Disparity of Cervical Cancer Risk in Young Japanese Women: Bipolarized Status of HPV Vaccination and Cancer Screening
Abstract
1. Introduction
2. Methods
2.1. Survey of Cervical Cancer Screening Rates in HPV-Vaccinated and Unvaccinated Women
2.2. Interview Survey of the Vaccinated and the Unvaccinated Women
2.3. Internet Survey of Vaccinated and Unvaccinated Women Aged 20 or 21
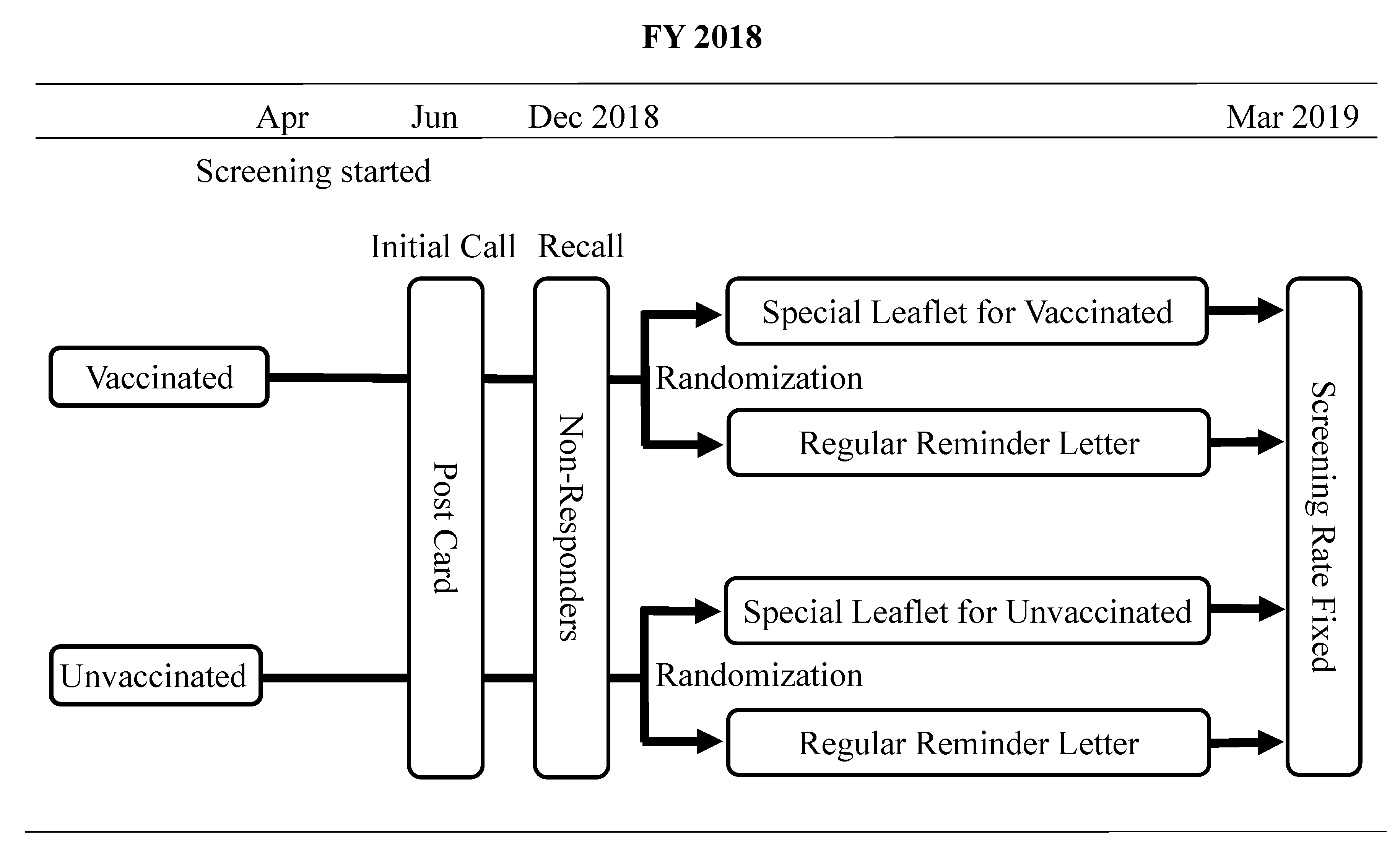
2.4. A Prospective Comparison of Different Recommendation tools for Screening According to the Respondent’s HPV Vaccination Status
2.5. Statistical Analysis
2.6. Informed Consent and Ethical Approval
3. Results
3.1. Cervical Cancer Screening Rates in Vaccinated and Unvaccinated Women at Age 20–21
3.2. Interview Survey for Preparation of Recommendation Message
3.3. Internet Survey for Preparation of Information Tools
3.4. Information Leaflets for Cervical Cancer Screening Tailored for Vaccination Status
3.5. A Randomized Comparison of Different Recommendation Tools for Screening Tailored for Different HPV Vaccination Status
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- U.S. Cancer Statistics Working Group. United States Cancer Statistics: 1999–2014 Incidence and Mortality Web-Based Report; U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, and National Cancer Institute: Atlanta, GA, USA. Available online: https://www.cdc.gov/cancer/uscs/ (accessed on 5 April 2020).
- Luostarinen, T.; Apter, D.; Dillner, J.; Eriksson, T.; Harjula, K.; Natunen, K.; Paavonen, J.; Pukkala, E.; Lehtinen, M. Vaccination protects against invasive HPV-associated cancers. Int. J. Cancer 2018, 142, 2186–2187. [Google Scholar] [CrossRef] [PubMed]
- Lei, J.; Ploner, A.; Elfstrom, M.; Wang, J.; Roth, A.; Fang, F.; Sundstrom, K.; Dillner, J.; Sparen, P. HPV vaccination and the risk of invasive cervical cancer. N. Engl. J. Med. 2020, 383, 1340–1348. [Google Scholar] [CrossRef] [PubMed]
- Hall, M.T.; Simms, K.T.; Lew, J.B.; Smith, M.A.; Brotherton, J.M.; Saville, M.; Frazer, I.H.; Canfell, K. The projected timeframe until cervical cancer elimination in Australia: A modelling study. Lancet Public Health 2019, 4, e19–e27. [Google Scholar] [CrossRef]
- The Ministry of Health, Labor and Welfare, Japan. Comprehensive Survey of Living Conditions. Available online: https://www.mhlw.go.jp/toukei/saikin/hw/k-tyosa/k-tyosa18/index.html (accessed on 5 April 2020).
- Garland, S.M.; Brown, D.R. Potential of the quadrivalent human papillomavirus vaccine in the prevention and treatment of cervical cancer. Expert Opin. Biol. Ther. 2014, 14, 527–534. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, J.; Kamiura, S.; Okayama, K.; Okodo, M.; Shibata, T.; Osaka, Y.; Fujita, S.; Takata, E.; Takagi, H.; Takakura, M.; et al. Single type infection of human papillomavirus as a cause for high-grade cervical intraepithelial neoplasia and invasive cancer in Japan. Papillomavirus Res. 2018, 6, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Ueda, Y.; Enomoto, T.; Sekine, M.; Takata, T.; Morimoto, A. Japan’s failure to vaccinate girls against human papillomavirus. Am. J. Obstet. Gynecol. 2015, 212, 405–406. [Google Scholar] [CrossRef] [PubMed]
- Hanley, S.J.; Yoshioka, E.; Ito, Y.; Kishi, R. HPV vaccination crisis in Japan. Lancet 2015, 385, 2571. [Google Scholar] [CrossRef]
- Sekine, M.; Kudo, R.; Adachi, S.; Yamaguchi, M.; Ueda, Y.; Takata, T.; Morimoto, A.; Tanaka, Y.; Yagi, A.; Miyagi, E.; et al. Japan’s Ongoing crisis HPV vaccination. Int. J. Pathol. Clin. Res. 2016, 2, 39. [Google Scholar] [CrossRef]
- Ikeda, S.; Ueda, Y.; Yagi, A.; Matsuzaki, S.; Kobayashi, E.; Kimura, T.; Miyagi, E.; Sekine, M.; Enomoto, T.; Kudoh, K.; et al. HPV vaccination in Japan: What is happening in Japan? Expert Rev. Vaccines 2019, 18, 323–325. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa, S.; Ueda, Y.; Yagi, A.; Ikeda, S.; Hiramatsu, K.; Kimura, T. Corrected human papillomavirus vaccination rates for each birth fiscal year in Japan. Cancer Sci. 2020, 111, 2156–2162. [Google Scholar] [CrossRef] [PubMed]
- Yagi, A.; Ueda, Y.; Kakuda, M.; Tanaka, Y.; Ikeda, S.; Matsuzaki, S.; Kobayashi, E.; Morishima, T.; Miyashiro, I.; Fukui, K.; et al. Epidemiologic and clinical analysis of cervical cancer using data from the population-based Osaka Cancer Registry. Cancer Res. 2019, 79, 1252–1259. [Google Scholar] [CrossRef] [PubMed]
- Guo, F.; Hirth, J.M.; Berenson, A.B. Human papillomavirus vaccination and Pap smear uptake among young women in the United States: Role of provider and patient. J. Women’s Health 2017, 26, 1114–1122. [Google Scholar] [CrossRef] [PubMed]
- Taniguchi, M.; Ueda, Y.; Yagi, A.; Ikeda, S.; Endo, M.; Tomimatsu, T.; Nakayama, T.; Sekine, M.; Enomoto, T.; Kimura, T. Cervical cancer screening rate differs by HPV vaccination status: An interim analysis. Vaccine 2019, 37, 4424–4426. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, M.; Sekine, M.; Kudo, R.; Adachi, S.; Ueda, Y.; Miyagi, E.; Hara, M.; Hanley, S.J.B.; Enomoto, E. Differential misclassification between self-reported status and official HPV vaccination records in Japan: Implications for evaluating vaccine safety and effectiveness. Papillomavirus Res. 2018, 6, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, Y.; Ueda, Y.; Egawa-Takata, T.; Yagi, A.; Yoshino, K.; Kimura, T. Outcomes for girls without HPV vaccination in Japan. Lancet Oncol. 2016, 17, 868–869. [Google Scholar] [CrossRef]
- Yagi, A.; Ueda, Y.; Nakagawa, S.; Ikeda, S.; Tanaka, Y.; Sekine, M.; Miyagi, E.; Enomoto, T.; Kimura, T. Potential for cervical cancer incidence and death resulting from Japan’s current policy of prolonged suspension of its governmental recommendation of the HPV vaccine. Sci. Rep. 2020, 10, 15945. [Google Scholar] [CrossRef] [PubMed]
- The OECD Health Care Quality Indicators Project: Cancer Care, Screening Survival and Mortality for Cervical Cancer, Cervical Cancer Screening, Percentage of Women Aged 20–69 Screened. Available online: http://www.oecd.org/health/health-systems/healthcarequalityindicators.htm (accessed on 10 February 2021).
- Ministry of Health, Labor and Welfare, Japan. Available online: http://www.mhlw.go.jp/toukei/saikin/hw/k-tyosa/k-tyosa10/toukei.html (accessed on 10 February 2021).
| City | Vaccinated | Unvaccinated | p-Value |
|---|---|---|---|
| Toyonaka | 64/2010 (3.2%) | 19/1037 (1.8%) | 0.034 |
| Iwaki | 166/1687 (9.8%) | 40/853 (4.7%) | <0.01 |
| Total | 230/3697 (6.2%) | 59/1890 (3.1%) | <0.01 |
| Characteristics | Vaccinated | Unvaccinated | p-Value |
|---|---|---|---|
| (n = 206) | (n = 206) | ||
| Marriage Status | 0.72 | ||
| Married | 19 (9.2%) | 16 (7.8%) | |
| Unmarried | 187 (90.8%) | 190 (92.2%) | |
| Childbearing | 1 | ||
| Yes | 17 (8.3%) | 16 (7.8%) | |
| No | 189 (91.7%) | 190 (92.2%) | |
| Housemate | 0.18 | ||
| Yes | 143 (69.4%) | 156 75.7%) | |
| No | 63 (30.6%) | 50 (24.3%) | |
| Jobs | <0.001 | ||
| Employed | 22 (10.7%) | 52 (25.2%) | |
| Housewives | 184 (89.3%) | 154 (74.8%) | |
| (including students) | |||
| Sexual Experience * | 0.46 | ||
| Yes | 105 (55.3%) | 107 (59.1%) | |
| No | 85 (44.7%) | 74 (40.9%) | |
| Smoking | 0.53 | ||
| Currently smokes | 7(3.4%) | 12 (5.8%) | |
| Has smoked | 26 (12.6%) | 25 (12.1%) | |
| Never smoked | 173 (84.0%) | 168 (81.6%) | |
| Knowledge about cervical cancer | |||
| Cause of cervical cancer is predominantly HPV | 0.46 | ||
| Yes | 69 (33.5%) | 61 (29.6%) | |
| No | 137 (66.5%) | 145 (70.4%) | |
| HPV is transmitted by sexual intercourse | 1 | ||
| Yes | 60 (29.1%) | 59 (28.6%) | |
| No | 146 (70.9%) | 147 (71.4%) | |
| Cervical cancer has been increasing in younger generations | 0.072 | ||
| Yes | 130 (63.1%) | 111 (53.9%) | |
| No | 76 (36.9%) | 95 (46.1%) | |
| Cervical cancer treatment possibly affects fertility | 0.16 | ||
| Yes | 164 (79.6%) | 151 (73.3%) | |
| No | 42 (20.4%) | 55 (26.7%) | |
| Cervical cancer may result in death | 0.027 | ||
| Yes | 136 (66.0%) | 113 (54.9%) | |
| No | 70 (34.0%) | 93 (45.1%) | |
| Health consciousness and behavior | |||
| Intension to receive cervical cancer screening | 0.0064 | ||
| 138 (67.0%) | 110 (53.4%) | ||
| Gynecology consultation history * | 0.27 | ||
| Yes | 91 (45.3%) | 79 (39.7%) | |
| No | 110 (54.7%) | 120 (60.3%) | |
| Have talked about cervical cancer with a family member | 0.33 | ||
| Yes | 87 (42.2%) | 74 (35.9%) | |
| No | 98 (47.6%) | 104 (50.5%) | |
| Not remember | 21 (10.2%) | 28 (13.6%) | |
| Recommended cervical cancer screening by a family member | 0.3 | ||
| Yes | 51 (24.8%) | 48 (23.3%) | |
| No | 142 (68.9%) | 136 (66.0%) | |
| Don’t remember | 13 (6.3%) | 22 (10.7%) | |
| Family members receive cancer screenings | 0.16 | ||
| Regularly | 27 (13.1%) | 16 (7.8%) | |
| Irregularly | 34 (16.5%) | 42 (20.4%) | |
| Never/don’t know | 145 (70.4%) | 148 (71.8%) |
| (A) Change of intention for receiving cervical cancer screening after reading the message | |||
| Change of intention for receiving screening | |||
| Enhanced | Unchanged or decreased | p-value | |
| Vaccinated (n = 206) | 120 (58.3%) | 86 (41.7%) | 0.075 |
| Unvaccinated (n = 206) | 101 (49.0%) | 105 (51.0%) | |
| (B) Intention to receive cervical cancer screening within two years—before and after reading the message | |||
| Intention to receive cervical cancer screening within two years | |||
| Before | After | p-value | |
| Vaccinated (n = 206) | 43 (20.9%) | 71 (34.5%) | 0.0029 |
| Unvaccinated (n = 206) | 39 (18.9%) | 66 (32.0%) | 0.0032 |
| Vaccinated | Unvaccinated |
|---|---|
| 1. I found out that cervical cancer screening is free. | 1. I found out that cervical cancer screening is free. |
| 110/120 (91.7%) | 88/101 (87.1%) |
| 2. I found out that I could have cervical cancer myself. | 2. I found out how scary cervical cancer is. |
| 108/120 (90.0%) | 87/101 (86.1%) |
| 3. I found out that cervical cancer screening is recommended for ages 20 and up. | 3. I found out that cervical cancer screening is recommended for ages 20 and up. |
| 105/120 (87.5%) | 85/101 (84.2%) |
| 4. I found out that it’s better to receive cervical cancer screening, even though I’ve been vaccinated. | 4. I found out that I could have cervical cancer myself. |
| 105/120 (87.5%) | 81/101 (80.2%) |
| 5. I found out that more people die of cervical cancer than I thought. | 5. I found out what kind of examination the cervical cancer screening is. |
| 103/120 (85.8%) | 78/101 (77.2%) |
| 6. I found out how scary cervical cancer is. | 6. I found out that more people die of cervical cancer than I thought. |
| 102/120 (85.0%) | 77/101 (76.2%) |
| City | Regular Reminder Letter | Special Leaflet | p-Value |
|---|---|---|---|
| Vaccinated | 44/687 (6.4%) | 51/688 (7.4%) | 0.52 |
| Unvaccinated | 13/334 (3.9%) | 17/332 (5.1%) | 0.46 |
| Total | 57/1021 (5.6%) | 68/1020 (6.7%) | 0.31 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Taniguchi, M.; Ueda, Y.; Yagi, A.; Miyoshi, A.; Tanaka, Y.; Minekawa, R.; Endo, M.; Tomimatsu, T.; Hirai, K.; Nakayama, T.; et al. Disparity of Cervical Cancer Risk in Young Japanese Women: Bipolarized Status of HPV Vaccination and Cancer Screening. Vaccines 2021, 9, 280. https://doi.org/10.3390/vaccines9030280
Taniguchi M, Ueda Y, Yagi A, Miyoshi A, Tanaka Y, Minekawa R, Endo M, Tomimatsu T, Hirai K, Nakayama T, et al. Disparity of Cervical Cancer Risk in Young Japanese Women: Bipolarized Status of HPV Vaccination and Cancer Screening. Vaccines. 2021; 9(3):280. https://doi.org/10.3390/vaccines9030280
Chicago/Turabian StyleTaniguchi, Mariko, Yutaka Ueda, Asami Yagi, Ai Miyoshi, Yusuke Tanaka, Ryoko Minekawa, Masayuki Endo, Takuji Tomimatsu, Kei Hirai, Tomio Nakayama, and et al. 2021. "Disparity of Cervical Cancer Risk in Young Japanese Women: Bipolarized Status of HPV Vaccination and Cancer Screening" Vaccines 9, no. 3: 280. https://doi.org/10.3390/vaccines9030280
APA StyleTaniguchi, M., Ueda, Y., Yagi, A., Miyoshi, A., Tanaka, Y., Minekawa, R., Endo, M., Tomimatsu, T., Hirai, K., Nakayama, T., & Kimura, T. (2021). Disparity of Cervical Cancer Risk in Young Japanese Women: Bipolarized Status of HPV Vaccination and Cancer Screening. Vaccines, 9(3), 280. https://doi.org/10.3390/vaccines9030280







