Abstract
Background: In this retrospective study, we report the effectiveness and safety of a dedicated extracorporeal carbon dioxide removal (ECCO2R) device in critically ill patients. Methods: Adult patients on mechanical ventilation due to acute respiratory distress syndrome (ARDS) or decompensated chronic obstructive pulmonary disease (dCOPD), who were treated with a dedicated ECCO2R device (CO2RESET, Eurosets, Medolla, Italy) in case of hypercapnic acidemia, were included. Repeated measurements of CO2 removal (VCO2) at baseline and 1, 12, and 24 h after the initiation of therapy were recorded. Results: Over a three-year period, 11 patients received ECCO2R (median age 60 [43–72] years) 3 (2–39) days after ICU admission; nine patients had ARDS and two had dCOPD. Median baseline pH and PaCO2 levels were 7.27 (7.12–7.33) and 65 (50–84) mmHg, respectively. With a median ECCO2R blood flow of 800 (500–800) mL/min and maximum gas flow of 6 (2–14) L/min, the VCO2 at 12 h after ECCO2R initiation was 157 (58–183) mL/min. Tidal volume, respiratory rate, and driving pressure were significantly reduced over time. Few side effects were reported. Conclusions: In this study, a dedicated ECCO2R device provided a high VCO2 with a favorable risk profile.
1. Introduction
Mechanical ventilation (MV) is a crucial intervention for patients with severe respiratory insufficiency who cannot maintain effective gas exchange through spontaneous breathing [1]. However, numerous detrimental consequences of MV have been identified, including lung over-inflation, oxygen toxicity, right ventricular failure, and ventilator-associated pneumonia (VAP), which have a profound impact on the management of ventilated patients [2,3]. In patients with acute respiratory failure, a ventilation strategy designed to minimize alveolar damage associated with MV, i.e., ventilator-induced lung injury (VILI), such as a low tidal volume approach, has been shown to effectively decrease mortality [4,5].
Recent studies have proposed a modern ventilatory approach (“mechanical load sparing”) based on the concept of protective ventilation, which includes small tidal volumes, low respiratory rates, and limited plateau pressures, even for patients with decompensated chronic obstructive pulmonary disease (COPD) in the peri- and post-operative setting [6,7]. However, this approach is challenging to implement due to the risk of hypercapnia, which is associated with pulmonary hypertension, decreased renal blood flow, and the release of endogenous catecholamines [8]. An adjuvant strategy, such as partial extracorporeal carbon dioxide removal (ECCO2R) using a dedicated device, appears to be an attractive solution to control hypercapnia in this setting [9].
ECCO2R involves an extracorporeal device operating on one or two venous access, a blood pump, a membrane lung, and a sweep gas system; the low blood flow (0.4–1.0 L/min) generated can provide CO2 removal without significant effect on blood oxygenation and target arterial CO2 (PaCO2) can be easily achieved by adjusting the sweep gas flow through the membrane lung [9,10]. However, for lower ranges of blood flow (i.e., 0.4 L/min), the membrane lung is often incorporated into continuous renal replacement therapy (CRRT) [9,11]. This implementation may be limited by the capability of CRRT devices to achieve such blood flows and by the smaller cannulas used for dialysis catheters, which could increase the risk of flow turbulence and hemolysis [12]. Moreover, lower CO2 extraction devices (i.e., low blood flow and low surface area) have been associated with a lower proportion of patients achieving adequate CO2 removal and a higher incidence of hemolysis and bleeding than higher CO2 extraction devices (i.e., higher blood flow and larger membrane surface area) [13]. Furthermore, full extracorporeal membrane oxygenation (ECMO) is frequently employed to perform CO2 removal at high ranges of blood flow (i.e., 1.0 L/min). However, this approach is associated with a similar rate of complications, economic burden, and organizational issues as ECMO use [14].
A new device has been recently made available on the market, which is entirely dedicated to ECCO2R with a reasonably high maximum blood flow (i.e., 0.8 L/min). This device produces a high CO2 removal rate of up to 150 mL/min in an animal model of induced hypercapnia [15]. However, human data on the effectiveness of such device are lacking. Therefore, the aim of this study was to assess the effectiveness and safety of a novel ECCO2R system in the removal of CO2 in patients with acute severe hypercapnia requiring MV.
2. Materials and Methods
2.1. Study Design
This was a retrospective multicentric study that included all adult (>18 years of age) patients treated with ECCO2R (CO2RESET—Eurosets, Medolla, Italy) in participating centers according to the decision of the treating physician for (a) acute respiratory distress syndrome (ARDS) or decompensated chronic obstructive pulmonary disease (dCOPD) and (b) pH < 7.25 and PaCO2 > 60 mmHg despite the optimal setting of MV. Separate ethics approval for this study was obtained from each participating center (i.e., Brussels, Modena and Pavia), and informed consent was waived because of the retrospective nature of the study. The study was conducted according to the requirements of the Declaration of Helsinki.
2.2. Intervention
CO2RESET is a CE-marked device that includes a new volumetric capnometer. It has a roller pump and a maximum blood flow of 800 mL/min. The membrane lung surface area is 1.81 m2 and the priming volume is 120 mL (Figure 1).

Figure 1.
Representation of the CO2RESET device (left) and the membrane lung (right).
This device incorporates a mid-range infrared sensor placed in the mainstream, unlike standard devices that use side-stream sampling, at the membrane lung exhaust connector. Additionally, a flow sensor device is situated at the membrane lung sweep gas inlet. The concentration of CO2 is calculated based on the CO2 absorption characteristics of the radiation variation, similar to that of common capnometers. However, the combination of the capnometer and flowmeter allows for the continuous evaluation of the percentage of CO2 exhaust by the membrane lung, as well as the continuous calculation of CO2 removal (VCO2, mL/min). The VCO2 measurement has been validated using standard measurements [16]. Furthermore, a temperature control system placed inside the capnometer measuring cell maintains the temperature of the gas exhaust between 40 and 42 °C, preventing condensation and misleading measurements. Ultimately, dedicated software tools analyze the measurements and display the inlet gas flow, pre- and post-membrane lung pressures, and VCO2.
This medical equipment is intended for extracorporeal CO2 removal and is designed to be used in hypercapnic patients receiving mechanical ventilation. In all participating centers, CO2RESET was implanted percutaneously using either two heparin-coated cannulas or a single-vessel (i.e., double-lumen) cannulation, according to local practices and availability. The device was not used in case of severe hypoxemia, in case of contraindication to systemic anticoagulation, a body mass index (BMI) <15 or >40 kg/m2, or a moribund patient with do-not-resuscitate orders. CO2RESET priming consisted of a Plasmalyte solution (Baxter Healthcare Corporation, Deerfield, MA, USA). The monitoring of heart and lung function, hemodynamic targets, the initiation of anticoagulants and anticoagulation targets, and thresholds for red blood cell transfusion (RBCT) were left at the discretion of the treating team. Device weaning was decided according to local protocols.
2.3. Data Collection
We gathered demographic data, pre-existing chronic disease history, and admission diagnosis of all patients. The severity of illness was evaluated using the Acute Physiology and Chronic Health Evaluation (APACHE) II score [17] on ICU admission and the Sequential Organ Failure Assessment (SOFA) [18] score on the day ECCO2R was initiated. We documented the requirement for MV, vasoactive agents, anticoagulants, and blood transfusions, as well as the duration of ICU stay and overall ICU and hospital mortalities. ECCO2R data were collected, including indications, configuration, weaning, circuit function, and biological data, on the day of initiation and 24 h after implementation. Arterial blood gas analyses, MV settings, and the use of sedatives and/or neuromuscular blocking agents (NMBAs) at the beginning of ECCO2R, and at 1, 12 (±1), and 24 (±2) h thereafter were also recorded, when feasible. These time points were selected because they were available in all participating centers according to the local monitoring protocols.
2.4. Patients’ Selection and Study Outcomes
The primary outcome was to assess the maximum VCO2 value within the first 12 h of therapy. Secondary outcomes included (a) hospital mortality; (b) weaning from MV; (c) the occurrence of any clinical adverse events, such as moderate or severe bleeding, red blood cell transfusion (RBCT), any cardiac arrhythmias, hypotension, the need for vasopressors, and the occurrence of cardiac arrest; (d) the occurrence of adverse events associated with the extracorporeal device, including kinking of tubing, clotting, accidental decannulation, membrane lung failure, pump failure, and circuit damage.
2.5. Statistical Analysis
As this was a retrospective study, no sample size calculation was initially made. However, considering that the expected maximum VCO2 from CO2RESET of 100 (±15) mL/min would be superior to the VCO2 values achieved with other low blood flow devices, i.e., around 45 (±10) mL/min [12,13,19,20], we calculated a posteriori that a sample size of at least 9 patients was, therefore, required to achieve 90% power in detecting a superiority of CO2RESET for the primary endpoint. Data are presented as the median (ranges) or count (%). Data from repeated measures were analyzed using the Kruskal–Wallis test, followed by the Bonferroni post hoc analysis to evaluate differences between each time point. For biological measurements, a Wilcoxon matched-pairs signed rank test was used. All the statistical analyses for this study were performed in R version 3.6.0 (R Foundation for Statistical Computing, Vienna, Austria). The p-values were two-tailed and values < 0.05 were considered statistically significant.
3. Results
3.1. Study Population
Between January 2020 and December 2022, a total of 11 patients received ECCO2R treatment at three participating medical centers (Brussels, n = 8; Modena, n = 2; Pavia, n = 1). The primary baseline characteristics are presented in Table 1. The median age of the patients was 60 (43–72) years. The median APACHE II score upon admission and SOFA score on the day of ECCO2R initiation were 19 (16–24) and 9 (7–10), respectively. Among the patients, nine had ARDS (six with COVID-19 and three with sepsis), while two had dCOPD (one with bacterial infection and the other with viral pulmonary infection). The median times from ICU admission to MV and from ICU admission to ECCO2R initiation were 1 (1–3) days and 3 (2–39) days, respectively. None of the patients required CRRT during the ECCO2R therapy.

Table 1.
Characteristics of the study population. Data are reported as count (%) or median (ranges).
3.2. ECCO2R Implementation
The median baseline pH and PaCO2 levels were 7.27 (7.12–7.33) and 65 (50–84) mmHg, respectively. The median baseline ventilatory settings are presented in Table 2; the median driving pressure was 21 (14–24) cmH2O. Two patients failed prone positioning to improve hypercapnia and ventilatory mechanics, and nine patients were on norepinephrine (median dose of 8 [3–12] mcg/min). At baseline, all patients were receiving continuous infusion of sedatives and opioids, and 10 (91%) patients were administered NMBAs.

Table 2.
Time course of main study variables, including biological testing. Data are presented as median (ranges) or count (%).
Regarding configuration, all patients received dual-site cannulation, with the drainage cannula inserted via the femoral (n = 7) or left subclavian (n = 4) vein, with a median cannula size of 18 (16–21) Fr. A return cannula was inserted via the right jugular vein in all patients, with a median cannula size of 15 (15–18) Fr. The median duration of ECCO2R was 6 days (3–17) days. Anticoagulation was initiated immediately after ECCO2R implantation using continuous intravenous infusion of unfractionated heparin, targeting an activated clotting time of 160–200 s, as measured by the available devices in each center.
3.3. Primary Outcome
With a median ECCO2R blood flow of 800 (500–800) mL/min and a maximum sweep gas flow of 6 (2–14) L/min, VCO2 at 12 h after ECCO2R initiation was 157 (58–183) mL/min. Compared to the values reported for low-flow ECCO2R devices (i.e., 45 ± 10 mL/min), the observed VCO2 values were significantly higher (p = 0.009). The maximum VCO2 over the first 24 h was 161 (72–188) mL/min; VCO2 values over time are presented in Figure 2.
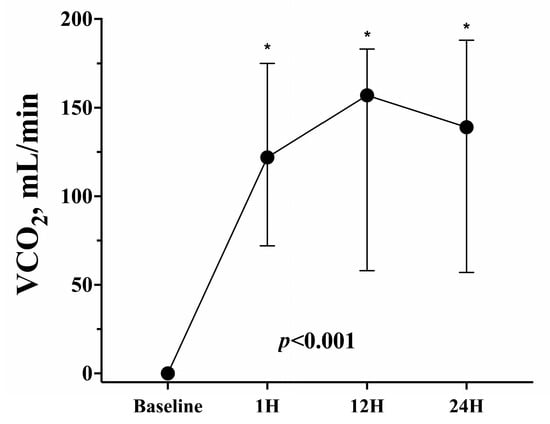
Figure 2.
CO2 removal (VCO2) over time. * indicates significant differences with baseline values.
Tidal volume, respiratory rate, and driving pressure significantly decreased over time when compared to the baseline values (Table 2 and Figure 3). At 24 h, pH was 7.41 (7.35–7.50) and PaCO2 was 45 (39–49) mmHg. The biological changes at 24 h after ECCO2R initiation are reported in Table 2.
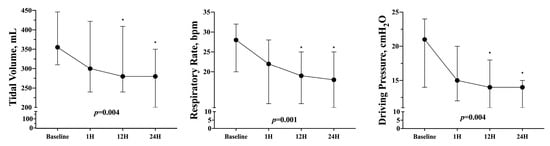
Figure 3.
Tidal volume, respiratory rate, and driving pressure change over time. * indicates significant differences with baseline values.
3.4. Secondary Outcomes
The ECCO2R device was successfully weaned in seven patients (64%). Hospital mortality was observed in seven patients (64%, including three of those in whom ECCO2R was weaned), mainly because of multiple organ failure (n = 3), refractory hypoxemia (n = 3; all patients were not eligible for ECMO), and septic shock (n = 1).
In three patients, a second circuit was required either due to membrane lung clotting (n = 2), occurring after 5 and 6 days, or circuit expiration (n = 1), happening after 7 days. One instance of device malfunction was observed in the first treated patient, attributed to a software bug in the heparin syringe calibration, which was eventually resolved without injury to the patient. No pump failure, circuit damage, catheter kinking, or dislodgment was reported. Three patients developed hematomas at the drainage cannulation site, and two of them required red blood cell transfusions (1 and 4 packs) due to bleeding. No cases of air embolism or catheter infection were reported. None of the patients experienced cardiac arrhythmia or cardiac arrest during ECCO2R treatment. No additional patients required vasopressors in the 48 h following ECCO2R initiation.
4. Discussion
The results of this study suggest that ECCO2R, using a dedicated device, is an effective and safe method for managing hypercapnic acidemia in critically ill patients with ARDS or dCOPD. Also, higher blood flow and VCO2 are important advantages over ECCO2R devices used with CRRT. The significant reduction in ventilatory mechanical load observed over time highlights the potential of ECCO2R to reduce ventilator-induced lung injury. Moreover, the low incidence of adverse events associated with CO2RESET in this study is encouraging.
In individuals experiencing acute respiratory failure, ECCO2R is often employed as an adjunct to MV to provide additional support for gas exchange [19]. ECCO2R therapy can be used in critically ill patients with ARDS to facilitate ultra-protective lung ventilation (UPLV) and decrease VILI by reducing tidal volume, driving pressures, and respiratory rate, while also controlling respiratory acidosis [19,20,21]. Additionally, ECCO2R therapy may be implemented in individuals with dCOPD exhibiting severe respiratory acidosis and hypercapnic respiratory failure to avoid intubation in those at risk of non-invasive ventilation failure or to expedite weaning and promote early extubation in individuals requiring MV [22]. Combes et al. demonstrated that the UPLV strategy was feasible in 78% and 82% of patients with moderate ARDS at 8 and 24 h after implementation [21]. However, a secondary analysis of this database showed that UPLV was more frequently achieved in patients with devices having high VCO2 and blood flow compared to lower blood flow, which significantly questioned the role of ECCO2R implemented in CRRT devices in such patients [13]. A recent randomized trial including 412 adult patients receiving MV for acute hypoxemic respiratory failure and randomized to early ECCO2R for UPLV was stopped early due to futility, as ECCO2R to facilitate lower tidal volume ventilation did not significantly reduce 90-day mortality compared to conventional ventilation strategies [23]. Although our results do not add evidence on the effectiveness of ECCO2R on patient-relevant outcomes or on the optimal timing and eligibility criteria to initiate such therapy, we demonstrated that a dedicated ECCO2R device can provide a very high VCO2, which will result in a rapid improvement in gas exchange and ventilatory settings. The significant reduction in tidal volume, driving pressure, and respiratory rate resulted in more protective lung ventilation. Although we did not specifically calculate the mechanical power related to mechanical ventilation nor assess the long-term effects of this ECCO2R device, such a solution could be a suitable and balanced approach to avoid ineffective CO2 removal from low blood flow devices and, perhaps, to avoid the need of ECMO support later on, with a reduced risk of potential side effects.
The membrane of the lung plays a crucial role in extracorporeal CO2 removal. In particular, the surface area of the membrane is an important factor in the ECCO2R device efficacy, as it directly affects the efficiency of gas exchange [24]. A larger surface area allows for greater contact between the blood and gas phase, facilitating the diffusion of CO2 and oxygen across the membrane. Polymeric hollow fiber membranes can provide a much larger surface area than traditional gas absorption towers or liquid extraction columns; the structure of these membranes is designed to be thin and porous, enabling rapid gas exchange while maintaining adequate mechanical strength [25]. As different types of membranes are available for ECCO2R devices, they vary in their characteristics and performance. Some commonly used membranes include polymethylpentene (PMP), polypropylene hollow fibers, and silicone membranes. These membranes differ in their gas permeability, biocompatibility, durability, and resistance to clot formation [26]. The membrane used in the CO2RESET device is more efficient than other low-flow devices in eliminating CO2 while maintaining similar biocompatibility. Moreover, higher blood flow can increase CO2 exchange and minimize the risk of clot formation [27]. Additionally, the durability of the membrane is essential to ensure the longevity of the ECCO2R device. However, it is important to acknowledge that some low-flow devices are available to provide much higher CO2 removal rates (i.e., 75 mL/min), although some data are only related to in vitro models [25]. Furthermore, it is worth noting that other devices have demonstrated VCO2 values of approximately 140 mL/min when utilizing a blood flow rate of 750 mL/min [28]. However, it is important to acknowledge that these findings originated from an animal study and have not yet been replicated in human subjects. Therefore, clinicians must carefully consider the characteristics and efficacy of the ECCO2R device when selecting it for a patient, taking into account the anticipated impact on gas exchange in the treated individual.
Another important finding is the relatively low occurrence of side effects with the CO2RESET device [22,29]. In a previous study, ECCO2R-related episodes of hemolysis and bleeding were higher with lower extraction (n = 33) devices than with higher extraction (n = 62) devices, and adverse events were reported in 39% of patients, including two severe adverse events directly attributed to ECCO2R [13]. Additionally, ECCO2R has been associated with a significantly lower number of ventilator-free days compared to standard care, and serious adverse events were reported in 31% of ECCO2R patients [23]. The reasons for the differences with the existing literature, whether related to the characteristics of the device, the use of higher blood flow, better local anticoagulation practices, patient selection, and/or the use of double cannulation, remain unclear. However, given the inconclusive evidence of its effectiveness and the relatively high number of adverse events reported in previous studies, CO2RESET may represent an appropriate choice to achieve a satisfactory risk/benefit balance with this approach. One patient encountered a severe bleeding incident at the cannulation site, necessitating the administration of four units of red blood cell transfusions. However, it is important to note that complications associated with cannulation are not specific to the CO2RESET device, as they can potentially occur with any extracorporeal therapy.
This study has several limitations that should be acknowledged. First, it is important to note that the study had a small sample size, and larger studies are needed to confirm these findings. The results may also be dependent on local experience, may limit their generalizability, and require external validation. Second, other side effects, such as hemolysis and thrombocytopenia, were not systematically collected. While the definition of hemolysis in this setting remains controversial [30] and free hemoglobin was not homogeneously measured in the participating centers, thrombocytopenia may be due to other mechanisms, such as sepsis, drug reactions, or bleeding, and may provide difficult-to-interpret findings in the absence of a control group. Third, we did not include a parallel control group using a low blood flow device. However, the measured VCO2 with CO2RESET was significantly higher than the reported rates with other devices, and the configuration of those devices (i.e., cannula size and blood flow) limited their ability to obtain higher CO2 removal rates. Finally, only data at 24 h were collected. Future studies on the CO2RESET device should focus on several days of therapy to understand whether the CO2 removal rate remains stable over the entire operation period.
5. Conclusions
In this study, the use of the CO2RESET device showed to be effective for CO2 elimination in selected ARDS and dCOPD patients, with few side effects. Future studies are required to describe its effectiveness in fewer selected patients, as well as other potential side effects and pitfalls.
Author Contributions
F.S.T., L.N., F.A., S.R., J.M., A.A., A.M. and M.B. performed the experiments. F.S.T., M.B., L.M.B., M.V.M. and M.D.N. conceived and designed the experimental layout; all the other authors evaluated and analyzed the data, supported the writing of the manuscript, and studied and discussed the literature and available results. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study received was approved by the Institutional Review Board of the Erasme Hospital (P2018/128) and extended therefore to other centers.
Informed Consent Statement
Patient consent was waived due to the retrospective nature of the study.
Data Availability Statement
Data are available upon request from the corresponding author.
Acknowledgments
We are thankful to all perfusionists and ICU teams for their valuable contribution to treating such patients.
Conflicts of Interest
F.S.T., M.D.N., M.B., L.M.B. and M.V.M. are on the Advisory Board of EUROSETS srl.
References
- Marini, J.J. Mechanical ventilation: Past lessons and the near future. Crit. Care 2013, 17, S1. [Google Scholar] [CrossRef]
- Dreyfuss, D.; Soler, P.; Basset, G.; Saumon, G. High inflation pressure pulmonary edema. Respective effects of high airway pressure, high tidal volume, and positive end-expiratory pressure. Am. Rev. Respir. Dis. 1988, 137, 1159–1164. [Google Scholar] [CrossRef]
- Silva, P.L.; Ball, L.; Rocco, P.R.M.; Pelosi, P. Physiological and Pathophysiological Consequences of Mechanical Ventilation. Semin. Respir. Crit. Care Med. 2022, 43, 321–334. [Google Scholar] [CrossRef]
- Jaber, S.; Jung, B.; Matecki, S.; Petrof, B.J. Clinical review: Ventilator-induced diaphragmatic dysfunction-human studies confirm animal model findings! Crit. Care 2011, 15, 206. [Google Scholar] [CrossRef]
- Fan, E.; Del Sorbo, L.; Goligher, E.C.; Hodgson, C.L.; Munshi, L.; Walkey, A.J.; Adhikari, N.K.J.; Amato, M.B.P.; Branson, R.; Brower, R.G.; et al. An Official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine Clinical Practice Guideline: Mechanical Ventilation in Adult Patients with Acute Respiratory Distress Syndrome. Am. J. Respir. Crit. Care Med. 2017, 195, 1253–1263. [Google Scholar] [CrossRef]
- Neto, A.S.; Simonis, F.D.; Barbas, C.S.; Biehl, M.; Determann, R.M.; Elmer, J.; Friedman, G.; Gajic, O.; Goldstein, J.N.; Linko, R.; et al. Lung-Protective Ventilation With Low Tidal Volumes and the Occurrence of Pulmonary Complications in Patients Without Acute Respiratory Distress Syndrome: A Systematic Review and Individual Patient Data Analysis. Crit. Care Med. 2015, 43, 2155–2163. [Google Scholar] [CrossRef]
- Yang, D.; Grant, M.C.; Stone, A.; Wu, C.L.; Wick, E.C. A Meta-analysis of Intraoperative Ventilation Strategies to Prevent Pulmonary Complications: Is Low Tidal Volume Alone Sufficient to Protect Healthy Lungs? Ann. Surg. 2016, 263, 881–887. [Google Scholar] [CrossRef]
- Contreras, M.; Masterson, C.; Laffey, J.G. Permissive hypercapnia: What to remember. Curr. Opin. Anaesthesiol. 2015, 28, 26–37. [Google Scholar] [CrossRef]
- Combes, A.; Auzinger, G.; Capellier, G.; Du Cheyron, D.; Clement, I.; Consales, G.; Dabrowski, W.; De Bels, D.; De Molina Ortiz, F.J.G.; Gottschalk, A.; et al. ECCO2R therapy in the ICU: Consensus of a European round table meeting. Crit. Care 2020, 24, 490. [Google Scholar] [CrossRef]
- Ficial, B.; Vasques, F.; Zhang, J.; Whebell, S.; Slattery, M.; Lamas, T.; Daly, K.; Agnew, N.; Camporota, L. Physiological Basis of Extracorporeal Membrane Oxygenation and Extracorporeal Carbon Dioxide Removal in Respiratory Failure. Membranes 2021, 11, 225. [Google Scholar] [CrossRef]
- Nentwich, J.; Wichmann, D.; Kluge, S.; Lindau, S.; Mutlak, H.; John, S. Low-flow CO2 removal in combination with renal replacement therapy effectively reduces ventilation requirements in hypercapnic patients: A pilot study. Ann. Intensive Care 2019, 9, 3. [Google Scholar] [CrossRef]
- Moerer, O.; Harnisch, L.O.; Barwing, J.; Heise, D.; Heuer, J.F.; Quintel, M. Minimal-flow ECCO2R in patients needing CRRT does not facilitate lung-protective ventilation. J. Artif. Organs 2019, 22, 68–76. [Google Scholar] [CrossRef]
- Combes, A.; Tonetti, T.; Fanelli, V.; Pham, T.; Pesenti, A.; Mancebo, J.; Brodie, D.; Ranieri, V.M. Efficacy and safety of lower versus higher CO2 extraction devices to allow ultraprotective ventilation: Secondary analysis of the SUPERNOVA study. Thorax 2019, 74, 1179–1181. [Google Scholar] [CrossRef]
- Dhamija, A.; Thibault, D.; Fugett, J.; Hayanga, H.K.; McCarthy, P.; Badhwar, V.; Awori Hayanga, J.W. Incremental effect of complications on mortality and hospital costs in adult ECMO patients. Perfusion 2022, 37, 461–469. [Google Scholar] [CrossRef]
- Di Nardo, M.; Annoni, F.; Su, F.; Belliato, M.; Lorusso, R.; Broman, L.M.; Malfertheiner, M.; Creteur, J.; Taccone, F.S. Evaluation of a New Extracorporeal CO2 Removal Device in an Experimental Setting. Membranes 2020, 11, 8. [Google Scholar] [CrossRef]
- Montalti, A.; Belliato, M.; Gelsomino, S.; Nalon, S.; Matteucci, F.; Parise, O.; De Jong, M.; Makhoul, M.; Johnson, D.M.; Lorusso, R. Continuous monitoring of membrane lung carbon dioxide removal during ECMO: Experimental testing of a new volumetric capnometer. Perfusion 2019, 34, 538–543. [Google Scholar] [CrossRef]
- Knaus, W.A.; Draper, E.A.; Wagner, D.P.; Zimmerman, J.E. APACHE II: A severity of disease classification system. Crit. Care Med. 1985, 13, 818–829. [Google Scholar] [CrossRef]
- Vincent, J.L.; Moreno, R.; Takala, J.; Willatts, S.; De Mendonça, A.; Bruining, H.; Reinhart, C.K.; Suter, P.M.; Thijs, L.G. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996, 22, 707–710. [Google Scholar] [CrossRef]
- Morelli, A.; Del Sorbo, L.; Pesenti, A.; Ranieri, V.M.; Fan, E. Extracorporeal carbon dioxide removal (ECCO2R) in patients with acute respiratory failure. Intensive Care Med. 2017, 43, 519–530. [Google Scholar] [CrossRef]
- Schmidt, M.; Jaber, S.; Zogheib, E.; Godet, T.; Capellier, G.; Combes, A. Feasibility and safety of low-flow extracorporeal CO2 removal managed with a renal replacement platform to enhance lung-protective ventilation of patients with mild-to-moderate ARDS. Crit. Care 2018, 22, 122. [Google Scholar] [CrossRef]
- Combes, A.; Fanelli, V.; Pham, T.; Ranieri, V.M. European Society of Intensive Care Medicine Trials Group and the “Strategy of Ultra-Protective lung ventilation with Extracorporeal CO2 Removal for New-Onset moderate to severe ARDS” (SUPERNOVA) investigators. Feasibility and safety of extracorporeal CO2 removal to enhance protective ventilation in acute respiratory distress syndrome: The SUPERNOVA study. Intensive Care Med. 2019, 45, 592–600. [Google Scholar]
- Zhu, Y.; Zhen, W.; Zhang, X.; Shi, Z.; Zhang, L.; Zhou, J.; Meng, X. Extracorporeal Carbon Dioxide Removal in Patients with Acute Respiratory Distress Syndrome or Chronic Obstructive Pulmonary Disease: A Systematic Review and Meta-Analysis. Blood Purif. 2023, 52, 103–113. [Google Scholar] [CrossRef]
- McNamee, J.J.; Gillies, M.A.; Barrett, N.A.; Perkins, G.D.; Tunnicliffe, W.; Young, D.; Bentley, A.; Harrison, D.A.; Brodie, D.; Boyle, A.J.; et al. Effect of Lower Tidal Volume Ventilation Facilitated by Extracorporeal Carbon Dioxide Removal vs Standard Care Ventilation on 90-Day Mortality in Patients With Acute Hypoxemic Respiratory Failure: The REST Randomized Clinical Trial. JAMA 2021, 326, 1013–1023. [Google Scholar] [CrossRef]
- Duscio, E.; Cipulli, F.; Vasques, F.; Collino, F.; Rapetti, F.; Romitti, F.; Behnemann, T.; Niewenhuys, J.; Tonetti, T.; Pasticci, I.; et al. Extracorporeal CO2 Removal: The Minimally Invasive Approach, Theory, and Practice. Crit. Care Med. 2019, 47, 33–40. [Google Scholar] [CrossRef]
- Hospach, I.; Goldstein, J.; Harenski, K.; Laffey, J.G.; Pouchoulin, D.; Raible, M.; Votteler, S.; Storr, M. In vitro characterization of PrismaLung+: A novel ECCO2R device. Intensive Care Med. Exp. 2020, 8, 14. [Google Scholar] [CrossRef]
- Ghasem, N. Modeling and Simulation of the Impact of Feed Gas Perturbation on CO2 Removal in a Polymeric Hollow Fiber Membrane. Polymers 2022, 14, 3783. [Google Scholar] [CrossRef]
- Sun, L.; Kaesler, A.; Fernando, P.; Thompson, A.J.; Toomasian, J.M.; Bartlett, R.H. CO2 clearance by membrane lungs. Perfusion 2018, 33, 249–253. [Google Scholar] [CrossRef]
- Karagiannidis, C.; Kampe, K.A.; Sipmann, F.S.; Larsson, A.; Hedenstierna, G.; Windisch, W.; Mueller, T. Veno-venous extracorporeal CO2 removal for the treatment of severe respiratory acidosis: Pathophysiological and technical considerations. Crit. Care 2014, 18, R124. [Google Scholar] [CrossRef]
- Taccone, F.S.; Malfertheiner, M.V.; Ferrari, F.; Di Nardo, M.; Swol, J.; Broman, L.M.; Vercaemst, L.; Barrett, N.; Pappalardo, F.; Belohlavek, J.; et al. Extracorporeal CO2 removal in critically ill patients: A systematic review. Minerva Anestesiol. 2017, 83, 762–772. [Google Scholar] [CrossRef]
- Materne, L.A.; Hunsicker, O.; Menk, M.; Graw, J.A. Hemolysis in patients with Extracorporeal Membrane Oxygenation therapy for severe Acute Respiratory Distress Syndrome—A systematic review of the literature. Int. J. Med. Sci. 2021, 18, 1730–1738. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).