Has Clinical and Epidemiological Varicella Burden Changed over Time in Children? Overview on Hospitalizations, Comorbidities and Costs from 2010 to 2017 in Italy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population and Study Period
2.3. Data Sources
2.3.1. Hospital Discharge Records
2.3.2. Chronic Condition Data Warehouse (CCDWH)
2.3.3. Varicella Vaccination Offer
2.4. Direct Costs
2.5. Statistical Analysis
3. Results
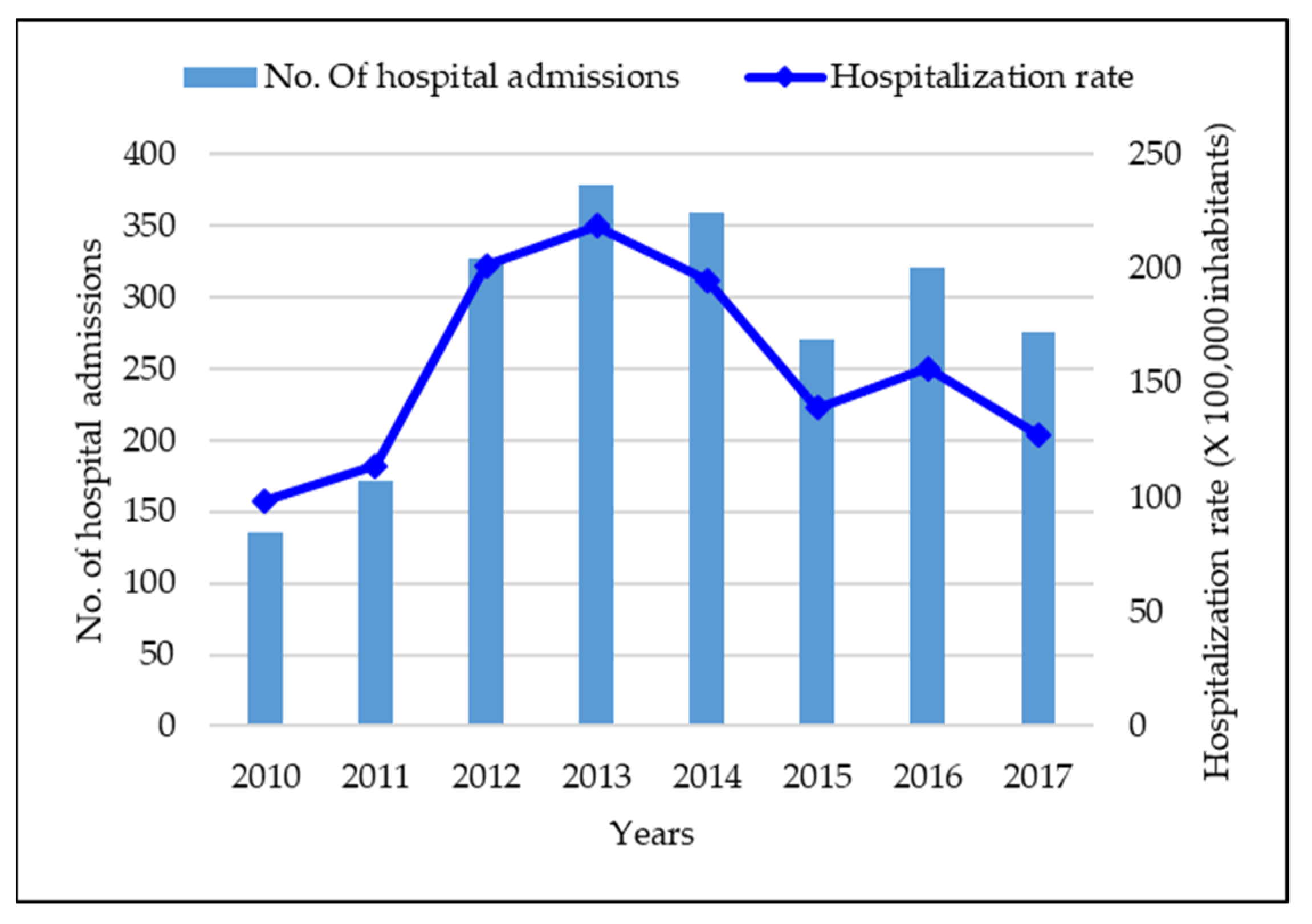
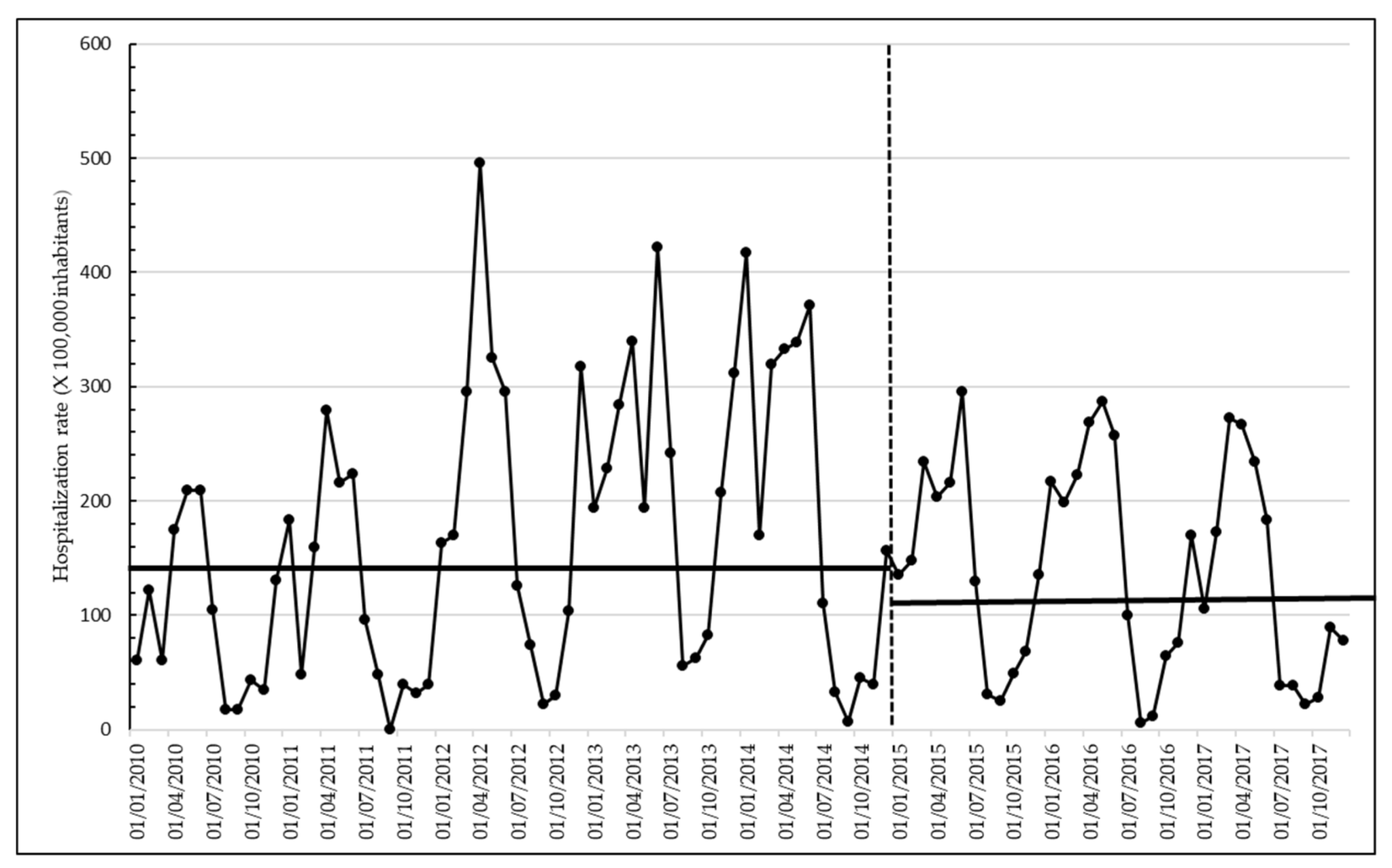
3.1. Epidemiological and Clinical Burden
3.2. Economic Burden
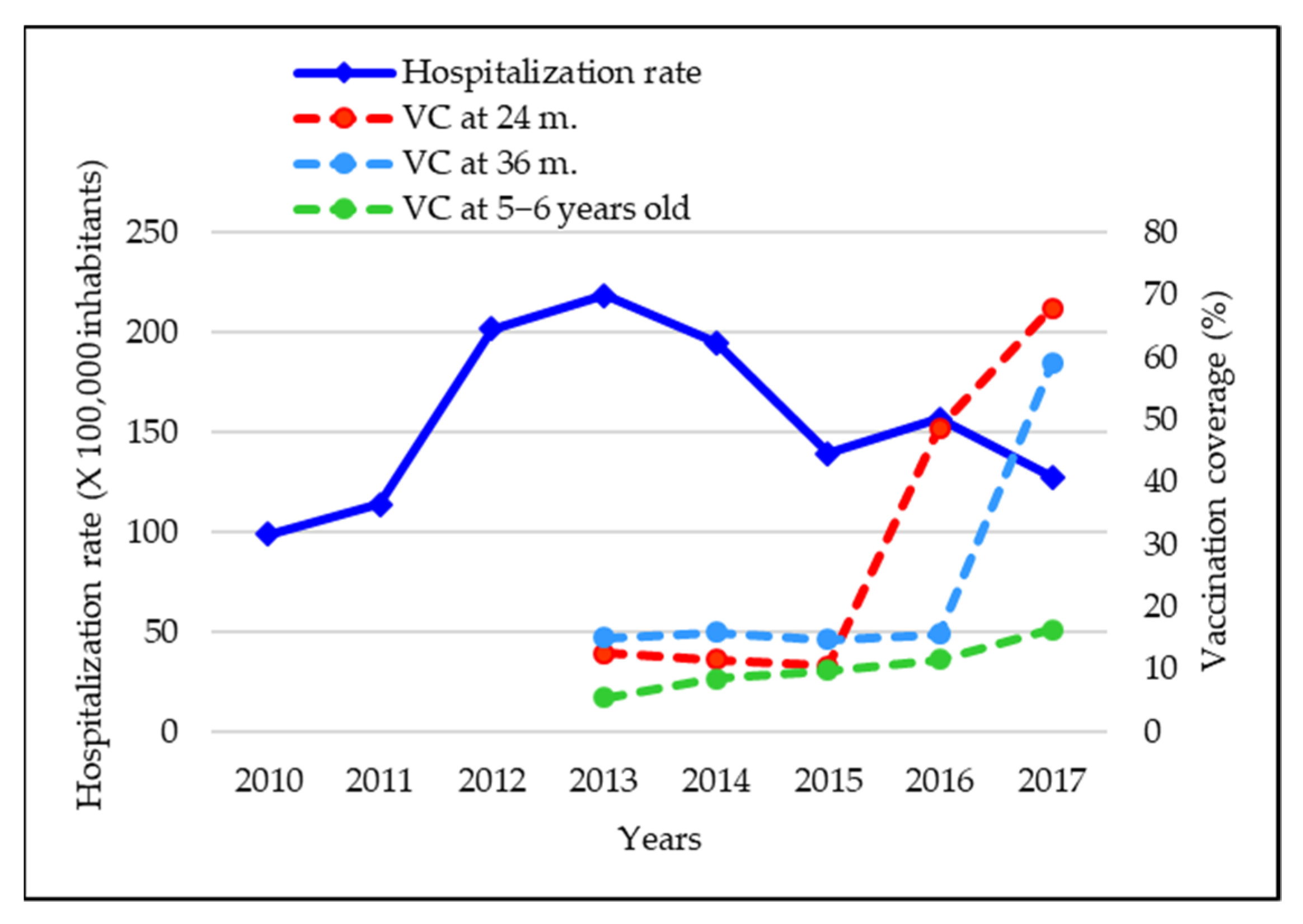
3.3. Vaccination Coverages in the Study Population
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Heininger, U.; Seward, J.F. Varicella. Lancet 2006, 368, 1365–1376. [Google Scholar] [CrossRef]
- Arvin, A.M. Varicella-zoster virus. Clin. Microbiol. Rev. 1996, 9, 361–381. [Google Scholar] [CrossRef] [PubMed]
- Gershon, A.A.; Breuer, J.; Cohen, J.I.; Cohrs, R.J.; Gershon, M.D.; Gilden, D.; Grose, C.; Hambleton, S.; Kennedy, P.G.; Oxman, M.N.; et al. Varicella zoster virus infection. Nat. Rev. Dis. Primers 2015, 1, 15016. [Google Scholar] [CrossRef] [Green Version]
- Varicella and herpes zoster vaccines: WHO position paper, June 2014-Recommendations. Vaccine 2016, 34, 198–199. [CrossRef] [PubMed]
- Bonanni, P.; Breuer, J.; Gershon, A.; Gershon, M.; Hryniewicz, W.; Papaevangelou, V.; Rentier, B.; Rümke, H.; Sad-zot-Delvaux, C.; Senterre, J.; et al. Varicella vaccination in Europe—Taking the practical approach. BMC Med. 2009, 7, 26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- European Centre for Disease Prevention and Control (ECDC). Varicella Vaccination in the European Union. Stockholm: ECDC: s.n. 2015. Available online: https://www.ecdc.europa.eu/sites/default/files/media/en/publications/Publications/Varicella-Guidance-2015.pdf (accessed on 16 September 2021).
- Riera-Montes, M.; Bollaerts, K.; Heininger, U.; Hens, N.; Gabutti, G.; Gil, A.; Nozad, B.; Mirinaviciute, G.; Flem, E.; Souverain, A.; et al. Estimation of the burden of varicella in Europe before the introduction of universal childhood immunization. BMC Infect. Dis. 2017, 17, 353. [Google Scholar] [CrossRef] [PubMed]
- Meszner, Z.; Molnar, Z.; Rampakakis, E.; Yang, H.K.; Kuter, B.J.; Wolfson, L.J. Economic burden of varicella in children 1–12 Years of age in Hungary, 2011–2015. BMC Infect. Dis. 2017, 17, 495. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gabutti, G.; Franchi, M.; Maniscalco, L.; Stefanati, A. Varicella-zoster virus: Pathogenesis, incidence patterns and vaccination programs. Minerva Pediatr. 2016, 68, 213–225. [Google Scholar]
- Gil, A.; Oyagüez, I.; Carrasco, P.; González, A. Epidemiology of primary varicella hospitalizations in Spain. Vaccine 2001, 20, 295–298. [Google Scholar] [CrossRef]
- Liese, J.G.; Grote, V.; Rosenfeld, E.; Fischer, R.; Belohradsky, B.H.; Kries, R.V.; ESPED Varicella Study Group. The burden of varicella complications before the introduction of routine varicella vaccination in Germany. J. Pediatr. Infect. Dis. 2008, 27, 119–124. [Google Scholar] [CrossRef]
- Grimprel, E.; Levy, C.; de La Rocque, F.; Cohen, R.; Soubeyrand, B.; Caulin, E.; Derrough, T.; Lecuyer, A.; d’Athis, P.; Gaudelus, J.; et al. Paediatric varicella hospitalisations in France: A nationwide survey. Clin. Microbiol. Infect. 2007, 13, 546–549. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spackova, M.; Muehlen, M.; Siedler, A. Complications of varicella after implementation of routine childhood varicella vaccination in Germany. J. Pediatr. Infect. Dis. 2010, 29, 884–886. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marchetto, S.; de Benedictis, F.M.; de Martino, M.; Versace, A.; Chiappini, E.; Bertaine, C.; Osimani, P.; Cordiali, R.; Gabiano, C.; Galli, L. Epidemiology of hospital admissions for chickenpox in children: An Italian multicentre study in the pre-vaccine era. Acta Paediatr. 2007, 96, 1490–1493. [Google Scholar] [CrossRef] [PubMed]
- Helmuth, I.G.; Poulsen, A.; Suppli, C.H.; Mølbak, K. Varicella in Europe-A review of the epidemiology and experience with vaccination. Vaccine 2015, 33, 2406–2413. [Google Scholar] [CrossRef]
- Warren-Gash, C.; Forbes, H.; Breuer, J. Varicella and herpes zoster vaccine development: Lessons learned. Expert Rev Vaccines 2017, 16, 1191–1201. [Google Scholar] [CrossRef] [Green Version]
- Strategic Advisory Group of Experts on Immunisation Varicella Wroking Group. Systematic Review of Available Evidence on Effectiveness and Duration of Protection of Varicella Vaccines. 2014. Available online: https://www.who.int/immunization/sage/meetings/2014/april/4_Systematic_review_on_effectiveness_and_duration_of_protection_of_varicella_vaccines.pdf (accessed on 16 September 2021).
- Papaloukas, O.; Giannouli, G.; Papaevangelou, V. Successes and challenges in varicella vaccine. Ther. Adv. Vaccines 2014, 2, 39–55. [Google Scholar] [CrossRef] [Green Version]
- Unim, B.; Saulle, R.; Boccalini, S.; Taddei, C.; Ceccherini, V.; Boccia, A.; Bonanni, P.; La Torre, G. Economic evaluation of Varicella vaccination: Results of a systematic review. Hum. Vaccines Immunother. 2013, 9, 1932–1942. [Google Scholar] [CrossRef] [Green Version]
- Trucchi, C.; Gabutti, G.; Cristina Rota, M.; Bella, A. Burden of varicella in Italy, 2001–2010: Analysis of data from multiple sources and assessment of universal vaccination impact in three pilot regions. J. Med. Microbiol. 2015, 64, 1387–1394. [Google Scholar] [CrossRef]
- Amodio, E.; Tramuto, F.; Cracchiolo, M.; Sciuto, V.; De Donno, A.; Guido, M.; Rota, M.C.; Gabutti, G.; Vitale, F. The impact of ten years of infant universal Varicella vaccination in Sicily, Italy (2003–2012). Hum. Vaccines Immunother. 2015, 11, 236–239. [Google Scholar] [CrossRef] [Green Version]
- Ministero Della Salute. Piano Nazionale Prevenzione Vaccinale (PNPV) 2012–2014. Available online: https://www.salute.gov.it/imgs/C_17_pubblicazioni_1721_allegato.pdf (accessed on 16 September 2021).
- Piano Nazionale Prevenzione Vaccinale (PNPV) 2017–2019. Available online: https://www.salute.gov.it/imgs/C_17_pubblicazioni_2571_allegato.pdf (accessed on 16 September 2021).
- Giammanco, G.; Ciriminna, S.; Barberi, I.; Titone, L.; Lo Giudice, M.; Biasio, L.R. Universal varicella vaccination in the Sicilian paediatric population: Rapid uptake of the vaccination programme and morbidity trends over five years. Eurosurveillance 2009, 14, 19321. [Google Scholar] [CrossRef]
- Aggiornamento Piano Regionale Prevenzione Vaccinale. Bollettino Ufficiale Della Regione Liguria. Parte II 21.01.2015. Available online: http://www.asl5.liguria.it/Portals/0/Comunicati/20150409_piano%20regionale%20vaccini%20liguria%202014.pdf (accessed on 16 September 2021).
- Varela, F.H.; Pinto, L.A.; Scotta, M.C. Global impact of varicella vaccination programs. Hum. Vaccines Immunother. 2019, 15, 645–657. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Waye, A.; Jacobs, P.; Tan, B. The impact of the universal infant varicella immunization strategy on Canadian varicella-related hospitalization rates. Vaccine 2013, 31, 4744–4748. [Google Scholar] [CrossRef]
- Tan, B.; Bettinger, J.; McConnell, A.; Scheifele, D.; Halperin, S.; Vaudry, W.; Law, B.; Members of the Canadian Immunization Monitoring Program, Active (IMPACT). The effect of funded varicella immunization programs on varicella-related hospitalizations in IMPACT centers, Canada, 2000–2008. J. Pediatr. Infect. Dis. 2012, 31, 956–963. [Google Scholar] [CrossRef]
- Ozdemir, H.; Candir, M.O.; Karbuz, A.; Belet, N.; Tapisiz, A.; Ciftçi, E.; Ince, E. Chickenpox complications, incidence and financial burden in previously healthy children and those with an underlying disease in Ankara in the pre-vaccination period. Turk. J. Pediatr. Dis. 2011, 53, 614–625. [Google Scholar]
- Piazza, M.F.; Paganino, C.; Amicizia, D.; Trucchi, C.; Orsi, A.; Astengo, M.; Romairone, P.; Simonetti, S.; Icardi, G.; Ansaldi, F. The Unknown Health Burden of Herpes Zoster Hospitalizations: The Effect on Chronic Disease Course in Adult Patients ≥50 Years. Vaccines 2020, 8, 20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Azzari, C.; Massai, C.; Poggiolesi, C.; Indolfi, G.; Spagnolo, G.; De Luca, M.; Gervaso, P.; de Martino, M.; Resti, M. Cost of varicella-related hospitalisations in an Italian paediatric hospital: Comparison with possible vaccination expenses. Curr. Med. Res. Opin. 2007, 23, 2945–2954. [Google Scholar] [CrossRef] [PubMed]
- Ministero dell’Economia e delle Finanze. Libro Verde Della Spesa Pubblica 2007—Aggiornato Con l’indice dei Prezzi al Consumo Ministero dell’Economia e Delle Finanze. 2007. Available online: https://www.mef.gov.it/ministero/commissioni/ctfp/documenti (accessed on 16 September 2021).
- Kuter, B.; Matthews, H.; Shinefield, H.; Black, S.; Dennehy, P.; Watson, B.; Reisinger, K.; Kim, L.L.; Lupinacci, L.; Hartzel, J.; et al. Ten year follow-up of healthy children who received one or two injections of varicella vaccine. J. Pediatr. Infect. Dis. 2004, 23, 132–137. [Google Scholar] [CrossRef]
- Prymula, R.; Bergsaker, M.R.; Esposito, S.; Gothefors, L.; Man, S.; Snegova, N.; Štefkovičova, M.; Usonis, V.; Wysocki, J.; Douha, M.; et al. Protection against varicella with two doses of combined measles-mumps-rubella-varicella vaccine versus one dose of monovalent varicella vaccine: A multicentre, observer-blind, randomised, controlled trial. Lancet 2014, 383, 1313–1324. [Google Scholar] [CrossRef]
- Gabutti, G.; Rota, M.C.; Guido, M.; De Donno, A.; Bella, A.; Ciofi degli Atti, M.L.; Crovari, P.; Seroepidemiology Group. The epidemiology of Varicella Zoster Virus infection in Italy. BMC Public Health 2008, 8, 372. [Google Scholar] [CrossRef] [Green Version]
- Regional Law 29/07/2016, n.17. Istituzione dell’Azienda Ligure Sanitaria della Regione Liguria (A.Li.Sa.) e Indirizzi per il Riordino Delle Disposizioni Regionali in Materia Sanitaria e Sociosanitaria. Bollettino Ufficiale n.15, 30/07/2016. Available online: http://lrv.regione.liguria.it/liguriass_prod/articolo?urndoc=urn:nir:regione.liguria:legge:2016-07-29;17&pr=idx,0;artic,1;articparziale,0 (accessed on 22 November 2021).
| ICD-9-CM | Description |
|---|---|
| 052.0 | Post-varicella encephalitis |
| 052.1 | Varicella (hemorrhagic) pneumonia |
| 052.2 | Post-varicella myelitis |
| 052.7 | Varicella with other specified complications |
| 052.8 | Varicella with unspecified complication |
| 052.9 | Varicella without mention of complication |
| Comorbidities n. (%) | Total Events | ED Accesses | Hospitalization Preceded or Not by ED Access |
|---|---|---|---|
| Patients without comorbidities | 2083 (93.03) | 1893 (93.99) | 190 (84.44) |
| ≥1 comorbidity | 156 (6.97) | 121 (6.01) | 35 (15.56) |
| C02—Transplant | 0 (0.0) | 0 (0.00) | 0 (0.00) |
| C03—Chronic renal failure | 2 (1.28) | 0 (0.00) | 2 (5.71) |
| C04—HIV/AIDS | 0 (0.0) | 0 (0.00) | 0 (0.00) |
| C05—Cancer | 4 (2.56) | 2 (1.65) | 2 (5.71) |
| C06—Diabetes | 6 (3.85) | 3 (2.48) | 3 (8.57) |
| C07—Cardiovascular disease | 32 (20.51) | 26 (21.49) | 6 (17.14) |
| C07S1—Hypertension | 1 (3.13) | 0 (0.00) | 1 (16.67) |
| C07S2—Ischemic heart disease | 0 (0.00) | 0 (0.00) | 0 (0.00) |
| C07S3—Valvular heart disease | 27 (84.38) | 23 (88.46) | 4 (66.67) |
| C07S4—Arrhythmic myocardiopathy | 3 (9.38) | 1 (3.85) | 2 (33.33) |
| C07S5—Non-arrhythmic myocardiopathy | 0 (0.00) | 0 (0.00) | 0 (0.00) |
| C07S6—Heart failure | 0 (0.00) | 0 (0.00) | 0 (0.00) |
| C07V1—Arterial vasculopathy | 0 (0.00) | 0 (0.00) | 0 (0.00) |
| C07V2—Venous vascular disease | 1 (3.13) | 1 (3.85) | 0 (0.00) |
| C07V3—Cerebral vasculopathy | 3 (9.38) | 2 (7.69) | 1 (16.67) |
| C08—Bronchopneumopathy | 87 (55.77) | 69 (57.02) | 18 (51.43) |
| C08A—Asthma | 86 (98.85) | 69 (100.00) | 17 (94.44) |
| C08B—COPD | 1 (1.15) | 0 (0.00) | 1 (5.56) |
| C08C—Respiratory failure/oxygen therapy | 1 (1.15) | 0 (0.00) | 1 (5.56) |
| C09—Gastroenteropathy | 3 (1.92) | 2 (1.65) | 1 (2.86) |
| C10—Neuropathy | 13 (8.33) | 9 (7.44) | 4 (11.43) |
| C11—Autoimmune disease | 3 (1.92) | 2 (1.65) | 1 (2.86) |
| C12—Endocrine and metabolic disease | 5 (3.21) | 2 (1.65) | 3 (8.57) |
| C13—Rare disease | 10 (6.41) | 5 (4.13) | 5 (14.29) |
| C14—Psychosis | 6 (3.85) | 6 (4.96) | 0 (0.00) |
| Comorbidities | OR | Low 95% CI | Up 95% CI | p-Value |
|---|---|---|---|---|
| C02—Transplant | - | - | - | - |
| C03—Chronic renal failure | 2.488 | 0.294 | 9.409 | 0.397 |
| C04—HIV/AIDS | - | - | - | - |
| C05—Cancer | 0.391 | 0.105 | 1.022 | 0.057 |
| C06—Diabetes | 1.726 | 0.620 | 3.873 | 0.293 |
| C07—Cardiovascular disease | 1.178 | 0.790 | 1.718 | 0.405 |
| C08—Bronchopneumopathy | 1.629 | 1.204 | 2.204 | 0.001 |
| C09—Gastroenteropathy | 0.496 | 0.101 | 1.483 | 0.307 |
| C10—Neuropathy | 1.108 | 0.576 | 1.957 | 0.808 |
| C11—Autoimmune disease | 0.641 | 0.130 | 1.916 | 0.635 |
| C12—Endocrine and metabolic disease | 0.539 | 0.172 | 1.287 | 0.214 |
| C13—Rare disease | 0.442 | 0.208 | 0.836 | 0.008 |
| C14—Psychosis | 0.734 | 0.265 | 1.639 | 0.600 |
| Total Events | ED Accesses | Hospitalization Preceded or Not by ED Access | ||||
|---|---|---|---|---|---|---|
| Year | Number | Costs (Adjusted for Inflation) | Number | Costs (Adjusted for Inflation) | Number | Costs (Adjusted for Inflation) |
| 2010 | 138 | €61,747 (€67,489) | 113 | €2076 (€2269) | 25 | €59,670 (€65,219) |
| 2011 | 173 | €72,058 (€77,102) | 135 | €2549 (€2727) | 38 | €69,509 (€74,375) |
| 2012 | 334 | €66,037 (€68,480) | 308 | €6757 (€7007) | 26 | €59,280 (€61,473) |
| 2013 | 390 | €100,147 (€101,649) | 351 | €8049 (€8170) | 39 | €92,097 (€93,478) |
| 2014 | 363 | €71,941 (€72,588) | 333 | €7945 (€8017) | 30 | €63,996 (€64,573) |
| 2015 | 271 | €44,670 (€45,429) | 257 | €6287 (€6373) | 14 | €38,383 (€39,036) |
| 2016 | 332 | €127,852 (€129,642) | 289 | €6285 (€6373) | 43 | €121,567 (€123,269) |
| 2017 | 285 | €79,854 (€80,253) | 255 | €5997 (€6027) | 30 | €73,857 (€74,226) |
| Total | 2286 | €624,305 (€642,634) | 2041 | €45,945 (€46,984) | 245 | €578,360 (€595,649) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Piazza, M.F.; Amicizia, D.; Paganino, C.; Marchini, F.; Astengo, M.; Grammatico, F.; Trucchi, C.; Romairone, P.; Simonetti, S.; Sticchi, C.; et al. Has Clinical and Epidemiological Varicella Burden Changed over Time in Children? Overview on Hospitalizations, Comorbidities and Costs from 2010 to 2017 in Italy. Vaccines 2021, 9, 1485. https://doi.org/10.3390/vaccines9121485
Piazza MF, Amicizia D, Paganino C, Marchini F, Astengo M, Grammatico F, Trucchi C, Romairone P, Simonetti S, Sticchi C, et al. Has Clinical and Epidemiological Varicella Burden Changed over Time in Children? Overview on Hospitalizations, Comorbidities and Costs from 2010 to 2017 in Italy. Vaccines. 2021; 9(12):1485. https://doi.org/10.3390/vaccines9121485
Chicago/Turabian StylePiazza, Maria Francesca, Daniela Amicizia, Chiara Paganino, Francesca Marchini, Matteo Astengo, Federico Grammatico, Cecilia Trucchi, Paolo Romairone, Simona Simonetti, Camilla Sticchi, and et al. 2021. "Has Clinical and Epidemiological Varicella Burden Changed over Time in Children? Overview on Hospitalizations, Comorbidities and Costs from 2010 to 2017 in Italy" Vaccines 9, no. 12: 1485. https://doi.org/10.3390/vaccines9121485
APA StylePiazza, M. F., Amicizia, D., Paganino, C., Marchini, F., Astengo, M., Grammatico, F., Trucchi, C., Romairone, P., Simonetti, S., Sticchi, C., & Ansaldi, F. (2021). Has Clinical and Epidemiological Varicella Burden Changed over Time in Children? Overview on Hospitalizations, Comorbidities and Costs from 2010 to 2017 in Italy. Vaccines, 9(12), 1485. https://doi.org/10.3390/vaccines9121485






