In Vivo Validation of a Nanostructured Electrospun Polycaprolactone Membrane Loaded with Gentamicin and Nano-Hydroxyapatite for the Treatment of Periodontitis
Abstract
1. Introduction
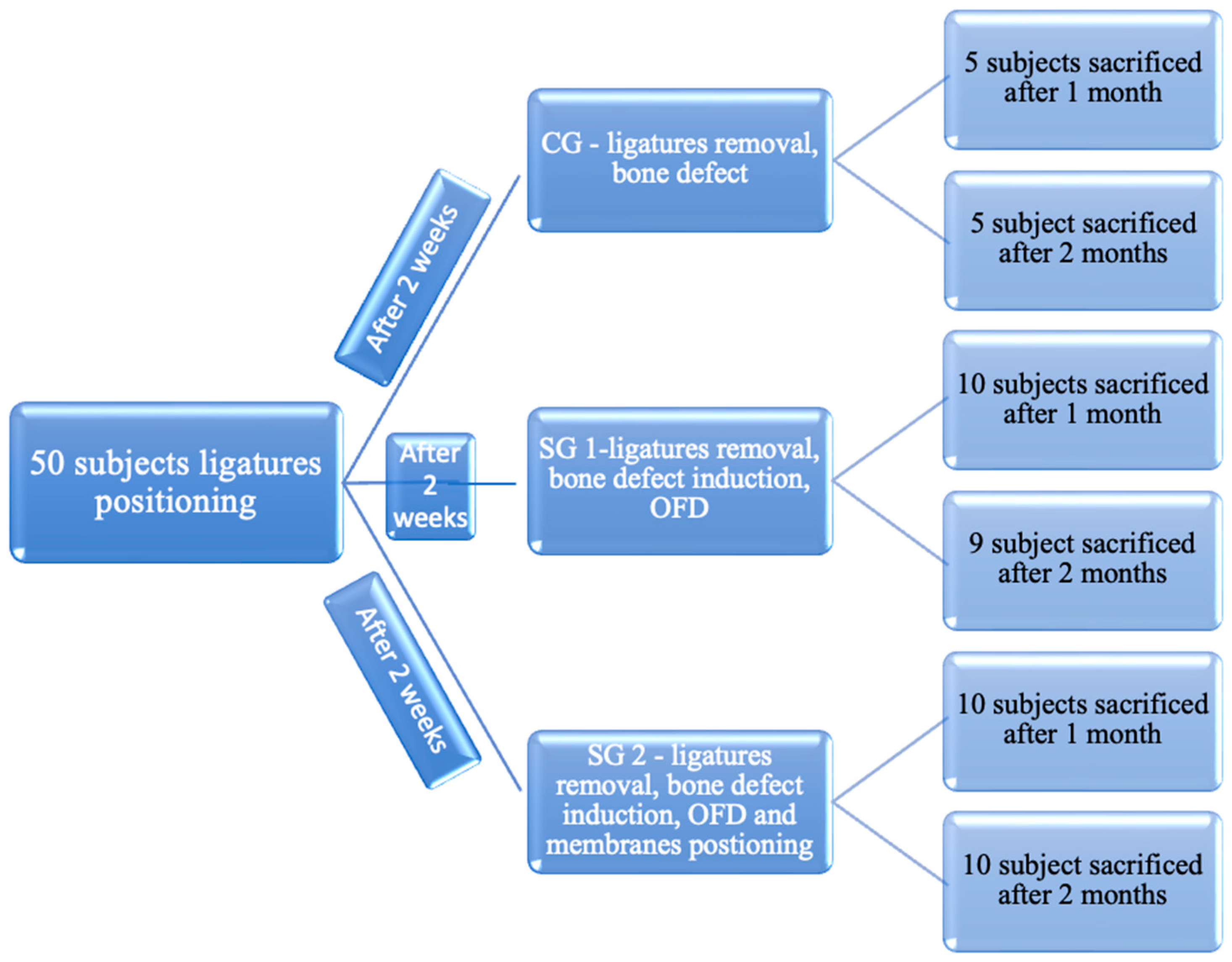
2. Materials and Methods
2.1. The Method of Obtaining the NM
2.2. In Vitro Assays of the NM
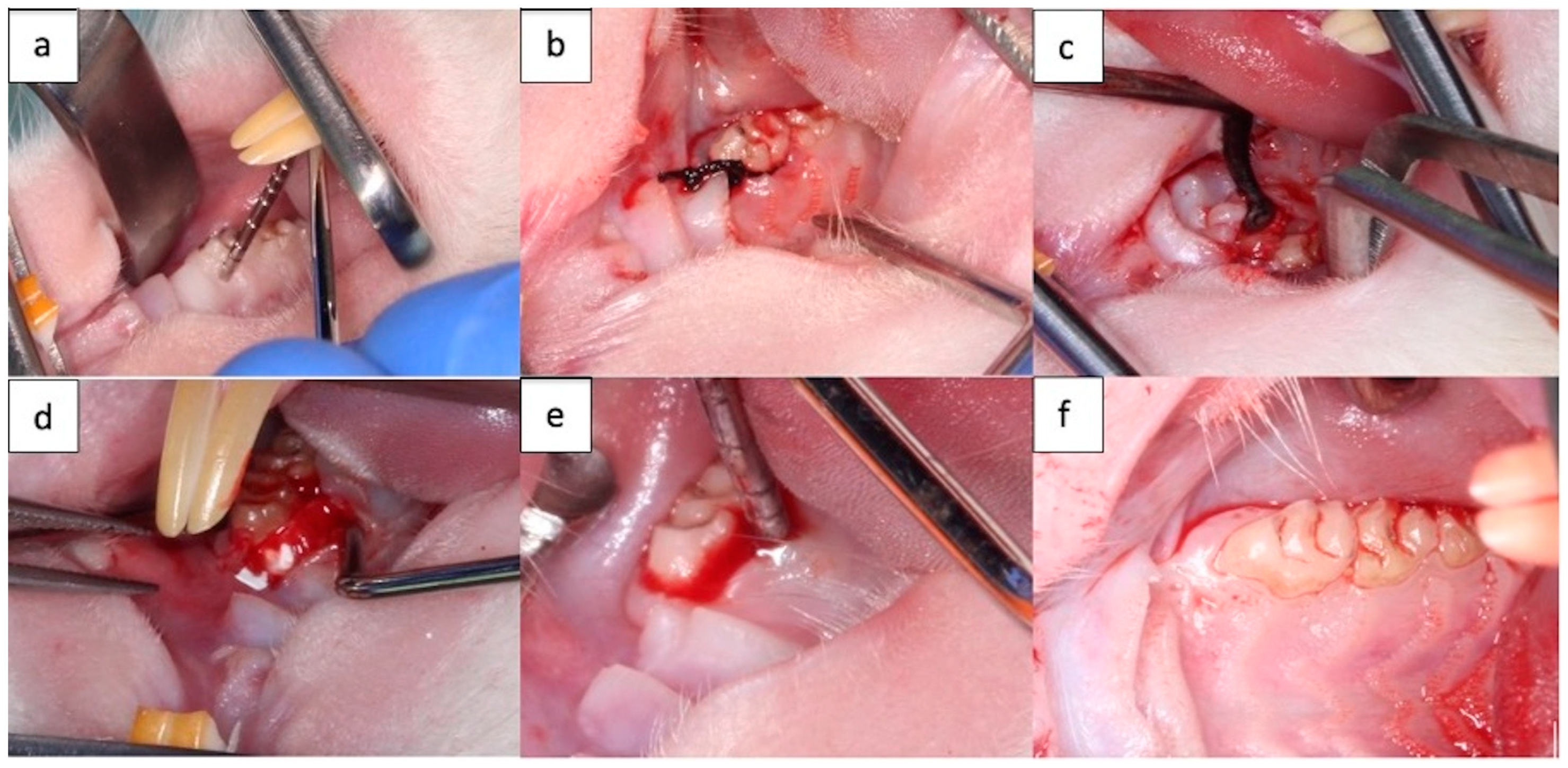
2.3. Rat Periodontal Defect Model Preparation
2.4. Clinical Observation
2.5. Microbiological Analysis
2.6. Blood and Saliva Samples
2.7. Histological Analysis
2.8. Statistical Analysis
3. Results
3.1. Clinical Assessment
3.1.1. The Effects of Ligature Placement (Procedure 1)
3.1.2. The Effects of the Intermediate Procedure Applied after Removing the Ligature
Changes to the Weight of the Subjects
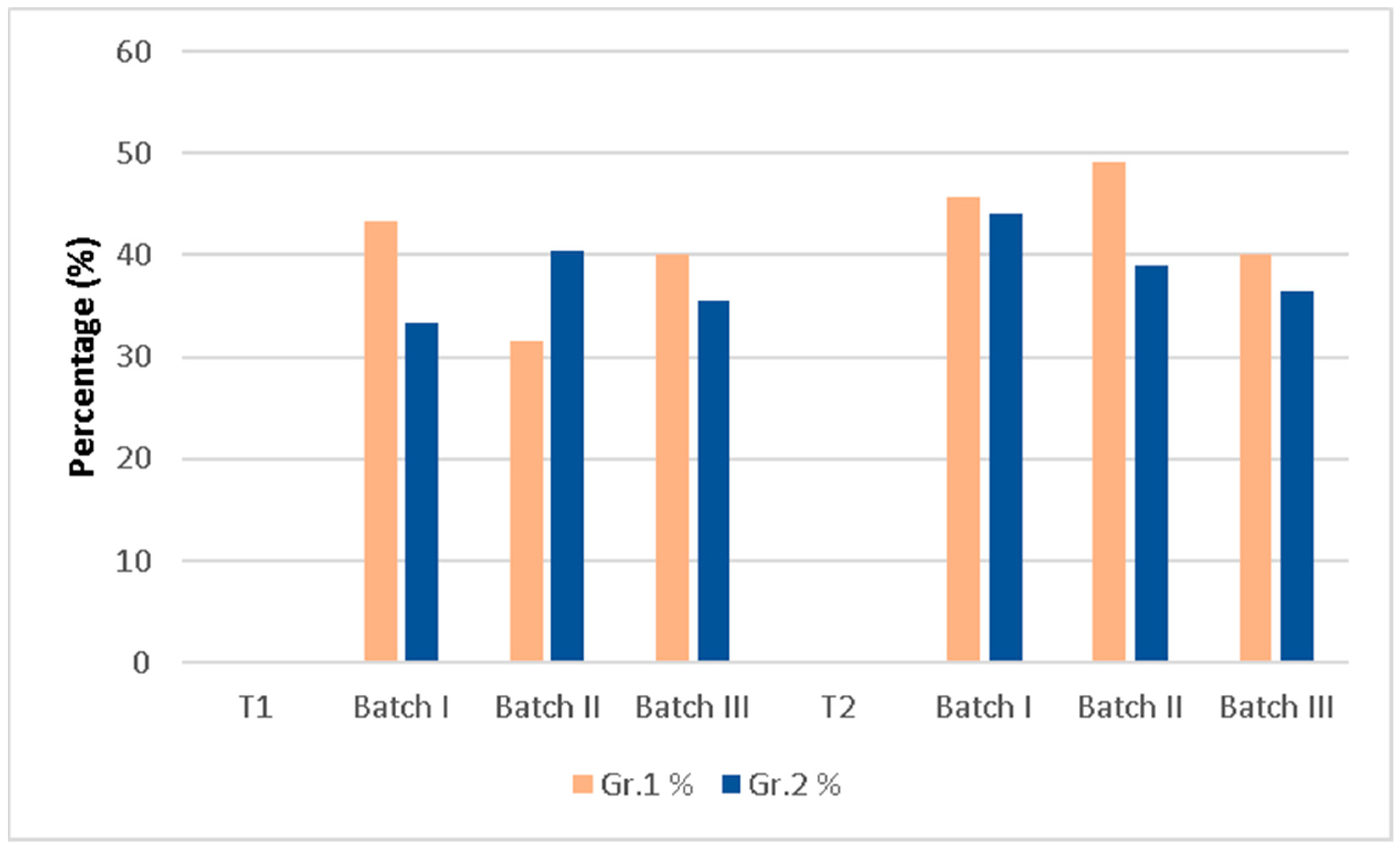
Probing Depths (PD)
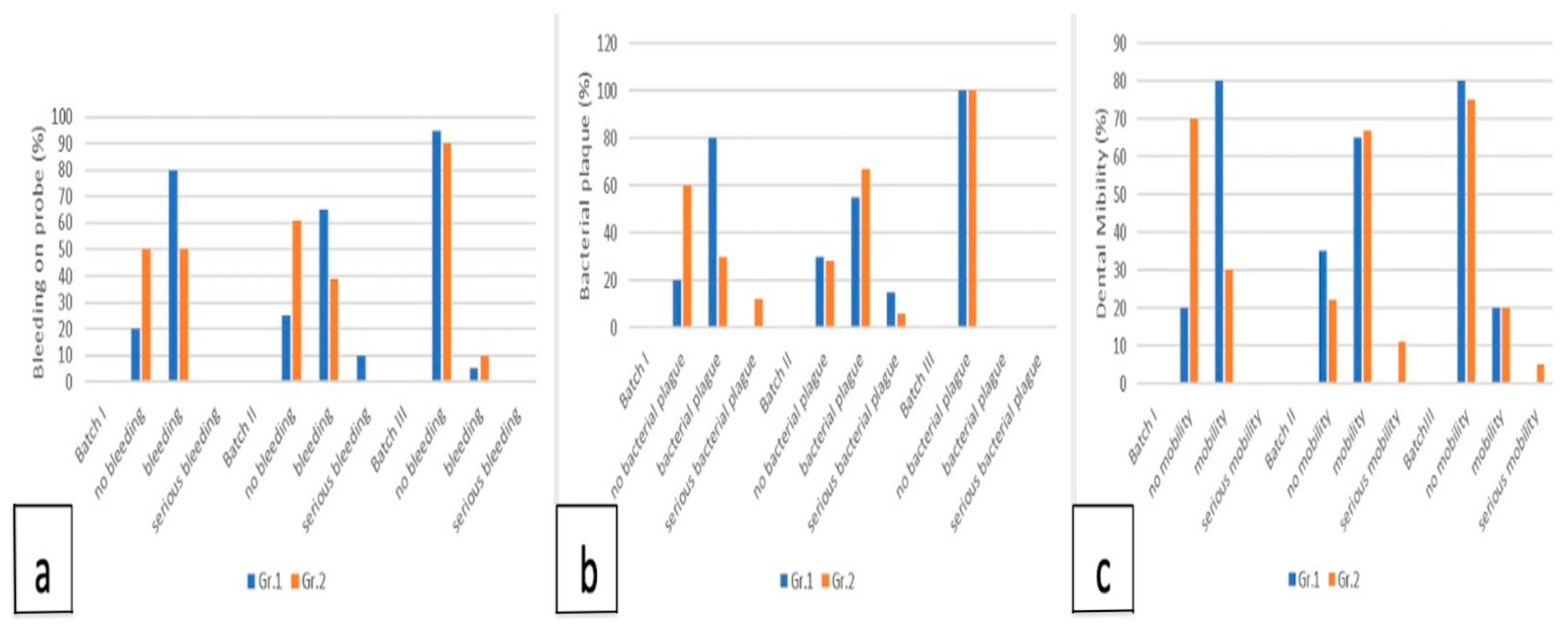
Bleeding on Probing, Dental Mobility, Bacterial Plaque
3.2. Microbiological Analysis
3.2.1. The Effects of Ligature Placement on NTG and Microbiological Flora
3.2.2. The Effects of the Intermediate Procedure Applied after Removing the Ligature on NTG and Pathogenic Flora
NTG
Pathogenic Flora
3.3. Blood and Saliva Sample Results
3.3.1. The Effect of the Ligature on MMP-8 and CRP
3.3.2. The Effect of the Intermediate Procedure on MMP-8 and CRP
Correlation for MMP-8
Correlation for CRP
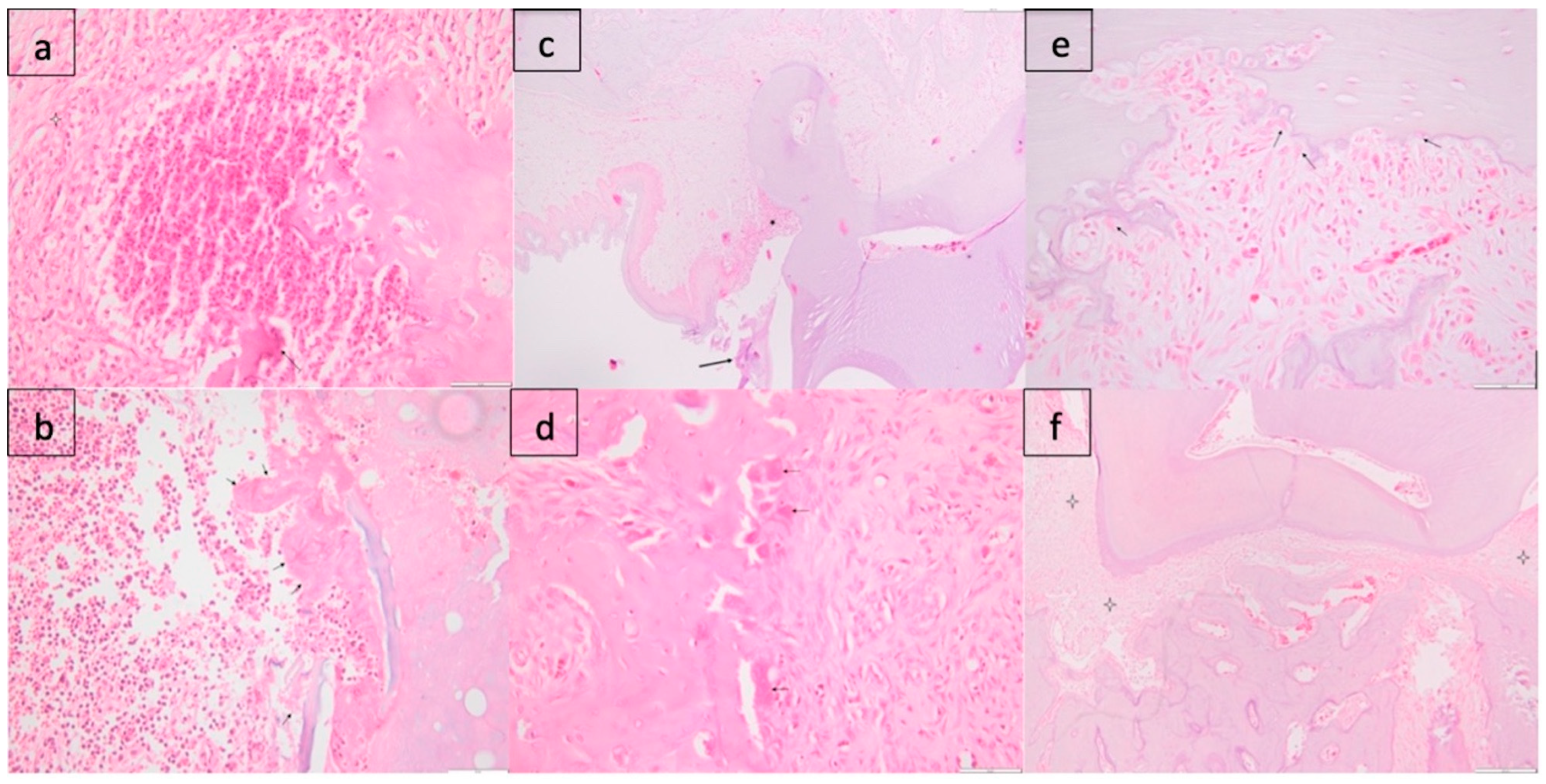
3.4. Histological Analysis
3.4.1. Batch I
Gr. 1
Gr. 2
3.4.2. Batch II
Gr. 1
Gr. 2
3.4.3. Batch III
Gr. 1
Gr. 2
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pihlstrom, B.L.; Michalowicz, B.S.; Johnson, N.W. Periodontal diseases. Lancet 2005, 366, 1809–1820. [Google Scholar] [CrossRef]
- Brown, L.J.; Johns, B.A.; Wall, T.P. The economics of periodontal diseases. Periodontol. 2000 2002, 29, 223–234. [Google Scholar] [CrossRef]
- De Pablo, P.; Chapple, I.L.; Buckley, C.D.; Dietrich, T. Periodontitis in systemic rheumatic diseases. Nat. Rev. Rheumatol. 2009, 5, 218–224. [Google Scholar] [CrossRef]
- Desvarieux, M.; Demmer, R.T.; Rundek, T.; Boden-Albala, B.; Jacobs, D.R., Jr.; Sacco, R.L.; Papapanou, P.N. Periodontal microbiota and carotid intima-media thickness: The Oral Infections and Vascular Disease Epidemiology Study (INVEST). Circulation 2005, 111, 576–582. [Google Scholar] [CrossRef]
- Xiong, X.; Buekens, P.; Fraser, W.D.; Beck, J.; Offenbacher, S. Periodontal disease and adverse pregnancy outcomes: A systematic review. BJOG 2006, 113, 135–143. [Google Scholar] [CrossRef] [PubMed]
- Holt, S.C.; Ebersole, J.L. Porphyromonas gingivalis, Treponema denticola, and Tannerella forsythia: The ‘red complex’, a prototype polybacterial pathogenic consortium in periodontitis. Periodontol. 2000 2005, 38, 72–122. [Google Scholar] [CrossRef] [PubMed]
- Chapple, I.L.C. Reactive oxygen species and antioxidants in inflammatory diseases. J. Clin. Periodontol. 1997, 24, 287–296. [Google Scholar] [CrossRef] [PubMed]
- Chapple, I.L.C.; Brock, G.; Eftimiadi, C.; Matthews, J.B. Glutathione in gingival crevicular fluid and its relation to local antioxidant capacity in periodontal health and disease. J. Clin. Pathol. Mol. Pathol. 2002, 55, 367–373. [Google Scholar] [CrossRef] [PubMed]
- Kesavalu, L.; Bakthavatchalu, V.; Rahman, M.M.; Su, J.; Raghu, B.; Dawson, D.; Fernandes, G.; Ebersole, J.L. Omega-3 fatty acid regulates inflammatory cytokine/mediator messenger RNA expression in Porphyromonas gingivalis-induced experimental periodontal disease. Oral Microbiol. Immunol. 2007, 22, 232–239. [Google Scholar] [CrossRef]
- Waddington, R.J.; Moseley, R.; Embery, G. Reactive oxygen species: A potential role in the pathogenesis of periodontal diseases. Oral Dis. 2000, 6, 138–151. [Google Scholar] [CrossRef]
- Enwonwu, C.O. Cellular and molecular effects of malnutrition and their relevance to periodontal diseases. J. Clin. Periodontol. 1994, 21, 643–657. [Google Scholar] [CrossRef] [PubMed]
- Enwonwu, C.O. Interface of malnutrition and periodontal diseases. Am. J. Clin. Nutr. 1995, 61, 430S–436S. [Google Scholar] [CrossRef] [PubMed]
- Kowashi, Y.; Jaccard, F.; Cimasoni, G. Sulcular polymorphonuclear leucocytes and gingival exudate during experimental gingivitis in man. J. Periodontal Res. 1980, 15, 152–158. [Google Scholar] [CrossRef]
- Gustafsson, A. Increased release of free oxygen radicals from peripheral neutrophils in adult periodontitis after Fcγ-receptor stimulation. J. Clin. Periodontol. 1996, 23, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Key, L.L., Jr.; Wolf, W.C.; Gundberg, C.M.; Ries, W.L. Superoxide and bone resorption. Bone 1994, 15, 431–436. [Google Scholar] [CrossRef]
- Bretz, W.A.; Weyant, R.J.; Corby, P.M.; Ren, D.; Weissfeld, L.; Kritchevsky, S.B.; Harris, T.; Kurella, M.; Satterfield, S.; Visser, M.; et al. Systemic inflammatory markers, periodontal diseases, and periodontal infections in an elderly population. J. Am. Geriatr. Soc. 2005, 53, 1532–1537. [Google Scholar] [CrossRef]
- Ebersole, J.L.; Taubman, M.A. The protective nature of host responses in periodontal diseases. Periodontol. 2000 1994, 5, 112–141. [Google Scholar] [CrossRef]
- Garlet, G.P.; Martins, W., Jr.; Fonseca, B.A.L.; Ferreira, B.R.; Silva, J.S. Matrix metalloproteinases, their physiological inhibitors and osteoclast factors are differentially regulated by the cytokine profile in human periodontal disease. J. Clin. Periodontol. 2004, 31, 671–679. [Google Scholar] [CrossRef]
- Rathnayake, N.; Gieselmann, D.R.; Heikkinen, A.M.; Tervahartiala, T.; Sorsa, T. Salivary Diagnostics—Point-of-Care diagnostics of MMP-8 in dentistry and medicine. Diagnostics 2017, 7, 7. [Google Scholar] [CrossRef]
- Sharma, C.G.; Pradeep, A.R. Gingival crevicular fluid osteopontin levels in periodontal health and disease. J. Periodontol. 2006, 77, 1674–1680. [Google Scholar] [CrossRef]
- Ardite, E.; Sans, M.; Panés, J.; Romero, F.J.; Piqué, J.M.; Fernández-Checa, J.C. Replenishment of glutathione levels improves mucosal function in experimental acute colitis. Lab. Investig. 2000, 80, 735–744. [Google Scholar] [CrossRef]
- Becker, W.; Becker, B.E.; Ochsenbein, C.; Kerry, G.; Caffesse, R.; Morrison, E.C.; Prichard, J. A longitudinal study comparing scaling, osseous surgery and modified Widman procedures: Results after one year. J. Periodontol. 1988, 59, 351–365. [Google Scholar] [CrossRef] [PubMed]
- Caton, J.; Nyman, S.; Zander, H. Histometric evaluation of periodontal surgery. II. Connective tissue attachment levels after four regenerative procedures. J. Clin. Periodontol. 1980, 7, 224–231. [Google Scholar] [CrossRef] [PubMed]
- Kaldahl, W.B.; Kalkwarf, K.L.; Patil, K.D.; Molvar, M.P.; Dyer, J.K. Long-term evaluation of periodontal therapy: I. Response to 4 therapeutic modalities. J. Periodontol. 1996, 67, 93–102. [Google Scholar] [CrossRef]
- Bowers, G.M.; Chadroff, B.; Carnevale, R.; Mellonig, J.; Corio, R.; Emerson, J.; Stevens, M.; Romberg, E. Histologic evaluation of new attachment apparatus formation in humans: Part III. J. Periodontol. 1989, 60, 683–693. [Google Scholar] [CrossRef]
- Buser, D.; Brägger, U.; Lang, N.; Nyman, S. Regeneration and enlargement of jaw bone using guided tissue regeneration. Clin. Oral Implant. Res. 1990, 1, 22–32. [Google Scholar] [CrossRef] [PubMed]
- Garrett, S. Periodontal regeneration around natural teeth. Ann. Periodontol. 1996, 1, 621–666. [Google Scholar] [CrossRef]
- Bunyaratavej, P.; Wang, H.L. Collagen membranes: A review. J. Periodontol. 2001, 72, 215–229. [Google Scholar] [CrossRef]
- Qasim, S.B.; Delaine-Smith, R.M.; Fey, T.; Rawlinson, A.; Rehman, I.U. Freeze gelated porous membranes for periodontal tissue regeneration. Acta Biomater. 2015, 23, 317–328. [Google Scholar] [CrossRef]
- Lee, B.S.; Lee, C.C.; Wang, Y.P.; Chen, H.J.; Lai, C.H.; Hsieh, W.L.; Chen, Y.W. Controlled-release of tetracycline and lovastatin by PLGA-chitosan nanoparticles enhances periodontal regeneration in dogs. Int. J. Nanomed. 2016, 11, 285–297. [Google Scholar] [CrossRef]
- Monteiro, N.; Martins, M.; Martins, A.; Fonseca, N.A.; Moreira, J.o.N.; Reis, R.L.; Neves, N.M. Antibacterial activity of chitosan nanofiber meshes with liposomes immobilized releasing gentamicin. Acta Biomater. 2015, 18, 196–205. [Google Scholar] [CrossRef]
- Yamano, S.; Haku, K.; Yamanaka, T.; Dai, J.; Takayama, T.; Shohara, R.; Tachi, K.; Ishioka, M.; Hanatani, S.; Karunagaran, S. The effect of a bioactive collagen membrane releasing PDGF or GDF-5 on bone regeneration. Biomaterials 2014, 35, 2446–2453. [Google Scholar] [CrossRef] [PubMed]
- Korkusuz, F.; Korkusuz, P.; Ekşioĝlu, F.; Gürsel, I.; Hasirci, V. In vivo response to biodegradable controlled antibiotic release systems. J. Biomed. Mater. Res. 2001, 55, 217–228. [Google Scholar] [CrossRef] [PubMed]
- Taubes, G. The bacteria fight back. Science 2008, 321, 35661. [Google Scholar] [CrossRef] [PubMed]
- Bailey, S.R. Local drug delivery: Current applications. Prog. Cardiovasc. Dis. 1997, 40, 193–204. [Google Scholar] [CrossRef] [PubMed]
- Osorio, R.; Alfonso-Rodriguez, C.A.; Medina-Castillo, A.L.; Alaminos, M.; Toledano, M. Bioactive Polymeric Nanoparticles for Periodontal Therapy. PLoS ONE 2016, 11, e0166217. [Google Scholar] [CrossRef]
- Nowzari, H.; Matian, F.; Slots, J. Periodontal pathogens on polytetrafluoroethylene membrane for guided tissue regeneration inhibit healing. J. Clin. Peridontol. 1995, 22, 469–474. [Google Scholar] [CrossRef]
- Sariibrahimoglu, K.; Yang, W.; Leeuwenburgh, S.C.G.; Yang, F.; Wolke, J.G.C.; Zuo, Y.; Li, Y.; Jansen, J.A. Development of porous polyurethane/strontium-substituted hydroxyapatite composites for bone regeneration. J. Biomed. Mater. Res. A 2015, 103, 1930–1939. [Google Scholar] [CrossRef]
- Bottino, M.C.; Thomas, V.; Janowski, G.M. A novel spatially designed and functionally graded electrospun membrane for periodontal regeneration. Acta Biomater. 2011, 7, 216–224. [Google Scholar] [CrossRef] [PubMed]
- Mirica, I.-C.; Furtos, G.; Moldovan, M.; Prodan, D.; Petean, I.; Campian, R.-S.; Pall, E.; Lucaciu, O. Morphology, Cytotoxicity, and Antimicrobial Activity of Electrospun Polycaprolactone Biomembranes with Gentamicin and Nano-Hydroxyapatite. Membranes 2024, 14, 10. [Google Scholar] [CrossRef]
- Mirică, I.C.; Furtos, G.; Lucaciu, O.; Păscuţa, P.; Vlassa, M.; Moldovan, M.; Câmpian, R.S. Electrospun membranes based on polycaprolactone, nano-Hydroxyapatite and metronidazole. Materials 2021, 14, 931. [Google Scholar] [CrossRef] [PubMed]
- Lehmann, N.; Christ, T.; Daugs, A.; Bloch, O.; Holinski, S. EDC-crosslinking of decellularized tissue-a promising approach? Tissue Eng. Part A 2017, 13, 675–682. [Google Scholar] [CrossRef] [PubMed]
- Boșca, A.B.; Dinte, E.; Colosi, H.; Ilea, A.; Câmpian, R.S.; Uifălean, A.; Parvu, A.E. Curcumin effect on nitro-oxidative stress in ligature-induced rat periodontitis. Rom. Biotechnol. Lett. 2015, 20, 10708–10717. [Google Scholar]
- Diaz Padilla, N.; Bleeker, W.K.; Lubbers, Y.; Rigter, G.M.; Van Mierlo, G.J.; Daha, M.R.; Hack, C.E. Rat C-reactive protein activates the autologous complement system. Immunology 2003, 109, 564–571. [Google Scholar] [CrossRef] [PubMed]
- Statitics Kingdom. Available online: https://www.statskingdom.com/shapiro-wilk-test-calculator.html (accessed on 5 January 2024).
- Jeremy Stangroom. Social Science Statistics. 2023. Available online: https://www.socscistatistics.com/ (accessed on 29 December 2023).
- Li, N.; Jiang, L.; Jin, H.; Wu, Y.; Liu, Y.; Huang, W.; Wei, L.; Zhou, Q.; Chen, F.; Gao, Y.; et al. An enzyme-responsive membrane for antibiotic drug release and local periodontal treatment. Colloids Surf. B Biointerfaces 2019, 183, 110454. [Google Scholar] [CrossRef] [PubMed]
- Nasajpour, A.; Ansari, S.; Rinoldi, C.; Rad, A.S.; Aghaloo, T.; Shin, S.R.; Mishra, Y.K.; Adelung, R.; Swieszkowski, W.; Annabi, N.; et al. A Multifunctional Polymeric Periodontal Membrane with Osteogenic and Antibacterial Characteristics. Adv. Funct. Mater. 2018, 28, 1703437. [Google Scholar] [CrossRef]
- Liu, X.; He, X.; Jin, D.; Wu, S.; Wang, H.; Yin, M.; Aldalbahi, A.; El-Newehy, M.; Mo, X.; Wu, J. A biodegradable multifunctional nanofibrous membrane for periodontal tissue regeneration. Acta Biomater. 2020, 108, 207–222. [Google Scholar] [CrossRef]
- Ren, S.; Zhou, Y.; Zheng, K.; Xu, X.; Yang, J.; Wang, X.; Miao, L.; Wei, H.; Xu, Y. Cerium oxide nanoparticles loaded nanofibrous membranes promote bone regeneration for periodontal tissue engineering. Bioact. Mater. 2021, 7, 242–253. [Google Scholar] [CrossRef]
- Shang, L.; Liu, Z.; Ma, B.; Shao, J.; Wang, B.; Ma, C.; Ge, S. Dimethyloxallyl glycine/nanosilicates-loaded osteogenic/angiogenic difunctional fibrous structure for functional periodontal tissue regeneration. Bioact. Mater. 2020, 6, 1175–1188. [Google Scholar] [CrossRef]


| T0 | T1 | p-Value | ||
|---|---|---|---|---|
| Weight (g) ± SE | 307.55 ± 3.34 | 291.87 ± 4.42 | p < 0.0001 | |
| Probing Depths (mm) ± SE | 0.212 ± 0.01 | 1.1153 ± 0.02 | p < 0.0001 | |
| Bleeding on Probing (No) | 0 | 90 [89 *, 1 **] | 91.83% | |
| Dental Mobility (No) | 0 | 72 [55 *, 13 **, 4 ***] | 73.46% | |
| Bacterial plaque (No) | 0 | 74 [58 *, 14 **,2 ***] | 75.51% |
| Average Values (g) ± SE | m1 (g) at T1 | m2 (g) at T2 | Correlation between Groups Correlation between Batches |
|---|---|---|---|
| Batch 1 | BIII vs. BI Gr. 2 p = 0.044045 | ||
| Gr. 1 | 299.6 ± 13.17 | 300.8 ± 10.16 | p = 0.00843 |
| Gr. 2 | 298.6 ± 12.44 | 343.2 ± 13.32 | |
| Batch II | BIII vs. BII Gr. 1 p = 0.03689 | ||
| Gr. 1 | 263.7 ± 11.16 | 286.1 ± 13.49 | p = 0.002409 |
| Gr. 2 | 301.4 ± 10.41 | 339.9 ± 8.85 | |
| Batch III | B III vs. BII Gr. 2 p = 0.012545 | ||
| Gr. 1 | 286.1 ± 7.71 | 317.1 ± 9.01 | p = 0.000288 |
| Gr. 2 | 310.0 ± 4.57 | 370.1 ± 8.52 |
| Average Values (mm) ± SE | PD (mm) at T1 | PD (mm) at T2 | Correlation between Batches |
|---|---|---|---|
| Batch 1 | B II vs. B I Gr. 2 p = 0.0294 | ||
| Gr. 1 | 1.00 ± 0.01 | 0.92 ± 0.04 | |
| Gr. 2 | 1.03 ± 0.02 | 0.83 ± 0.15 | B III vs. B I Gr. 2 p = 0.0006 |
| Batch II | B III vs. B I Gr. 1 p = 0.0004 | ||
| Gr. 1 | 1.29 ± 0.08 | 0.94 ± 0.08 | |
| Gr. 2 | 1.09 ± 0.03 | 1.02 ± 0.08 | B III vs. B II Gr. 2 p < 0.0001 |
| Batch III | B III vs. B II Gr. 1 p < 0.0001 | ||
| Gr. 1 | 1.12 ± 0.04 | 0.42 ± 0.05 | |
| Gr. 2 | 1.07 ± 0.047 | 0.24 ± 0.047 |
| NTG (×1000 UFC/mL) (No) | No at T0 | No at T1 | % at T0/T1 | p |
|---|---|---|---|---|
| <1 | 46 | 2 | 91.84%/4.08% | p < 0.00001 |
| 1–3 | 2 | 19 | 4.08%/38.77% | χ2 = 73.2383 |
| >3 | 1 | 28 | 2.04%/57.14% | |
| Pathogenic Flora (No) | Abundance (%) | |||
| Streptococcus mutans | 12 (total) 12 * | 31 (total), 27 *** | 28.7 25 | χ2 = 44.219, p < 0.0001 |
| Staphylococcus aureus | 6 (total), 5 * | 36 (total), 8 *** | 33.34 7.41 | χ2 = 24.81, p < 0.0001 |
| Actinomyces weissii | 25 (total) 24 * | 11 (total) 8 *** | 10.19 7.41 | χ2 = 24.81, p < 0.0001 |
| Average Concentration at T0 | Average Concentration at T1 | p | |
|---|---|---|---|
| MMP-8 ng/mL saliva | 99.88 ± 6.93 | 293.95 ± 28.10 | p < 0.0001 |
| CRP μg/mL blood | 271.86 ± 29.07 | 568.33 ± 65.91 | p = 0.0027 |
| Average Concentration at T1 | Average Concentration at T2 | |
|---|---|---|
| Batch I | ||
| Gr. 1 | 191.50 ± 88.50 | 118.65 ± 11.27 |
| Gr. 2 | 193.28 ± 148.37 | 163.83 ± 11.27 |
| Bath II | ||
| Gr. 1 | 377.25 ± 274.54 | 119.12 ± 55.56 |
| Gr. 2 | 332.32 ± 255.68 | 207.23 ± 41.21 |
| Batch III | ||
| Gr. 1 | 584.49 ± 264.39 | 112.41 ± 26.49 |
| Gr. 2 | 325.38 ± 173.83 | 172.23 ± 141.51 |
| Average Concentration at T1 (μg/mL) | Average Concentration at T2 (μg/mL) | ||
|---|---|---|---|
| Batch I | Gr. 1 | 304.44 ± 63.03 | 295.55 ± 38.07 |
| Gr. 2 | 656.00 ± 200.7 | 572.00 ± 132.5 | |
| Batch II | Gr. 1 | 454.00 ± 305.42 | 370.55 ± 258.87 |
| Gr. 2 | 551.66 ± 118.98 | 515.55 ± 99.36 | |
| Batch III | Gr. 1 | 744.00 ± 17.28 | 558.80 ± 141.69 |
| Gr.2 | 559.00 ± 131.60 | 465.50 ± 87.65 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lucaciu, P.O.; Repciuc, C.C.; Matei, I.A.; Fiț, N.I.; Andrei, S.; Marica, R.; Petrescu, B.N.; Crișan, B.; Aghiorghiesei, O.; Mirică, I.C.; et al. In Vivo Validation of a Nanostructured Electrospun Polycaprolactone Membrane Loaded with Gentamicin and Nano-Hydroxyapatite for the Treatment of Periodontitis. Membranes 2024, 14, 60. https://doi.org/10.3390/membranes14030060
Lucaciu PO, Repciuc CC, Matei IA, Fiț NI, Andrei S, Marica R, Petrescu BN, Crișan B, Aghiorghiesei O, Mirică IC, et al. In Vivo Validation of a Nanostructured Electrospun Polycaprolactone Membrane Loaded with Gentamicin and Nano-Hydroxyapatite for the Treatment of Periodontitis. Membranes. 2024; 14(3):60. https://doi.org/10.3390/membranes14030060
Chicago/Turabian StyleLucaciu, Patricia Ondine, Călin Cosmin Repciuc, Ioana A. Matei, Nicodim I. Fiț, Sanda Andrei, Raluca Marica, Bianca Nausica Petrescu, Bogdan Crișan, Ovidiu Aghiorghiesei, Ioana Codruța Mirică, and et al. 2024. "In Vivo Validation of a Nanostructured Electrospun Polycaprolactone Membrane Loaded with Gentamicin and Nano-Hydroxyapatite for the Treatment of Periodontitis" Membranes 14, no. 3: 60. https://doi.org/10.3390/membranes14030060
APA StyleLucaciu, P. O., Repciuc, C. C., Matei, I. A., Fiț, N. I., Andrei, S., Marica, R., Petrescu, B. N., Crișan, B., Aghiorghiesei, O., Mirică, I. C., Apostu, D., Saroși, C., Onișor, F., Vanea, E., Iușan, S. A. L., Mureșan, G. C., Condor, A.-M., Oprița, E., & Gherman, L.-M. (2024). In Vivo Validation of a Nanostructured Electrospun Polycaprolactone Membrane Loaded with Gentamicin and Nano-Hydroxyapatite for the Treatment of Periodontitis. Membranes, 14(3), 60. https://doi.org/10.3390/membranes14030060











