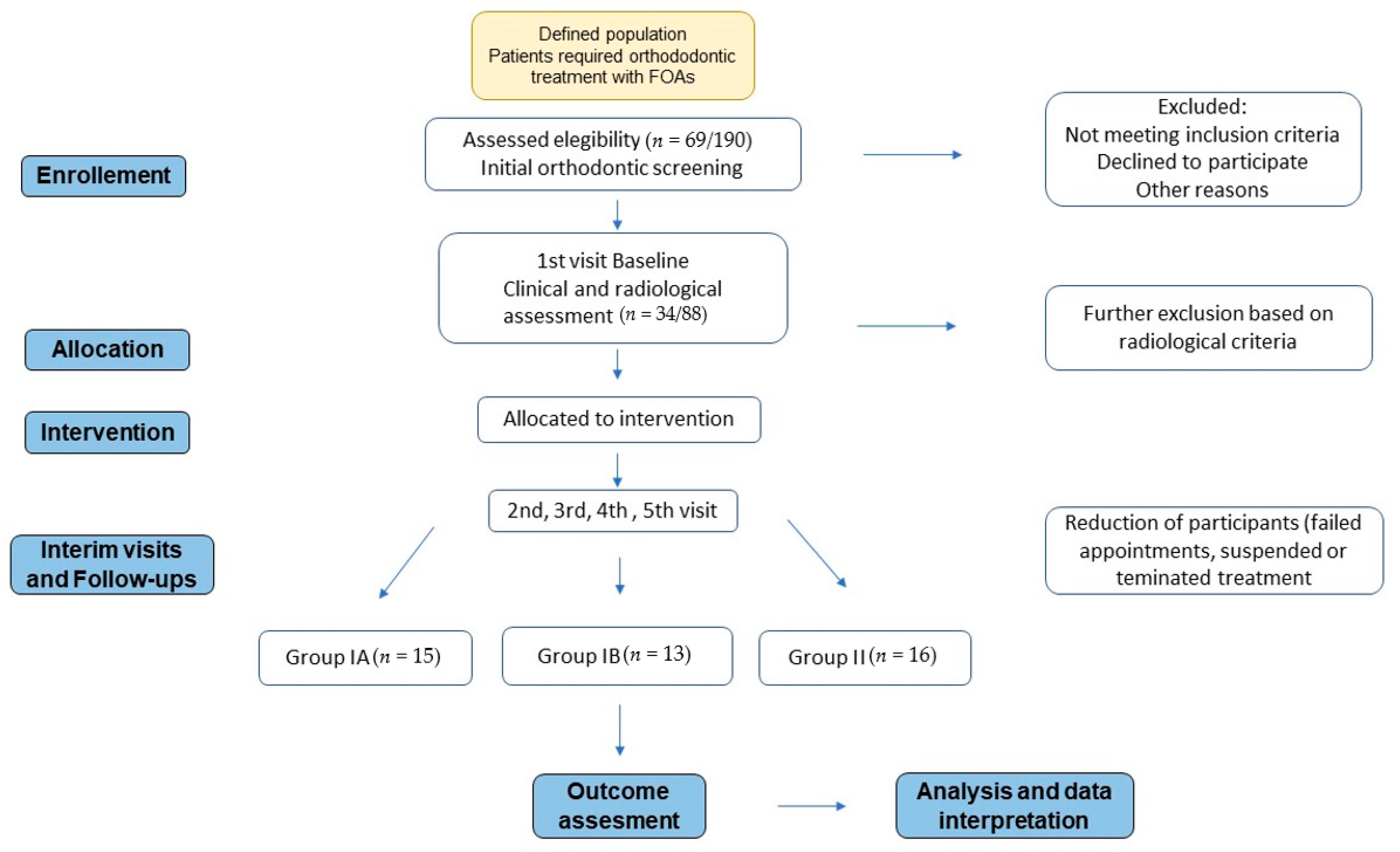
2. Materials and Methods
2.1. Cohort Selection and Sample Distribution
2.2. Eligibility Criteria
2.2.1. Inclusion Criteria
- Patients aged 16–40 treated with FOAs and had at least one endodontically treated tooth
- Good general systemic health, no underlying medical conditions, not on medications for chronic diseases or affecting bone/connective tissue structures
- No active periodontal diseases
- No removable prosthodontic appliances
- Optimal oral hygiene
- Valid informed written consent obtained as a compulsory requirement for participation in the study
2.2.2. Exclusion Criteria
- Patients with underlying chronic medical conditions, either acquired or congenital
- Pregnancy
- Patients with allergy to any dental material used
- Multiple missing posterior teeth
- Periodontal diseases
- Temporomandibular disorder and bruxism
- Oral mucosal diseases
- Persons who were not dentally fit before the orthodontic treatment
- Patients who have already been treated with the FOAs
- Poor oral hygiene
- Medications that can affect the efficiency and outcome of the orthodontic treatment: Bisphosphonates, steroids, calcium supplementation
- Unable to select a control, intact tooth
- Periapical index score above 1
2.2.3. Minimising Chance Error, Bias and Confounding
2.3. Orthodontic Treatment Protocol and Clinical Stages
- 022 MC Carriere MBT (metal)
- 022 Clarity S.L. MBT (cosmetic)
2.4. Radiographic Examination
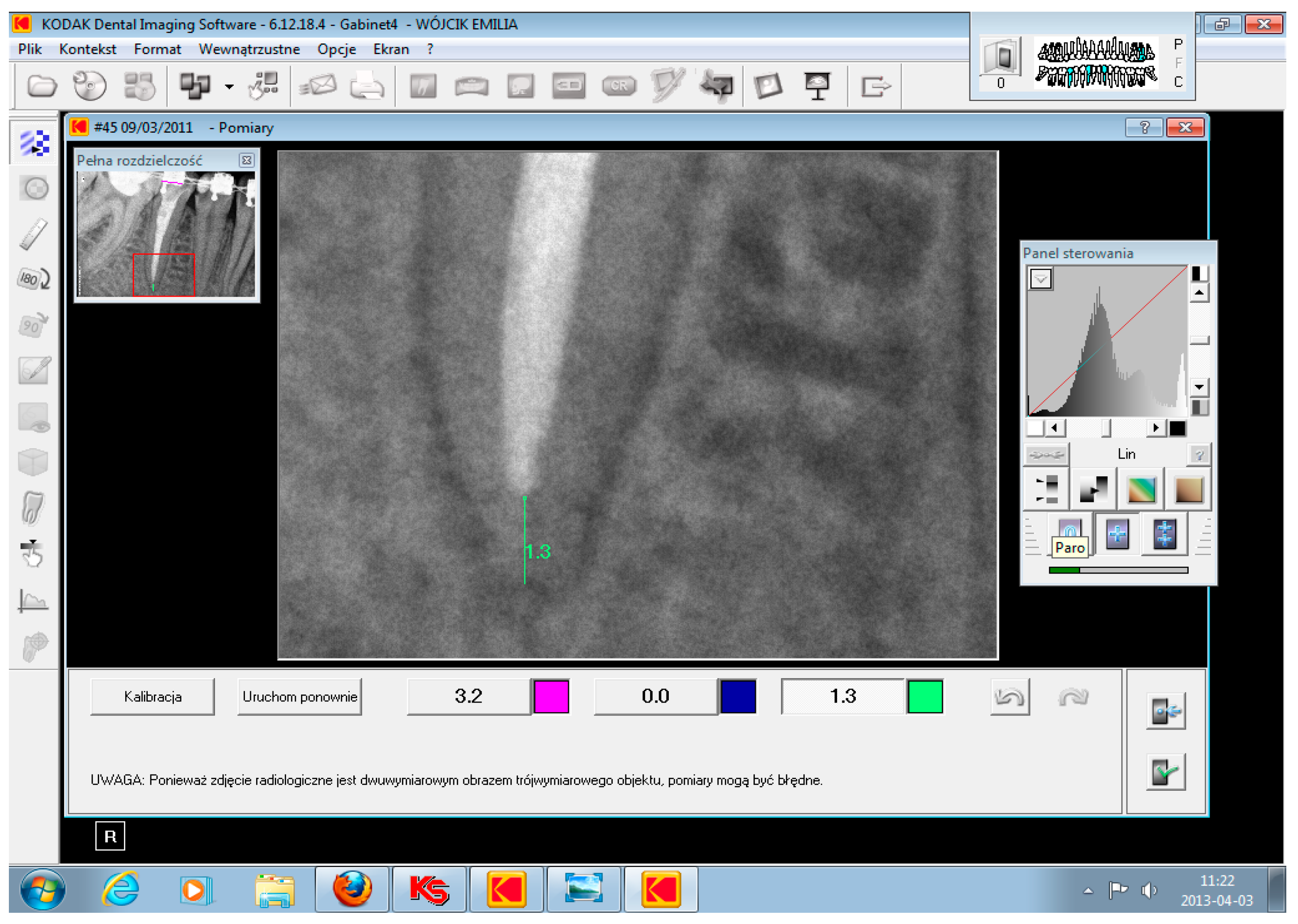
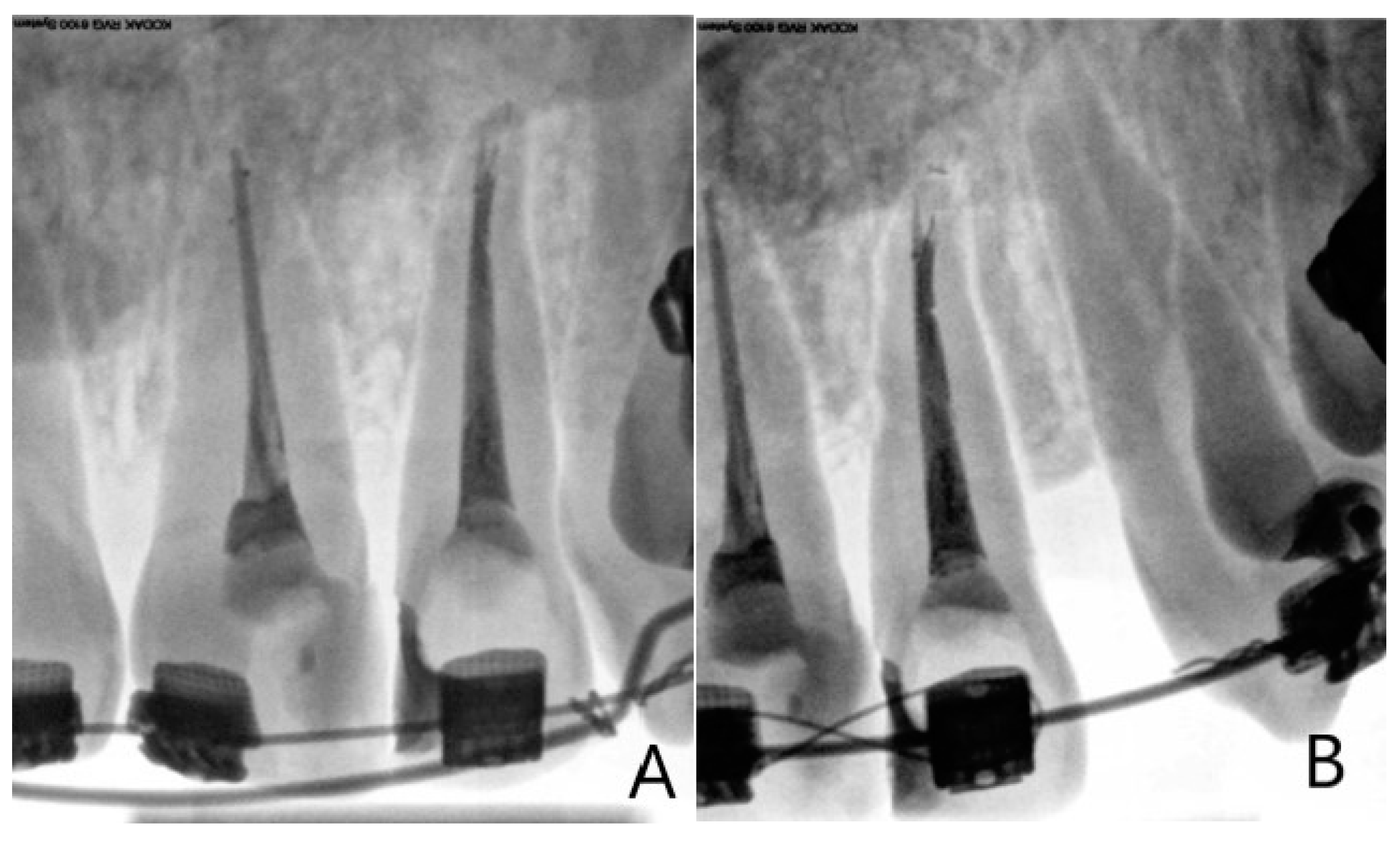
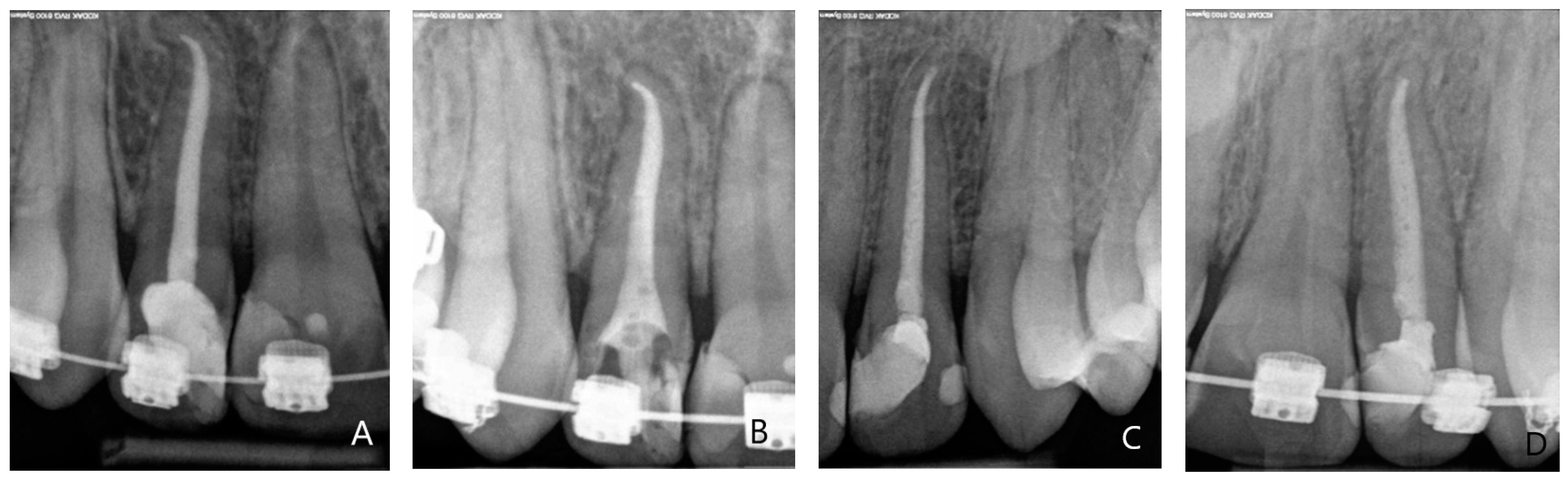
2.5. Analysis of the Intraoral Periapical Radiographs of Endodontically Treated Teeth
- The whole tooth structure was visible, from the root apex to the incisal/occlusal edge;
- The specific parameters of apical and periodontal elements taken into consideration during a radiological assessment of ETT were:
- apical range and homogeneity of root canal obturation (only for initial IPRs assessment to select/exclude cases);
- root’s radiological length (mm);
- periodontal space width (PAI scoring system, Ostravik criteria);
- shape and morphological profile of the root (Mirabella and Artun criteria);
- presence/absence of apical external root resorption (Levander and Malmgren criteria).
2.5.1. Apical Range and Homogeneity of Root Canal Obturation
2.5.2. Roots Radiological Length
2.5.3. Periapical Structures and Periodontal Ligament Space Assessment Periapical Index
2.5.4. Assessment of the Root Morphology
2.5.5. External Apical Root Resorption Assessment Levander and Malmgren Scale
- No changes in root shape or surface (no resorption, intact external outline)
- Irregular root contour/outline, root length has not yet been altered
- Minor root resorption apically, limited to maximum of 2 mm (<2 mm)
- Severe resorption from 2 mm to one-third, ¼ of the root length has been resorbed
- Extreme resorption, exceeding one-third of the original root length.
2.6. Statistical Analysis
3. Results
3.1. Participants and Material Characteristics
3.2. The Impact of Orthodontic Treatment Duration
3.3. Changes in Radiological Length of ETT
3.4. Changes of PDL Space Width in ETT
3.5. Morphological Profile of Root Apex
3.6. The Assessment of Root Apex Resorption Using the Lavender and Malmgren Scale
3.7. The Effect of the Application of Additional Orthodontic Forces Applied
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mah, R.; Holland, G.R.; Pechowih, E. Periapical changes after orthodontic movement of root-filled ferret canines. J. Endod. 1996, 22, 298–303. [Google Scholar] [CrossRef]
- Spurrier, S.W.; Hall, S.H.; Joondeph, D.R.; Shapiro, P.A. A comparison of apical root resorption during orthodontic treatment in endodontically treated and vital teeth. Am. J. Dentofac. Orthop. 1990, 97, 130–134. [Google Scholar] [CrossRef]
- Esteves, T.; Ramos, A.L.; Pereira, C.M. Orthodontic Root Resorption of Endodontically Treated Teeth. J. Endod. 2007, 33, 119–122. [Google Scholar] [CrossRef] [PubMed]
- Zachrisson, B.U.; Alnaes, L. Periodontal Condition in orthodontically treated and untreated individuals II. Alveolar bone loss: Radiographic findings. Angle Orthod. 1974, 44, 48–55. [Google Scholar] [PubMed]
- Wickwire, N.A.; McNell, M.H.; Norton, L.A. The Effect of Tooth Movement Upon Endodontically Treated Teeth. Angle Orthod. 1974, 44, 235–242. [Google Scholar] [PubMed]
- Mattison, G.D.; Delivanis, H.P.; Delivanis, P.D. Orthodontic root resorption of vital and endodontically treated teeth. J. Endod. 1984, 10, 354–358. [Google Scholar] [CrossRef]
- Hamilton, R.S.; Gutmann, J.L. Endodontic-orthodontic relationships: A review of integrated treatment planning challenges. Int. Endod. J. 1999, 32, 343–360. [Google Scholar] [CrossRef]
- Steadman, S.R. Resume of the literature on root resorption. Angle Orthod. 1942, 12, 283–286. [Google Scholar]
- Leach, H.A.; Ireland, A.J.; Whaites, E.J. Radiographic diagnosis of root resorption in relation to orthodontics. BDJ 2001, 13, 16–22. [Google Scholar] [CrossRef] [Green Version]
- Mirabella, A.D.; Artun, J. Prevalence and severity of apical root resorption of maxillary anterior teeth in adult orthodontic patients. Eur. J. Orthod. 1995, 17, 93–99. [Google Scholar] [CrossRef]
- Artun, J.; Hullenaar, R.V.; Doppel, D. Identification of orthodontic patients at risk of severe apical root resorption. AJODO 2009, 135, 448–455. [Google Scholar]
- Lee, Y.J.; Lee, T.Y. External root resorption during orthodontic treatment in root-filled teeth and contralateral teeth with vital pulp: A clinical study of contributing factors. Am. J. Orthod. Dentofacial Orthop. 2016, 149, 84–91. [Google Scholar] [CrossRef] [PubMed]
- Bender, I.B.; Byers, M.R.; Mori, K. Periapical replacement resorption of permanent, vital, endodontically treated incisors after orthodontic movement: Report of two cases. J. Endod. 1997, 23, 768–773. [Google Scholar] [CrossRef]
- Sampaio de Souza, R.; Gandini, L.G.; de Souza, V. Influence of orthodontic dental movement on the healing process of teeth with periapical lesions. J. Endod. 2006, 32, 115–119. [Google Scholar]
- Remington, D.N.; Joondeph, D.R.; Artun, J. Long term evaluation of root resorption occurring during orthodontic treatment. AJODO 1989, 96, 43–46. [Google Scholar] [CrossRef]
- Beck, V.J.; Stacknik, S.; Chandler, N.P.; Farella, M. Orthodontic tooth movement of traumatised or root-canal-treated teeth: A clinical review. N. Z. Dent. J. 2013, 109, 6–11. [Google Scholar] [PubMed]
- Nerwich, A.; Frigdor, D.; Messer, H.H. pH changes in root dentin over a 4-w eek period following root canal dressing with calcium hydroxide. J. Endod. 1993, 19, 302–306. [Google Scholar] [CrossRef]
- Mattion, G.D.; Gholston, I.R.; Boyd, P. Orthodontic external root resorption: Endodontic considerations. J. Endod. 1983, 9, 253–256. [Google Scholar] [CrossRef]
- Kindelan, S.A.; Day, P.F.; Kindelan, J.D. Dental trauma: An overview of its influence on the management of orthodontic treatment. Part 1. J. Orthod. 2008, 35, 68–78. [Google Scholar] [CrossRef]
- Khan, A.R.; Fida, M.; Shaikh, A. Evaluation of Apical Root Resorption in Endodontically Treated and Vital Teeth in Adult Orthodontic Subjects. J. Ayub. Med. Coll. Abbottabad 2018, 30, 506–510. [Google Scholar]
- Kucukkeles, N.; Acar, A.; Biren, S.; Arun, T. Comparisons between cervical vertebrae and hand-wrist maturation for the assessment of skeletal maturity. J. Clin. Pediatr. Dent. 1999, 1, 47–52. [Google Scholar]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ 2007, 335, 806–808. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Altman, D.G.; Simera, I.; Hoey, J.; Moher, D.; Schulz, K. EQUATOR: Reporting guidelines for health research. Lancet 2008, 371, 1149–1150. [Google Scholar] [CrossRef] [Green Version]
- Mortazavi, H.; Baharvand, M. Review of common conditions associated with periodontal ligament widening. Imaging Sci. Dent. 2016, 46, 229–237. [Google Scholar] [CrossRef] [Green Version]
- Dudic, A.; Giannopoulou, K.; Leuzinger, M. Detection of apical root resorption after orthodontic treatment by using panoramic radiography and cone-beam computed tomography of super-high resolution. AJODO 2009, 135, 434–437. [Google Scholar] [CrossRef] [PubMed]
- Martínez Beneyto, Y.; Alcaráz Banos, M.; Pérez Lajarin, L.; Rushton, V.E. Clinical justification of dental radiology in adult patients: A review of the literature. Med. Oral Patol. Oral Cir. Bucal 2007, 12, E244–E251. [Google Scholar]
- Janson, G.R.P.; de Luca Canto, G.; Martinez, D.R. A radiographic comparison of apical root resorption after orthodontic treatment with 3 different fixed appliance techniques. AJODO 1999, 118, 262–273. [Google Scholar] [CrossRef]
- Lindskog, S.; Blomlof, L.; Hammarstrom, L. Evidence of a role of odontogenic epithelium in maintaining the periodontal space. J. Clin. Periodontol. 1988, 15, 371–373. [Google Scholar] [CrossRef]
- Huumonen, S.; Ostravik, D. Radiological aspects of apical periodontitis. Endod. Top. 2002, 1, 3–25. [Google Scholar] [CrossRef]
- Deane, S.; Jones, A.S.; Petocz, P. Physical properties of root cementum: Part 12. The incidence of physiologic root resorption on unerupted third premolars and its comparison with orthodontically treated premolars: A microcomputed-tomography study. AJODO 2009, 136, 148.e1–148.e9. [Google Scholar] [CrossRef]
- Smale, I.; Artun, J.; Behbehani, F. Apical root resorption 6 months after initiation of fixed orthodontic appliance therapy. AJODO 2005, 128, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Lavander, E.; Bajka, R.; Malmgren, O. Early radiographic sign of apical root resorption during orthodontic treatment: A study of maxillary incisors. Eur. J. Orthod. 1998, 20, 57–63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sameshima, G.T.; Sinclair, P.M. Predicting and preventing root resorption: Part II. Diagnostic factors. Am. J. Orthod. Dentofac. Orthop. 2002, 119, 505–510. [Google Scholar] [CrossRef] [PubMed]
- Konopka, E.; Matthews-Brzozowska, T. Metodyka pomiarów resorpcji wierzchołkowej korzeni zębów—Przegląd piśmiennictwa. Dent. Forum 2010, 38, 87–89. [Google Scholar]
- Gonzales, C.; Hotokezaka, H.; Yoshimatsu, M. Force Magnitude and Duration Effects on Amount of Tooth Movement and Root Resorption in the Rat Molar. Angle Orthod. 2008, 78, 502–509. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paetyangkul, A.; Turk, T.; Elekdag-Turk, S. Physical Properties of root cementum: Part 14. The amount of root resorption after force application for 12 weeks on maxillary and mandibular premolars: A microcomputed-tomography study. AJODO 2009, 136, 492.e1–492.e9. [Google Scholar] [CrossRef] [PubMed]
- Cheng, L.L.; Turk, T.; Elekdag-Turk, S. Physical properties of root cementum: Part 13. Repair of root resorption 4 and 8 weeks after the application of continuous light and heavy forces for 4 weeks: A microcomputed-tomography study. AJODO 2009, 136, 320.e1–320.e10. [Google Scholar] [CrossRef] [PubMed]
- Van Leeuwen, E.J.; Kuijpers-Jagtman, A.M.; Von den Hoff, J.W.; Wagener, F.A.; Maltha, J.C. Rate of orthodontic tooth movement after changing the force magnitude: An experimental study in beagle dogs. Orthod. Craniofac. Res. 2010, 13, 238–245. [Google Scholar] [CrossRef]
- Ren, Y.; Maltha, J.C.; Liem, R. Age-dependent external root resorption during tooth movement in rats. Acta Odontol. Scand. 2008, 66, 93–98. [Google Scholar] [CrossRef]
- Dudic, A.; Giannopoulou, K.; Martinz, M. Diagnostic accuracy of digitized periapical radiographs validated against micro-computed tomography scanning in evaluating orthodontically induced apical root resorption. Eur. J. Oral Sci. 2008, 116, 467–472. [Google Scholar] [CrossRef]
- Ballard, D.J.; Jones, A.S.; Petocz, P. Physical properties of root cementum: Part 11. Continuous vs intermittent controlled orthodontic forces on root resorption. A microcomputed—Tomography study. AJODO 2009, 136, 8.e1–8.e8. [Google Scholar] [CrossRef] [PubMed]
- Maltha, J.C.; Leeuwen, E.J.; Dijkman, G.E. Incidence and severity of root resorption in orthodontically moved premolars in dogs. Orthod. Craniofacial Res. 2004, 7, 115–121. [Google Scholar] [CrossRef]
- Wierzbicki, T.; El-Bialy, T.; Aldaghreer, S. Analysis of Orthodontically Induced Tooth Resorption Using Micro-Computed Tomography (Micro-CT). Angle Orthod. 2009, 79, 91–96. [Google Scholar] [CrossRef]
- Owman-Moll, P.; Kurol, J.; Lundgren, D. Continuous versus interrupted continuous orthodontic force related to early tooth movement and root resorption. Angle Orthod. 1995, 65, 395–402. [Google Scholar]
- Linge, L.; Linge, B.O. Patient characteristics and treatment variables associated with apical root resorption during orthodontic treatment. AJODO 1991, 99, 35–43. [Google Scholar] [CrossRef]
- Sringkarnboriboon, S.; Matsumoto, Y.; Soma, K. Root Resorption Related to Hypofunctional Periodontium in Experimental Tooth Movement. J. Dent. Res. 2003, 82, 486–490. [Google Scholar] [CrossRef] [PubMed]
- Santos, S.M.C.; Soares, J.A.; Costa, G.M. Radiographic Parameters of Quality of Root Canal Fillings and Periapical Status: A Retrospective Cohort Study. J. Endod. 2010, 36, 1932–1937. [Google Scholar] [CrossRef]
- Tondelli, P.M.; Mendonca, M.R.; Pereira, A.L.P. Knowledge on dental trauma and orthodontic tooth movement held by a group of orthodontists. Braz. Oral Res. 2010, 24, 76–82. [Google Scholar] [CrossRef] [Green Version]
- Igarashi, K.; Adachi, H.; Mitani, H.; Shinoda, H. Inhibitory effect of the topical administration of Bisphodphonate (Risedronate) on root resorption incident to orthodontic tooth movement in rats. J. Dent. Res. 1996, 75, 1644–1649. [Google Scholar]
- Barbagallo, L.J.; Jones, A.S.; Petocz, P. Physical properties of root cementum: Part 10. Comparison of the effects of invisible removable thermoplastic appliances with light and heavy orthodontic forces on premolar cementum. A microcomputed-tomography study. AJODO 2008, 133, 218–227. [Google Scholar] [CrossRef]
- Parker, R.J.; Harris, E.F. Directions of orthodontic tooth movements associated with external apical root resorption of maxillary central incisor. AJODO 1998, 114, 677–683. [Google Scholar] [CrossRef]
- Ioannidou-Marathiotou, I.; Zafeiriadis, A.A.; Papadopoulos, M.A. Root resorption of endodontically treated teeth following orthodontic treatment: A meta-analysis. Clin. Oral Investig. 2013, 17, 1733–1744. [Google Scholar] [CrossRef] [PubMed]
- Pizzo, G.; Licata, M.E.; Guiglia, R.; Giuliana, G. Root resorption and orthodontic treatment. Review of the literature. Minerva Stomatol. 2007, 56, 31–44. [Google Scholar] [PubMed]
- Beck, B.W.; Harris, E.F. Apical root resorption in orthodontically treated subjects: Analysis of edgewise and light wire mechanics. AJODO 1994, 105, 350–361. [Google Scholar] [CrossRef]
- Harris, E.; Baker, W.C. Loss of root length and crystal bone height before and during treatment in adolescent and adult orthodontic patients. AJODO 1990, 98, 463–469. [Google Scholar]
- Mohandesan, H.; Ravanmehr, H.; Valaei, N. A radiographic analysis of external apical root resorption of maxillary incisors during active orthodontic treatment. Eur. J. Orthod. 2007, 29, 134–139. [Google Scholar] [CrossRef] [PubMed] [Green Version]




| Group | Description and Details | |
|---|---|---|
| I | A | Asymptomatic teeth without periapical pathologies, endodontically treated according to ESE guidelines Radiologically scored using the ESE criteria (4–6 points) Orthodontic treatment started 0–6 months after the endodontic treatment was completed |
| B | Asymptomatic teeth with no periapical pathologies, endodontically treated according to the modern ESE guidelines Radiologically scored using ESE criteria 4–6 points. Orthodontic treatment started 6 months after the endodontic treatment was completed | |
| IA + IB | Asymptomatic teeth without periapical lesions, endodontically treated using modern endodontics Radiologically scored using ESE endodontic criteria: 4–6 points | |
| II | Asymptomatic teeth without periapical pathologies, treated with conventional endodontic methods | |
| III | Asymptomatic, control, intact teeth at the same patients as the one fter endodontic treatment, Corresponding teeth, same anatomical group on the opposite site in the same dental arch | |
| Stage of the Study | Clinical Stage | Description | |
|---|---|---|---|
| 1 | I | Orthodontic consultation | Dental and medical history Extra and intraoral examination Functional examination Analysis of the facial features (photo) Dental impressions for the diagnostic models |
| 2 | Orthodontic treatment plan | Analysis of diagnostic models and photos Analysis of extraoral radiographs: Orthopantomogram and teleradiography Orthodontic treatment plan set up | |
| 3 | Selection of patients | Assessment of intraoral periapical radiographs of endodontically treated teeth Assessment of oral health status and systemic health of the patients included Assessment of control tooth status | |
| 4 | II | Endodontic treatment | Performed following ESE standards |
| 5 | III | Orthodontic treatment | Fitting of the fixed orthodontic appliance Regular follow-ups and recalls |
| 6 | IV | Regular review of teeth selected for the study | Clinical and radiological assessment performed during five review appointments |
| 7 | Verification of the investigated group | Assessment of the quality of intraoral periapical radiographs Elimination of teeth not fulfilling the criteria | |
| 8 | V | Data analysis, results validation, conclusions | Statistical analysis of the obtained data Discussion of the results, Conclusions |
| Group | Initial Number of Patients | Initial Number of Teeth | Final Number of Patients | Final Number of Teeth |
|---|---|---|---|---|
| IA | 69 | 95 | 34 | 15 |
| IB | 13 | |||
| II | 16 | |||
| III | 95 | 44 |
| Visit | Group IA + IB Median (Min–Max) {Quartile Lower Upper} | Group II Median (Min–Max) {Quartile Lower Upper} | Mann-Whitney Test (p) | |
|---|---|---|---|---|
| 2nd | 0.2 (0−3.8) {0.05−0.4} | 0.1 (0−1.2) {0−0.35} | 0.4642 | |
| 3rd | 0.3 (0−3.6) {0.05−0.8} | 0.35 (0−1.2) {0.05−0.7} | 0.9611 | |
| 4th | 0.3 (0−3.5) {0−1.2} | 0.3 (0−2.2) {0.1−0.9} | 0.7053 | |
| 5thANOVA Friedman (p) | 0.2 (0−3.5) {0−1.3} 0.1771 | 0.4 (0−2) {0.1−1.2} 0.0276 * | 0.5664 | |
| Comparison between next visits Wilcoxon test | 2nd 3rd | _____ | P = 0.0446 * | |
| 3rd 4th | _____ | P = 0.4326 | ||
| 4th 5th | _____ | P = 0.8753 | ||
| Group | 1st app. | 2nd app. | 3rd app. | 4th app. | 5th app. | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PAI | PAI | PAI | PAI | PAI | ||||||||||
| 1 | 1 | 2 | 3 | 1 | 2 | 3 | 1 | 2 | 3 | 1 | 2 | 3 | ||
| IA + IB | 28 | 28 | 11 | 16 | 1 | 8 | 15 | 5 | 9 | 15 | 4 | 14 | 13 | 1 |
| 100% | 39% | 57.4% | 3.6% | 28% | 54% | 18% | 32% | 54% | 14% | 50% | 46.4% | 3.6% | ||
| II | 16 | 16 | 10 | 5 | 1 | 5 | 9 | 2 | 4 | 10 | 2 | 9 | 7 | 0 |
| 100% | 62% | 31.7% | 6.3% | 31% | 56% | 13% | 25% | 62% | 13% | 56% | 44% | 0% | ||
| Changes in PDL Space: PAI ≥ 2 | ||
|---|---|---|
| Appointment | IA + IB (n = 28) | II (n = 16) |
| 1st | 0% | 0% |
| 2nd | 61% | 37% |
| 3rd | 71% | 69% |
| 4th | 68% | 75% |
| 5th | 50% | 44% |
| Q Cochrane (p) test | <0.0001 | <0.0001 |
| Group | Number of Teeth | 1st app. | 2nd app. | 3rd app. | 4th app. | 5th app. |
|---|---|---|---|---|---|---|
| Number of Teeth with EARR | ||||||
| IA + IB | 28 | 0 | 3 | 6 | 6 | 6 |
| II | 16 | 0 | 1 | 4 | 4 | 4 |
| Group | Number of Teeth with EARR | Characteristics | Last Appointment (5th) Status of the Root | ||||
|---|---|---|---|---|---|---|---|
| Duration of Treatment (Months) | Shape of the Root | Additional Appliances | Tooth | EARR Grade | |||
| IA + IB | 6 | 36 | Tśr = 21.4 | n | yes | 11 | 3 |
| 30 | n | yes | 22 | 2 | |||
| 26 | F | yes | 11 | 2 | |||
| 20 | C | yes | 12 | 2 | |||
| 20 | C | yes | 22 | 3 | |||
| 19 | n | yes | 21 | 2 | |||
| II | 5 | 18 | n | no | 35 | 1 | |
| 30 | n | yes | 21 | 2 | |||
| 24 | F | yes | 11 | 1 | |||
| 26 | F | no | 11 | 2 | |||
| Appointment | EARR Scale | Group | Test Ch | |
|---|---|---|---|---|
| IA + IB (n = 28) | II (n = 16) | |||
| 2nd | 0 | 89.5% | 94% | 0.7305 |
| 1 | 3.5% | 0% | ||
| 2 | 3.5% | 6% | ||
| 3 | 3.5% | 0% | ||
| 3rd | 0 | 79 % | 75% | 0.3956 |
| 1 | 3.5% | 19% | ||
| 2 | 14% | 6% | ||
| 3 | 3.5% | 0% | ||
| 4th | 0 | 79% | 75% | 0.6358 |
| 1 | 0% | 12.5% | ||
| 2 | 14% | 12.5% | ||
| 3 | 7% | 0% | ||
| 5th | 0 | 79% | 75% | 0.6358 |
| 1 | 0% | 12.5% | ||
| 2 | 14% | 12.5% | ||
| 3 | 7% | 0% | ||
| Appointment | EARR Score | Additional Orthodontic Forces | Test Ch Yatesa | |
|---|---|---|---|---|
| YES (n = 20) | NO (n = 24) | |||
| 2nd | 0 | 80% | 100% | 0.0765 |
| >1 | 20% | 0% | ||
| 3rd | 0 | 60% | 92% | 0.0328 |
| >1 | 40% | 8% | ||
| 4th | 0 | 60% | 92% | 0.0328 |
| >1 | 40% | 8% | ||
| 5th | 0 | 60% | 92% | 0.0328 |
| >1 | 40% | 8% | ||
| PDL Space width-PAI Index | |||||
|---|---|---|---|---|---|
| Appointment | Additional Forces | PAI = 1 | PAI = 2 | PAI = 3 | p |
| 2nd | NO | 62.5% | 37.5% | 0% | 0.0473 |
| YES | 30% | 60% | 10% | ||
| 3rd | NO | 42% | 58% | 0% | 0.0068 |
| YES | 15% | 50% | 35% | ||
| 4th | NO | 42% | 54% | 4% | 0.0632 |
| YES | 15% | 60% | 25% | ||
| 5th | NO | 58% | 42% | 0% | 0.5460 |
| YES | 45% | 50% | 5% | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pustułka, K.; Trzcionka, A.; Dziedzic, A.; Skaba, D.; Tanasiewicz, M. The Radiological Assessment of Root Features and Periodontal Structures in Endodontically Treated Teeth Subjected to Forces Generated by Fixed Orthodontic Appliances. A Prospective, Clinical Cohort Study. J. Clin. Med. 2021, 10, 2078. https://doi.org/10.3390/jcm10102078
Pustułka K, Trzcionka A, Dziedzic A, Skaba D, Tanasiewicz M. The Radiological Assessment of Root Features and Periodontal Structures in Endodontically Treated Teeth Subjected to Forces Generated by Fixed Orthodontic Appliances. A Prospective, Clinical Cohort Study. Journal of Clinical Medicine. 2021; 10(10):2078. https://doi.org/10.3390/jcm10102078
Chicago/Turabian StylePustułka, Katarzyna, Agata Trzcionka, Arkadiusz Dziedzic, Dariusz Skaba, and Marta Tanasiewicz. 2021. "The Radiological Assessment of Root Features and Periodontal Structures in Endodontically Treated Teeth Subjected to Forces Generated by Fixed Orthodontic Appliances. A Prospective, Clinical Cohort Study" Journal of Clinical Medicine 10, no. 10: 2078. https://doi.org/10.3390/jcm10102078
APA StylePustułka, K., Trzcionka, A., Dziedzic, A., Skaba, D., & Tanasiewicz, M. (2021). The Radiological Assessment of Root Features and Periodontal Structures in Endodontically Treated Teeth Subjected to Forces Generated by Fixed Orthodontic Appliances. A Prospective, Clinical Cohort Study. Journal of Clinical Medicine, 10(10), 2078. https://doi.org/10.3390/jcm10102078







