Interactive, Narrative-Based Digital Health Interventions for Vaccine Communication: Scoping Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Overview
2.1.1. Stage 1: Identifying Research Questions
2.1.2. Stage 2: Identifying Relevant Studies
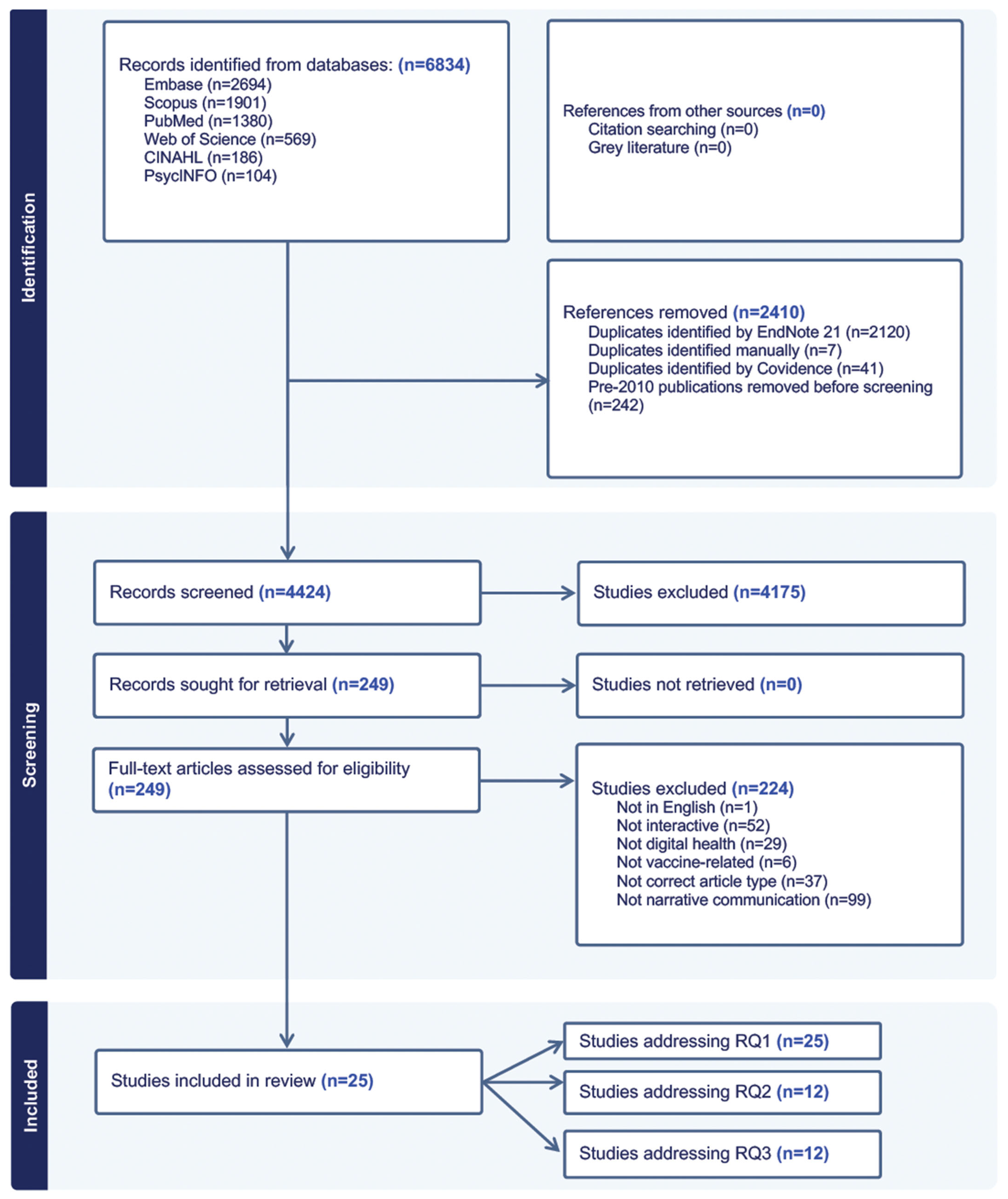
2.1.3. Stage 3: Study Selection
2.1.4. Stage 4: Charting the Data
2.1.5. Stage 5: Collating, Summarizing, and Reporting Results
3. Results
3.1. RQ1: How Have Interactive, Narrative-Based Digital Health Interventions Been Used for Vaccine Communication?
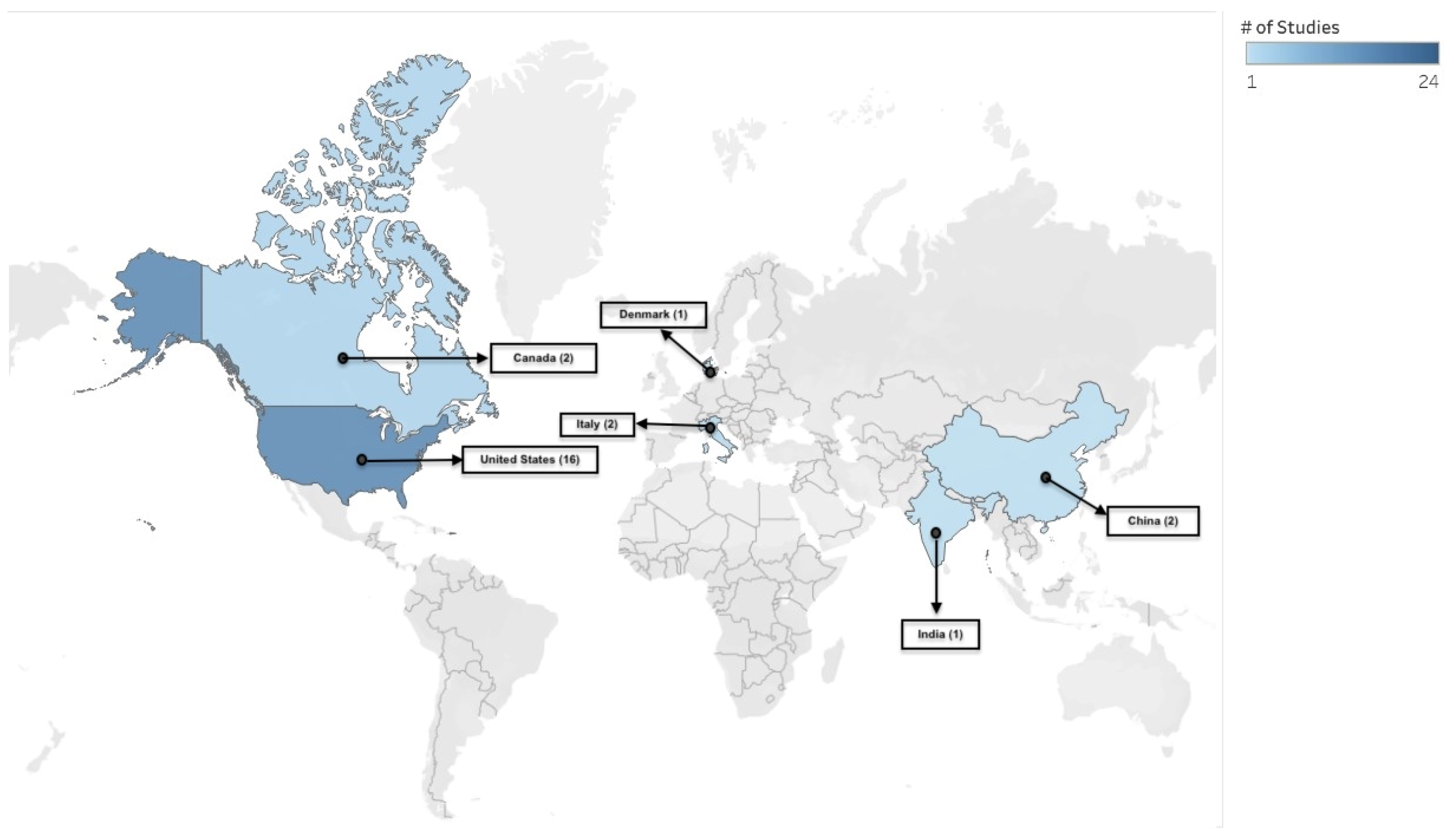
3.1.1. Characteristics of Included Studies
3.1.2. Study Demographics, Communication Strategies and Objectives
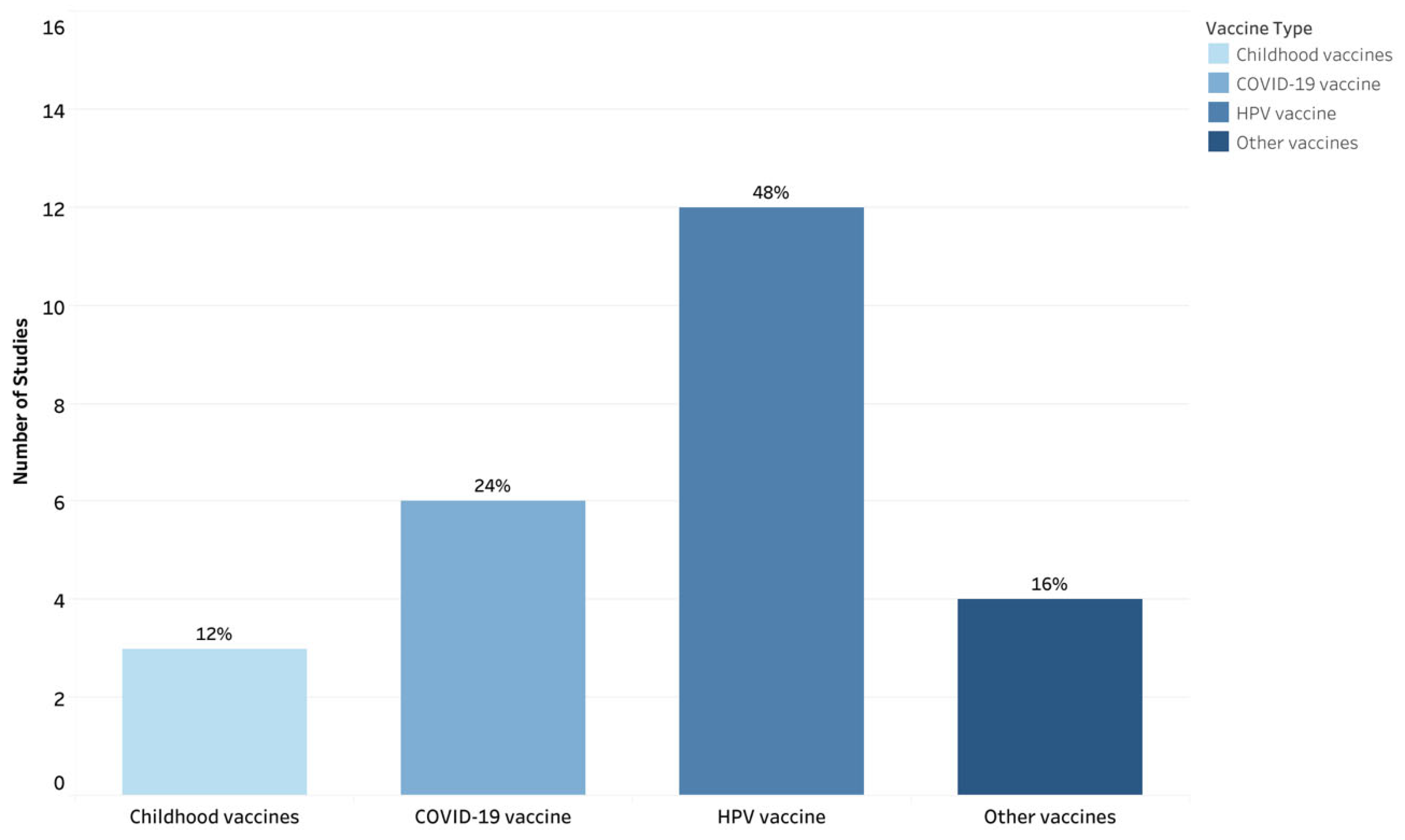
3.1.3. Vaccines and Vaccination Communication Purpose
3.1.4. Digital Health Interventions
3.1.5. Narrative Communication
3.1.6. Interactivity
3.2. RQ2: How Have Interactive, Narrative-Based Digital Health Interventions Been Evaluated for Promoting Vaccination Intention or Uptake?
3.3. RQ3: What Implementation Factors Are Associated with the Use of Narrative-Based Digital Health Interventions for Vaccine Communication?
3.4. Protocol Deviations
4. Discussion
4.1. Principal Findings
4.2. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Disclaimer
Abbreviations
| App | Application |
| CYOA | Choose-your-own-adventure |
| HPV | Human Papillomavirus |
| MMR | Measles, mumps, and rubella |
| NS | Not specified |
| PRISMA-ScR | Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews |
| RCT | Randomized control trial |
| RQ | Research Question |
| USA | United States |
| VPDs | Vaccine-preventable Diseases |
| VR | Virtual Reality |
| WHO | World Health Organization |
References
- Shattock, A.J.; Johnson, H.C.; Sim, S.Y.; Carter, A.; Lambach, P.; Hutubessy, R.C.W.; Thompson, K.M.; Badizadegan, K.; Lambert, B.; Ferrari, M.J.; et al. Contribution of vaccination to improved survival and health: Modelling 50 years of the Expanded Programme on Immunization. Lancet 2024, 403, 2307–2316. [Google Scholar] [CrossRef]
- Larson, H.J.; Schulz, W.S.; Tucker, J.D.; Smith, D.M. Measuring vaccine confidence: Introducing a global vaccine confidence index. PLoS Curr. 2015, 7, 25789200. [Google Scholar] [CrossRef]
- Borges do Nascimento, I.J.; Pizarro, A.B.; Almeida, J.M.; Azzopardi-Muscat, N.; Gonçalves, M.A.; Björklund, M.; Novillo-Ortiz, D. Infodemics and health misinformation: A systematic review of reviews. Bull. World Health Organ. 2022, 100, 544–561. [Google Scholar] [CrossRef]
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Xu, J. A Meta-Analysis Comparing the Effectiveness of Narrative vs. Statistical Evidence: Health vs. Non-Health Contexts. Health Commun. 2023, 38, 3113–3123. [Google Scholar] [CrossRef]
- Zebregs, S.; van den Putte, B.; Neijens, P.; de Graaf, A. The differential impact of statistical and narrative evidence on beliefs, attitude, and intention: A meta-analysis. Health Commun. 2015, 30, 282–289. [Google Scholar] [CrossRef]
- Braddock, K.; Dillard, J.P. Meta-analytic evidence for the persuasive effect of narratives on beliefs, attitudes, intentions, and behaviors. Commun. Monogr. 2016, 83, 446–467. [Google Scholar] [CrossRef]
- Shelby, A.; Ernst, K. Story and science: How providers and parents can utilize storytelling to combat anti-vaccine misinformation. Hum. Vaccines Immunother. 2013, 9, 1795–1801. [Google Scholar] [CrossRef]
- Dube, E.; Trottier, M.E.; Greyson, D.; MacDonald, N.E.; Meyer, S.B.; MacDonald, S.E.; Driedger, S.M.; Witteman, H.O.; Ouakki, M.; Gagnon, D. Use of narratives to enhance childhood vaccine acceptance: Results of an online experiment among Canadian parents. Hum. Vaccines Immunother. 2024, 20, 2379093. [Google Scholar] [CrossRef] [PubMed]
- Conlin, J.; Kumble, S.; Baker, M.; Shen, F. Re-Routing Persuasion: How Conversion Messages Boost Attitudes and Reduce Resistance Among Holdouts Unvaccinated for COVID-19. Health Commun. 2024, 39, 2834–2849. [Google Scholar] [CrossRef]
- Hinyard, L.J.; Kreuter, M.W. Using narrative communication as a tool for health behavior change: A conceptual, theoretical, and empirical overview. Health Educ. Behav. 2007, 34, 777–792. [Google Scholar] [CrossRef]
- Winskell, K.; Sabben, G.; Obong’o, C. Interactive Narrative in a Mobile Health Behavioral Intervention (Tumaini): Theoretical Grounding and Structure of a Smartphone Game to Prevent HIV Among Young Africans. JMIR Serious Games 2019, 7, e13037. [Google Scholar] [CrossRef] [PubMed]
- Haji Said, A.; Winskell, K.; Bednarczyk, R.A.; Reardon, E.E.; Vasudevan, L. Interactive Narrative-Based Digital Health Interventions for Vaccine Communication: Protocol for a Scoping Review. JMIR Res. Protoc. 2024, 13, e51137. [Google Scholar] [CrossRef]
- World Health Organization. Recommendations on Digital Interventions for Health System Strengthening. 2019. Available online: https://www.who.int/publications/i/item/9789241550505 (accessed on 25 September 2025).
- Lo Moro, G.; Ferrara, M.; Langiano, E.; Accortanzo, D.; Cappelletti, T.; De Angelis, A.; Esposito, M.; Prinzivalli, A.; Sannella, A.; Sbaragli, S.; et al. Countering vaccine hesitancy: A systematic review of interventions to strengthen healthcare professionals’ action. Eur. J. Public Health 2023, 33, 905–915. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Schank, R.C.; Berman, T.R. The pervasive role of stories in knowledge and action. In Narrative Impact: Social and Cognitive Foundations; Green, M.C., Strange, J.J., Brock, T.C., Eds.; Lawrence Erlbaum Associates Publishers: Mahwah, NJ, USA, 2002; pp. 287–313. [Google Scholar]
- World Health Organization. Classification of Digital Health Interventions V1.0. 2018. Available online: https://www.who.int/publications/i/item/WHO-RHR-18.06? (accessed on 25 September 2025).
- Galhardi, C.; Freire, N.; Marques Fagundes, M.; Minayo, M.; Cunha, I. Fake news e hesitação vacinal no contexto da pandemia da COVID-19 no Brasil. Ciênc. Saúde Coletiva 2022, 27, 1849–1858. [Google Scholar]
- Stoner, M.C.D.; Tweedy, D.; Comello, M.G.L.; Toval, C.; Pettifor, A.E.; Larsen, M.A.; Baez, A.; Maragh-Bass, A.C.; Tolley, E.E.; Browne, E.N.; et al. Using narratives to inform the development of a digital health intervention related to COVID-19 vaccination in Black young adults in Georgia, North Carolina and Alabama. Vaccine 2022, 40, 6908–6916. [Google Scholar] [CrossRef]
- Zhu, A.; Amith, M.; Tang, L.; Cunningham, R.; Xu, A.; Boom, J.A.; Tao, C. Experimenting with a Prototype Interactive Narrative Game to Improve Knowledge and Beliefs for the HPV Vaccine. HCI Int Late Break. Pap. 2021, 13097, 186–201. [Google Scholar]
- Streuli, S.; Ibrahim, N.; Mohamed, A.; Sharma, M.; Esmailian, M.; Sezan, I.; Farrell, C.; Sawyer, M.; Meyer, D.; El-Maleh, K.; et al. Development of a culturally and linguistically sensitive virtual reality educational platform to improve vaccine acceptance within a refugee population: The SHIFA community engagement-public health innovation programme. BMJ Open 2021, 11, e051184. [Google Scholar] [CrossRef]
- Maragh-Bass, A.; Comello, M.L.; Tolley, E.E.; Stevens, D., Jr.; Wilson, J.; Toval, C.; Budhwani, H.; Hightow-Weidman, L. Digital Storytelling Methods to Empower Young Black Adults in COVID-19 Vaccination Decision-Making: Feasibility Study and Demonstration. JMIR Form. Res. 2022, 6, e38070. [Google Scholar] [CrossRef]
- Cates, J.R.; Fuemmeler, B.F.; Diehl, S.J.; Stockton, L.L.; Porter, J.; Ihekweazu, C.; Gurbani, A.S.; Coyne-Beasley, T. Developing a Serious Videogame for Preteens to Motivate HPV Vaccination Decision Making: Land of Secret Gardens. Games Health J. 2018, 7, 51–66. [Google Scholar] [CrossRef]
- Cates, J.R.; Fuemmeler, B.F.; Stockton, L.L.; Diehl, S.J.; Crandell, J.L.; Coyne-Beasley, T. Evaluation of a Serious Video Game to Facilitate Conversations About Human Papillomavirus Vaccination for Preteens: Pilot Randomized Controlled Trial. JMIR Serious Games 2020, 8, e16883. [Google Scholar] [CrossRef]
- Lee, S.; Yoon, H.; Chen, L.; Juon, H.S. Culturally appropriate photonovel development and process evaluation for hepatitis B prevention in Chinese, Korean, and Vietnamese American communities. Health Educ. Behav. 2013, 40, 694–703. [Google Scholar] [CrossRef]
- Teitelman, A.M.; Gregory, E.F.; Jayasinghe, J.; Wermers, Z.; Koo, J.H.; Morone, J.F.; Leri, D.C.; Davis, A.; Feemster, K.A. Vaccipack, A Mobile App to Promote Human Papillomavirus Vaccine Uptake Among Adolescents Aged 11 to 14 Years: Development and Usability Study. JMIR Nurs. 2020, 3, e19503. [Google Scholar] [CrossRef]
- Silesky, M.D.; Panchal, D.; Fields, M.; Peña, A.S.; Diez, M.; Magdaleno, A.; Frausto-Rodriguez, P.; Bonnevie, E. A Multifaceted Campaign to Combat COVID-19 Misinformation in the Hispanic Community. J. Community Health 2023, 48, 286–294. [Google Scholar] [CrossRef] [PubMed]
- Peck, J.L.; Stanton, M.; Reynolds, G.E. Smartphone preventive health care: Parental use of an immunization reminder system. J. Pediatr. Health Care 2014, 28, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Buller, D.B.; Pagoto, S.; Henry, K.; Berteletti, J.; Walkosz, B.J.; Bibeau, J.; Baker, K.; Hillhouse, J.; Arroyo, K.M. Human Papillomavirus Vaccination and Social Media: Results in a Trial with Mothers of Daughters Aged 14–17. Front. Digit. Health 2021, 3, 683034. [Google Scholar] [CrossRef] [PubMed]
- Nowak, G.J.; Evans, N.J.; Wojdynski, B.W.; Ahn, S.J.G.; Len-Rios, M.E.; Carera, K.; Hale, S.; McFalls, D. Using immersive virtual reality to improve the beliefs and intentions of influenza vaccine avoidant 18-to-49-year-olds: Considerations, effects, and lessons learned. Vaccine 2020, 38, 1225–1233. [Google Scholar] [CrossRef]
- Hopfer, S.; Phillips, K.K.; Weinzierl, M.; Vasquez, H.E.; Alkhatib, S.; Harabagiu, S.M. Adaptation and Dissemination of a National Cancer Institute HPV Vaccine Evidence-Based Cancer Control Program to the Social Media Messaging Environment. Front. Digit. Health 2022, 4, 819228. [Google Scholar] [CrossRef]
- Kim, M.; Lee, H.; Kiang, P.; Allison, J. Development and acceptability of a peer-paired, cross-cultural and cross-generational storytelling HPV intervention for Korean American college women. Health Educ. Res. 2019, 34, 483–494. [Google Scholar] [CrossRef]
- Piltch-Loeb, R.; Su, M.; Hughes, B.; Testa, M.; Goldberg, B.; Braddock, K.; Miller-Idriss, C.; Maturo, V.; Savoia, E. Testing the Efficacy of Attitudinal Inoculation Videos to Enhance COVID-19 Vaccine Acceptance: Quasi-Experimental Intervention Trial. JMIR Public Health Surveill. 2022, 8, e34615. [Google Scholar] [CrossRef]
- Hakim, H.; Bettinger, J.A.; Chambers, C.T.; Driedger, S.M.; Dubé, E.; Gavaruzzi, T.; Giguere, A.M.C.; Kavanagh, É.; Leask, J.; MacDonald, S.E.; et al. A Web Application About Herd Immunity Using Personalized Avatars: Development Study. J. Med. Internet Res. 2020, 22, e20113. [Google Scholar] [CrossRef]
- Kandasamy, S.; Ariyarajah, A.; Limbachia, J.; An, D.; Lopez, L.; Manoharan, B.; Pacht, E.; Silver, A.; Uddandam, A.; Vansjalia, K.M.; et al. South Asian Youth as Vaccine Agents of Change (SAY-VAC): Evaluation of a public health programme to mobilise and empower South Asian youth to foster COVID-19 vaccine-related evidence-based dialogue in the Greater Toronto and Hamilton Area, Canada. BMJ Open 2022, 12, e061619. [Google Scholar] [CrossRef]
- Macario, E.; Matiella, A.C. A bilingual webnovela on the human papillomavirus: Will Latinas and health professionals use it? J. Commun. Healthc. 2015, 8, 55–66. [Google Scholar] [CrossRef]
- Fadda, M.; Galimberti, E.; Fiordelli, M.; Schulz, P.J. Evaluation of a Mobile Phone-Based Intervention to Increase Parents’ Knowledge About the Measles-Mumps-Rubella Vaccination and Their Psychological Empowerment: Mixed-Method Approach. JMIR mHealth uHealth 2018, 6, e59. [Google Scholar] [CrossRef]
- Occa, A.; Stahl, H.M.; Julien-Bell, S. Helping Children to Participate in Human Papillomavirus-Related Discussions: Mixed Methods Study of Multimedia Messages. JMIR Form. Res. 2022, 6, e28676. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, E.A.; Loft, L.H.; Jacobsen, S.U.; Søborg, B.; Bigaard, J. Strategic health communication on social media: Insights from a Danish social media campaign to address HPV vaccination hesitancy. Vaccine 2020, 38, 4909–4915. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Zhang, W. The use of Web-based interactive technology to promote HPV vaccine uptake among young females: A randomized controlled trial. BMC Womens Health 2021, 21, 277. [Google Scholar] [CrossRef] [PubMed]
- Luk, T.T.; Lui, J.H.T.; Wang, M.P. Efficacy, Usability, and Acceptability of a Chatbot for Promoting COVID-19 Vaccination in Unvaccinated or Booster-Hesitant Young Adults: Pre-Post Pilot Study. J. Med. Internet Res. 2022, 24, e39063. [Google Scholar] [CrossRef]
- Johri, M.; Chandra, D.; Kone, K.G.; Sylvestre, M.P.; Mathur, A.K.; Harper, S.; Nandi, A. Social and Behavior Change Communication Interventions Delivered Face-to-Face and by a Mobile Phone to Strengthen Vaccination Uptake and Improve Child Health in Rural India: Randomized Pilot Study. JMIR mHealth uHealth 2020, 8, e20356. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.K.; Su, L.Y. When a Personal HPV Story on a Blog Influences Perceived Social Norms: The Roles of Personal Experience, Framing, Perceived Similarity, and Social Media Metrics. Health Commun. 2020, 35, 438–446. [Google Scholar] [CrossRef]
- Lin, C.; Mullen, J.; Smith, D.; Kotarba, M.; Kaplan, S.J.; Tu, P. Healthcare Providers’ Vaccine Perceptions, Hesitancy, and Recommendation to Patients: A Systematic Review. Vaccines 2021, 9, 713. [Google Scholar] [CrossRef]
- de Koning, R.; Gonzalez Utrilla, M.; Spanaus, E.; Moore, M.; Lomazzi, M. Strategies used to improve vaccine uptake among healthcare providers: A systematic review. Vaccine X 2024, 19, 100519. [Google Scholar] [CrossRef] [PubMed]
- Cole-Lewis, H.; Ezeanochie, N.; Turgiss, J. Understanding Health Behavior Technology Engagement: Pathway to Measuring Digital Behavior Change Interventions. JMIR Form. Res. 2019, 3, e14052. [Google Scholar] [CrossRef] [PubMed]
| Device Type & No. of Studies (N=) | Primary Digital Modality | Target User |
|---|---|---|
| Multi-device compatibility (e.g., mobile, computer, or tablet) (N = 7) [21,24,25,26,28,38,43] | App [21,25,26,28]; Chatbot [43]; Webnovela [38]; Digital Health Intervention with Digital Storytelling [24] | Parent-adolescent dyads [25,26,28]; Latinas and Health professionals [38]; young Black or African American adults [21,24]; young adults [43] |
| Mobile (N = 4) [30,39,42,44] | App [30,39,44]; Web-based Interactive Technology [42] | Parents [30,39,44]; Chinese Female Undergraduates [42] |
| Computer (N = 2) [36,40] | Web Application [36]; Animated Video and Web-based Game [40] | Men and Women [36]; Middle School Children [40] |
| Virtual Reality (N = 2) [23,32] | 360° Video Animation [23]; VR, video, or e-pamphlet [32] | Somali Adults [23]; Vaccine-avoidant Adults [32] |
| Not Specified (N = 10) [22,27,29,31,33,34,35,37,41,45] | Social Media [31,33,41]; Blog on social media [45]; Mass media [29]; Videos [35,37]; Storytelling video [34]; Prototype Interactive Narrative Game [22]; Photonovel [27] | College students [22,45]; Hispanic communities [29]; Asian Americans [27]; Korean American women [34]; South Asian Youth [37]; Youth and Parents [33]; Mothers of Daughters [31,41]; Unvaccinated Individuals [35] |
| Author, Year, & Country | Study Design & Demographics (N=) | Vaccine | Theoretical Underpinnings or Behavioral Constructs | Digital Health Intervention, & Communication Objective or Process | Interactive Narrative |
|---|---|---|---|---|---|
| Stoner, et al. (2022), USA [21] | Online survey; Young Black or African American adults (N = 150) | COVID-19 vaccine | Social cognitive theory | CYOA (Tough Talks) App communicated COVID-19 vaccination by addressing vaccine, provider, and system mistrust. | Narratives simulated vaccine decision-making scenarios shaped by social influences, fears, and misinformation. Interactivity involved selecting responses to each scenario. |
| Zhu et al. (2021), USA [22] | RCT; College students (N = 99) | HPV vaccine | Self-determination theory | A serious game (Vaccination Vacation) communicated the HPV virus and vaccine by integrating real-life experiences to improve vaccine awareness. | Real-life patient narratives inspired the game’s characters. Interactivity was facilitated via an action component using a virtual machine to attack cells of HPV-related cancers. The game challenged players to convince characters to receive vaccination by selecting responses from a pool of options. |
| Streuli, et al. (2021), USA [23] | Community-based participatory research; Somali adults (N = 60 refugees, N = 7 expert advisors) | Childhood vaccines | Information retention and behavior change | The VR addressed vaccine misinformation through a culturally and linguistically tailored approach. | Narrative followed an expectant mother who discovered the MMR vaccine at a doctor’s visit, explored MMR vaccine science, and debunked of MMR-autism myth. Interactive prompts within the VR encouraged user self-reflection. |
| Maragh-Bass, et al. (2022), USA [24] | Feasibility study & demonstration; Young Black Adults (N = 11) | COVID-19 vaccine | Decision-making | Culturally tailored digital health intervention (Tough Talks: COVID) empowered young Black people to make autonomous decisions about COVID-19 vaccine receipt. | Narrative addressed vulnerability to COVID-19, vaccine hesitancy, countered misinformation, and community connections. Digital storytelling workshops were interactive and featured icebreakers, with participants co-creating a narrative and each contributing a sentence. |
| Cates et al. (2018), USA [25] | Focus group discussions; Pre-teens (N = 16), and mothers (N = 9) | HPV vaccine | Self-determination theory and health belief model | Serious game (Land of Secret Gardens) educated preteens about HPV infection and vaccine while ensuring the content was age-appropriate and captured their interest. | An educational narrative on HPV infection and vaccination. Interactive mini games, such as finding hidden objects and defending plants from the HPV virus. Completing tasks earned rewards, allowing players to “protect” their garden (body) with a vaccine-symbolizing “potion”. |
| Cates et al. (2020), USA [26] | Pilot randomized controlled trial; Parent-preteen dyads (N = 55) | HPV vaccine | Self-determination theory | Serious game (Land of Secret Gardens) educated preteens about HPV infection and vaccination and encouraged dialogue with parents and healthcare providers. For healthcare providers, communication materials comprised brochures, posters, and interactive online training. | Same as Cates et al. [25]. |
| Lee, et al. (2013), USA [27] | Randomized community trial; Chinese, Korean, and Vietnamese (N = 441) | Hepatitis B vaccine | Self-efficacy and intention | Culturally tailored (photonovel) was developed to increase awareness of Hepatitis B vaccination and screening via PowerPoint presentation, role-play video, and a Q&A session. | The narrative depicted storylines from common life experiences in the community and key concerns about Hepatitis B. Actors, photography, and a respected physician played as actors for cultural relevance. Interactive “fact boxes” and a Q&A section increased engagement and provided additional information. |
| Teitelman, et al. (2020), USA [28] | Development and usability study; Adolescents (N = 20; aged 11–14 years) and parents (N = 34) | Primary: (HPV vaccine); secondary: (adolescent vaccines) | Integrated behavioral model | An app (Vaccipack) provided vaccine information and addressed parental beliefs influencing adolescent’s HPV vaccination decisions. | Narratives comprised 26 short stories written from the perspectives of parents, adolescents, and clinicians. The app was interactive and delivered a new story weekly via push notifications, promoting sustained engagement over the six-month period required for the two-dose HPV vaccine series. |
| Silesky, et al. (2022), USA [29] | Media monitoring study; Hispanic adults | COVID-19 vaccine | Attitudes and beliefs | A (mass media communication strategy) including radio PSAs, op-eds, satellite media tours, website, and social media platforms like Instagram and Facebook via (El Beacon) was developed to counter COVID-19 vaccine misinformation and promote uptake through fact-based messaging delivered by trusted community voices. | The narrative featured prompts debunking common COVID-19 vaccine misinformation and sharing positive, personal vaccination messages tailored to the Hispanic community. Prompts were regularly updated to reflect evolving misinformation, and an interactive format encouraged engagement through comments and likes. |
| Peck, et al. (2014), USA [30] | Descriptive study design; Parents or guardians (N = 262, average age 34–35 years) | Childhood vaccines | Health belief model | A Call the Shots (CTS) app served as a vaccination reminder system for parents and provided information on vaccines recommended at each provider visit. | Narrative featured personal stories from families affected by VPDs. The CTS platform was interactive, allowing parents to connect with other parents through social media, as well as their child’s provider. |
| Buller, et al. (2021), USA [31] | RCT; Mothers (N = 869, mean age of 43.1 years), with N = 469 teenage daughters (mean age of 15.3 years) | HPV vaccine; secondary: (influenza vaccine) | Social cognitive, transportation, and diffusion of innovations theories | A social media campaign (Health Chat) was delivered in 2 Facebook groups to promote vaccination. Posts incorporated social norms-based appeals, appearance-based and health-risk messaging. | Some of the posts in the social media campaign were in narrative format (e.g., a story about someone who died from cervical cancer). The interactive feature included reactions to posts (likes, loves, sad) and comments. |
| Nowak, et al. (2020), USA [32] | One-way between-subjects experimental design; Adults (N = 171, age of 18–49 years) | Influenza vaccine | Perceptions, beliefs, confidence, and intentions | Whether the use of (VR, video, or e-pamphlet) could improve influenza-related perceptions, beliefs, confidence, and intentions among individuals who avoid vaccination. | Narrative depicted an individual spreading the flu in public, while the interactive VR component shrank the individual to a cellular level, immersing participants in a storyline about flu transmission, immune response, and vaccine benefits. |
| Hopfer, et al. (2022), USA [33] | Observational study; Youth and young adults (11–26 years), and parents of adolescents (N = NS) | HPV vaccine | Centering and discourse coherence theories | A social media strategy, via Instagram, TikTok, and Twitter, was utilized to distribute videos that presented vaccine decision narratives told by youth through informal conversation. | Thirteen short videos featured narratives set in diverse social contexts (e.g., peer, doctor, and parent conversations) emphasizing the benefits of HPV vaccination. Interactivity was encouraged through commenting, emoji reactions, and content sharing. |
| Kim, et al. (2019), USA [34] | RCT; Korean or Korean American female students (N = 104, mean age of 21.7 years) | HPV vaccine | Storytelling/Narrative communication theory | An HPV video intervention promoted HPV vaccination through culturally relevant storytelling. | An interactive peer-paired storytelling approach, with two storytellers engaging in a dialogue, responding to interviewer prompts, and building on each other’s reflections. |
| Piltch-Loeb, et al. (2022), USA [35] | Quasi-experimental Trial; Unvaccinated individuals (N = 1991, mean age of 40.7 years) | COVID-19 vaccine | Inoculation theory | 30-s inoculation videos aimed to promote resistance against persuasion against COVID-19 vaccine misinformation. | The narrative was presented in video formats (fact-based, rhetoric-focused, and hybrid), which countered anti-vaccine misinformation through an inoculation video warning of manipulation techniques and a stimulus video demonstrating them. Interactive component asked participants to answer questions evaluating their perceptions of the content. |
| Hakim, et al. (2020), Canada [36] | Development study; Men and women (N = 110, mean age of 38 years) | Measles, pertussis, and influenza vaccines | Health belief model, Gestalt visual principles, cognitive theory of multimedia learning, and affect heuristic | A (web application) communicated the concept of community immunity to individuals with diverse educational backgrounds while simultaneously assessing their cognitive and emotional responses. | The narrative illustrated community immunity, while the interactive feature allowed participants to create avatars of themselves and their social circles. These avatars were incorporated into a two-minute visualization showing how vaccination coverage and social interactions affect disease spread. |
| Kandasamy, et al. (2022), Canada [37] | Cross-sectional and one-group pretest–post-test design; South Asian youth (N = 30, aged 18–29 years) | COVID-19 vaccine | Knowledge and confidence | A digital media health program (SAY-VAC) consisted of a video and an information sheet to address COVID-19 vaccine concerns, and improve confidence. | A culturally tailored narrative promoted COVID-19 vaccination and addressed concerns (e.g., vaccine ingredients). Interactivity was facilitated by youth Ambassadors who used the video to initiate discussions with family and community members and encourage vaccination. |
| Macario, et al. (2015), USA [38] | Formative research (pre- and post-survey, focus group discussion, online survey); Latinas (N = 84), and health professionals (N = 41) | HPV vaccine | Social cognitive theory, exchange theory, the health belief model, the theory of reasoned action, the trans-theoretical model of health behavior change, and diffusion of innovations | A (webnovela) addressed knowledge gaps about higher HPV incidence and cervical cancer among Latinas. The webnovela incorporated voice-overs, still photos, short video clips, and the use of culturally relevant language (e.g., Spanglish). | The narrative followed three young Latino friends who discovered HPV and its consequences, tracing their reactions, information-seeking, and decisions to vaccinate and promote vaccination. The interactive features included dialog, thought bubbles, and voiceovers, which allowed users to explore the characters’ journeys through vaccination access and screening. |
| Fadda, et al. (2018), Italy [39] | Randomized control trial; Women and men (N = 140) | MMR vaccine | Knowledge, confidence, decision-making, and psychological empowerment | Two mobile-based apps (MorbiQuiz) aimed to improve parents’ MMR vaccine knowledge and decision-making: one used gamified questions, the other employed video narratives and messages to increase psychological empowerment. | The narrative featured an actress playing a mother who recounted how she became empowered to vaccinate her child with MMR. The interactive component included a gamified intervention that awarded points (stars) for correct answers, with a leaderboard enabled for score comparison and competition. |
| Occa, et al. (2022), Italy [40] | Mixed Methods Study; Middle school students (N = 35, aged 11–12 years) | HPV vaccine | Theory of planned behavior and social cognitive theory | An animated video and web-based game (Salut e HPV or Health and HPV) were utilized as part of a communication strategy to increase children’s knowledge and positive perceptions about HPV and HPV vaccination. | The narrative featured a healthcare professional who addressed questions and concerns, normalized HPV vaccination, and supported character identification. The interactive game allowed children to choose characters, track progress, earn points, receive feedback while promoting engagement, autonomy, and skill development. |
| Pedersen, et al. (2020), Denmark [41] | Evaluation of social media campaign; (Primary target: mothers of daughters aged 10–14 years; secondary target: fathers) | HPV vaccine | Attitudes | A social media strategy, including Facebook, Instagram, and YouTube, communicated messages about the safety and effectiveness of the HPV vaccine. | Personal cervical cancer narratives and health professional experiences were featured to increase authenticity and relevance. Interactive calls-to-action encouraged viewer engagement through likes, shares, and comments. |
| Wang, et al. (2021), China [42] | RCT; Chinese (N = 180 female undergraduate students) | HPV vaccine | Theory of information avoidance and the limited capacity model of motivated mediated messages | A (web-based interactive technology) sought to influence young females’ intention to vaccinate by allowing them to read or interact with content. | The narrative followed XiaoA, a young woman diagnosed with HPV, through four phases of her experience: diagnosis, work life, relationships, and a medical consultation. An interactive condition allowed participants to guide her decisions at key points, shaping her journey and exploring potential consequences of different decisions. |
| Luk, et al. (2022), China [43] | Pre-post pilot study; Chinese adults (N = 290, mean age of 21.4) | COVID-19 vaccine | Knowledge and decision-making | Chatbot (Vac Chat, Fact Check) communicated information about COVID-19 disease and vaccination. | The narrative was delivered via a chatbot in a conversational format with predefined rules and natural language processing. The chatbot covered information on COVID-19 disease, vaccination benefits, myths, boosters, and service access. Interactive menu options were utilized for user engagement. |
| Johri, et al. (2020), India [44] | Cluster-randomized pilot Trial; Households (N = 387 with children aged 0–12 months) | Childhood vaccines | Knowledge and attitudes | mHealth mobile app (Tika Vaani) educated beneficiaries about vaccination and dispelled vaccine-related misinformation. | The narrative was delivered through entertainment educational audio capsules promoting vaccination and child health. The interactive component included voice reminders and face-to-face meetings to educate and engage beneficiaries about vaccination and child health. |
| Lee, et al. (2020), NS [45] | Randomized online experiment; College students (N = 220, mean age of 22.74) | HPV vaccine | Perceived social norms, perceived similarity, framing (gain vs. loss), and personal experience | A (social media personal blog) was developed to investigate whether a personal narrative can influence perceived social norm, specifically examining the role of perceived similarity with the blogger and social media metrics in shaping perceptions. | Four stimulus narratives featured either gain-framed (HPV vaccination prevents cancer) or loss-framed (cancer risk from non-vaccination). An interactive manipulation of reads, shares, and comments was used to assess perceptions, engagement, and perceived credibility or relatability of the narratives. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haji Said, A.; Syed, F.; Ma, I.; Akbar, R.; Ramprasad, N.; Reardon, E.E.; Bednarczyk, R.A.; Winskell, K.; Vasudevan, L. Interactive, Narrative-Based Digital Health Interventions for Vaccine Communication: Scoping Review. Vaccines 2025, 13, 1220. https://doi.org/10.3390/vaccines13121220
Haji Said A, Syed F, Ma I, Akbar R, Ramprasad N, Reardon EE, Bednarczyk RA, Winskell K, Vasudevan L. Interactive, Narrative-Based Digital Health Interventions for Vaccine Communication: Scoping Review. Vaccines. 2025; 13(12):1220. https://doi.org/10.3390/vaccines13121220
Chicago/Turabian StyleHaji Said, Ahmed, Fiona Syed, Isabelle Ma, Rida Akbar, Nidhi Ramprasad, Erin E. Reardon, Robert A. Bednarczyk, Kate Winskell, and Lavanya Vasudevan. 2025. "Interactive, Narrative-Based Digital Health Interventions for Vaccine Communication: Scoping Review" Vaccines 13, no. 12: 1220. https://doi.org/10.3390/vaccines13121220
APA StyleHaji Said, A., Syed, F., Ma, I., Akbar, R., Ramprasad, N., Reardon, E. E., Bednarczyk, R. A., Winskell, K., & Vasudevan, L. (2025). Interactive, Narrative-Based Digital Health Interventions for Vaccine Communication: Scoping Review. Vaccines, 13(12), 1220. https://doi.org/10.3390/vaccines13121220







