Development and Investigation of a New Polysulfone Dialyzer with Increased Membrane Hydrophilicity
Abstract
:1. Introduction
2. Development of a New Dialyzer
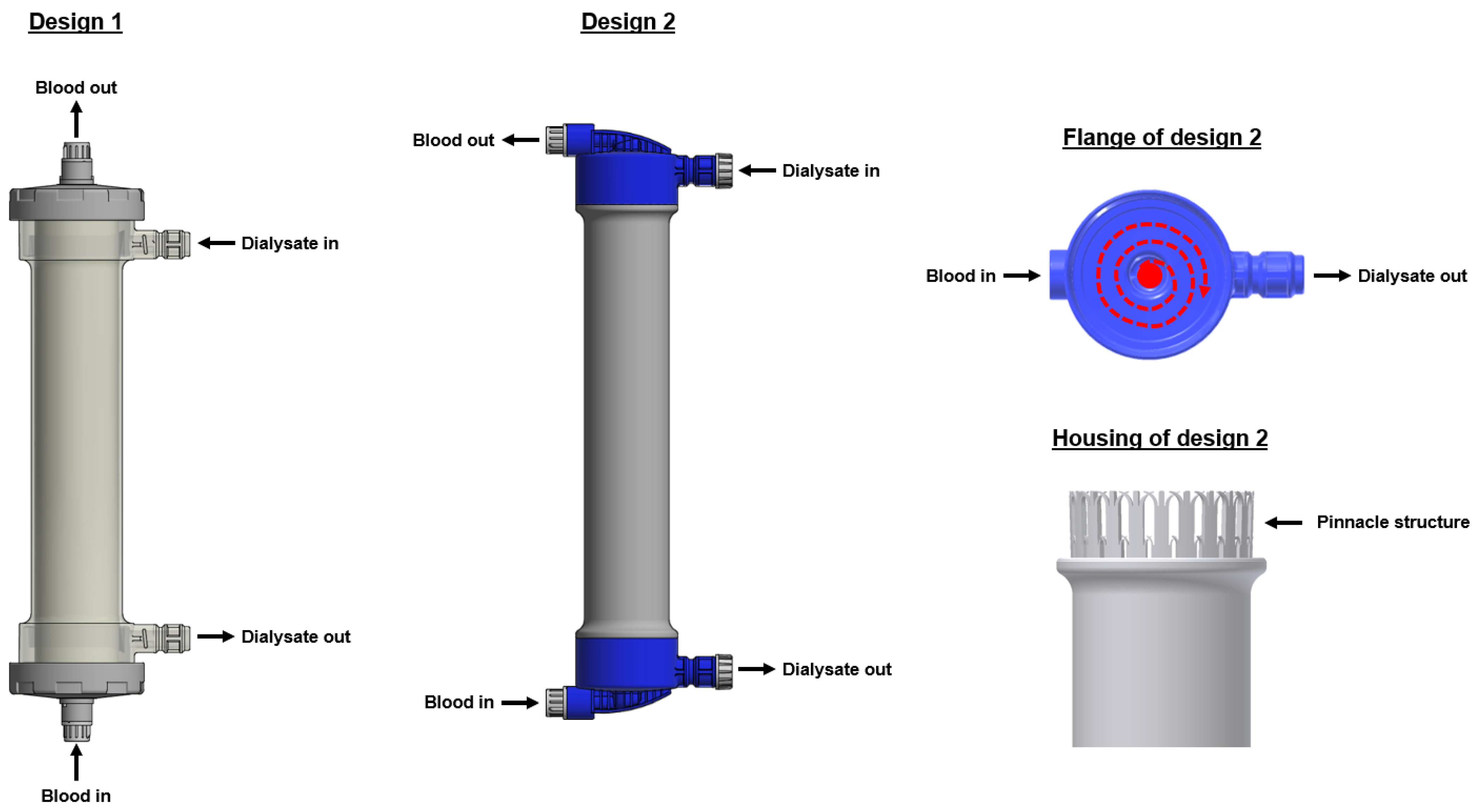
2.1. Outer Dialyzer Design
2.2. Dialyzer Membrane
3. Investigation of a New Dialyzer
3.1. Membrane Characterization
3.1.1. Characterization of PVP Content and Elution
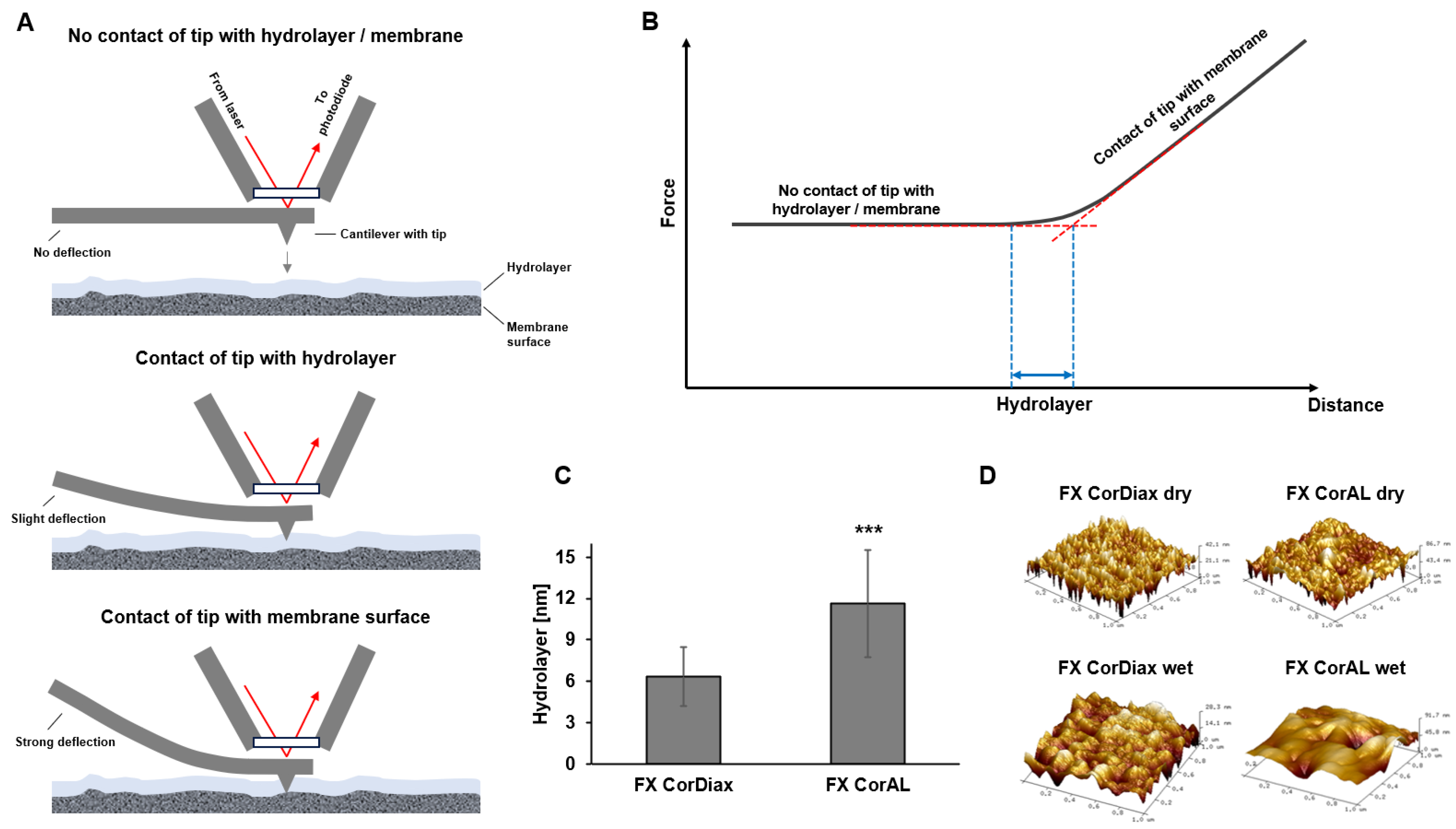
3.1.2. Characterization of Membrane Hydrophilicity
3.1.3. Characterization of Membrane Fouling
3.2. In Vitro and Clinical Investigation of Performance, Hemocompatibility and Safety
3.2.1. Overview of In Vitro and Clinical Studies with the New Polysulfone Dialyzer
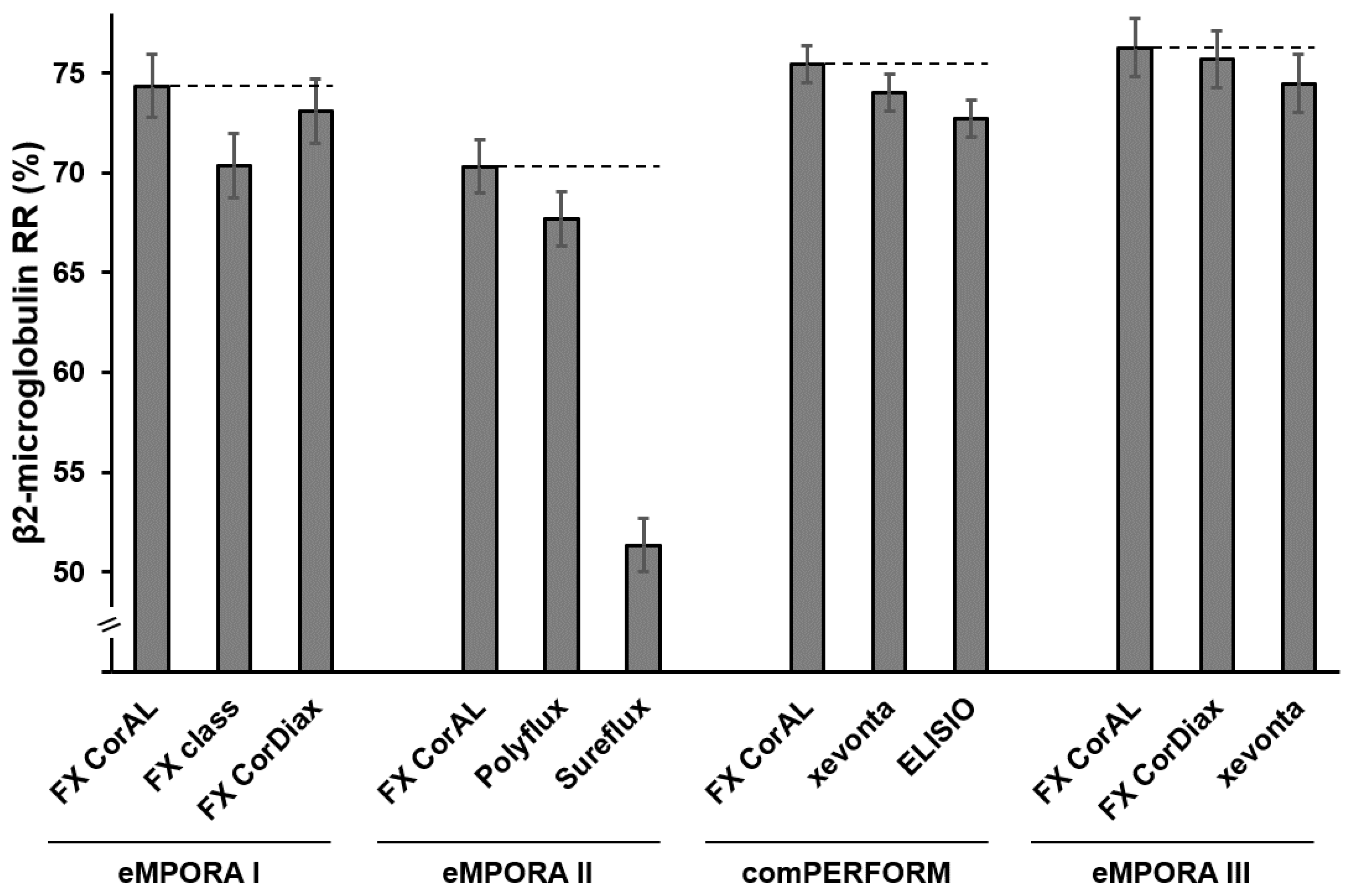
3.2.2. Investigation of Performance
Importance of a High-Performing Dialyzer
Investigation of Performance in In Vitro Studies
Investigation of Performance in Clinical Studies
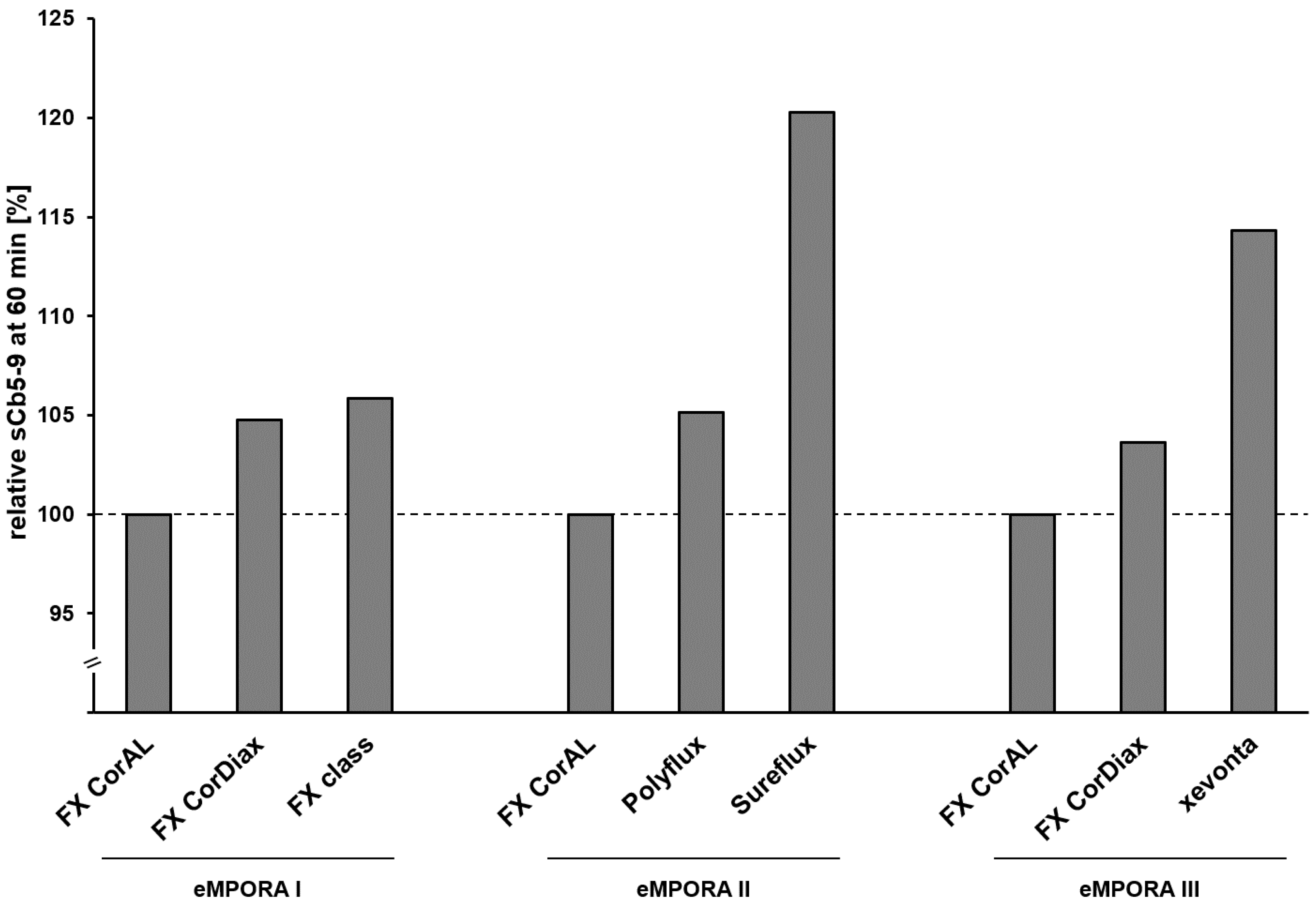
3.2.3. Investigation of Hemocompatibility
Importance of a Hemocompatible Dialyzer
- Complement activation
- 2.
- Platelet activation and coagulation
- 3.
- Cell activation, inflammation and oxidative stress
Investigation of Hemocompatibility in In Vitro Studies
Investigation of Hemocompatibility in Clinical Studies
3.2.4. Investigation of Safety
Investigation of Safety in Clinical Studies
Investigation of Safety in FX CorAL Studies
- Safety population and methodology
- 2.
- ADE Types and Frequency
- 3.
- FX CorAL safety profile
4. Conclusions and Future Directions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ADE | Adverse device effects |
| AE | Adverse event |
| AFM | Atomic force microscopy |
| AUC | Area under the curve |
| BMI | Body mass index |
| β2-m | β2-microglobulin |
| β-TG | β-Thromboglobulin |
| C3a | Complement factor C3a |
| C5a | Complement factor C5a |
| ESKD | End-stage kidney disease |
| GSH-Px | Glutathione peroxidase |
| HDF | Hemodiafiltration |
| hsCRP | High-sensitivity C-reactive protein |
| IL-6 | Interleukin 6 |
| IL-8 | Interleukin 8 |
| LTB4 | Leukotriene B4 |
| MDA | Malondialdehyde |
| MWCO | Molecular weight cut-off |
| MWRO | Molecular weight retention onset |
| nsAE | Non-serious adverse event |
| PMMA | Polymethylmethacrylate |
| PMN elastase | Polymorphonuclear elastase |
| PRO | Patient reported outcomes |
| PVP | Polyvinylpyrrolidone |
| RR | Removal rate |
| RRT | Renal replacement therapy |
| SAE | Serious adverse event |
| sC5b-9 | Complement factor sC5b-9 |
| sICAM-1 | Soluble intercellular adhesion molecule 1 |
| TAT | Thrombin-antithrombin |
| TMP | Transmembrane pressure |
| TxB2 | Thromboxane B2 |
| XPS | X-ray photoelectron spectroscopy |
References
- Saran, R.; Robinson, B.; Abbott, K.C.; Bragg-Gresham, J.; Chen, X.; Gipson, D.; Gu, H.; Hirth, R.A.; Hutton, D.; Jin, Y.; et al. US Renal Data System 2019 Annual Data Report: Epidemiology of Kidney Disease in the United States. Am. J. Kidney Dis. 2020, 75, A6–A7. [Google Scholar] [CrossRef] [PubMed]
- Thurlow, J.S.; Joshi, M.; Yan, G.; Norris, K.C.; Agodoa, L.Y.; Yuan, C.M.; Nee, R. Global Epidemiology of End-Stage Kidney Disease and Disparities in Kidney Replacement Therapy. Am. J. Nephrol. 2021, 52, 98–107. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.C.; Kim, J.H.; Sung, J.; Kim, H.-C.; Kang, E.; Lee, S.H.; Kim, J.K.; Kim, H.C.; Min, B.G.; Ronco, C. Effects of Arterial Port Design on Blood Flow Distribution in Hemodialyzers. Blood Purif. 2009, 28, 260–267. [Google Scholar] [CrossRef] [PubMed]
- Kulz, M. In Vitro and in Vivo Evaluation of a New Dialyzer. Nephrol. Dial. Transplant. 2002, 17, 1475–1479. [Google Scholar] [CrossRef]
- Ronco, C.; Bowry, S.K.; Brendolan, A.; Crepaldi, C.; Soffiati, G.; Fortunato, A.; Bordoni, V.; Granziero, A.; Torsello, G.; La Greca, G. Hemodialyzer: From Macro-Design to Membrane Nanostructure; the Case of the FX-Class of Hemodialyzers. Kidney Int. Suppl. 2002, 61, S126–S142. [Google Scholar] [CrossRef]
- Said, N.; Lau, W.J.; Ho, Y.-C.; Lim, S.K.; Zainol Abidin, M.N.; Ismail, A.F. A Review of Commercial Developments and Recent Laboratory Research of Dialyzers and Membranes for Hemodialysis Application. Membranes 2021, 11, 767. [Google Scholar] [CrossRef]
- Lang, T.; Zawada, A.M.; Theis, L.; Braun, J.; Ottillinger, B.; Kopperschmidt, P.; Gagel, A.; Kotanko, P.; Stauss-Grabo, M.; Kennedy, J.P.; et al. Hemodiafiltration: Technical and Medical Insights. Bioengineering 2023, 10, 145. [Google Scholar] [CrossRef]
- Bowry, S.K. Dialysis Membranes Today. Int. J. Artif. Organs 2002, 25, 447–460. [Google Scholar] [CrossRef]
- Ronco, C.; Clark, W.R. Haemodialysis Membranes. Nat. Rev. Nephrol. 2018, 14, 394–410. [Google Scholar] [CrossRef]
- Zawada, A.M.; Lang, T.; Ottillinger, B.; Kircelli, F.; Stauss-Grabo, M.; Kennedy, J.P. Impact of Hydrophilic Modification of Synthetic Dialysis Membranes on Hemocompatibility and Performance. Membranes 2022, 12, 932. [Google Scholar] [CrossRef]
- Zawada, A.M.; Emal, K.; Förster, E.; Saremi, S.; Delinski, D.; Theis, L.; Küng, F.; Xie, W.; Werner, J.; Stauss-Grabo, M.; et al. Hydrophilic Modification of Dialysis Membranes Sustains Middle Molecule Removal and Filtration Characteristics. Membranes 2024, 14, 83. [Google Scholar] [CrossRef]
- Zawada, A.M.; Melchior, P.; Schall, C.; Erlenkötter, A.; Lang, T.; Keller, T.; Stauss-Grabo, M.; Kennedy, J.P. Time-resolving Characterization of Molecular Weight Retention Changes among Three Synthetic High-flux Dialyzers. Artif. Organs 2022, 46, 1318–1327. [Google Scholar] [CrossRef] [PubMed]
- Zawada, A.M.; Melchior, P.; Erlenkötter, A.; Delinski, D.; Stauss-Grabo, M.; Kennedy, J.P. Polyvinylpyrrolidone in Hemodialysis Membranes: Impact on Platelet Loss during Hemodialysis. Hemodial. Int. 2021, 25, 498–506. [Google Scholar] [CrossRef]
- Melchior, P.; Erlenkötter, A.; Zawada, A.M.; Delinski, D.; Schall, C.; Stauss-Grabo, M.; Kennedy, J.P. Complement Activation by Dialysis Membranes and Its Association with Secondary Membrane Formation and Surface Charge. Artif. Organs 2021, 45, 770–778. [Google Scholar] [CrossRef] [PubMed]
- Hayama, M. Nanoscopic Behavior of Polyvinylpyrrolidone Particles on Polysulfone/Polyvinylpyrrolidone Film. Biomaterials 2004, 25, 1019–1028. [Google Scholar] [CrossRef]
- Zhu, L.; Song, H.; Wang, J.; Xue, L. Polysulfone Hemodiafiltration Membranes with Enhanced Anti-Fouling and Hemocompatibility Modified by Poly(Vinyl Pyrrolidone) via in Situ Cross-Linked Polymerization. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 74, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.; Zhu, L.; Zhu, L.; Zhang, H.; Zhu, B.; Xu, Y. Antifouling and Antimicrobial Polymer Membranes Based on Bioinspired Polydopamine and Strong Hydrogen-Bonded Poly (N-Vinyl Pyrrolidone). ACS Appl. Mater. Interfaces 2013, 5, 12895–12904. [Google Scholar] [CrossRef]
- Ran, F.; Nie, S.; Zhao, W.; Li, J.; Su, B.; Sun, S.; Zhao, C. Biocompatibility of Modified Polyethersulfone Membranes by Blending an Amphiphilic Triblock Co-Polymer of Poly(Vinyl Pyrrolidone)-b-Poly(Methyl Methacrylate)-b-Poly(Vinyl Pyrrolidone). Acta Biomater. 2011, 7, 3370–3381. [Google Scholar] [CrossRef]
- Hayama, M.; Yamamoto, K.; Kohori, F.; Sakai, K. How Polysulfone Dialysis Membranes Containing Polyvinylpyrrolidone Achieve Excellent Biocompatibility? J. Membr. Sci. 2004, 234, 41–49. [Google Scholar] [CrossRef]
- Wang, H.; Yu, T.; Zhao, C.; Du, Q. Improvement of Hydrophilicity and Blood Compatibility on Polyethersulfone Membrane by Adding Polyvinylpyrrolidone. Fibers Polym. 2009, 10, 1–5. [Google Scholar] [CrossRef]
- Koga, Y.; Fujieda, H.; Meguro, H.; Ueno, Y.; Aoki, T.; Miwa, K.; Kainoh, M. Biocompatibility of Polysulfone Hemodialysis Membranes and Its Mechanisms: Involvement of Fibrinogen and Its Integrin Receptors in Activation of Platelets and Neutrophils. Artif. Organs 2018, 42, E246–E258. [Google Scholar] [CrossRef] [PubMed]
- Bowry, S.K.; Chazot, C. The Scientific Principles and Technological Determinants of Haemodialysis Membranes. Clin. Kidney J. 2021, 14, i5–i16. [Google Scholar] [CrossRef] [PubMed]
- Ekdahl, K.N.; Soveri, I.; Hilborn, J.; Fellström, B.; Nilsson, B. Cardiovascular Disease in Haemodialysis: Role of the Intravascular Innate Immune System. Nat. Rev. Nephrol. 2017, 13, 285–296. [Google Scholar] [CrossRef]
- Ronco, C.; Brendolan, A.; Nalesso, F.; Zanella, M.; De Cal, M.; Corradi, V.; Virzì, G.M.; Ferrari, F.; Garzotto, F.; Lorenzin, A.; et al. Prospective, Randomized, Multicenter, Controlled Trial (TRIATHRON 1) on a New Antithrombogenic Hydrophilic Dialysis Membrane. Int. J. Artif. Organs 2017, 40, 234–239. [Google Scholar] [CrossRef]
- Kislikova, M.; Vega, A.; Verde, E.; Abad, S.; Vaca, M.; Acosta, A.; González, A.; Bascuñana, A.; Mijailova, A.; Nava, C.; et al. Depurative Capacity toward Medium Molecules of the Dialyzer Toray NV-U® HydrolinkTM: A New Hydrophilic Membrane to Perform Online Hemodiafiltration. Int. J. Artif. Organs 2024, 47, 795–801. [Google Scholar] [CrossRef]
- Kakuta, T.; Komaba, H.; Takagi, N.; Takahashi, Y.; Suzuki, H.; Hyodo, T.; Nagaoka, M.; Tanaka, R.; Iwao, S.; Ishida, M.; et al. A Prospective Multicenter Randomized Controlled Study on Interleukin-6 Removal and Induction by a New Hemodialyzer With Improved Biocompatibility in Hemodialysis Patients: A Pilot Study. Ther. Apher. Dial. 2016, 20, 569–578. [Google Scholar] [CrossRef]
- Maduell, F.; Escudero-Saiz, V.J.; Cuadrado-Payán, E.; Rodriguez-Garcia, M.; Gómez, M.; Rodas, L.M.; Fontseré, N.; Salgado, M.D.C.; Casals, G.; Rico, N.; et al. A Study on the Safety and Efficacy of an Innovative Hydrophilic Dialysis Membrane. Membranes 2025, 15, 30. [Google Scholar] [CrossRef] [PubMed]
- Oshihara, W.; Ueno, Y.; Fujieda, H. A New Polysulfone Membrane Dialyzer, NV, with Low-Fouling and Antithrombotic Properties. Contrib. Nephrol. 2017, 189, 222–229. [Google Scholar] [CrossRef]
- Murakami, J.; Kaneko, I.; Kimata, N.; Mineshima, M.; Akiba, T. Problems in the Evaluation of Polyvinylpyrrolidone (PVP) Elution from Polysulfone Membrane Dialyzers Sterilized by Gamma-Ray Irradiation. Ren. Replace. Ther. 2016, 2, 36. [Google Scholar] [CrossRef]
- Lee, G.T.; Hong, Y.K. Manufacturing and Separation Characteristics of Hemodialysis Membranes to Improve Toxin Removal Rate. Adv. Polym. Technol. 2022, 2022, 2565010. [Google Scholar] [CrossRef]
- Abdelrasoul, A.; Westphalen, H.; Saadati, S.; Shoker, A. Hemodialysis Biocompatibility Mathematical Models to Predict the Inflammatory Biomarkers Released in Dialysis Patients Based on Hemodialysis Membrane Characteristics and Clinical Practices. Sci. Rep. 2021, 11, 23080. [Google Scholar] [CrossRef] [PubMed]
- Kiguchi, T.; Ito, H.; Yamashita, A.C. Effect of Membrane Surface Area on Solute Removal Performance of Dialyzers with Fouling. Membranes 2022, 12, 684. [Google Scholar] [CrossRef] [PubMed]
- Boschetti-de-Fierro, A.; Voigt, M.; Storr, M.; Krause, B. MCO Membranes: Enhanced Selectivity in High-Flux Class. Sci. Rep. 2015, 5, 18448. [Google Scholar] [CrossRef] [PubMed]
- Morti, S.M.; Zydney, A.L. Protein-Membrane Interactions during Hemodialysis: Effects on Solute Transport. ASAIO J. 1998, 44, 319–326. [Google Scholar] [CrossRef]
- Langsdorf, L.J.; Zydney, A.L. Effect of Blood Contact on the Transport Properties of Hemodialysis Membranes: A Two-Layer Membrane Model. Blood Purif. 1994, 12, 292–307. [Google Scholar] [CrossRef]
- Kim, T.R.; Hadidi, M.; Motevalian, S.P.; Sunohara, T.; Zydney, A.L. Effects of Plasma Proteins on the Transport and Surface Characteristics of Polysulfone/Polyethersulfone and Asymmetric Cellulose Triacetate High Flux Dialyzers. Artif. Organs 2018, 42, 1070–1077. [Google Scholar] [CrossRef]
- Röckel, A.; Hertel, J.; Fiegel, P.; Abdelhamid, S.; Panitz, N.; Walb, D. Permeability and Secondary Membrane Formation of a High Flux Polysulfone Hemofilter. Kidney Int. 1986, 30, 429–432. [Google Scholar] [CrossRef]
- Canaud, B. Recent Advances in Dialysis Membranes. Curr. Opin. Nephrol. Hypertens. 2021, 30, 613–622. [Google Scholar] [CrossRef]
- Kempkes-Koch, M.; Stauss-Grabo, M.; Erlenkötter, A.; Rauber, L.; Kennedy, J.; Gauly, A.; Schmidt-Gürtler, H. MO387 Clinical performance, hemocompatibility and safety of a new dialyzer with a modified polysulfone membrane. Nephrol. Dial. Transplant. 2021, 36, gfab082.0041. [Google Scholar] [CrossRef]
- Ehlerding, G.; Erlenkötter, A.; Gauly, A.; Griesshaber, B.; Kennedy, J.; Rauber, L.; Ries, W.; Schmidt-Gürtler, H.; Stauss-Grabo, M.; Wagner, S.; et al. Performance and Hemocompatibility of a Novel Polysulfone Dialyzer: A Randomized Controlled Trial. Kidney360 2021, 2, 935–945. [Google Scholar] [CrossRef]
- Ehlerding, G.; Ries, W.; Kempkes-Koch, M.; Ziegler, E.; Erlenkötter, A.; Zawada, A.M.; Kennedy, J.P.; Ottillinger, B.; Stauss-Grabo, M.; Lang, T. Randomized Comparison of Three High-Flux Dialyzers during High-Volume Online Hemodiafiltration—The comPERFORM Study. Clin. Kidney J. 2022, 15, 672–680. [Google Scholar] [CrossRef] [PubMed]
- Ehlerding, G.; Ries, W.; Kempkes-Koch, M.; Ziegler, E.; Ronová, P.; Krizsán, M.; Verešová, J.; Böke, M.; Erlenkötter, A.; Nitschel, R.; et al. Randomized Investigation of Increased Dialyzer Membrane Hydrophilicity on Hemocompatibility and Performance. BMC Nephrol. 2024, 25, 220. [Google Scholar] [CrossRef] [PubMed]
- Kuragano, T.; Kida, A.; Furuta, M.; Nanami, M.; Otaki, Y.; Hasuike, Y.; Nonoguchi, H.; Nakanishi, T. The Impact of Β2-Microglobulin Clearance on the Risk Factors of Cardiovascular Disease in Hemodialysis Patients. ASAIO J. 2010, 56, 326–332. [Google Scholar] [CrossRef]
- Kaizu, Y.; Ohkawa, S.; Odamaki, M.; Ikegaya, N.; Hibi, I.; Miyaji, K.; Kumagai, H. Association between Inflammatory Mediators and Muscle Mass in Long-Term Hemodialysis Patients. Am. J. Kidney Dis. 2003, 42, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Neirynck, N.; Vanholder, R.; Schepers, E.; Eloot, S.; Pletinck, A.; Glorieux, G. An Update on Uremic Toxins. Int. Urol. Nephrol. 2013, 45, 139–150. [Google Scholar] [CrossRef]
- Wolley, M.; Jardine, M.; Hutchison, C.A. Exploring the Clinical Relevance of Providing Increased Removal of Large Middle Molecules. Clin. J. Am. Soc. Nephrol. 2018, 13, 805–814. [Google Scholar] [CrossRef]
- Canaud, B.; Blankestijn, P.J.; Grooteman, M.P.C.; Davenport, A. Why and How High Volume Hemodiafiltration May Reduce Cardiovascular Mortality in Stage 5 Chronic Kidney Disease Dialysis Patients? A Comprehensive Literature Review on Mechanisms Involved. Semin. Dial. 2022, 35, 117–128. [Google Scholar] [CrossRef]
- Cheung, A.K.; Rocco, M.V.; Yan, G.; Leypoldt, J.K.; Levin, N.W.; Greene, T.; Agodoa, L.; Bailey, J.; Beck, G.J.; Clark, W.; et al. Serum β-2 Microglobulin Levels Predict Mortality in Dialysis Patients: Results of the HEMO Study. J. Am. Soc. Nephol. 2006, 17, 546–555. [Google Scholar] [CrossRef]
- Okuno, S.; Ishimura, E.; Kohno, K.; Fujino-Katoh, Y.; Maeno, Y.; Yamakawa, T.; Inaba, M.; Nishizawa, Y. Serum 2-Microglobulin Level Is a Significant Predictor of Mortality in Maintenance Haemodialysis Patients. Nephrol. Dial. Transplant. 2008, 24, 571–577. [Google Scholar] [CrossRef]
- Pifer, T.B.; Mccullough, K.P.; Port, F.K.; Goodkin, D.A.; Maroni, B.J.; Held, P.J.; Young, E.W. Mortality Risk in Hemodialysis Patients and Changes in Nutritional Indicators: DOPPS. Kidney Int. 2002, 62, 2238–2245. [Google Scholar] [CrossRef]
- Canaud, B.; Ye, X.; Usvyat, L.; Kooman, J.; van der Sande, F.; Raimann, J.; Wang, Y.; Kotanko, P. Clinical and Predictive Value of Simplified Creatinine Index Used as Muscle Mass Surrogate in End-Stage Kidney Disease Haemodialysis Patients—Results from the International MONitoring Dialysis Outcome Initiative. Nephrol. Dial. Transplant. 2020, 35, 2161–2171. [Google Scholar] [CrossRef] [PubMed]
- de Mutsert, R.; Grootendorst, D.C.; Axelsson, J.; Boeschoten, E.W.; Krediet, R.T.; Dekker, F.W. the NECOSAD Study Group. Excess Mortality Due to Interaction between Protein-Energy Wasting, Inflammation and Cardiovascular Disease in Chronic Dialysis Patients. Nephrol. Dial. Transplant. 2008, 23, 2957–2964. [Google Scholar] [CrossRef] [PubMed]
- Blankestijn, P.J.; Vernooij, R.W.M.; Hockham, C.; Strippoli, G.F.M.; Canaud, B.; Hegbrant, J.; Barth, C.; Covic, A.; Cromm, K.; Cucui, A.; et al. Effect of Hemodiafiltration or Hemodialysis on Mortality in Kidney Failure. N. Engl. J. Med. 2023, 389, 700–709. [Google Scholar] [CrossRef] [PubMed]
- Maduell, F.; Broseta, J.J.; Rodríguez-Espinosa, D.; Rodas, L.M.; Gómez, M.; Arias-Guillén, M.; Fontseré, N.; Vera, M.; Salgado, M.D.C.; Rico, N.; et al. Comparison of Efficacy and Safety of the New Generation Helixone Dialyzers. Nefrología 2024, 44, 354–361. [Google Scholar] [CrossRef]
- Losappio, V.; Franzin, R.; Infante, B.; Godeas, G.; Gesualdo, L.; Fersini, A.; Castellano, G.; Stallone, G. Molecular Mechanisms of Premature Aging in Hemodialysis: The Complex Interplay between Innate and Adaptive Immune Dysfunction. Int. J. Mol. Sci. 2020, 21, 3422. [Google Scholar] [CrossRef]
- Bowry, S.K.; Kircelli, F.; Himmele, R.; Nigwekar, S.U. Blood-Incompatibility in Haemodialysis: Alleviating Inflammation and Effects of Coagulation. Clin. Kidney J. 2021, 14, i59–i71. [Google Scholar] [CrossRef]
- Poppelaars, F.; Faria, B.; Gaya da Costa, M.; Franssen, C.F.M.; van Son, W.J.; Berger, S.P.; Daha, M.R.; Seelen, M.A. The Complement System in Dialysis: A Forgotten Story? Front. Immunol. 2018, 9, 71. [Google Scholar] [CrossRef]
- Mares, J.; Richtrova, P.; Hricinova, A.; Tuma, Z.; Moravec, J.; Lysak, D.; Matejovic, M. Proteomic Profiling of Blood-Dialyzer Interactome Reveals Involvement of Lectin Complement Pathway in Hemodialysis-Induced Inflammatory Response. Proteom. Clin. Appl. 2010, 4, 829–838. [Google Scholar] [CrossRef]
- Nilsson, B.; Ekdahl, K.N.; Mollnes, T.E.; Lambris, J.D. The Role of Complement in Biomaterial-Induced Inflammation. Mol. Immunol. 2007, 44, 82–94. [Google Scholar] [CrossRef]
- Chenoweth, D.E.; Cheung, A.K.; Henderson, L.W. Anaphylatoxin Formation during Hemodialysis: Effects of Different Dialyzer Membranes. Kidney Int. 1983, 24, 764–769. [Google Scholar] [CrossRef]
- de Borst, M.H. The Complement System in Hemodialysis Patients: Getting to the Heart of the Matter. Nephron 2016, 132, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Kourtzelis, I.; Markiewski, M.M.; Doumas, M.; Rafail, S.; Kambas, K.; Mitroulis, I.; Panagoutsos, S.; Passadakis, P.; Vargemezis, V.; Magotti, P.; et al. Complement Anaphylatoxin C5a Contributes to Hemodialysis-Associated Thrombosis. Blood 2010, 116, 631–639. [Google Scholar] [CrossRef]
- François, K.; Orlando, C.; Jochmans, K.; Cools, W.; De Meyer, V.; Tielemans, C.; Wissing, K.M. Hemodialysis Does Not Induce Detectable Activation of the Contact System of Coagulation. Kidney Int. Rep. 2020, 5, 831–838. [Google Scholar] [CrossRef]
- Lucchi, L.; Ligabue, G.; Marietta, M.; Delnevo, A.; Malagoli, M.; Perrone, S.; Stipo, L.; Grandi, F.; Albertazzi, A. Activation of Coagulation During Hemodialysis: Effect of Blood Lines Alone and Whole Extracorporeal Circuit. Artif. Organs 2006, 30, 106–110. [Google Scholar] [CrossRef]
- Milburn, J.A.; Ford, I.; Mutch, N.J.; Fluck, N.; Brittenden, J. Thrombin-Anti-Thrombin Levels and Patency of Arterio-Venous Fistula in Patients Undergoing Haemodialysis Compared to Healthy Volunteers: A Prospective Analysis. PLoS ONE 2013, 8, e67799. [Google Scholar] [CrossRef]
- Hernández, M.R.; Galán, A.M.; Lozano, M.; Bozzo, J.; Cases, A.; Escolar, G.; Calls, J.; Ordinas, A. Platelet-Leukocyte Activation during Hemodialysis Detected with a Monoclonal Antibody to Leukocyte Integrin CD11b. Nephron 1998, 80, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Daikidou, D.-V.; Lioulios, G.; Sampani, E.; Xochelli, A.; Nikolaidou, V.; Moysidou, E.; Christodoulou, M.; Iosifidou, A.; Iosifidou, M.; Briza, D.; et al. Prospective Analysis of B Lymphocyte Subtypes, before and after Initiation of Dialysis, in Patients with End-Stage Renal Disease. Life 2023, 13, 860. [Google Scholar] [CrossRef] [PubMed]
- Singh, V.; Kaur, R.; Kumari, P.; Pasricha, C.; Singh, R. ICAM-1 and VCAM-1: Gatekeepers in Various Inflammatory and Cardiovascular Disorders. Clin. Chim. Acta 2023, 548, 117487. [Google Scholar] [CrossRef]
- Daugirdas, J.T.; Bernardo, A.A. Hemodialysis Effect on Platelet Count and Function and Hemodialysis-Associated Thrombocytopenia. Kidney Int. 2012, 82, 147–157. [Google Scholar] [CrossRef]
- Rogacev, K.S.; Ziegelin, M.; Ulrich, C.; Seiler, S.; Girndt, M.; Fliser, D.; Heine, G.H. Haemodialysis-Induced Transient CD16+ Monocytopenia and Cardiovascular Outcome. Nephrol. Dial. Transplant. 2009, 24, 3480–3486. [Google Scholar] [CrossRef]
- Maher, J.F.; Schreiner, G.E. Hazards and Complications of Dialysis. N. Engl. J. Med. 1965, 273, 370–377. [Google Scholar] [CrossRef]
- Salem, M.; Ivanovich, P.T.; Ing, T.S.; Daugirdas, J.T. Adverse Effects of Dialyzers Manifesting during the Dialysis Session. Nephrol. Dial. Transplant. 1994, 9 (Suppl. S2), 127–137. [Google Scholar] [PubMed]
- Himmelfarb, J. Hemodialysis Complications. Am. J. Kidney Dis. 2005, 45, 1122–1131. [Google Scholar] [CrossRef] [PubMed]
- Wong, B.; Zimmerman, D.; Reintjes, F.; Courtney, M.; Klarenbach, S.; Dowling, G.; Pauly, R.P. Procedure-Related Serious Adverse Events Among Home Hemodialysis Patients: A Quality Assurance Perspective. Am. J. Kidney Dis. 2014, 63, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Saha, M.; Allon, M. Diagnosis, Treatment, and Prevention of Hemodialysis Emergencies. Clin. J. Am. Soc. Nephrol. 2017, 12, 357–369. [Google Scholar] [CrossRef]
- Scherer, J.S.; Combs, S.A.; Brennan, F. Sleep Disorders, Restless Legs Syndrome, and Uremic Pruritus: Diagnosis and Treatment of Common Symptoms in Dialysis Patients. Am. J. Kidney Dis. 2017, 69, 117–128. [Google Scholar] [CrossRef]
- Greenberg, K.I.; Choi, M.J. Hemodialysis Emergencies: Core Curriculum 2021. Am. J. Kidney Dis. 2021, 77, 796–809. [Google Scholar] [CrossRef]
- Davenport, A.; Vervloet, M. Effects of Convective Dialysis Techniques on Electrolytes and Mineral Metabolism. In Hemodiafiltration; Nubé, M.J., Grooteman, M.P.C., Blankestijn, P.J., Eds.; Springer International Publishing: Cham, Switzerland, 2016; pp. 121–135. ISBN 978-3-319-23331-4. [Google Scholar]
- Dekker, M.J.E.; Kooman, J.P. Fluid Status Assessment in Hemodialysis Patients and the Association with Outcome: Review of Recent Literature. Curr. Opin. Nephrol. Hypertens. 2018, 27, 188–193. [Google Scholar] [CrossRef]
- Hecking, M.; Madero, M.; Port, F.K.; Schneditz, D.; Wabel, P.; Chazot, C. Fluid Volume Management in Hemodialysis: Never Give Up! Kidney Int. 2023, 103, 2–5. [Google Scholar] [CrossRef]
- Milinkovic, M.; Zidverc-Trajkovic, J.; Sternic, N.; Trbojevic-Stankovic, J.; Maric, I.; Milic, M.; Andric, B.; Nikic, P.; Jovanovic, P.; Rosic, P.; et al. Hemodialysis Headache. Clin. Nephrol. 2009, 71, 158–163. [Google Scholar] [CrossRef]
- Loutradis, C.; Sarafidis, P.A.; Ferro, C.J.; Zoccali, C. Volume Overload in Hemodialysis: Diagnosis, Cardiovascular Consequences, and Management. Nephrol. Dial. Transplant. 2021, 36, 2182–2193. [Google Scholar] [CrossRef] [PubMed]
- Kanbay, M.; Ertuglu, L.A.; Afsar, B.; Ozdogan, E.; Siriopol, D.; Covic, A.; Basile, C.; Ortiz, A. An Update Review of Intradialytic Hypotension: Concept, Risk Factors, Clinical Implications and Management. Clin. Kidney J. 2020, 13, 981–993. [Google Scholar] [CrossRef] [PubMed]
- Sars, B.; van der Sande, F.M.; Kooman, J.P. Intradialytic Hypotension: Mechanisms and Outcome. Blood Purif. 2020, 49, 158–167. [Google Scholar] [CrossRef] [PubMed]
- Davenport, A. Why Is Intradialytic Hypotension the Commonest Complication of Outpatient Dialysis Treatments? Kidney Int. Rep. 2023, 8, 405–418. [Google Scholar] [CrossRef]
- Canzanello, V.J.; Burkart, J.M. Hemodialysis-Associated Muscle Cramps. Semin. Dial. 1992, 5, 299–304. [Google Scholar] [CrossRef]
- Sav, M.Y.; Sav, T.; Senocak, E.; Sav, N.M. Hemodialysis-related Headache. Hemodial. Int. 2014, 18, 725–729. [Google Scholar] [CrossRef]
- Pun, P.H.; Middleton, J.P. Dialysate Potassium, Dialysate Magnesium, and Hemodialysis Risk. J. Am. Soc. Nephrol. 2017, 28, 3441–3451. [Google Scholar] [CrossRef]
- Boyer, C.J.; Swartz, R.D. Severe Clotting During Extracorporeal Dialysis Procedures. Semin. Dial. 1991, 4, 69–71. [Google Scholar] [CrossRef]
- Hornig, C.; Bowry, S.K.; Kircelli, F.; Kendzia, D.; Apel, C.; Canaud, B. Hemoincompatibility in Hemodialysis-Related Therapies and Their Health Economic Perspectives. J. Clin. Med. 2024, 13, 6165. [Google Scholar] [CrossRef]
- Fadem, S.Z. Blood Clotting Complications in Dialysis. In Complications in Dialysis; Fadem, S.Z., Moura-Neto, J.A., Golper, T.A., Eds.; Springer International Publishing: Cham, Switzerland, 2023; pp. 203–218. ISBN 978-3-031-44556-9. [Google Scholar]
- Polaschegg, H. Red Blood Cell Damage from Extracorporeal Circulation in Hemodialysis. Semin. Dial. 2009, 22, 524–531. [Google Scholar] [CrossRef]
- Tharmaraj, D.; Kerr, P.G. Haemolysis in Haemodialysis. Nephrology 2017, 22, 838–847. [Google Scholar] [CrossRef] [PubMed]
- Yoon, J.; Thapa, S.; Chow, R.D.; Jaar, B.G. Hemolysis as a Rare but Potentially Life-Threatening Complication of Hemodialysis: A Case Report. BMC Res. Notes 2014, 7, 475. [Google Scholar] [CrossRef]
- Röckel, A.; Klinke, B.; Hertel, J.; Baur, X.; Thiel, C.; Abdelhamid, S.; Fiegel, P.; Walb, D. Allergy to Dialysis Materials. Nephrol. Dial. Transplant. 1989, 4, 646–652. [Google Scholar]
- Mukaya, J.E.; Jacobson, M.S.; Esprit, D.; Ajayi, T. Allergic Reaction to Polysulphone Membrane Dialyser Masquerading as Infection. BMJ Case Rep. 2015, bcr2014208591. [Google Scholar] [CrossRef] [PubMed]
- Sayeed, K.; Murdakes, C.; Spec, A.; Gashti, C. Anaphylactic Shock at the Beginning of Hemodialysis. Semin. Dial. 2016, 29, 81–84. [Google Scholar] [CrossRef] [PubMed]
- Shu, K.-H.; Kao, T.-W.; Chiang, W.-C.; Wu, V.-C. A Case of Anaphylactic Shock Induced by FX60 Polysulfone Hemodialyzer but Not F6-HPS Polysulfone Hemodialyzer: Polysulfone Hemodialyzer Anaphylaxis. Hemodial. Int. 2014, 18, 841–845. [Google Scholar] [CrossRef]
- Bacelar Marques, I.D.; Pinheiro, K.F.; de Freitas do Carmo, L.P.; Costa, M.C.; Abensur, H. Anaphylactic Reaction Induced by a Polysulfone/Polyvinylpyrrolidone Membrane in the 10th Session of Hemodialysis with the Same Dialyzer. Hemodial. Int. 2011, 15, 399–403. [Google Scholar] [CrossRef]
- Martin-Navarro, J.; Esteras, R.; Castillo, E.; Carriazo, S.; Fernández-Prado, R.; Gracia-Iguacel, C.; Mas Fontao, S.; Ortíz, A.; González-Parra, E. Reactions to Synthetic Membranes Dialyzers: Is There an Increase in Incidence? Kidney Blood Press. Res. 2019, 44, 907–914. [Google Scholar] [CrossRef]
- Ohashi, N.; Yonemura, K.; Goto, T.; Suzuki, H.; Fujigaki, Y.; Yamamoto, T.; Hishida, A. A Case of Anaphylactoid Shock Induced by the BS Polysulfone Hemodialyzer but Not by the F8-HPS Polysulfone Hemodialyzer. Clin. Nephrol. 2003, 60, 214–217. [Google Scholar] [CrossRef]
- Glorieux, G.; Hulko, M.; Speidel, R.; Brodbeck, K.; Krause, B.; Vanholder, R. Looking beyond Endotoxin: A Comparative Study of Pyrogen Retention by Ultrafilters Used for the Preparation of Sterile Dialyis Fluid. Sci. Rep. 2014, 4, 6390. [Google Scholar] [CrossRef]
- Hindman, S.; Carson, L.; Favero, M.; Petersen, N.; Schonberger, L.; Solano, J. Pyrogenic reactions during haemodialysis caused by extramural endotoxin. Lancet 1975, 306, 732–734. [Google Scholar] [CrossRef] [PubMed]
- Catapano, G.; Morrone, G.; Hu, L.; Fragomeni, G.; Buscaroli, A. Endotoxin-Retentive Filters for the Online Preparation of Ultrapure Dialysis Fluid and Non-Pyrogenic Substitution Fluid: A Critical Review and Reference Guide. Membranes 2025, 15, 51. [Google Scholar] [CrossRef]
- Axley, B.; Speranza-Reid, J.; Williams, H. Venous Needle Dislodgement in Patients on Hemodialysis. Nephrol. Nurs. J. 2012, 39, 435–445; quiz 446. [Google Scholar] [PubMed]
- Tennankore, K.K.; d’Gama, C.; Faratro, R.; Fung, S.; Wong, E.; Chan, C.T. Adverse Technical Events in Home Hemodialysis. Am. J. Kidney Dis. 2015, 65, 116–121. [Google Scholar] [CrossRef]
- MacRae, J.M.; Dipchand, C.; Oliver, M.; Moist, L.; Lok, C.; Clark, E.; Hiremath, S.; Kappel, J.; Kiaii, M.; Luscombe, R.; et al. Arteriovenous Access Failure, Stenosis, and Thrombosis. Can. J. Kidney Health Dis. 2016, 3, 2054358116669126. [Google Scholar] [CrossRef] [PubMed]
- Franchin, M.; Tadiello, M.; Guzzetti, L.; Gattuso, A.; Mauri, F.; Cervarolo, M.C.; D’Oria, M.G.G.; Tozzi, M. Acute Problems of Hemodialysis Access: Thrombosis, Aneurysms, Symptomatic High-Flow Fistulas, and Complications Related to Central Lines. Semin. Vasc. Surg. 2023, 36, 300–306. [Google Scholar] [CrossRef]
- Kumbar, L.; Yee, J. Current Concepts in Hemodialysis Vascular Access Infections. Adv. Chronic. Kidney Dis. 2019, 26, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Vesely, T.M. Air Embolism during Insertion of Central Venous Catheters. J. Vasc. Interv. Radiol. 2001, 12, 1291–1295. [Google Scholar] [CrossRef]
- Sweet, S.J.; McCarthy, S.; Steingart, R.; Callahan, T. Hemolytic Reactions Mechanically Induced by Kinked Hemodialysis Lines. Am. J. Kidney Dis. 1996, 27, 262–266. [Google Scholar] [CrossRef]
- Malinauskas, R.A. Decreased Hemodialysis Circuit Pressures Indicating Postpump Tubing Kinks: A Retrospective Investigation of Hemolysis in Five Patients. Hemodial. Int. 2008, 12, 383–393. [Google Scholar] [CrossRef]
- Patel, N.; Dalal, P.; Panesar, M. Fellows’ Forum Fellows’ Forum in Dialysis Edited by Mark A. Perazella: Dialysis Disequilibrium Syndrome: A Narrative Review. Semin. Dial. 2008, 21, 493–498. [Google Scholar] [CrossRef] [PubMed]
- Raina, R.; Davenport, A.; Warady, B.; Vasistha, P.; Sethi, S.K.; Chakraborty, R.; Khooblall, P.; Agarwal, N.; Vij, M.; Schaefer, F.; et al. Dialysis Disequilibrium Syndrome (DDS) in Pediatric Patients on Dialysis: Systematic Review and Clinical Practice Recommendations. Pediatr. Nephrol. 2022, 37, 263–274. [Google Scholar] [CrossRef] [PubMed]
- Stuard, S.; Ridel, C.; Cioffi, M.; Trost-Rupnik, A.; Gurevich, K.; Bojic, M.; Karibayev, Y.; Mohebbi, N.; Marcinkowski, W.; Kupres, V.; et al. Hemodialysis Procedures for Stable Incident and Prevalent Patients Optimize Hemodynamic Stability, Dialysis Dose, Electrolytes, and Fluid Balance. J. Clin. Med. 2024, 13, 3211. [Google Scholar] [CrossRef] [PubMed]
- Pedreros-Rosales, C.; Jara, A.; Lorca, E.; Mezzano, S.; Pecoits-Filho, R.; Herrera, P. Unveiling the Clinical Benefits of High-Volume Hemodiafiltration: Optimizing the Removal of Medium-Weight Uremic Toxins and Beyond. Toxins 2023, 15, 531. [Google Scholar] [CrossRef]
- Rose, M.; Fischer, F.H.; Liegl, G.; Strippoli, G.F.M.; Hockham, C.; Vernooij, R.W.M.; Barth, C.; Canaud, B.; Covic, A.; Cromm, K.; et al. The CONVINCE Randomized Trial Found Positive Effects on Quality of Life for Patients with Chronic Kidney Disease Treated with Hemodiafiltration. Kidney Int. 2024, 106, 961–971. [Google Scholar] [CrossRef]
| Study Title | Comparators | Investigations | Study Findings for FX CorAL | Study Reference |
|---|---|---|---|---|
| Complement activation by dialysis membranes and its association with secondary membrane formation and surface charge | FX CorAL FX CorDiax xevonta Polyflux ELISIO FDX THERANOVA SUREFLUX |
|
| Melchior et al. (2021) [14] |
| Polyvinylpyrrolidone in hemodialysis membranes: Impact on platelet loss during hemodialysis | FX CorAL FX CorDiax xevonta ELISIO Polyflux THERANOVA |
|
| Zawada et al. (2021) [13] |
| Time-resolving characterization of molecular weight retention changes among three synthetic high-flux dialyzers | FX CorAL ELISIO xevonta |
|
| Zawada et al. (2022) [12] |
| Impact of Hydrophilic Modification of Synthetic Dialysis Membranes on Hemocompatibility and Performance | FX CorAL FX CorDiax |
|
| Zawada et al. (2022) [10] |
| Hydrophilic Modification of Dialysis Membranes Sustains Middle Molecule Removal and Filtration Characteristics | FX CorAL FX CorDiax xevonta Diacap Pro HF ELISIO DORA Revaclear Cellentia |
|
| Zawada et al. (2024) [11] |
| Study Acronym/ Study Title | Study Design | Therapy | Number of Patients * | Duration | Comparators | Primary Endpoint | Further Endpoints | Study Findings for FX CorAL | Study Reference |
|---|---|---|---|---|---|---|---|---|---|
| eMPORA I/ Safety and clinical performance of a dialyzer with a modified polysulfone membrane | Open, multicenter, randomized controlled trial (Germany) | Online-post dilution HDF/ without autosub plus | 45 | 4 weeks | FX CorAL FX CorDiax FX class | β2-m removal rate (non-inferiority of FX CorAL) |
|
| Kempkes-Koch et al. (2021) [39] |
| eMPORA II/ Comparative safety and clinical performance of dialyzers applied during post-dilution online hemodiafiltration | Open, multicenter, randomized controlled trial (Germany) | Online-post dilution HDF/ without autosub plus | 58 | 4 weeks | FX CorAL Polyflux SUREFLUX | β2-m removal rate (non-inferiority of FX CorAL) |
|
| Ehlerding et al. (2021) [40] |
| comPERFORM/ Comparative clinical performance of dialyzers applied during high volume online hemodiafiltration | Open, multicenter, randomized controlled trial (Germany) | Online-post dilution HDF/ with autosub plus | 52 | 5 weeks | FX CorAL ELISIO xevonta | β2-m removal rate (non-inferiority/superiority of FX CorAL) |
|
| Ehlerding et al. (2022) [41] |
| eMPORA III/ Comparison of clinical performance and hemocompatibility of dialyzers applied during postdilution online hemodiafiltration | Open, multi-center, randomized controlled trial (Germany, Czech Republic, Hungary) | Online-post dilution HDF/ without autosub plus | 76 | 14 weeks | FX CorAL FX CorDiax xevonta | β2-m removal rate (non-inferiority/superiority of FX CorAL) |
|
| Ehlerding et al. (2024) [42] |
| eMPORA I | eMPORA II | comPERFORM | eMPORA III | |
|---|---|---|---|---|
| Patient characteristics * | ||||
| Age [years] | 66.3 ± 13.6 | 67.8 ± 13.4 | 64.8 ± 14.5 | 67.0 ± 15.6 |
| Gender [% male] | 76 | 74 | 85 | 74 |
| Mean BMI [kg/m2] | 27.7 ± 5.8 | 28.9 ± 6.6 | 28.2 ± 7.5 | 27.3 ± 5.1 |
| Diabetes [%] | 31 | 36 | 21 | 34 |
| Median time on RRT [months] | 42 | 50 | 56 | 40 |
| Treatment parameter (online post-dilution HDF) ** | ||||
| Blood flow rate [mL/min] | 303 ± 29 | 306 ± 29 | 331 ± 12 | 345 ± 44 |
| Dialysate flow rate [mL/min] | 499 ± 5 | 500 ± 0.1 | 529 ± 19 | 577 ± 96 |
| Substitution volume [L] | 20.2 ± 5.7 | 17.6 ± 4.5 | 25.4 ± 2.8 | 21.0 ± 3.2 |
| Ultrafiltration volume [L] | 1.9 ± 1.1 | 2.2 ± 1.2 | 2.0 ± 0.2 | 2.3 ± 1.0 |
| Effective treatment time [min] | 269 ± 29 | 272 ± 29 | 273 ± 14 | 262 ± 21 |
| Performance Parameter | eMPORA I | eMPORA II | comPERFORM | eMPORA III | ||||
|---|---|---|---|---|---|---|---|---|
| FX CorAL vs. | FX CorAL vs. | FX CorAL vs. | FX CorAL vs. | |||||
| FX CorDiax | FX class | SUREFLUX | Polyflux | xevonta | ELISIO | FX CorDiax | xevonta | |
| β2-m RR [non-inferiority] | ★ | ★ | ★ | ★ | ★ | ★ | ★ | ★ |
| β2-m RR [superiority] | - | - | ★ | c | ★ | ★ | c | ★ |
| β2-m clearance | c | ★ | ★ | c | ★ | ★ | c | ★ |
| Myoglobin RR | c | ★ | # | # | ★ | ★ | ★ | ★ |
| Myoglobin clearance | c | ★ | # | c | ★ | c | ★ | ★ |
| Phosphate RR | # | # | c | c | c | c | c | c |
| Phosphate clearance | c | c | c | c | c | c | c | c |
| Creatinine RR | # | c | c | c | c | c | c | c |
| Creatinine clearance | c | c | # | c | c | c | c | c |
| Urea RR | c | c | c | c | c | c | c | c |
| Urea clearance | c | c | # | # | c | c | c | c |
| Albumin loss | - | - | - | - | c | c | - | - |
| Performance Parameter | eMPORA I | eMPORA II | eMPORA III | ||||
|---|---|---|---|---|---|---|---|
| FX CorAL vs. | FX CorAL vs. | FX CorAL vs. | |||||
| FX CorDiax | FX class | SUREFLUX | Polyflux | FX CorDiax | xevonta | ||
| Complement activation | C3a | c15 | c15 | ★15 | c15 | ★15 | ★15 |
| C5a | c15 | ★15 | ★15 | c15 | - | - | |
| sC5b-9 | c15 | ★15 | ★60 | ★60 | c60 | ★60 | |
| Cell activation/ inflammation | Leukocyte counts | c15 | c15 | ★15 | ★15 | ★15 | c15 |
| Monocyte counts | c240 | c240 | c240 | c240 | c15 | ★15 | |
| Neutrophile counts | c240 | c240 | c240 | c240 | ★15 | c15 | |
| PMN elastase | c240 | c240 | c240 | ★240 | ★60 | ★60 | |
| LTB4 | - | - | - | - | ★15 | c15 | |
| IL-6 | - | - | - | - | cAUC | cAUC | |
| IL-8 | - | - | - | - | cAUC | cAUC | |
| sICAM-1 | - | - | - | - | c240 | c240 | |
| hsCRP | c240 | c240 | - | - | c0 | c0 | |
| Platelet activation/ coagulation | Platelet counts | c240 | c240 | c240 | ★240 | c15 | c15 |
| β-TG | - | - | c240 | c240 | ★60 | ★60 | |
| TxB2 | - | - | - | - | c15 | #15 | |
| TAT | c240 | c240 | c240 | c240 | - | - | |
| Oxidative stress | MDA | - | - | - | - | cAUC | cAUC |
| GSH-Px activity | - | - | - | - | cAUC | cAUC | |
| Contact phase activation | Kallikrein | c240 | c240 | c240 | c240 | - | - |
| Level 1 Term | Adverse Event (MedDRA PT) | Total Occurrences [Device Related/ Procedure Related/Both] | Frequency Per Patient [%] * [Device Related/ Procedure Related/ Both] | Frequency Per Treatment [%] ** [Device Related/ Procedure Related/ Both] | Occurrences Per Device [Device Related/Procedure Related/Both] | |
|---|---|---|---|---|---|---|
| FX CorAL *** | Other Dialyzers **** | |||||
| Electrolyte imbalance |
| 41 [3/27/11] | 16.5 [1.2/10.8/4.4] | 1.0 [0.1/0.7/0.3] | 11 [2/9/0] Frequency per treatment: 0.8% | 30 [1/18/11] Frequency per treatment: 1.1% |
| Fluid imbalance |
| 27 [8/9/10] | 10.8 [3.2/3.6/4.0] | 0.7 [0.2/0.2/0.2] | 10 [5/2/3] Frequency per treatment: 0.7% | 17 [3/7/7] Frequency per treatment: 0.6% |
| Pruritus, non-allergic |
| 6 [0/0/6] | 2.4 [0/0/2.4] | 0.1 [0/0/0.1] | 1 [0/0/1] Frequency per treatment: 0.1% | 5 [0/0/5] Frequency per treatment: 0.2% |
| Device malfunction (clotting, thrombosis) |
| 5 [0/2/3] | 2.0 [0/0.8/1.2] | 0.1 [0/<0.1/0.1] | 3 [0/2/1] Frequency per treatment: 0.2% | 2 [0/0/2] Frequency per treatment: 0.1% |
| Procedural complication (blood-side) |
| 4 [0/4/0] | 1.6 [0/1.6/0] | 0.1 [0/0.1/0] | 1 [0/1/0] Frequency per treatment: 0.1% | 3 [0/3/0] Frequency per treatment: 0.1% |
| Peripheral vascular disorder |
| 3 [2/0/1] | 1.2 [0.8/0/0.4] | 0.1 [<0.1/0/<0.1] | 1 [1/0/0] Frequency per treatment: 0.1% | 2 [1/0/1] Frequency per treatment: 0.1% |
| Vascular hypertensive disorder |
| 2 [0/2/0] | 0.8 [0/0.8/0] | <0.1 [0/<0.1/0] | 2 [0/2/0] Frequency per treatment: 0.1% | 0 [0/0/0] Frequency per treatment: 0% |
| Device mechanical failure |
| 2 [1/0/1] | 0.8 [0.4/0/0.4] | <0.1 [<0.1/0/<0.1] | 0 [0/0/0] Frequency per treatment: 0% | 2 [1/0/1] Frequency per treatment: 0.1% |
| Anemia |
| 1 [0/0/1] | 0.4 [0/0/0.4] | <0.1 [0/0/<0.1] | 0 [0/0/0] Frequency per treat-ment: 0% | 1 [0/0/1] Frequency per treatment: <0.1% |
| Vasoconstriction, vascular insufficiency |
| 2 [0/2/0] | 0.8 [0/0.8/0] | <0.1 [0/<0.1/0] | 0 [0/0/0] Frequency per treat-ment: 0% | 2 [0/2/0] Frequency per treat-ment: 0.1% |
| Infection |
| 1 [0/0/1] | 0.4 [0/0/0.4] | <0.1 [0/0/<0.1] | 0 [0/0/0] Frequency per treat-ment: 0% | 1 [0/0/1] Frequency per treat-ment: <0.1% |
| Total | 94 [14/46/34] | 37.8 [5.6/18.5/13.7] | 2.3 [0.3/1.1/0.8] | 29 [8/16/5] Frequency per treat-ment: 2.1% | 65 [6/30/29] Frequency per treat-ment: 2.4% | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zawada, A.M.; Griesshaber, B.; Ottillinger, B.; Erlenkötter, A.; Crook, N.; Boyington, S.; Stauss-Grabo, M.; Kennedy, J.P.; Lang, T. Development and Investigation of a New Polysulfone Dialyzer with Increased Membrane Hydrophilicity. Membranes 2025, 15, 132. https://doi.org/10.3390/membranes15050132
Zawada AM, Griesshaber B, Ottillinger B, Erlenkötter A, Crook N, Boyington S, Stauss-Grabo M, Kennedy JP, Lang T. Development and Investigation of a New Polysulfone Dialyzer with Increased Membrane Hydrophilicity. Membranes. 2025; 15(5):132. https://doi.org/10.3390/membranes15050132
Chicago/Turabian StyleZawada, Adam M., Bettina Griesshaber, Bertram Ottillinger, Ansgar Erlenkötter, Nathan Crook, Skyler Boyington, Manuela Stauss-Grabo, James P. Kennedy, and Thomas Lang. 2025. "Development and Investigation of a New Polysulfone Dialyzer with Increased Membrane Hydrophilicity" Membranes 15, no. 5: 132. https://doi.org/10.3390/membranes15050132
APA StyleZawada, A. M., Griesshaber, B., Ottillinger, B., Erlenkötter, A., Crook, N., Boyington, S., Stauss-Grabo, M., Kennedy, J. P., & Lang, T. (2025). Development and Investigation of a New Polysulfone Dialyzer with Increased Membrane Hydrophilicity. Membranes, 15(5), 132. https://doi.org/10.3390/membranes15050132






