Global Prevalence and Drivers of Dental Students’ COVID-19 Vaccine Hesitancy
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Instrument
2.4. Ethical Considerations
2.5. Statistical Analysis
3. Results
3.1. Demographic Characteristics
3.2. COVID-19-Related Experience
3.3. COVID-19 Vaccine-Related Attitudes
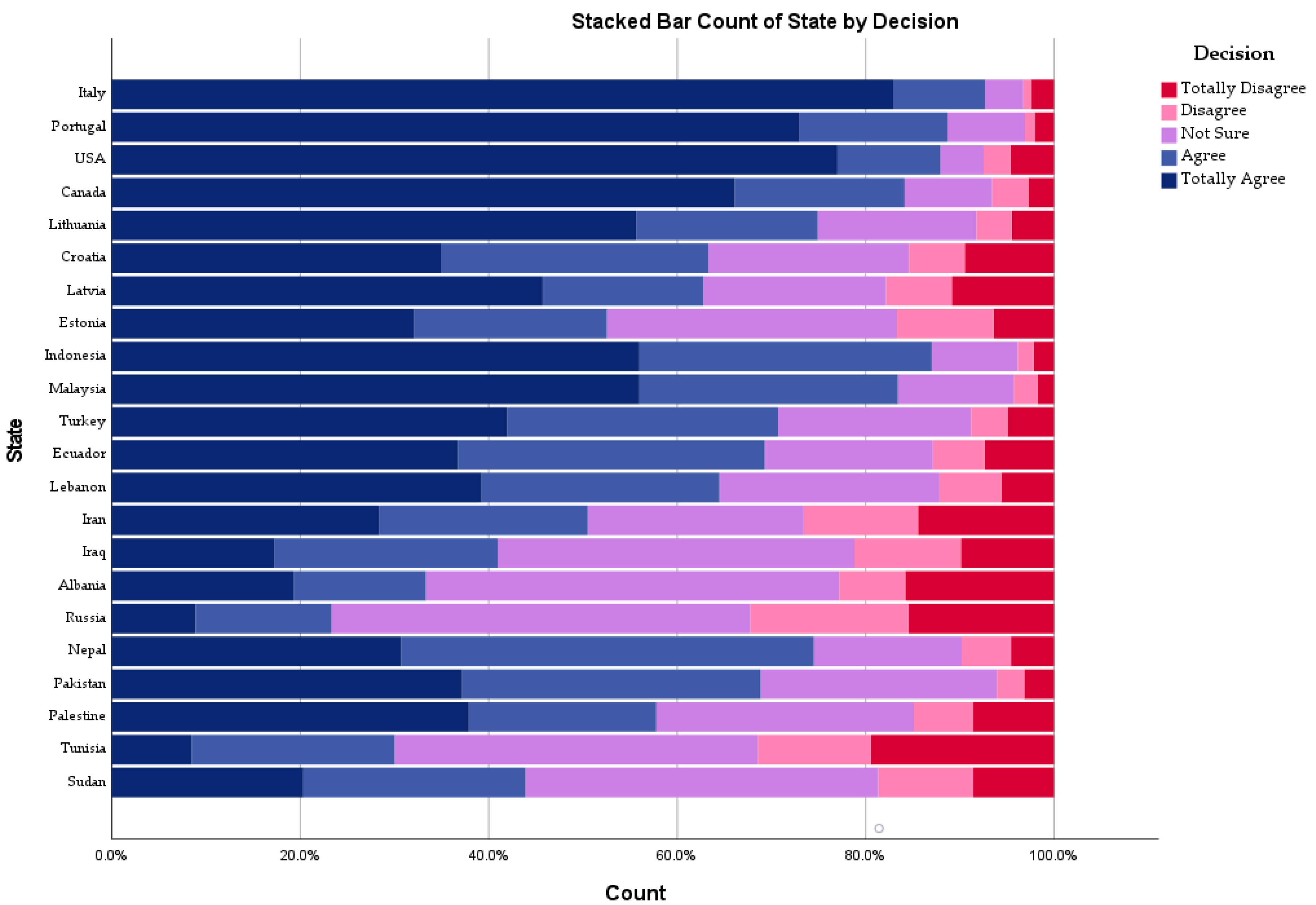
3.4. Drivers of COVID-19 Vaccine-Related Attitude
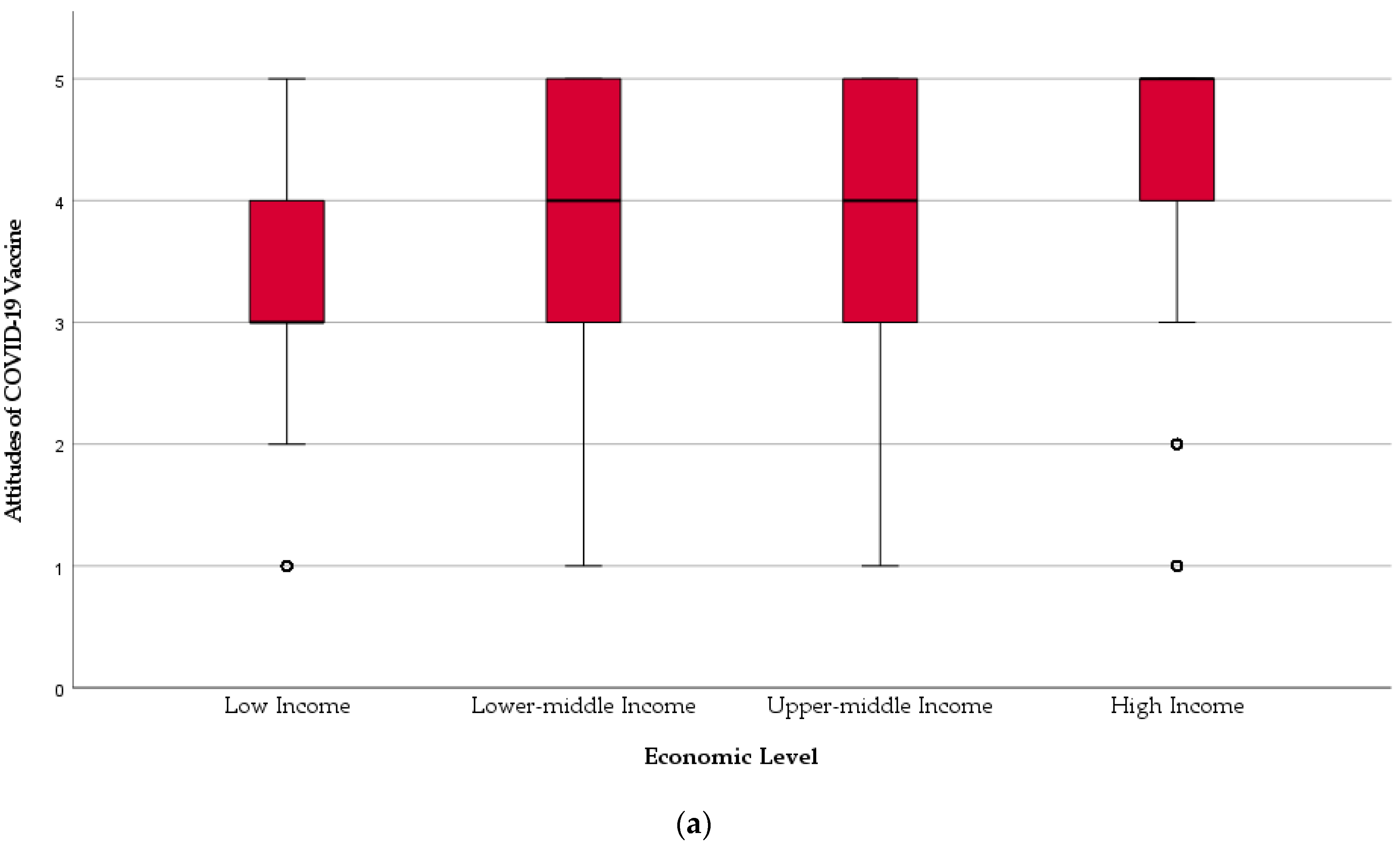
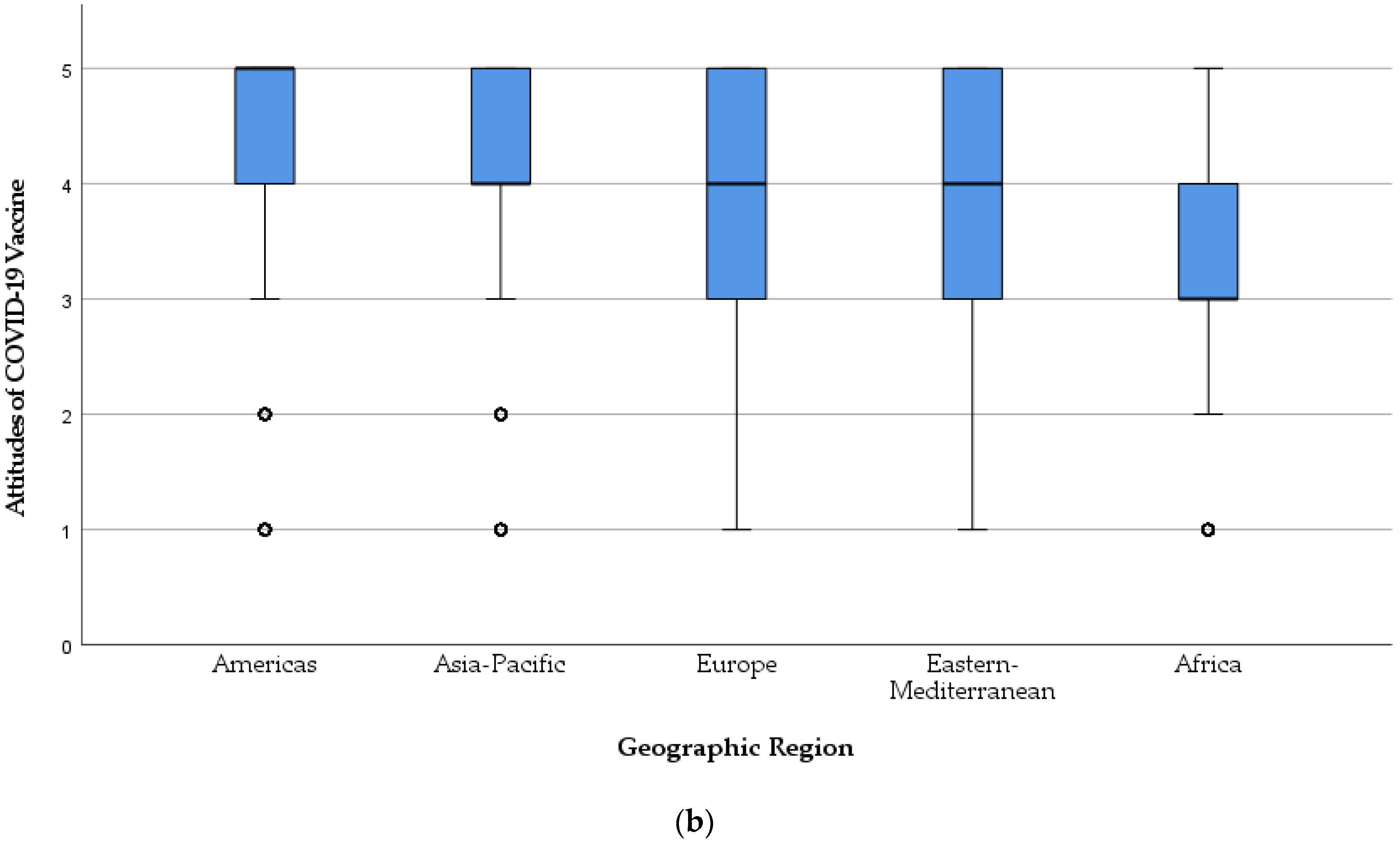
3.5. Demographic Determinants of COVID-19 Vaccine-Related Attitude
3.6. Drivers of Dental Students’ COVID-19 Vaccine Acceptance
3.6.1. Contextual Drivers
3.6.2. Individual Drivers
3.6.3. Vaccine-Specific Drivers
4. Discussion
4.1. Study Strengths
4.2. Study Limitations
4.3. Study Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Members of IADS-SCORE Consortium
- Faculty of Dentistry, McGill University, Canada (Jacques Jaar); Schulich School of Medicine & Dentistry, Western University, Canada (Nima Lighvan); Faculty of Dentistry, University of British Columbia, Canada (Karen Lin);
- Faculty of Dentistry, SEGi University, Malaysia (Sandy Tan Qing Wen); Faculty of Dentistry, University of Malaya, Malaysia (Tan Hian Wei);
- School of Dentistry, Kathmandu University School of Medical Sciences, Nepal (Nitesh Singh);
- Department of Oral and Maxillofacial Surgery, School of Dentistry, Zanjan University of Medical Sciences, Iran (Parsa Firoozi); Faculty of Dentistry, Islamic Azad University Isfahan, Iran (Mohammad Mostafa Aghamohseni; Samin Sirous);
- Institute of Dentistry, CMH Lahore Medical College and Institute of Dentistry, Pakistan (Aneeqa Aslam; Maha Sohail); Dental College, Akhtar Saeed Medical and Dental College, Pakistan (Mehroz Ahmad Khan);
- Faculty of Dentistry, Beirut Arab University, Lebanon (Julien Issa; Mirna Abou Ibrahim);
- Faculty of Dental Medicine, Catholic University of Portugal, Portugal (António Coimbra Amaral);
- Faculty of Dental Sciences, Aldent University, Albania (Ersid Domnori);
- Faculty of Odontology, Universidad San Francisco De Quito, Ecuador (Jorge Ayala); Faculty of Odontology, Catholic University of Cuenca, Ecuador (Maria Sol Medina);
- Faculty of Dentistry, Universitas Indonesia, Indonesia (Viandra Tjokroadiredjo; Farih Aminah);
- Department of Dentistry, Al-rafidain University College, Iraq (Noor Sarmad); College of Dentistry, Uruk University, Iraq (Nabaa Abduladheem); Department of Dentistry, Al-rasheed University College, Iraq (Batool Mohammed);
- Department of Neuroscience, Reproductive Sciences and Dentistry, University of Naples Federico II, Italy (Matteo Cafasso); Department of Biomedical, Surgical and Dental Sciences, School of Dentistry, University of Milan, Italy (Gregorio Tortora); Department of Medicine and Surgery, School of Dentistry, University of Insubria, Italy (Anita Homayuni);
- Faculty of Dentistry, Rīga Stradiņš University, Latvia (Kristīne Romanovska);
- Faculty of Odontology, Medical Academy, Lithuanian University of Health Sciences, Lithuania (Kristė Trijonytė; Julius Mikonis);
- Faculty of Dentistry, University of Khartoum, Sudan (Ahmed Abdalla); Faculty of Dentistry, Al Neelain University, Sudan (Zeinab Hassan); Faculty of Dentistry, University of Medical Sciences and Technology, Sudan (Aya Abdelrahim);
- Faculty of Dental Medicine, Monastir University, Tunisia (Haythem Ben Hadj Belgacem; Maya Fedhila);
- Faculty of Dentistry, Istanbul University, Turkey (İrem Erdoğdu); Faculty of Dentistry, Beykent University, Turkey (Berk Koparan); Faculty of Dentistry, Yeditepe University, Turkey (Ezgi Yeşïltan); Faculty of Dentistry, Marmara University, Turkey (Serap Beşïroğlu);
- Faculty of Dentistry, Ural State Medical University, Russia (Tatiana Spitsyna);
- Faculty of Dental Medicine, University of Rijeka, Croatia (Valentina Mar-asović; Elizabeta Vrkljan; Lovre Labura);
- Institute of Dentistry, Faculty of Medicine, University of Tartu, Estonia (Estelle Saavaste);
- College of Dentistry, University of Florida, United States of America (Natalie Atyeo); School of Dentistry, University of Michigan, United States of America (Alexandra Herzog);
- Oral Health Research and Promotion Unit, Faculty of Dentistry, Al-Quds University, Palestine (Mayar Danadneh);
References
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Strategic Advisory Group of Experts on Immunization (SAGE). Vaccine Hesitancy Survey Questions Related to SAGE Vaccine Hesitancy Matrix. Available online: https://www.who.int/immunization/programmes_systems/Survey_Questions_Hesitancy.pdf (accessed on 14 March 2021).
- Butler, R.; MacDonald, N.E. Diagnosing the determinants of vaccine hesitancy in specific subgroups: The Guide to Tailoring Immunization Programmes (TIP). Vaccine 2015, 33, 4176–4179. [Google Scholar] [CrossRef]
- Verger, P.; Fressard, L.; Collange, F.; Gautier, A.; Jestin, C.; Launay, O.; Raude, J.; Pulcini, C.; Peretti-Watel, P. Vaccine Hesitancy Among General Practitioners and Its Determinants During Controversies: A National Cross-sectional Survey in France. EBioMedicine 2015, 2, 891–897. [Google Scholar] [CrossRef]
- Rubin, G.J.; Potts, H.W.W.; Michie, S. Likely uptake of swine and seasonal flu vaccines among healthcare workers. A cross-sectional analysis of UK telephone survey data. Vaccine 2011, 29, 2421–2428. [Google Scholar] [CrossRef]
- Karafillakis, E.; Dinca, I.; Apfel, F.; Cecconi, S.; Wűrz, A.; Takacs, J.; Suk, J.; Celentano, L.P.; Kramarz, P.; Larson, H.J. Vaccine hesitancy among healthcare workers in Europe: A qualitative study. Vaccine 2016, 34, 5013–5020. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Vaccine Acceptance is the Next Hurdle. Available online: https://www.who.int/news-room/feature-stories/detail/vaccine-acceptance-is-the-next-hurdle (accessed on 15 April 2021).
- Oberg, E.B.; Frank, E. Physicians’ health practices strongly influence patient health practices. J. R. Coll. Physicians Edinb. 2009, 39, 290–291. [Google Scholar] [CrossRef]
- Frank, E. Physician Health and Patient Care. JAMA 2004, 291, 637. [Google Scholar] [CrossRef]
- Royal College of Physicians and Surgeons of Canada. Physician Competency Framework 2005. Available online: http://www.royalcollege.ca/rcsite/documents/canmeds/the-7-canmeds-roles-e.pdf (accessed on 14 April 2021).
- Laschinger, H.K.; Tresolini, C.P. An exploratory study of nursing and medical students health promotion counselling self-efficacy. Nurse Educ. Today 1999, 19, 408–418. [Google Scholar] [CrossRef]
- Nouri, K.; Huber, D.; Walch, K.; Promberger, R.; Buerkle, B.; Ott, J.; Tempfer, C.B. Fertility awareness among medical and non-medical students: A case-control study. Reprod. Biol. Endocrinol. 2014, 12, 94. [Google Scholar] [CrossRef] [PubMed]
- Pinelli, C.; Neri, S.D.N.; Loffredo, L.D.C.M. Dental students’ reports of occupational exposures to potentially infectious biological material in a Brazilian School of Dentistry. Cad. Saúde Colet. 2016, 24, 162–169. [Google Scholar] [CrossRef][Green Version]
- Davide, S.; Macarelli, C.; Lam, A. Vaccination Recommendations for Oral Health Professionals. Available online: https://decisionsindentistry.com/article/vaccination-recommendations-for-oral-health-professionals/ (accessed on 15 April 2021).
- De Souza, R.; Namen, F.M.; Galan, J.; Vieira, C.; Sedano, H.O. Infection Control Measures Among Senior Dental Students in Rio de Janeiro State, Brazil. J. Public Health Dent. 2006, 66, 282–284. [Google Scholar] [CrossRef]
- Singh, A.; Purohit, B.M.; Bhambal, A.; Saxena, S.; Singh, A.; Gupta, A. Knowledge, Attitudes, and Practice Regarding Infection Control Measures Among Dental Students in Central India. J. Dent. Educ. 2011, 75, 421–427. [Google Scholar] [CrossRef]
- Shetty, S.; Prabhu, S.; Shetty, V.; Shetty, A.K. Knowledge, attitudes and factors associated with acceptability of human papillomavirus vaccination among undergraduate medical, dental and nursing students in South India. Hum. Vaccines Immunother. 2019, 15, 1656–1665. [Google Scholar] [CrossRef] [PubMed]
- Rutkoski, H.; Tay, D.L.; Dixon, B.L.; Pinzon, L.M.; Mooney, R.; Winkler, J.R.; Kepka, D. A Multi-state Evaluation of Oral Health Students’ Knowledge of Human Papillomavirus-Related Oropharyngeal Cancer and HPV Vaccination. J. Cancer Educ. 2020, 35, 1017–1025. [Google Scholar] [CrossRef] [PubMed]
- Farsi, N.J.; Al Sharif, S.; Al Qathmi, M.; Merdad, M.; Marzouki, H.; Merdad, L. Knowledge of Human Papillomavirus (HPV) and Oropharyngeal Cancer and Acceptability of the HPV Vaccine among Dental Students. Asian Pac. J. Cancer Prev. 2020, 21, 3595–3603. [Google Scholar] [CrossRef]
- Mahesh, R.; Arthi, C.; Victor, S.; AshokKumar, S. Hepatitis B Infection Awareness among Dental Graduate Students: A Cross Sectional Study. Int. Sch. Res. Not. 2014, 2014, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M.; Dababseh, D.; Eid, H.; Hasan, H.; Taim, D.; Al-Mahzoum, K.; Al-Haidar, A.; Yaseen, A.; Ababneh, N.; Assaf, A.; et al. Low COVID-19 Vaccine Acceptance Is Correlated with Conspiracy Beliefs among University Students in Jordan. Int. J. Environ. Res. Public Health 2021, 18, 2407. [Google Scholar] [CrossRef]
- Bertoncello, C.; Ferro, A.; Fonzo, M.; Zanovello, S.; Napoletano, G.; Russo, F.; Baldo, V.; Cocchio, S. Socioeconomic Determinants in Vaccine Hesitancy and Vaccine Refusal in Italy. Vaccines 2020, 8, 276. [Google Scholar] [CrossRef]
- Gerussi, V.; Peghin, M.; Palese, A.; Bressan, V.; Visintini, E.; Bontempo, G.; Graziano, E.; De Martino, M.; Isola, M.; Tascini, C. Vaccine Hesitancy among Italian Patients Recovered from COVID-19 Infection towards Influenza and Sars-Cov-2 Vaccination. Vaccines 2021, 9, 172. [Google Scholar] [CrossRef]
- Puri, N.; Coomes, E.A.; Haghbayan, H.; Gunaratne, K. Social media and vaccine hesitancy: New updates for the era of COVID-19 and globalized infectious diseases. Hum. Vaccines Immunother. 2020, 16, 2586–2593. [Google Scholar] [CrossRef]
- Schernhammer, E.; Weitzer, J.; Laubichler, M.D.; Birmann, B.M.; Bertau, M.; Zenk, L.; Caniglia, G.; Jäger, C.C.; Steiner, G. Correlates of COVID-19 vaccine hesitancy in Austria: Trust and the government. J. Public Health 2021, 5. [Google Scholar] [CrossRef]
- Ali, S.N.; Hanif, W.; Patel, K.; Khunti, K. Ramadan and COVID-19 vaccine hesitancy—A call for action. Lancet 2021, 397, 1443–1444. [Google Scholar] [CrossRef]
- International Association of Dental Students (IADS). Delegates List: Governance. Available online: https://iads-web.org/governance/delegates/ (accessed on 14 March 2021).
- KoBoToolbox. Harvard Humanitarian Initiative. Available online: https://support.kobotoolbox.org/welcome.html (accessed on 15 August 2020).
- International Association of Dental Students (IADS). Workforce: Governance. Available online: https://iads-web.org/governance/workforce/ (accessed on 14 March 2021).
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Br. Med. J. 2007, 335, 806–808. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC). Epi InfoTM for Windows. Available online: https://www.cdc.gov/epiinfo/pc.html (accessed on 25 December 2020).
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Proton Technologies AG. General Data Protection Regulation (GDPR) Compliance Guidelines. HORIZON 2020—Project REP-791727-1. Available online: https://gdpr.eu/ (accessed on 1 May 2021).
- SPSS Inc. IBM SPSS Statistics 27. Available online: https://www.ibm.com/support/pages/node/3006603 (accessed on 14 March 2021).
- World Bank. World Bank Country and Lending Groups. Available online: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed on 14 March 2020).
- World Dental Federation (FDI). Regional Organizations: Our members. Available online: https://www.fdiworlddental.org/regional-organizations (accessed on 15 March 2021).
- Verger, P.; Scronias, D.; Dauby, N.; Adedzi, K.A.; Gobert, C.; Bergeat, M.; Gagneur, A.; Dubé, E. Attitudes of healthcare workers towards COVID-19 vaccination: A survey in France and French-speaking parts of Belgium and Canada, 2020. Eurosurveillance 2021, 26, 2002047. [Google Scholar] [CrossRef]
- Grech, V.; Bonnici, J.; Zammit, D. Vaccine hesitancy in Maltese family physicians and their trainees vis-à-vis influenza and novel COVID-19 vaccination. Early Hum. Dev. 2020, 105259. [Google Scholar] [CrossRef] [PubMed]
- Neumann-Böhme, S.; Varghese, N.E.; Sabat, I.; Barros, P.P.; Brouwer, W.; Van Exel, J.; Schreyögg, J.; Stargardt, T. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur. J. Health Econ. 2020, 21, 977–982. [Google Scholar] [CrossRef]
- Saied, S.M.; Saied, E.M.; Kabbash, I.A.; Abdo, S.A.E. Vaccine hesitancy: Beliefs and barriers associated with COVID-19 vaccination among Egyptian medical students. J. Med. Virol. 2021. [Google Scholar] [CrossRef]
- Grech, V.; Gauci, C. Vaccine hesitancy in the University of Malta Faculties of Health Sciences, Dentistry and Medicine vis-à-vis influenza and novel COVID-19 vaccination. Early Hum. Dev. 2020, 105258. [Google Scholar] [CrossRef] [PubMed]
- Synnott, K. College Students’ COVID-19 Vaccine Hesitancy. SSRN 2020. [Google Scholar] [CrossRef]
- Jain, J.; Saurabh, S.; Goel, A.D.; Gupta, K.; Bhardwaj, P.; Raghav, P.R. COVID-19 vaccine hesitancy among undergraduate medical students: Results 2 from a nationwide survey in India. medRxiv 2021. [Google Scholar] [CrossRef]
- Sallam, M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef] [PubMed]
- Barello, S.; Nania, T.; Dellafiore, F.; Graffigna, G.; Caruso, R. ‘Vaccine hesitancy’ among university students in Italy during the COVID-19 pandemic. Eur. J. Epidemiol. 2020, 35, 781–783. [Google Scholar] [CrossRef] [PubMed]
- Szmyd, B.; Bartoszek, A.; Karuga, F.; Staniecka, K.; Błaszczyk, M.; Radek, M. Medical Students and SARS-CoV-2 Vaccination: Attitude and Behaviors. Vaccines 2021, 9, 128. [Google Scholar] [CrossRef]
- Council of European Dentists (CED). The EU Manual of Dental Practice 2014. Available online: https://cedentists.eu/library/eu-manual.html (accessed on 20 April 2021).
- American Dental Association (ADA). Dental Schools and Students. ADA Health Policy Institute FAQ. Available online: https://www.ada.org/en/science-research/health-policy-institute/dental-statistics/education (accessed on 20 April 2021).
- American Dental Association (ADA). Dental Workforce in the U.S. ADA Health Policy Institute FAQ. Available online: https://www.ada.org/en/science-research/health-policy-institute/dental-statistics/workforce (accessed on 20 April 2021).
- Prasanna, J.S.; Karunakar, P.; Sumadhura, C.; Aishwarya, M.D.; Monica, P.; Sayed, A.S. Women dentists: Changing the face of dentistry. J. Oral Res. Rev. 2015, 7, 69. [Google Scholar] [CrossRef]
- Shrirao, N. The Journey of Women in Dentistry. Dental Reach. Available online: https://dentalreach.today/editorial/the-journey-of-women-in-dentistry/ (accessed on 20 April 2021).
- Parkash, H.; Mathur, V.; Duggal, R.; Jhuraney, B. Dental Workforce Issues: A Global Concern. J. Dent. Educ. 2006, 70, 22–26. [Google Scholar] [CrossRef]
- Dror, A.A.; Eisenbach, N.; Taiber, S.; Morozov, N.G.; Mizrachi, M.; Zigron, A.; Srouji, S.; Sela, E. Vaccine hesitancy: The next challenge in the fight against COVID-19. Eur. J. Epidemiol. 2020, 35, 775–779. [Google Scholar] [CrossRef]
- Murphy, J.; Vallières, F.; Bentall, R.P.; Shevlin, M.; McBride, O.; Hartman, T.K.; McKay, R.; Bennett, K.; Mason, L.; Gibson-Miller, J.; et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat. Commun. 2021, 12, 1–15. [Google Scholar] [CrossRef]
- Soares, P.; Rocha, J.; Moniz, M.; Gama, A.; Laires, P.; Pedro, A.; Dias, S.; Leite, A.; Nunes, C. Factors Associated with COVID-19 Vaccine Hesitancy. Vaccines 2021, 9, 300. [Google Scholar] [CrossRef]
- Olomofe, C.O.; Soyemi, V.K.; Udomah, B.F.; Owolabi, A.O.; Ajumuka, E.E.; Igbokwe, C.M.; Ashaolu, U.O.; Adeyemi, A.O.; Aremu-Kasumu, Y.B.; Dada, O.F.; et al. Predictors of uptake of a potential COVID-19 vaccine among nigerian adults. medRxiv 2021. [Google Scholar] [CrossRef]
- Mahmud, S.; Mohsin, M.; Khan, I.A.; Mian, A.U.; Zaman, M.A. Acceptance of COVID-19 Vaccine and Its Determinants in Bangladesh. arXiv 2021, arXiv:2103.15206. [Google Scholar]
- Dereje, N.; Tesfaye, A.; Tamene, B.; Alemeshet, D.; Abe, H.; Tesfa, N.; Gedion, S.; Biruk, T.; Lakew, Y. COVID-19 Vaccine hesitancy in Addis Ababa, Ethiopia: A mixed-methods study. medRxiv 2021. [Google Scholar] [CrossRef]
- Lucia, V.C.; Kelekar, A.; Afonso, N.M. COVID-19 vaccine hesitancy among medical students. J. Public Health 2020, 2020, 1–5. [Google Scholar] [CrossRef]
- Kelekar, A.K.; Lucia, V.C.; Afonso, N.M.; Mascarenhas, A.K. COVID-19 vaccine acceptance and hesitancy among dental and medical students. J. Am. Dent. Assoc. 2021. [Google Scholar] [CrossRef] [PubMed]
- Abalkhail, M.S.; Alzahrany, M.S.; Alghamdi, K.A.; Alsoliman, M.A.; Alzahrani, M.A.; Almosned, B.S.; Gosadi, I.M.; Tharkar, S. Uptake of influenza vaccination, awareness and its associated barriers among medical students of a University Hospital in Central Saudi Arabia. J. Infect. Public Health 2017, 10, 644–648. [Google Scholar] [CrossRef]
- Pandey, D.; Vanya, V.; Bhagat, S.; Vs, B.; Shetty, J. Awareness and Attitude towards Human Papillomavirus (HPV) Vaccine among Medical Students in a Premier Medical School in India. PLoS ONE 2012, 7, e40619. [Google Scholar] [CrossRef] [PubMed]
- De Paula, S.I.; De Paula, G.I.; Cunegundes, K.S.A.; De Moraes-Pinto, M.I. Adherence to influenza vaccination among medical students during and after influenza a (H1N1) pandemic. Rev. Inst. Med. Trop. Sao Paulo 2016, 58, 82. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wicker, S.; Rabenau, H.F.; Von Gierke, L.; Francois, G.; Hambach, R.; De Schryver, A. Hepatitis B and influenza vaccines: Important occupational vaccines differently perceived among medical students. Vaccine 2013, 31, 5111–5117. [Google Scholar] [CrossRef]
- Li, H.O.-Y.; Bailey, A.; Huynh, D.; Chan, J. YouTube as a source of information on COVID-19: A pandemic of misinformation? BMJ Glob. Health 2020, 5, e002604. [Google Scholar] [CrossRef] [PubMed]
- Bonnevie, E.; Gallegos-Jeffrey, A.; Goldbarg, J.; Byrd, B.; Smyser, J. Quantifying the rise of vaccine opposition on Twitter during the COVID-19 pandemic. J. Commun. Health 2021, 14, 12–19. [Google Scholar] [CrossRef]
- Griffith, J.; Marani, H.; Monkman, H. COVID-19 Vaccine Hesitancy in Canada: Content Analysis of Tweets Using the Theoretical Domains Framework. J. Med. Internet Res. 2021, 23, e26874. [Google Scholar] [CrossRef] [PubMed]
- Mesch, G.S.; Schwirian, K.P. Social and political determinants of vaccine hesitancy: Lessons learned from the H1N1 pandemic of 2009-2010. Am. J. Infect. Control. 2015, 43, 1161–1165. [Google Scholar] [CrossRef] [PubMed]
- Crescitelli, M.E.D.; Ghirotto, L.; Sisson, H.; Sarli, L.; Artioli, G.; Bassi, M.; Appicciutoli, G.; Hayter, M. A meta-synthesis study of the key elements involved in childhood vaccine hesitancy. Public Health 2020, 180, 38–45. [Google Scholar] [CrossRef]
- Alawia, R.; Riad, A.; Kateeb, E. Risk perception and readiness of dental students to treat patients amid COVID-19: Implication for dental education. Oral Dis. 2020. [Google Scholar] [CrossRef]
- Alawia, R.; Riad, A.; Kateeb, E. Knowledge and attitudes among dental students about COVID-19 and its precautionary measures: A cross-sectional study. J. Oral Med. Oral Surg. 2021, 27, 17. [Google Scholar] [CrossRef]
- Machado, R.A.; Bonan, P.R.F.; Perez, D.E.D.C.; Júnior, H.M. COVID-19 pandemic and the impact on dental education: Discussing current and future perspectives. Braz. Oral Res. 2020, 34, e083. [Google Scholar] [CrossRef]
- Ghai, S. Are dental schools adequately preparing dental students to face outbreaks of infectious diseases such as COVID-19? J. Dent. Educ. 2020, 84, 631–633. [Google Scholar] [CrossRef] [PubMed]
- Meyer, M.N.; Gjorgjieva, T.; Rosica, D. Trends in Health Care Worker Intentions to Receive a COVID-19 Vaccine and Reasons for Hesitancy. JAMA Netw. Open 2021, 4, e215344. [Google Scholar] [CrossRef]
- Roser, M.; Ritchie, H.; Ortiz-Ospina, E.; Hasell, J. Coronavirus Pandemic (COVID-19). Available online: https://ourworldindata.org/coronavirus (accessed on 18 April 2020).
| Participant | κ Coefficient | Participant | κ Coefficient |
|---|---|---|---|
| No. 1 | 0.8 | No. 10 | 0.6 |
| No. 2 | 0.8 | No. 11 | 1.0 |
| No. 3 | 0.9 | No. 12 | 0.7 |
| No. 4 | 1.0 | No. 13 | 1.0 |
| No. 5 | 1.0 | No. 14 | 0.8 |
| No. 6 | 0.6 | No. 15 | 0.7 |
| No. 7 | 0.6 | No. 16 | 1.0 |
| No. 8 | 1.0 | No. 17 | 0.8 |
| No. 9 | 0.6 | No. 18 | 0.8 |
| Variable | Outcome | Frequency | Percentage | Cumulative Percentage |
|---|---|---|---|---|
| Gender | Female | 4682 | 70.5% | 70.5% |
| Male | 1836 | 27.7% | 98.2% | |
| Non-binary | 53 | 0.8% | 99% | |
| Prefer not to say | 68 | 1% | 100% | |
| Age | 17–22 years | 4218 | 63.5% | 63.5% |
| 23–40 years | 2421 | 36.5% | 100% | |
| Academic Level | 1st Year | 979 | 14.7% | 14.7% |
| 2nd Year | 1227 | 18.5% | 33.2% | |
| 3rd Year | 1422 | 21.4% | 54.6% | |
| 4th Year | 1259 | 19% | 73.6% | |
| 5th Year | 817 | 12.3% | 85.9% | |
| 6th Year | 240 | 3.6% | 89.5% | |
| Internship | 322 | 4.9% | 94.4% | |
| Fresh Graduate | 373 | 5.6% | 100% | |
| Country | Albania | 57 | 0.9% | 0.9% |
| Canada | 183 | 2.8% | 3.6% | |
| Croatia | 169 | 2.5% | 6.2% | |
| Ecuador | 381 | 5.7% | 11.9% | |
| Estonia | 78 | 1.2% | 13.1% | |
| Indonesia | 416 | 6.3% | 19.3% | |
| Iran | 388 | 5.8% | 25.2% | |
| Iraq | 354 | 5.3% | 30.5% | |
| Italy | 492 | 7.4% | 37.9% | |
| Latvia | 129 | 1.9% | 39.9% | |
| Lebanon | 107 | 1.6% | 41.5% | |
| Lithuania | 291 | 4.4% | 45.9% | |
| Malaysia | 350 | 5.3% | 51.1% | |
| Nepal | 153 | 2.3% | 53.4% | |
| Pakistan | 379 | 5.7% | 59.2% | |
| Palestine | 417 | 6.3% | 65.4% | |
| Portugal | 389 | 5.9% | 71.3% | |
| Russia | 596 | 9.0% | 80.3% | |
| Sudan | 467 | 7.0% | 87.3% | |
| Tunisia | 283 | 4.3% | 91.6% | |
| Turkey | 386 | 5.8% | 97.4% | |
| USA | 174 | 2.6% | 100% | |
| Geographic Region | Africa | 750 | 11.3% | 11.3% |
| Americas | 738 | 11.1% | 22.4% | |
| Asia-Pacific | 1298 | 19.6% | 41.9% | |
| Eastern Mediterranean | 1266 | 19.1% | 61% | |
| Europe | 2587 | 39% | 100% | |
| Economic Level | Low-income Economy | 467 | 7% | 7% |
| Lower-middle-income Economy | 1232 | 18.6% | 25.6% | |
| Upper-middle-income Economy | 3035 | 45.7% | 71.3% | |
| High-income Economy | 1905 | 28.7% | 100% |
| Variable | LLMI | UMHI | Total | Sig. 1 |
|---|---|---|---|---|
| I had been infected by SARS-CoV-2 | 332 (19.5%) | 773 (15.6%) | 1105 (16.6%) | <0.01 |
| I had been caring for someone with COVID-19 infection | 538 (31.7%) | 1270 (25.7%) | 1808 (27.2%) | <0.01 |
| I know someone who had COVID-19 infection | 1515 (89.2%) | 4286 (86.8%) | 5801 (87.4%) | 0.01 |
| I know someone who had died from COVID-19 infection | 945 (55.6%) | 2086 (42.2%) | 3031 (45.7%) | <0.01 |
| Variable | Outcome | LLMI | UMHI | Total | Sig. 1 |
|---|---|---|---|---|---|
| I am willing to take the COVID-19 vaccine once it becomes available to me. | Totally Disagree = 1 | 150 (8.8%) | 341 (6.9%) | 491 (7.4%) | 0.01 |
| Disagree = 2 | 126 (7.4%) | 308 (6.2%) | 434 (6.5%) | 0.09 | |
| Not Sure = 3 | 517 (30.4%) | 977 (19.8%) | 1494 (22.5%) | <0.01 | |
| Agree = 4 | 441 (26%) | 1054 (21.3%) | 1495 (22.5%) | <0.01 | |
| Totally Agree = 5 | 465 (27.4%) | 2260 (45.7%) | 2725 (41%) | <0.01 | |
| Total (1–5) | 3.56 ± 1.21 | 3.93 ± 1.23 | 3.83 ± 1.24 | <0.01 |
| Variable | Outcome | LLMI | UMHI | Total | Sig. 1 |
|---|---|---|---|---|---|
| Contextual Drivers | |||||
| Do reports you hear/read in the media/on social media make you re-consider the choice to take the COVID-19 vaccine? | Yes = 2 | 713 (42%) | 1504 (30.4%) | 2217 (33.4%) | |
| Not Sure = 1 | 464 (27.3%) | 1055 (21.4%) | 1519 (22.9%) | ||
| No = 0 | 522 (30.7%) | 2381 (48.2%) | 2903 (43.7%) | ||
| Total (0–2) | 1.11 ± 0.85 | 0.82 ± 0.87 | 0.9 ± 0.87 | <0.01 | |
| Do celebrities, religious or political leaders influence your decision about being vaccinated? | Yes = 2 | 362 (21.3%) | 716 (14.5%) | 1078 (16.2%) | |
| Not Sure = 1 | 227 (13.4%) | 600 (21.1%) | 827 (12.5%) | ||
| No = 0 | 1110 (65.3%) | 3624 (73.4%) | 4734 (71.3%) | ||
| Total (0–2) | 0.56 ± 0.82 | 0.41 ± 0.73 | 0.45 ± 0.76 | <0.01 | |
| Do you trust that your government is making decisions in your best interest with respect to what vaccines are provided (e.g., your government purchases the highest quality vaccines available)? | Yes = 2 | 460 (27.1%) | 1871 (37.9%) | 2331 (35.1%) | |
| Not Sure = 1 | 550 (32.4%) | 1580 (32%) | 2130 (32.1%) | ||
| No = 0 | 689 (40.6%) | 1489 (30.1%) | 2178 (32.8%) | ||
| Total (0–2) | 0.87 ± 0.81 | 1.08 ± 0.82 | 1.02 ± 0.82 | <0.01 | |
| Do you trust pharmaceutical companies to provide credible data on COVID-19 vaccine safety and the effectiveness of the vaccines? | Yes = 2 | 629 (37%) | 2521 (51%) | 3150 (47.4%) | |
| Not Sure = 1 | 579 (34.1%) | 1462 (29.6%) | 2041 (30.7%) | ||
| No = 0 | 491 (28.9%) | 957 (19.4%) | 1448 (21.8%) | ||
| Total (0–2) | 1.08 ± 0.81 | 1.32 ± 0.78 | 1.26 ± 0.79 | <0.01 | |
| Do you know anyone who will not take the vaccine because of religious or cultural values? | Yes = 2 | 289 (17%) | 1234 (25%) | 1523 (22.9%) | |
| Not Sure = 1 | 181 (10.7%) | 649 (13.1%) | 830 (12.5%) | ||
| No = 0 | 1229 (72.3%) | 3057 (61.9%) | 4286 (64.6%) | ||
| Total (0–2) | 0.45 ± 0.77 | 0.63 ± 0.86 | 0.58 ± 0.84 | <0.01 | |
| If “Yes”, do you agree with these people? | Yes = 2 | 52 (18%) | 135 (10.9%) | 187 (12.3%) | |
| Not Sure = 1 | 30 (10.4%) | 162 (13.1%) | 192 (12.6%) | ||
| No = 0 | 207 (71.6%) | 937 (75.9%) | 1144 (75.1%) | ||
| Total (0–2) | 0.46 ± 0.78 | 0.35 ± 0.67 | 0.37 ± 0.69 | <0.01 | |
| Individual/Group Drivers | |||||
| Do you think that there are better ways to prevent COVID-19 than using vaccines (e.g., developing immunity by becoming sick and recovering)? | Yes = 2 | 647 (38.1%) | 1109 (22.4%) | 1756 (26.4%) | |
| Not Sure = 1 | 432 (25.4%) | 1523 (30.8%) | 1955 (29.4%) | ||
| No = 0 | 620 (36.5%) | 2308 (46.7%) | 2928 (44.1%) | ||
| Total (0–2) | 1.02 ± 0.86 | 0.76 ± 0.8 | 0.82 ± 0.82 | <0.01 | |
| Do you feel you have enough information about COVID-19 vaccines and their safety? | Yes = 2 | 458 (27%) | 1633 (33.1%) | 2091 (31.5%) | |
| Not Sure = 1 | 399 (23.5%) | 1439 (29.1%) | 1838 (27.7%) | ||
| No = 0 | 842 (49.6%) | 1868 (37.8%) | 2710 (40.8%) | ||
| Total (0–2) | 0.77 ± 0.85 | 0.95 ± 0.84 | 0.91 ± 0.845 | <0.01 | |
| Vaccine-specific Drivers | |||||
| Do you think that the benefits of COVID-19 vaccines outweigh their reported side effects/ adverse reactions? | Yes = 2 | 683 (40.2%) | 2686 (54.4%) | 3369 (50.7%) | |
| Not Sure = 1 | 661 (38.9%) | 1421 (28.8%) | 2082 (31.4%) | ||
| No = 0 | 355 (20.9%) | 833 (16.9%) | 1188 (17.9%) | ||
| Total (0–2) | 1.19 ± 0.76 | 1.38 ± 0.76 | 1.33 ± 0.76 | <0.01 | |
| In general, when a new vaccine is introduced, are you inclined to consent to your vaccination? | Yes = 2 | 638 (37.6%) | 2233 (45.2%) | 2871 (43.2%) | |
| Not Sure = 1 | 556 (32.7%) | 1606 (32.5%) | 2162 (32.6%) | ||
| No = 0 | 505 (29.7%) | 1101 (22.3%) | 1606 (24.2%) | ||
| Total (0–2) | 1.08 ± 0.82 | 1.23 ± 0.79 | 1.19 ± 0.8 | <0.01 | |
| Do you feel confident that the health centre or doctor’s office will have the COVID-19 vaccines you need, when you need them? | Yes = 2 | 571 (33.6%) | 2132 (43.2%) | 2703 (40.7%) | |
| Not Sure = 1 | 617 (36.3%) | 1541 (31.2%) | 2158 (32.5%) | ||
| No = 0 | 511 (30.1%) | 1267 (25.6%) | 1778 (26.8%) | ||
| Total (0–2) | 1.04 ± 0.8 | 1.18 ± 0.81 | 1.14 ± 0.81 | <0.01 | |
| Variable | Outcome | Acceptance Level | Sig. 1 |
|---|---|---|---|
| Gender | Female | 3.83 ± 1.23 | 0.01 |
| Male | 3.87 ± 1.26 | ||
| Non-binary | 3.47 ± 1.42 | ||
| Prefer not to say | 3.44 ± 1.43 | ||
| Academic Level | 1st Year | 3.73 ± 1.28 | 0.11 |
| 2nd Year | 3.81 ± 1.19 | ||
| 3rd Year | 3.91 ± 1.19 | ||
| 4th Year | 3.90 ± 1.25 | ||
| 5th Year | 3.93 ± 1.25 | ||
| 6th Year | 3.80 ± 1.31 | ||
| Internship | 3.59 ± 1.26 | ||
| Fresh Graduate | 3.66 ± 1.26 | ||
| Clinical Training | Preclinical (1st year and 2nd year) | 3.77 ± 1.32 | 0.01 |
| Clinical (3rd year–Graduate) | 3.86 ± 1.24 | ||
| Country | Albania | 3.14 ± 1.27 | <0.01 |
| Canada | 4.41 ± 1 | ||
| Croatia | 3.73 ± 1.26 | ||
| Ecuador | 3.86 ± 1.19 | ||
| Estonia | 3.62 ± 1.22 | ||
| Indonesia | 4.37 ± 0.89 | ||
| Iran | 3.38 ± 1.38 | ||
| Iraq | 3.27 ± 1.17 | ||
| Italy | 4.7 ± 0.8 | ||
| Latvia | 3.8 ± 1.37 | ||
| Lebanon | 3.86 ± 1.18 | ||
| Lithuania | 4.18 ± 1.12 | ||
| Malaysia | 4.33 ± 0.91 | ||
| Nepal | 3.91 ± 1.04 | ||
| Pakistan | 3.97 ± 1.01 | ||
| Palestine | 3.72 ± 1.27 | ||
| Portugal | 4.57 ± 0.85 | ||
| Russia | 2.85 ±1.12 | ||
| Sudan | 3.37 ± 1.17 | ||
| Tunisia | 2.88 ± 1.2 | ||
| Turkey | 3.99 ± 1.11 | ||
| USA | 4.53 ± 1.04 | ||
| Geographic Region | Africa | 3.18 ± 1.2 | <0.01 |
| Americas | 4.15 ± 1.15 | ||
| Asia-Pacific | 4.19 ± 1 | ||
| Eastern Mediterranean | 3.5 ± 1.29 | ||
| Europe | 3.91 ± 1.26 | ||
| Economic Level | Low-income Economy | 3.37 ± 1.17 | <0.01 |
| Lower-middle-income Economy | 3.63 ± 1.23 | ||
| Upper-middle-income Economy | 3.66 ± 1.25 | ||
| High-income Economy | 4.36 ± 1.07 |
| Variable | No | Yes | Sig. 1 |
|---|---|---|---|
| I had been infected by SARS-CoV-2 | 3.88 ± 1.21 | 3.57 ± 1.36 | <0.01 |
| I had been caring for someone with COVID-19 infection | 3.89 ± 1.21 | 3.68 ± 1.31 | <0.01 |
| I know someone who had COVID-19 infection | 3.68 ± 1.25 | 3.86 ±1.24 | <0.01 |
| I know someone who had died from COVID-19 infection | 3.89 ± 1.22 | 3.77 ± 1.26 | <0.01 |
| Category | Driver | No | Yes | Sig. 1 |
|---|---|---|---|---|
| Contextual | Media | 3.99 ± 1.31 | 3.71 ± 1.21 | <0.01 |
| Public Figures | 3.87 ± 1.25 | 3.82 ± 1.27 | 0.24 | |
| Government | 3.37 ± 1.30 | 4.29 ± 1.10 | <0.01 | |
| Pharmaceuticals | 3.06 ± 1.30 | 4.31 ± 1.06 | <0.01 | |
| Values | 4.30 ± 1.05 | 2.75 ± 1.44 | <0.01 | |
| Individual/Group | Natural Immunity | 4.16 ± 1.11 | 3.35 ± 1.38 | <0.01 |
| Sufficient Knowledge | 3.48 ± 1.19 | 4.21 ± 1.23 | <0.01 | |
| Vaccine-specific | Risk/Benefit Ratio | 3.14 ± 1.37 | 4.31 ± 1.06 | <0.01 |
| New Vaccine | 3.06 ± 1.28 | 4.37 ± 1.03 | <0.01 | |
| Availability | 3.44 ± 1.3 | 4.17 ± 1.15 | <0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Riad, A.; Abdulqader, H.; Morgado, M.; Domnori, S.; Koščík, M.; Mendes, J.J.; Klugar, M.; Kateeb, E.; on behalf of IADS-SCORE. Global Prevalence and Drivers of Dental Students’ COVID-19 Vaccine Hesitancy. Vaccines 2021, 9, 566. https://doi.org/10.3390/vaccines9060566
Riad A, Abdulqader H, Morgado M, Domnori S, Koščík M, Mendes JJ, Klugar M, Kateeb E, on behalf of IADS-SCORE. Global Prevalence and Drivers of Dental Students’ COVID-19 Vaccine Hesitancy. Vaccines. 2021; 9(6):566. https://doi.org/10.3390/vaccines9060566
Chicago/Turabian StyleRiad, Abanoub, Huthaifa Abdulqader, Mariana Morgado, Silvi Domnori, Michal Koščík, José João Mendes, Miloslav Klugar, Elham Kateeb, and on behalf of IADS-SCORE. 2021. "Global Prevalence and Drivers of Dental Students’ COVID-19 Vaccine Hesitancy" Vaccines 9, no. 6: 566. https://doi.org/10.3390/vaccines9060566
APA StyleRiad, A., Abdulqader, H., Morgado, M., Domnori, S., Koščík, M., Mendes, J. J., Klugar, M., Kateeb, E., & on behalf of IADS-SCORE. (2021). Global Prevalence and Drivers of Dental Students’ COVID-19 Vaccine Hesitancy. Vaccines, 9(6), 566. https://doi.org/10.3390/vaccines9060566












