Persistence of Pneumococcal Serotype 3 in Adult Pneumococcal Disease in Hong Kong
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients and Isolates
2.2. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Disease and Outcomes
3.3. Serotypes
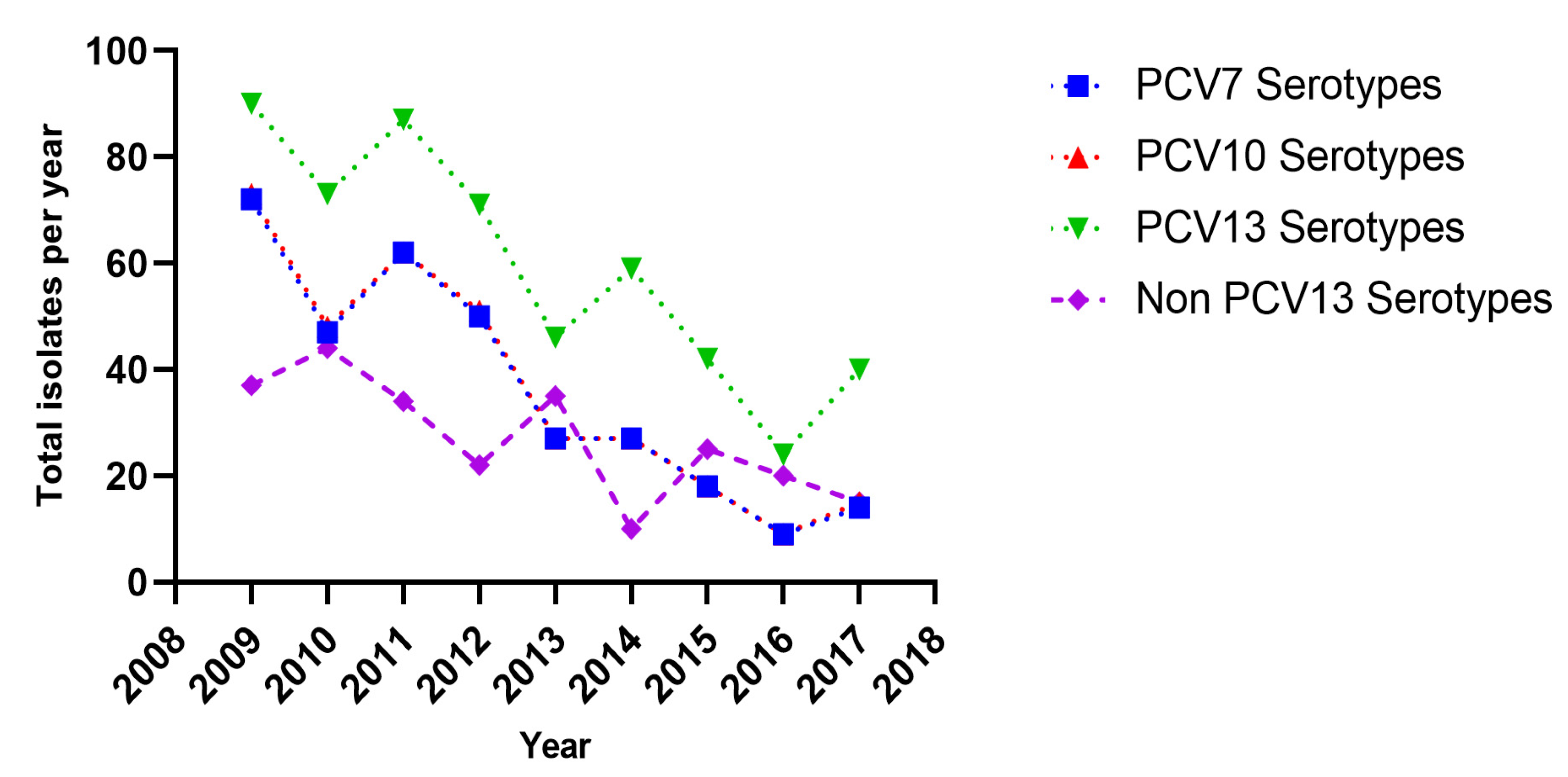
3.4. Antimicrobial Non-Susceptibility
3.5. Relationship of Serotypes with Disease/Antimicrobial Non-Susceptibilities
3.6. Thirty-Day Mortality, Patient and Organism Related Factors
3.7. Trends in Hospitalisation Rates Due to Pneumococcal Pneumonia
4. Discussion
5. Conclusions and Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Financial Disclosure
References
- Centre for Health Protection, Department of Health Hong Kong. Death Rates by Leading Causes of Death, 2001–2019. Available online: https://www.chp.gov.hk/en/statistics/data/10/27/117.html (accessed on 3 June 2021).
- Lui, G.; To, H.K.W.; Lee, N.; Chan, R.W.Y.; Li, T.; Wong, R.Y.K.; Hui, D.S.C.; Ip, M. Adherence to Treatment Guideline Improves Patient Outcomes in a Prospective Cohort of Adults Hospitalized for Community-Acquired Pneumonia. Open Forum Infect. Dis. 2020, 7, 146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, D. Review of Pneumococcal Vaccination and Invasive Pneumococcal Disease in Hong Kong; Communicable Disease Watch, Centre for Health: Hong Kong, China, 2018; Volume 15, pp. 4–5. Available online: https://www.chp.gov.hk/files/pdf/cdw_v15_1.pdf (accessed on 15 May 2021).
- Available online: Pneumococcal vaccination:People aged 65 years or above under the Government Vaccination Programme and the Vaccination Subsidy Scheme. Available online: https://www.chp.gov.hk/en/statistics/data/10/100044/6870.html (accessed on 3 June 2021).
- Scelfo, C.; Menzella, F.; Fontana, M.; Ghidoni, G.; Galeone, C.; Facciolongo, N.C. Pneumonia and Invasive Pneumococcal Diseases: The Role of Pneumococcal Conjugate Vaccine in the Era of Multi-Drug Resistance. Vaccines 2021, 9, 420. [Google Scholar] [CrossRef] [PubMed]
- Griffin, M.R.; Zhu, Y.; Moore, M.R.; Whitney, C.G.; Grijalva, C.G. U.S. Hospitalizations for Pneumonia after a Decade of Pneumococcal Vaccination. NEJM 2013, 369, 155–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moberley, S.; Holden, J.; Tatham, D.P.; Andrews, R.M. Vaccines for preventing pneumococcal infection in adults. Cochrane Database Syst. Rev. 2013, 2013, CD000422. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, J.M.; Jiang, Q.; Isturiz, R.E.; Sings, H.L.; Swerdlow, D.L.; Gessner, B.D.; Carrico, R.M.; Peyrani, P.; Wiemken, T.L.; Mattingly, W.A.; et al. Effectiveness of 13-valent pneumococcal conjugate vaccine against hospitalization for community-acquired pneumonia in older US adults: A test-negative design. Clin. Infect. Dis. 2018, 67, 1498–1506. [Google Scholar] [CrossRef] [PubMed]
- Said, M.A.; Johnson, H.L.; Nonyane, B.A.S.; Deloria-Knoll, M.; Brien, K.L.; Andreo, F.; Beovic, B.; Blanco, S.; Boersma, W.G.; Boulware, D.R.; et al. Estimating the Burden of Pneumococcal Pneumonia among Adults: A Systematic Review and Meta-Analysis of Diagnostic Techniques. PLoS ONE 2013, 8, e60273. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alanee, S.R.J.; McGee, L.; Jackson, D.; Chiou, C.C.; Feldman, C.; Morris, A.J.; Ortqvist, A.; Rello, J.; Luna, C.M.; Baddour, L.M.; et al. Association of Serotypes of Streptococcus pneumoniae with Disease Severity and Outcome in Adults: An International Study. Clin. Infect. Dis. 2007, 45, 46–51. [Google Scholar] [CrossRef] [Green Version]
- Centers for Disease Control and Prevention. Protocol for Multiplex PCR—S. pneumoniae Serotyping—Clinical Specimens-Latin America Set. Available online: https://www.cdc.gov/streplab/downloads/pcr-Latin-Amer-clinical-specimens.pdf (accessed on 21 August 2014).
- CLSI. Performance Standards for Antimicrobial Susceptibility Testing; 28th informational supplement; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2018. [Google Scholar]
- EUCAST. Breakpoints for Interpretation of MICs and Zone Diameters. Version 10.0. 2020. Available online: http://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoints_tables/v_10.0_Breakpoint_Tables.pdf (accessed on 28 January 2021).
- Sinus and Allergy Health Partnership. Antimicrobial treatment guidelines for acute bacterial rhinosinusitis. Otolaryngol. Head Neck Surg. 2004, 130, 1–45. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, M.R.; Felmingham, D.; Appelbaum, P.C.; Grüneberg, R.N. The Alexander Project 1998-2000: Susceptibility of pathogens isolated from community-acquired respiratory tract infection to commonly used antimicrobial agents. J. Antimicrob. Chemother. 2003, 52, 229–246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Hyndman, R.; Khandakar, Y. Automatic Time Series Forecasting: TheforecastPackage forR. J. Stat. Softw. 2008, 27, 1–22. [Google Scholar] [CrossRef] [Green Version]
- Ridda, I.; Dastouri, F.; King, C.; Yin, J.K.; Tashani, M.; Rashid, H. Vaccination of Older Adults with Dementia Against Respiratory Infections. Infect. Disord. Drug Targets 2014, 14, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Harboe, Z.B.; Dalby, T.; Weinberger, D.; Benfield, T.; Mølbak, K.; Slotved, H.C.; Suppli, C.H.; Konradsen, H.B.; Valentiner-Branth, P. Impact of 13-Valent Pneumococcal Conjugate Vaccination in Invasive Pneumococcal Disease Incidence and Mortality. Clin. Infect. Dis. 2014, 59, 1066–1073. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marrie, T.J.; Tyrrell, G.J.; Garg, S.; Vanderkooi, O.G. Factors Predicting Mortality in Invasive Pneumococcal Disease in Adults in Alberta. Medicine 2011, 90, 171–179. Available online: https://www.ncbi.nlm.nih.gov/pubmed/21512414 (accessed on 28 January 2021). [CrossRef] [PubMed]
- Wagenvoort, G.H.; Sanders, E.A.; De Melker, H.E.; Van Der Ende, A.; Vlaminckx, B.J.; Knol, M.J. Long-term mortality after IPD and bacteremic versus non-bacteremic pneumococcal pneumonia. Vaccine 2017, 35, 1749–1757. [Google Scholar] [CrossRef]
- Horácio, A.N.; Silva-Costa, C.; Lopes, J.P.; Ramirez, M.; Cristino, J.M.; Portuguese Group for the Study of Streptococcal Infections; Vaz, T.; Gião, M.; Ferreira, R.; Fonseca, A.B.; et al. Serotype 3 Remains the Leading Cause of Invasive Pneumococcal Disease in Adults in Portugal (2012–2014) Despite Continued Reductions in Other 13-Valent Conjugate Vaccine Serotypes. Front. Microbiol. 2016, 7, 1616. [Google Scholar] [CrossRef] [Green Version]
- Slotved, H.-C.; Dalby, T.; Harboe, Z.B.; Valentiner-Branth, P.; de Casadevante, V.F.; Espenhain, L.; Fuursted, K.; Konradsen, H.B. The incidence of invasive pneumococcal serotype 3 disease in the Danish population is not reduced by PCV-13 vaccination. Heliyon 2016, 2, e00198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- LeBlanc, J.J.; ElSherif, M.; Ye, L.; MacKinnon-Cameron, D.; Li, L.; Ambrose, A.; Hatchette, T.F.; Lang, A.L.; Gillis, H.; Martin, I.; et al. Burden of vaccine-preventable pneumococcal disease in hospitalized adults: A Canadian Immunization Research Network (CIRN) Serious Outcomes Surveillance (SOS) network study. Vaccine 2017, 35, 3647–3654. [Google Scholar] [CrossRef] [PubMed]
- Andrews, N.J.; Waight, P.A.; Burbidge, P.; Pearce, E.; Roalfe, L.; Zancolli, M.; Slack, M.; Ladhani, S.N.; Miller, E.; Goldblatt, D. Serotype-specific effectiveness and correlates of protection for the 13-valent pneumococcal conjugate vaccine: A postlicensure indirect cohort study. Lancet Infect. Dis. 2014, 14, 839–846. [Google Scholar] [CrossRef]
- Choi, E.H.; Zhang, F.; Lu, Y.-J.; Malley, R. Capsular Polysaccharide (CPS) Release by Serotype 3 Pneumococcal Strains Reduces the Protective Effect of Anti-Type 3 CPS Antibodies. Clin. Vaccine Immunol. 2016, 23, 162–167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Song, J.-H.; Dagan, R.; Klugman, K.P.; Fritzell, B. The relationship between pneumococcal serotypes and antibiotic resistance. Vaccine 2012, 30, 2728–2737. [Google Scholar] [CrossRef] [PubMed]
- González-Díaz, A.; Càmara, J.; Ercibengoa, M.; Cercenado, E.; Larrosa, N.; Quesada, M.; Fontanals, D.; Cubero, M.; Marimón, J.; Yuste, J.; et al. Emerging non-13-valent pneumococcal conjugate vaccine (PCV13) serotypes causing adult invasive pneumococcal disease in the late-PCV13 period in Spain. Clin. Microbiol. Infect. 2020, 26, 753–759. [Google Scholar] [CrossRef] [PubMed]
- Chan, C.C.; Subramanian, R.; Chong, P.; Nelson, E.A.S.; Lam, H.; Li, A.M.; Ip, M. Pneumococcal carriage in young children after introduction of PCV13 in Hong Kong. Vaccine 2016, 34, 3867–3874. [Google Scholar] [CrossRef] [PubMed]
- Liyanapathirana, V.; Nelson, E.A.S.; Ang, I.; Subramanian, R.; Ma, H.; Ip, M. Emergence of serogroup 15 Streptococcus pneumoniae of diverse genetic backgrounds following the introduction of pneumococcal conjugate vaccines in Hong Kong. Diagn. Microbiol. Infect. Dis. 2015, 81, 66–70. [Google Scholar] [CrossRef]
- Hurley, D.; Griffin, C.; Young, M.; Scott, D.A.; Pride, M.W.; Scully, I.L.; Ginis, J.; Severs, J.; Jansen, K.U.; Gruber, W.C.; et al. Safety, Tolerability, and Immunogenicity of a 20-Valent Pneumococcal Conjugate Vaccine (PCV20) in Adults 60 to 64 Years of Age. Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef]
- Torumkuney, D.; van, P.H.; Thinh, L.Q.; Koo, S.H.; Tan, S.H.; Lim, P.Q.; Sivhour, C.; Lamleav, L.; Somary, N.; Sosorphea, S.; et al. Results from the Survey of Antibiotic Resistance (SOAR) 2016–18 in Vietnam, Cambodia, Singapore and the Philippines: Data based on CLSI, EUCAST (dose-specific) and pharmacokinetic/pharmacodynamic (PK/PD) breakpoints. J. Antimicrob. Chemother. 2020, 75, i19–i42. [Google Scholar] [CrossRef] [PubMed]

| No. of Patients (N = 774) | 16–49 Years (N = 94) | 50–64 Years (N = 180) | 65–74 Years (N = 217) | ≥75 Years (N = 283) | p Value | |
|---|---|---|---|---|---|---|
| n (%) | ||||||
| Patient Characteristics | ||||||
| Sex | ||||||
| Males | 587 (75.8) | 53 (56.4) | 119 (66.1) | 186 (85.7) | 229 (80.9) | <0.001 |
| Females | 187 (24.2) | 41 (43.6) | 61 (33.9) | 31 (14.3) | 54 (19.1) | <0.001 |
| Comorbid Conditions | ||||||
| Diabetes | 127 (16.4) | 7 (7.45) | 23 (12.8) | 44 (20.3) | 53 (18.7) | 0.014 |
| Chronic obstructive pulmonary disease (COPD) (N = 755) | 198 (26.2) | 5 (5.32) | 14 (8.00) (N = 176) | 69 (33.2) (N = 208) | 110 (39.7) (N = 277) | <0.001 |
| Asthma | 53 (6.85) | 13 (13.8) | 12 (6.67) | 15 (6.91) | 13 (4.59) | 0.024 |
| History of tuberculosis (N = 769) | 87 (11.3) | 9 (9.60) | 9 (5.05) (N = 178) | 25 (11.6) (N = 215) | 44 (15.6) (N = 282) | 0.006 |
| Bronchiectasis | 45 (5.81) | 1 (1.06) | 9 (5.00) | 15 (6.91) | 20 (7.07) | 0.144 |
| Hypertension | 240 (31.0) | 7 (7.45) | 35 (19.4) | 79 (36.4) | 119 (42.0) | <0.001 |
| Ischaemic heart disease | 68 (8.79) | 2 (2.13) | 9 (5.00) | 17 (7.83) | 40 (14.1) | <0.001 |
| Congestive cardiac failure | 31 (4.01) | 2 (2.13) | 4 (2.22) | 6 (2.76) | 19 (6.71) | 0.035 |
| Cerebrovascular disease | 79 (10.2) | 1 (1.06) | 12 (6.67) | 28 (12.9) | 38 (13.4) | 0.001 |
| Hemiplegia or paraplegia | 20 (2.58) | 1 (1.06) | 3 (1.67) | 6 (2.76) | 10 (3.53) | 0.474 |
| Dementia | 28 (3.62) | 0 | 0 | 3 (1.38) | 25 (8.83) | <0.001 |
| Rheumatological diseases | 80 (10.3) | 5 (5.32) | 17 (9.44) | 29 (13.4) | 29 (10.2) | 0.177 |
| Presence of malignancy | 155 (20.0) | 7 (7.45) | 44 (24.4) | 45 (20.7) | 59 (20.8) | 0.009 |
| Liver disease | 59 (7.62) | 6 (6.38) | 25 (13.9) | 15 (6.91) | 13 (4.59) | 0.003 |
| Peptic ulcer disease | 42 (5.43) | 2 (2.13) | 6 (3.33) | 12 (5.53) | 22 (7.77) | 0.087 |
| Chronic renal disease (N = 773) | 57 (7.37) | 5 (5.32) | 13 (7.26) (N = 179) | 12 (5.53) | 27 (9.54) | 0.307 |
| Charlson Comorbidity Score | ||||||
| Mean score (SD) | 2.03 (± 2.43) | 0.947 (± 1.77) | 2.72 (± 2.99) | 2.07 (± 2.26) | 2.21 (± 2.28) | <0.001 |
| No. with Score ≥ 1, n (%) | 569 (73.5) | 40 (42.6) | 119 (66.1) | 175 (80.6) | 235 (83.0) | <0.001 |
| No. with Score ≥ 2, n (%) | 329 (42.5) | 17 (18.1) | 73 (40.6) | 102 (47.0) | 137(48.4) | <0.001 |
| Score ≥ 3, n (%) | 200 (26.2) | 9 (9.97) | 48 (26.8) | 53 (24.7) | 90 (32.6) | <0.001 |
| Disease | ||||||
| Disease Characteristics | ||||||
| Community acquired Infections (CAI) (N = 771) | 676 (87.7) | 86 (91.5) | 154 (86.5) | 187 (86.2) | 249 (88.3) | 0.564 |
| Invasive infections (IPD) * | 110 (14.2) | 17 (18.1) | 33 (18.3) | 20 (9.22) | 40 (14.1) | 0.044 |
| Broad disease category | ||||||
| Primary Bacteraemia | 14 (1.81) | 2 (2.13) | 5 (2.78) | 5 (2.30) | 2 (0.71) | 0.356 |
| Meningitis | 6 (0.78) | 1 (1.06) | 2 (1.11) | 1 (0.46) | 2 (0.71) | 0.882 |
| Pneumonia | 475 (61.4) | 64 (68.1) | 115 (63.9) | 109 (50.2) | 187 (66.1) | 0.001 |
| Bacteraemic pneumonia | 88 18.52) | 14 (21.9) | 25 (21.7) | 13 (11.95.99) | 36 (19.3) | 0.029 |
| Non-bacteraemic pneumonia | 305 (64.2) | 45 (70.3) | 82 (71.3) | 71 (65.1) | 107 (57.2) | 0.018 |
| Pneumonia with other lung conditions | 82 (17.3) | 5 (7.8) | 8 (7.0) | 25 (22.9) | 44 (23.5) | 0.001 |
| Exacerbation of other lung conditions | 125 (26.3) | 5 (7.8) | 9 (7.8) | 56 (51.4) | 55 (29.4) | <0.001 |
| Disease Progression | ||||||
| Presence of any complication | 149 (19.3) | 21 (22.3) | 39 (21.7) | 32 (14.7) | 57 (20.1) | 0.238 |
| Pleural effusion | 20 (2.58) | 5 (5.32) | 8 (4.44) | 3 (1.38) | 4 (1.41) | 0.045 |
| Septic shock | 46 (5.94) | 10 (10.6) | 20 (11.1) | 7 (3.23) | 9 (3.18) | <0.001 |
| Respiratory failure | 96 (12.4) | 15 (16.0) | 19 (10.6) | 24 (11.1) | 38 (13.4) | 0.514 |
| Lung collapse | 9 (1.16) | 0 | 4 (2.22) | 0 | 5 (1.77) | 0.097 |
| Renal failure | 27 (3.49) | 5 (5.32) | 9 (5.00) | 6 (2.76) | 7 (2.47) | 0.339 |
| Lung abscess | 5 (0.65) | 1 (1.06) | 3 (1.67) | 1 (0.46) | 0 | 0.162 |
| ICU admission (N = 770) | 70 (9.09) | 17 (18.1) | 28 (15.9) (N = 179) | 11 (5.12) (N = 215) | 14 (4.96) (N = 282) | <0.001 |
| Mean length of hospitalisation (days) | 7.71 (SD 10.1) | 7.51 (SD 13.6) | 8.94 (SD 11.5) | 7.16 (SD 8.26) | 7.42 (SD 8.69) | 0.320 |
| Outcome | ||||||
| Death at discharge | 36 (4.65) | 2 (2.13) | 10 (5.56) | 8 (3.69) | 16 (5.65) | 0.427 |
| Died within 48 h of admission | 10 (1.29) | 0 | 2 (1.11) | 2 (0.92) | 6 (2.12) | 0.387 |
| 30-day mortality (N = 765) | 60 (7.84) | 1 (1.08) (N = 93) | 10 (5.59) (N = 179) | 15 (6.98) (N = 215) | 34 (12.2) (N = 278) | 0.002 |
| Common Serotype/Group | Overall N (%) | 16–49 Years n (%) | 50–64 Years n (%) | 65–74 Years n (%) | ≥75 Years n (%) | p-Value |
|---|---|---|---|---|---|---|
| 19F | 192 (24.9) | 13 (13.8) | 28 (15.6) | 58 (26.7) | 93 (32.9) | <0.001 |
| 3 | 135 (17.5) | 25 (26.6) | 42 (23.3) | 33 (15.2) | 35 (12.4) | 0.001 |
| Serogroup 6 (6A/B/C/D) | 78 (10.1) | 9 (9.58) | 20 (11.1) | 24 (11.1) | 25 (8.83) | 0.813 |
| 19A | 48 (6.22) | 9 (9.58) | 11 (6.11) | 16 (7.37) | 12 (4.24) | 0.238 |
| 14 | 43 (5.57) | 5 (5.32) | 8 (4.44) | 9 (4.15) | 21 (7.42) | 0.372 |
| 23F | 41 (5.31) | 1 (1.06) | 11 (6.11) | 14 (6.45) | 15 (5.30) | 0.243 |
| Serogroup (15 A/B/C/F) | 33 (4.28) | 4 (4.26) | 10 (5.56) | 9 (4.15) | 10 (3.53) | 0.774 |
| Others ** | 202 (26.2) | 28 (29.8) | 50 (27.8) | 52 (23.9) | 73 (25.8) | 0.793 |
| Vaccine related serogroups | ||||||
| PCV 7 types | 326 (42.2) | 25 (26.6) | 59 (32.8) | 96 (44.2) | 146 (51.6) | <0.001 |
| PCV10 types | 330 (42.8) | 25 (26.6) | 59 (32.8) | 98 (45.2) | 148 (52.3) | <0.001 |
| PCV13 types | 532 (68.9) | 61 (64.9) | 117 (65.0) | 153 (70.5) | 201 (71.0) | 0.420 |
| PCV7 Serotypes (N = 326) | PCV10 Serotypes (N = 330) | PCV 13 Serotypes (N = 532) | Non PCV 13 Types (N = 242) | 19F (N = 192) | 3 (N = 135) | 19A (N = 48) | Serogroup 6 (N = 78) | 14 (N = 43) | 23F (N = 41) | Serogroup 15 (N = 33) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Year (N) | Total Isolates Per Year (%) | ||||||||||
| 2009 (127) | 72 (56.7) | 73 (57.5) | 90 (70.9) | 37 (29.1) | 33 (26.0) | 14 (11.0) | 2 (1.58) | 15 (11.8) | 12 (9.45) | 12 (9.45) | 5 (3.94) |
| 2010 (117) | 47 (40.2) | 48 (41.0) | 73 (62.4) | 44 (37.6) | 28 (23.9) | 13 (11.1) | 6 (5.13) | 18 (15.4) | 7 (5.98) | 5 (4.27) | 4 (3.42) |
| 2011 (121) | 62 (51.2) | 62 (51.2) | 87 (71.9) | 34 (28.1) | 38 (31.4) | 16 (13.2) | 8 (6.61) | 9 (7.44) | 8 (6.61) | 7 (5.79) | 4 (3.31) |
| 2012 (93) | 50 (53.8) | 51 (54.8) | 71 (76.3) | 22 (23.7) | 28 (30.1) | 19 (20.4) | 1 (1.08) | 12 (12.9) | 4 (4.30) | 9 (9.68) | 2 (2.15) |
| 2013 (81) | 27 (33.3) | 27 (33.3) | 46 (56.8) | 35 (42.3) | 16 (19.8) | 9 (11.1) | 6 (7.41) | 9 (11.1) | 5 (6.17) | 3 (3.70) | 8 (9.88) |
| 2014 (69) | 27 (39.1) | 27 (39.1) | 59 (85.5) | 10 (14.5) | 19 (27.5) | 18 (26.1) | 10 (14.5) | 6 (8.70) | 5 (7.25) | 3 (4.35) | 3 (4.35) |
| 2015 (67) | 18 (26.9) | 18 (26.9) | 42 (62.7) | 25 (37.3) | 11 (16.4) | 17 (25.4) | 5 (7.46) | 6 (8.96) | 1 (1.49) | 2 (2.99) | 5 (7.46) |
| 2016 (44) | 9 (20.5) | 9 (20.5) | 24 (54.5) | 20 (45.5) | 8 (18.2) | 9 (20.5) | 6 (13.6) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 1 (2.27) |
| 2017 (55) | 14 (25.5) | 15 (27.3) | 40 (72.7) | 15 (27.3) | 11 (20.0) | 20 (36.4) | 4 (7.27) | 3 (5.46) | 1 (1.82) | 0 (0.00) | 1 (1.82) |
| p value | <0.001 | <0.001 | 0.001 | 0.001 | 0.265 | <0.001 | 0.005 | 0.135 | 0.211 | 0.059 | 0.220 |
| Antibiotic | MIC Range (µg/mL) | MIC50 (µg/mL) | MIC90 (µg/mL) | % Non-Susceptible (n) | % Sensitive (n) | % Intermediate (n) | % Resistant (n) |
|---|---|---|---|---|---|---|---|
| Ciprofloxacin | ≤0.25–>32 | 1 | 2 | - | - | - | - |
| Levofloxacin | ≤0.25–>32 | 1 | 1 | 2.23 (17) | 97.8 (747) | 0.13 (1) | 2.09 (16) |
| Lincomycin | ≤0.25–>32 | >32 | >32 | - | - | - | - |
| Vancomycin | ≤0.03–1 | 0.25 | 0.5 | 0 | 100 (764) | - | - |
| Cefotaxime (non-meningitis) | ≤0.015–8 | 0.25 | 8 | 25.5 (195) | 74.5 (569) | 8.90 (68) | 16.6 (127) |
| Cefotaxime (meningitis) | ≤0.015–8 | 0.25 | 8 | 39.5 (302) | 60.5 (462) | 14.0 (107) | 25.5 (195) |
| Penicillin (non-meningitis) | ≤0.008–8 | 0.25 | 4 | 19.9 (152) | 80.1 (612) | 19.5 (149) | 0.39 (3) |
| Penicillin (meningitis) | ≤0.008–8 | 0.25 | 4 | 54.1 (413) | 45.9 (351) | 54.1 (413) | |
| Chloramphenicol | ≤1–32 | 2 | 4 | 8.25 (63) | 91.8 (701) | - | 8.25 (63) |
| Erythromycin | ≤0.015–>64 | >64 | >64 | 78.9 (603) | 21.1 (161) | 1.57 (12) | 77.4 (591) |
| Tetracycline | 0.03–>32 | 32 | >32 | 82.5 (630) | 17.5 (134) | 2.49 (19) | 80.0 (611) |
| Linezolid | ≤0.12–2 | 0.5 | 1 | 0 | 100 (764) | - | - |
| CLSI Breakpoints | EUCAST Breakpoints | PK/PD Breakpoints | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Antibiotic | MIC Range (µg/mL) | % Sensitive (n) | % Intermediate (n) | % Resistant (n) | % Sensitive (n) | %Intermediate (n) | % Resistant (n) | % Sensitive (n) | % Resistant (n) |
| Ciprofloxacin | ≤0.25–>32 | - | - | - | - | - | - | - | - |
| Levofloxacin | ≤0.25–>32 | 97.8 (747) | 0.13 (1) | 2.09 (16) | 0 | 97.8 (747) | 2.23 (17) | 97.6 (746) | 2.36 (18) |
| Lincomycin | ≤0.25–>32 | - | - | - | - | - | - | - | - |
| Vancomycin | ≤0.03–1 | 100 (764) | 0 | 0 | 100 (764) | 0 | 0 | - | - |
| Cefotaxime (non-meningitis) | ≤0.015–8 | 74.5 (569) | 8.90 (68) | 16.6 (127) | 60.5 (462) | 22.9 (175) | 16.6 (127) | - | - |
| Cefotaxime (meningitis) | ≤0.015–8 | 60.5 (462) | 14.0 (107) | 25.5 (195) | - | - | - | - | - |
| Penicillin (non-meningitis) | ≤0.008–8 | 80.1 (612) | 19.5 (149) | 0.39 (3) | 45.9 (351) | 34.2 (261) | 19.9 (152) | - | - |
| Penicillin (meningitis) | ≤0.008–8 | 45.9 (351) | - | 54.1 (413) | - | - | 54.1 (413) | - | - |
| Chloramphenicol | ≤1–32 | 91.8 (701) | - | 8.25 (63) | 94.4 (721) | - | 5.63 (43) | 91.8 (701) | 8.25 (63) |
| Erythromycin | ≤0.015–>64 | 21.1 (161) | 1.57 (12) | 77.4 (591) | 21.1 (161) | 1.57 (12) | 77.4 (591) | 21.1 (161) | 78.9 (603) |
| Tetracycline | 0.03–>32 | 17.5 (134) | 2.49 (19) | 80.0 (611) | 17.5 (134) | 2.49 (19) | 80.0 (611) | - | - |
| Linezolid | ≤0.12–2 | 100 (764) | 0 | 0 | 100 (764) | 0 | 0 | - | - |
| Serotypes/Groups | 19F (N = 192) | 3 (N = 135) * | 6 (N = 78) ** | 14 (N = 43) | 19A (N = 48) *** | 23F (N = 41) | 15 (N = 33) | |
|---|---|---|---|---|---|---|---|---|
| Outcome | n (%) | p Value | ||||||
| Antibiotic Non-Susceptibility | ||||||||
| Penicillin (non-meningitis) | 118 (61.5) | 1 (0.76) | 1 (1.32) | 1 (2.33) | 26 (55.3) | 0 | 0 | <0.001 |
| Penicillin (meningitis) | 178 (92.7) | 3 (2.27) | 57 (75.0) | 38 (88.4) | 41 (87.2) | 35 (85.4) | 15 (45.5) | <0.001 |
| Cefotaxime (non-meningitis) | 150 (78.1) | 1 (0.76) | 4 (5.26) | 3 (6.98) | 20 (42.6) | 9 (22.0) | 3 (9.09) | <0.001 |
| Cefotaxime (meningitis) | 167 (87.0) | 2 (1.52) | 25 (32.9) | 18 (41.9) | 37 (78.7) | 31 (75.6) | 6 (18.2) | <0.001 |
| Erythromycin | 186 (96.9) | 72 (54.6) | 72 (94.7) | 37 (86.1) | 44 (93.6) | 37 (90.2) | 28 (84.9) | <0.001 |
| Tetracycline | 183 (95.3) | 94 (71.2) | 67 (88.2) | 22 (51.2) | 45 (95.7) | 39 (95.1) | 25 (75.8) | <0.001 |
| Disease outcomes | ||||||||
| Invasive disease | 7 (3.65) | 37 (27.4) | 2 (2.56) | 11 (25.6) | 9 (18.8) | 3 (7.32) | 9 (27.3) | <0.001 |
| Bacteraemia | 0 | 3 (2.22) | 0 | 2 (4.65) | 1 (2.08) | 1 (2.44) | 3 (9.09) | 0.026 |
| Meningitis | 1 (0.52) | 0 | 0 | 0 | 1 (2.08) | 0 | 0 | 0.210 |
| Bacteraemic pneumonia | 6 (3.14) | 34 (25.2) | 2 (2.56) | 9 (20.9) | 7 (14.6) | 1 (2.44) | 6 (18.2) | <0.001 |
| Non-bacteraemic pneumonia | 76 (39.6) | 61 (45.2) | 35 (44.9) | 17 (39.5) | 19 (39.6) | 18 (43.9) | 9 (27.3) | 0.302 |
| Pneumonia with other lung conditions | 9(9.90) | 11(8.15) | 9(18.8) | 9(11.5) | 5(11.6) | 2(4.88) | 2(6.06) | 0.423 |
| Exacerbation of other lung conditions | 42 (21.9) | 4 (2.96) | 7 (14.6) | 16 (20.5) | 3 (6.98) | 8 (19.5) | 6 (18.2) | <0.001 |
| Presence of complications | 29 (15.1) | 39 (28.9) | 12 (15.4) | 7 (16.3) | 18 (37.5) | 5 (12.2) | 7 (21.2) | 0.001 |
| Pleural effusions | 3 (1.56) | 9 (6.67) | 0 | 2 (4.65) | 2 (4.17) | 0 | 0 | 0.049 |
| Respiratory failure | 20 (10.4) | 29 (21.5) | 9 (11.5) | 4 (9.30) | 10 (20.8) | 4 (9.76) | 4 (12.1) | 0.011 |
| Renal failure | 3 (1.56) | 13 (9.63) | 1 (1.28) | 1 (2.33) | 2 (4.17) | 0 | 1 (3.03) | 0.006 |
| Septic shock | 4 (2.09) | 19(14.1) | 2 (2.56) | 2 (4.65) | 6 (12.5) | 2 (4.88) | 2 (6.06) | <0.001 |
| ICU admissions | 4 (2.08) | 29 (21.5) | 6 (7.69) | 4 (9.30) | 10 (20.8) | 2 (4.88) | 2 (6.06) | <0.001 |
| Died within 48 h | 0 | 3 (2.22) | 0 | 0 | 2 (4.17) | 0 | 6 (6.06) | 0.061 |
| 30 day mortality **** | 16 (8.51) | 8 (6.02) | 3 (3.85) | 0 | 8 (16.7) | 2 (4.88) | 4 (12.1) | 0.096 |
| Factor | Odds Ratio (95% CI) | Univariate Analysis | Odds Ratio (95% CI) | Multivariate Analysis |
|---|---|---|---|---|
| p Value | p Value | |||
| Age ≥ 49 years | 8.86 (1.21–6.47) | 0.010 | ||
| Age ≥ 65 years | 2.62 (1.34–5.13) | 0.004 | ||
| Age ≥ 75 years | 2.47 (1.45–4.21) | 0.001 | 4.61 (1.25–17.0) | 0.022 |
| Invasive disease | 4.17 (2.35–7.38) | <0.001 | ||
| Bacteraemic pneumonia | 3.64 (1.97–6.73) | <0.001 | ||
| Meningitis | 12.3 (2.43–62.4) | 0.008 | ||
| Exacerbation of existing lung conditions | 0.166 (0.04–0.691) | 0.005 | ||
| Presence of complications | 5.43 (3.15–9.35) | <0.001 | 4.08 (1.02–16.3) | 0.046 |
| Pleural effusion | 4.18 (1.47–11.9) | 0.016 | 6.77 (1.17–39.4) | 0.033 |
| Septic shock | 3.38 (1.54–7.41) | 0.005 | ||
| Respiratory failure | 3.18 (1.73–5.84) | <0.001 | ||
| Lung collapse | 6.13 (1.49–25.1) | 0.027 | ||
| Renal failure | 4.77 (1.92–11.9) | 0.003 | ||
| ICU admission | 3.20 (1.63–6.27) | <0.001 | 9.01 (1.28–63.4) | 0.027 |
| Intubation/ventilatory support | 2.49 (1.13–6.27) | 0.027 | ||
| Serotype 19A | 2.56 (1.14–5.75) | 0.045 | ||
| Charlson comorbidity score ≥ 2 | 3.22 (1.83–5.66) | <0.001 | ||
| Charlson comorbidity score ≥ 3 | 2.35 (1.37–4.03) | 0.002 | ||
| Presence of malignancy | 2.98 (1.72–5.16) | <0.001 | ||
| Dementia | 3.62 (1.83–5.66) | <0.001 | ||
| Congestive cardiac failure | 2.37 (0.877–6.43) | 0.087 | ||
| Hospitalisation within 3 months prior to admission | 2.55 (1.49–4.37) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Subramanian, R.; Liyanapathirana, V.; Barua, N.; Sun, R.; Wang, M.H.; Ng, R.; Nelson, E.A.S.; Hui, D.S.; Ip, M. Persistence of Pneumococcal Serotype 3 in Adult Pneumococcal Disease in Hong Kong. Vaccines 2021, 9, 756. https://doi.org/10.3390/vaccines9070756
Subramanian R, Liyanapathirana V, Barua N, Sun R, Wang MH, Ng R, Nelson EAS, Hui DS, Ip M. Persistence of Pneumococcal Serotype 3 in Adult Pneumococcal Disease in Hong Kong. Vaccines. 2021; 9(7):756. https://doi.org/10.3390/vaccines9070756
Chicago/Turabian StyleSubramanian, Reema, Veranja Liyanapathirana, Nilakshi Barua, Rui Sun, Maggie Haitian Wang, Rita Ng, Edmund A. S. Nelson, David S. Hui, and Margaret Ip. 2021. "Persistence of Pneumococcal Serotype 3 in Adult Pneumococcal Disease in Hong Kong" Vaccines 9, no. 7: 756. https://doi.org/10.3390/vaccines9070756
APA StyleSubramanian, R., Liyanapathirana, V., Barua, N., Sun, R., Wang, M. H., Ng, R., Nelson, E. A. S., Hui, D. S., & Ip, M. (2021). Persistence of Pneumococcal Serotype 3 in Adult Pneumococcal Disease in Hong Kong. Vaccines, 9(7), 756. https://doi.org/10.3390/vaccines9070756






