12 Months Persistent Immunogenicity after Hepatitis B Vaccination in Patients with Type 2 Diabetes and Immunogenicity of Revaccination in Non-Responders: An Open-Label Randomized Controlled Trial
Abstract
1. Introduction
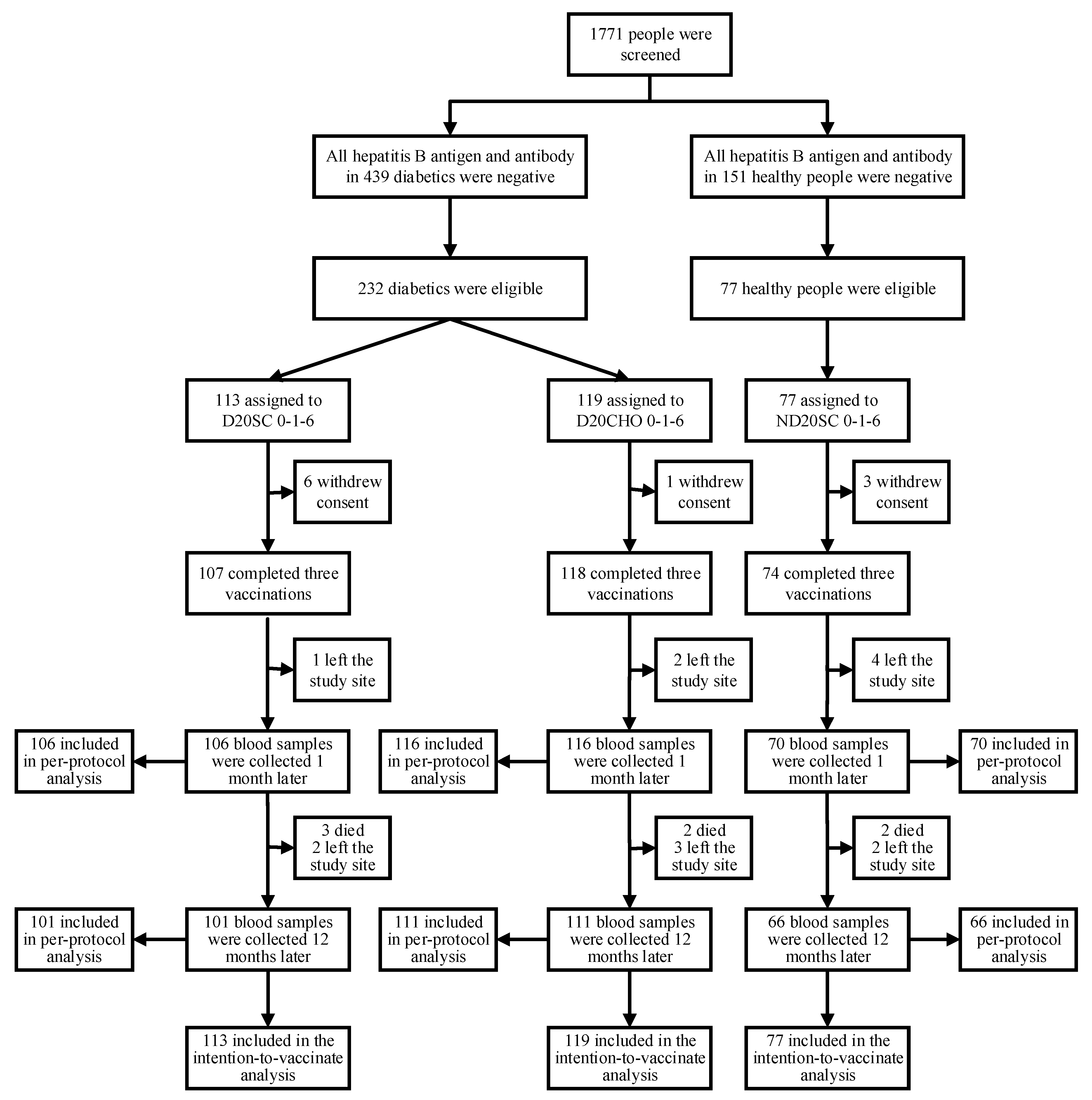
2. Methods
2.1. Study Design
2.2. Laboratory Assays
2.3. Ethical Approval
2.4. Statistical Analysis
3. Results
3.1. Participants’ Characteristics at Baseline
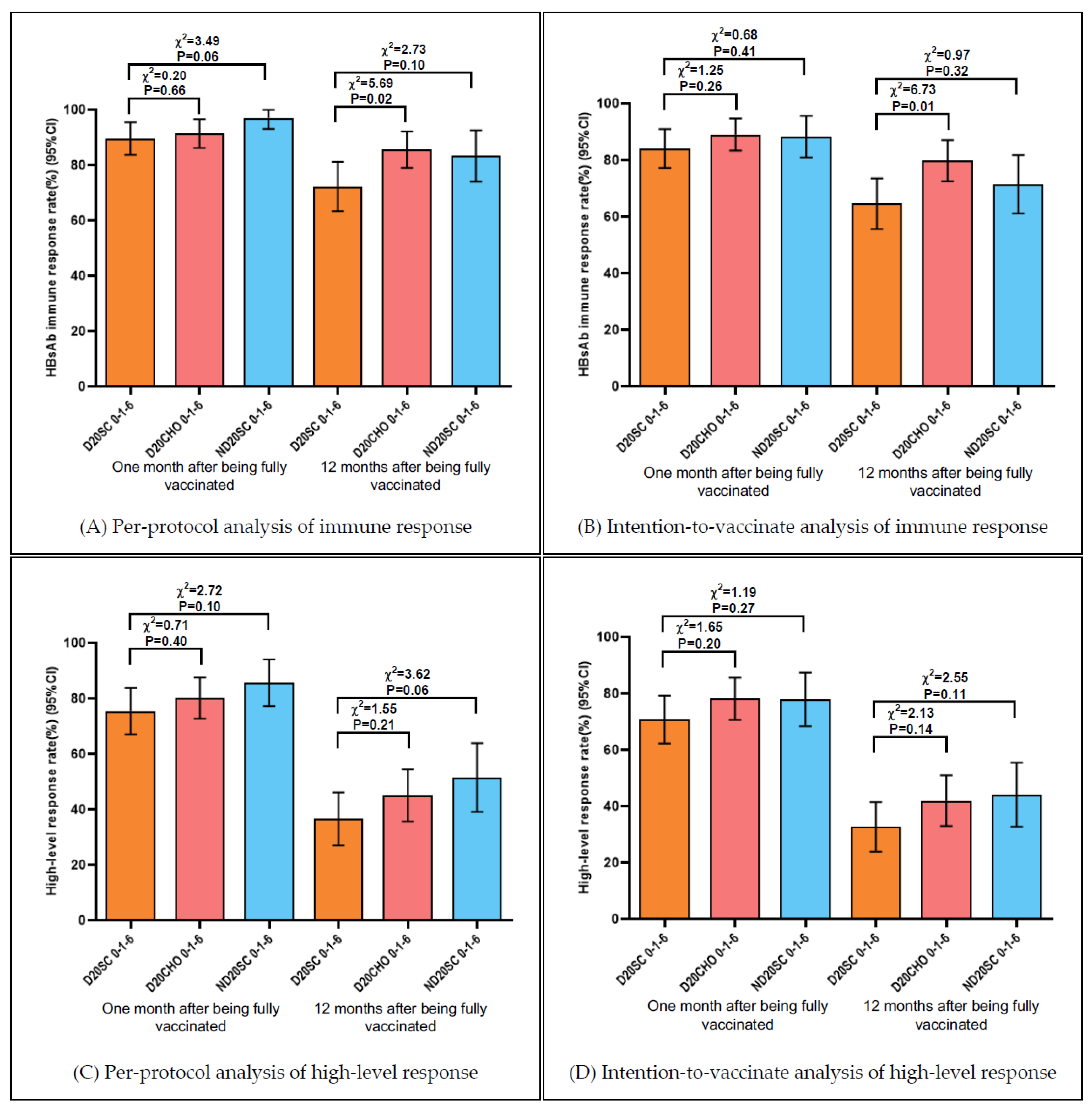
3.2. Anti-HBs Immune Response Rate and High-Level Response Rate One and Twelve Months after Being Fully Vaccinated
3.3. Maintenance of Anti-HBs Concentration after Twelve Months
3.4. Response after Revaccination of Non-Responders in Diabetic Patients
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Key Facts of Hepatitis B. Available online: https://www.who.int/news-room/fact-sheets/detail/hepatitis-b (accessed on 18 September 2021).
- Liu, J.; Liang, W.; Jing, W.; Liu, M. Countdown to 2030: Eliminating hepatitis B disease, China. Bull. World Health Organ. 2019, 97, 230–238. [Google Scholar] [CrossRef]
- Wang, H.; Men, P.; Xiao, Y.; Gao, P.; Lv, M.; Yuan, Q.; Chen, W.; Bai, S.; Wu, J. Hepatitis B infection in the general population of China: A systematic review and meta-analysis. BMC Infect. Dis. 2019, 19, 811. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Feng, D.; Xu, J.; Feng, X.; Dong, P.; Li, J.; Ye, Y.; Zhang, Y.; Guo, W. The prevalence of hepatitis B infection in central China: An adult population-based serological survey of a large sample size. J. Med. Virol. 2017, 89, 450–457. [Google Scholar]
- Zhang, H.; Li, Q.; Sun, J.; Wang, C.; Gu, Q.; Feng, X.; Du, B.; Wang, W.; Shi, X.; Zhang, S.; et al. Seroprevalence and risk factors for hepatitis B infection in an adult population in Northeast China. Int. J. Med. Sci. 2011, 8, 321–331. [Google Scholar] [CrossRef][Green Version]
- Liang, X.; Bi, S.; Yang, W.; Wang, L.; Cui, G.; Cui, F.; Zhang, Y.; Liu, J.; Gong, X.; Chen, Y.; et al. Epidemiological serosurvey of hepatitis B in China—Declining HBV prevalence due to hepatitis B vaccination. Vaccine 2009, 27, 6550–6557. [Google Scholar] [CrossRef] [PubMed]
- Ma, R.C.W. Epidemiology of diabetes and diabetic complications in China. Diabetologia 2018, 61, 1249–1260. [Google Scholar] [CrossRef]
- Reilly, M.L.; Schillie, S.F.; Smith, E.; Poissant, T.; Vonderwahl, C.W.; Gerard, K.; Baumgartner, J.; Mercedes, L.; Sweet, K.; Muleta, D.; et al. Increased risk of acute hepatitis B among adults with diagnosed diabetes mellitus. J. Diabetes Sci. Technol. 2012, 6, 858–866. [Google Scholar] [CrossRef]
- Han, B.F.; Yuan, Q.L.; Liu, J.; Cui, F.Q. The risk of hepatitis B virus infection in people with diabetes mellitus: A meta-analysis. Chin. J. Prev. Med. 2018, 52, 748–752. [Google Scholar]
- Sawyer, M.H.; Hoerger, T.J.; Murphy, T.V.; Schillie, S.F.; Hu, D.; Spradling, P.R.; Byrd, K.K.; Xing, J.; Reilly, M.L.; Tohme, R.A.; et al. Use of hepatitis B vaccination for adults with diabetes mellitus: Recommendations of the advisory committee on immunization practices (ACIP). Morb. Mortal. Wkly. Rep. 2011, 60, 1709–1711. [Google Scholar]
- WHO. Hepatitis B vaccines: WHO position paper, July 2017-Recommendations. Vaccine 2019, 37, 223–225. [Google Scholar] [CrossRef]
- Cui, F.; Shen, L.; Li, L.; Wang, H.; Wang, F.; Bi, S.; Liu, J.; Zhang, G.; Wang, F.; Zheng, H.; et al. Prevention of Chronic Hepatitis B after 3 Decades of Escalating Vaccination Policy, China. Emerg. Infect. Dis. 2017, 23, 765–772. [Google Scholar] [CrossRef] [PubMed]
- Cui, F.; Wang, X.; Cao, L.; Liang, X.; Lu, Y.; Hu, Y.; Hadler, S.C.; Shapiro, C.N.; Wiersma, S.T.; Ward, J.W. Progress in Hepatitis B Prevention Through Universal Infant Vaccination-China, 1997–2006. JAMA 2007, 298, 506–509. [Google Scholar]
- Chinese Society of Infectious Diseases, Chinese Medical Association; Chinese Society of Hepatology, Chinese Medical Association. Guidelines for the prevention and treatment of chronic hepatitis B (version 2019). J. Clin. Hepatol. 2019, 35, 2648–2669. [Google Scholar]
- Han, B.; Liu, W.; Du, J.; Liu, H.; Zhao, T.; Yang, S.; Wang, S.; Zhang, S.; Liu, B.; Liu, Y.; et al. Immunogenicity and safety of hepatitis B vaccination in patients with type 2 diabetes in China: An open-label randomized controlled trial. Vaccine 2021, 39, 3365–3371. [Google Scholar] [CrossRef]
- Andre, F.E. Summary of safety and efficacy data on a yeast-derived hepatitis B vaccine. Am. J. Med. 1989, 87, 14S–20S. [Google Scholar] [CrossRef]
- Zajac, B.A.; West, D.J.; Mcaleer, W.J.; Scolnick, E.M. Overview of Clinical-Studies with Hepatitis-B Vaccine Made by Recombinant-DNA. J. Infect. 1986, 13, 39–45. [Google Scholar] [CrossRef]
- Zhang, W.; Han, L.; Lin, C.; Wang, H.; Pang, X.; Li, L.; Gao, P.; Lin, H.; Gong, X.; Tang, Y.; et al. Surface antibody and cytokine response to recombinant Chinese hamster ovary cell (CHO) hepatitis B vaccine. Vaccine 2011, 29, 6276–6282. [Google Scholar] [CrossRef]
- Yan, B.; Zhang, L.; Lv, J.; Liu, J.; Feng, Y.; Xu, A.; Chen, S.; Gong, X.; Cui, F.; Liang, X. Comparison of the antibody response and related influencing factors after primary immunization by 10 μg hepatitis B vaccine made from recombinant DNA techniques in saccharomyces and hansenula polymorpha among adults. Chin. J. Epidemiol. 2012, 33, 988–989. [Google Scholar]
- Liu, J.; Yan, B.; Zhang, L.; Lv, J.; Feng, Y.; Ji, F.; Chen, S.; Xu, A. Comparison on the Antibody Response and Influenced Factors of Hepatitis B Vacine Made by Recombinant Dexyribonucleic Acid Techniques among Adults. Chin. J. Vaccines Immun. 2013, 19, 142–146. [Google Scholar]
- Feng, Y.L.; Shi, J.; Gao, L.Y.; Yao, T.; Feng, D.; Luo, D.; Li, Z.; Zhang, Y.; Wang, F.; Cui, F.; et al. Immunogenicity and safety of high-dose hepatitis B vaccine among drug users: A randomized, open-labeled, blank-controlled trial. Hum. Vaccines Immunother. 2017, 13, 1297–1303. [Google Scholar] [CrossRef][Green Version]
- Vargas, J.I.; Jensen, D.; Martinez, F.; Sarmiento, V.; Peirano, F.; Acuna, P.; Provoste, F.; Bustos, V.; Cornejo, F.; Fuster, A.; et al. Comparative Efficacy of a High-Dose vs Standard-Dose Hepatitis B Revaccination Schedule among Patients with HIV A Randomized Clinical Trial. JAMA Netw. Open 2021, 4, e2120929. [Google Scholar] [CrossRef]
- Zhang, Y.; Ma, J.C.; Qi, S.X.; Wang, F.; Zhao, C.; Bi, S.L. Effectiveness of a Chinese hamster ovary cell derived hepatitis B vaccine in Chinese rural communities. Vaccine 2011, 29, 3905–3908. [Google Scholar] [CrossRef]
- Wang, F.; Zhao, Y.L.; Ma, J.C.; Bi, S.L.; Zhang, Y.; Shen, L.P. Long-term efficacy of 10–12 years after being immunized with Chinese hamster ovary cell derived hepatitis B vaccine in Chinese Rural Communities. Vaccine 2012, 30, 2051–2053. [Google Scholar] [CrossRef]
- Wang, F.; Ma, J.; Hao, Z.; Zhang, Z.; Zhang, X.; Gao, Z.; Bi, S.; Shen, L.; Qiu, F.; Zhao, Y. The long-term efficacy of Chinese hamster ovary cell derived hepatitis B vaccine after being used for 14–16 years in Chinese rural communities. Vaccine 2015, 33, 294–297. [Google Scholar] [CrossRef]
- Wu, W.L.; Yan, B.Y.; Lyu, J.J.; Liu, J.Y.; Feng, Y.; Chen, S.Y.; Zhou, L.B.; Liang, X.F.; Cui, F.Q.; Wang, F.Z.; et al. Antibody persistence following primary vaccination with hepatitis B vaccine among normal and high-responder adults: A 5-year follow-up study. Chin. J. Prev. Med. 2016, 50, 484–490. [Google Scholar]
- Zhang, W.; Han, L.L.; Lin, C.Y.; Li, L.Q.; Gao, P.; Lin, H.; Gong, X.H.; Huang, F.; Tang, Y.Q.; Ma, J.X.; et al. Study on the cellular and humoral immunity effect of recombinant Chinese hamster ovary cell hepatitis B vaccine in adults. Chin. J. Prev. Med. 2010, 44, 918–922. [Google Scholar]
- Roznovsky, L.; Orsagova, I.; Kloudova, A.; Tvrdik, J.; Kabieszova, L.; Lochman, I.; Mrazek, J.; Hozakova, L.; Zjevikova, A.; Pliskova, L. Long-term protection against hepatitis B after newborn vaccination: 20-year follow-up. Infection 2010, 38, 395–400. [Google Scholar] [CrossRef]
- Lee, K.H.; Shim, K.S.; Lim, I.S.; Chae, S.A.; Yun, S.W.; Lee, N.M.; Choi, Y.B.; Yi, D.Y. Changes in hepatitis B virus antibody titers over time among children: A single center study from 2012 to 2015 in an urban of South Korea. BMC Pediatr. 2017, 17, 164. [Google Scholar] [CrossRef]
- Kakisaka, K.; Sakai, A.; Yoshida, Y.; Miyasaka, A.; Takahashi, F.; Sumazaki, R.; Takikawa, Y. Hepatitis B Surface Antibody Titers at One and Two Years after Hepatitis B Virus Vaccination in Healthy Young Japanese Adults. Internal Med. 2019, 58, 2349–2355. [Google Scholar] [CrossRef]
- Ren, W.; Ren, J.J.; Wu, Z.K.; Shen, L.Z.; Shan, H.; Dai, X.W.; Li, J.; Liu, Y.; Qiu, Y.; Yao, J.; et al. Long-term persistence of anti-HBs after hepatitis B vaccination among adults: 8-year results. Hum. Vaccines Immunother. 2020, 16, 687–692. [Google Scholar] [CrossRef]
- Fisman, D.N.; Agrawal, D.; Leder, K. The effect of age on immunologic response to recombinant hepatitis B vaccine: A meta-analysis. Clin. Infect. Dis. 2002, 35, 1368–1375. [Google Scholar] [CrossRef] [PubMed]
- Derave, S.; Heijtink, R.A.; Bakkerbendik, M.; Boot, J.; Schalm, S.W. Immunogenicity of Standard and Low-Dose Vaccination Using Yeast-Derived Recombinant Hepatitis-B Surface-Antigen in Elderly Volunteers. Vaccine 1994, 12, 532–534. [Google Scholar] [CrossRef][Green Version]
- Yang, S.; Tian, G.; Cui, Y.; Ding, C.; Deng, M.; Yu, C.; Xu, K.; Ren, J.; Yao, J.; Li, Y.; et al. Factors influencing immunologic response to hepatitis B vaccine in adults. Sci. Rep. 2016, 6, 27251. [Google Scholar] [CrossRef]
- Yang, L.; Yao, J.; Li, J.; Chen, Y.; Jiang, Z.G.; Ren, J.J.; Xu, K.; Ruan, B.; Yang, S.; Wang, B.; et al. Suitable hepatitis B vaccine for adult immunization in China. Immunol. Res. 2016, 64, 242–250. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lu, J.J.; Yan, B.Y.; Liu, J.Y.; Wu, W.L.; Feng, Y.; Xu, A.Q.; Zhang, L. Comparison of anti-HBs persistence after hepatitis B vaccination on two-dose schedule and three-dose schedule among adults: Results from a 12-year follow up study in China. Hum. Vaccines Immunother. 2019, 15, 1171–1176. [Google Scholar] [CrossRef]
- Cocchio, S.; Baldo, V.; Volpin, A.; Fonzo, M.; Floreani, A.; Furlan, P.; Mason, P.; Trevisan, A.; Scapellato, M.L. Persistence of Anti-Hbs after up to 30 Years in Health Care Workers Vaccinated against Hepatitis B Virus. Vaccines 2021, 9, 323. [Google Scholar] [CrossRef]
- Qiu, Y.; Ren, J.; Yao, J. Healthy adult vaccination: An urgent need to prevent hepatitis B in China. Hum. Vaccines Immunother. 2016, 12, 773–778. [Google Scholar] [CrossRef]
- Zhang, L.; Liu, J.; Lu, J.; Yan, B.; Song, L.; Li, L.; Cui, F.; Zhang, G.; Wang, F.; Liang, X.; et al. Antibody response to revaccination among adult non-responders to primary Hepatitis B vaccination in China. Hum. Vaccines Immunother. 2015, 11, 2716–2722. [Google Scholar] [CrossRef]
- Hou, J.; Wang, G.; Wang, F.; Cheng, J.; Ren, H.; Zhuang, H.; Sun, J.; Li, L.; Li, J.; Meng, Q.; et al. Guideline of Prevention and Treatment for Chronic Hepatitis B (2015 Update). J. Clin. Transl. Hepatol. 2017, 5, 297–318. [Google Scholar] [CrossRef]
- Pan, H.X.; Zeng, Y.; Song, X.F.; Zhang, Y.J.; Xu, K.; Liang, Z.L.; Zhu, F.C. Immune response to hepatitis B vaccine with high antigen content in non-responders after standard primary vaccination in Chinese adults. Vaccine 2014, 32, 3706–3712. [Google Scholar] [CrossRef]
- Egea, E.; Iglesias, A.; Salazar, M.; Morimoto, C.; Kruskall, M.S.; Awdeh, Z.; Schlossman, S.F.; Alper, C.A.; Yunis, E.J. The cellular basis for lack of antibody response to hepatitis B vaccine in humans. J. Exp. Med. 1991, 173, 531–538. [Google Scholar] [CrossRef] [PubMed]
- Godkin, A.; Davenport, M.; Hill, A.V. Molecular analysis of HLA class II associations with hepatitis B virus clearance and vaccine nonresponsiveness. Hepatology 2005, 41, 1383–1390. [Google Scholar] [CrossRef] [PubMed]
| D20SC 0-1-6 | D20CHO 0-1-6 | ND20SC 0-1-6 | χ2 | p | |
|---|---|---|---|---|---|
| Sex | 3.08 | 0.21 | |||
| Female | 70 (66.0) | 71 (61.2) | 37 (52.9) | ||
| Male | 36 (34.0) | 45 (38.8) | 33 (47.1) | ||
| Age (years) | 7.88 | 0.10 | |||
| ≤50 | 18 (17.0) | 21 (18.1) | 21 (30.0) | ||
| 50–60 | 52 (49.1) | 54 (46.6) | 35 (50.0) | ||
| >60 | 36 (34.0) | 41 (35.3) | 14 (20.0) | ||
| Education | 6.71 | 0.15 | |||
| Senior high school or above | 5 (4.7) | 9 (7.8) | 9 (12.9) | ||
| Junior high school | 23 (21.7) | 26 (22.4) | 21 (30.0) | ||
| Primary school or below | 78 (73.6) | 81 (69.8) | 40 (57.1) | ||
| Marriage | 2.40 | 0.30 | |||
| Married | 96 (90.6) | 110 (94.8) | 67 (95.7) | ||
| Unmarried | 10 (9.4) | 6 (5.2) | 3 (4.3) | ||
| Occupation | 2.13 | 0.35 | |||
| Farmer | 105 (99.1) | 112 (96.6) | 67 (95.7) | ||
| Others | 1 (0.9) | 4 (3.4) | 3 (4.3) | ||
| BMI (Mean ± Standard deviation) | 23.7 (3.1) | 22.8 (2.8) | 23.9 (3.5) | 2.50 a | 0.08 b |
| Duration of diabetes diagnosis (years) | |||||
| ≤2 | 13 (12.6) | 25 (24.3) | 5.77 | 0.12 | |
| 2–4 | 34 (33.0) | 29 (28.2) | |||
| 4–7 | 23 (22.3) | 32 (31.1) | |||
| >7 | 36 (35.0) | 30 (29.1) | |||
| Total | 106 (100.0) | 116 (100.0) | 70 (100.0) | ||
| Anti-HBs Concentration (mIU/mL) | Diabetic Groups | Control Group | χ2 * | p |
|---|---|---|---|---|
| Responders 12 Months after Being Fully Vaccinated/Initial Responders (%) | Responders 12 Months after Being Fully Vaccinated/Initial Responders (%) | |||
| 10–100 | 10/28 (35.7) | 4/8 (50.0) | 0.10 | 0.75 |
| 100–1000 | 69/82 (84.1) | 18/24 (75.0) | 0.53 | 0.47 |
| 1000–10,000 | 60/63 (95.2) | 21/24 (87.5) | 0.64 | 0.42 |
| >10,000 | 27/28 (96.4) | 12/12 (100.0) | 0.00 | 1.00 |
| χ2 # | 35.58 | 8.44 | ||
| p | <0.01 | <0.01 |
| Anti-HBs Concentration (mIU/mL) | Group SV60 | Group SV20 | χ2 | p |
|---|---|---|---|---|
| N. (%) | N. (%) | |||
| <10 | 0 (0) | 3 (33.3) | 7.92 | 0.048 |
| 10–100 | 2 (20.0) | 4 (44.4) | ||
| 100–1000 | 5 (50.0) | 2 (22.2) | ||
| 1000–10,000 | 3 (30.0) | 0 (0) | ||
| Total | 10 (100) | 9 (100) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, B.; Liu, W.; Du, J.; Liu, H.; Zhao, T.; Yang, S.; Wang, S.; Zhang, S.; Liu, B.; Liu, Y.; et al. 12 Months Persistent Immunogenicity after Hepatitis B Vaccination in Patients with Type 2 Diabetes and Immunogenicity of Revaccination in Non-Responders: An Open-Label Randomized Controlled Trial. Vaccines 2021, 9, 1407. https://doi.org/10.3390/vaccines9121407
Han B, Liu W, Du J, Liu H, Zhao T, Yang S, Wang S, Zhang S, Liu B, Liu Y, et al. 12 Months Persistent Immunogenicity after Hepatitis B Vaccination in Patients with Type 2 Diabetes and Immunogenicity of Revaccination in Non-Responders: An Open-Label Randomized Controlled Trial. Vaccines. 2021; 9(12):1407. https://doi.org/10.3390/vaccines9121407
Chicago/Turabian StyleHan, Bingfeng, Wu Liu, Juan Du, Hanyu Liu, Tianshuo Zhao, Shubo Yang, Shuai Wang, Sihui Zhang, Bei Liu, Yaqiong Liu, and et al. 2021. "12 Months Persistent Immunogenicity after Hepatitis B Vaccination in Patients with Type 2 Diabetes and Immunogenicity of Revaccination in Non-Responders: An Open-Label Randomized Controlled Trial" Vaccines 9, no. 12: 1407. https://doi.org/10.3390/vaccines9121407
APA StyleHan, B., Liu, W., Du, J., Liu, H., Zhao, T., Yang, S., Wang, S., Zhang, S., Liu, B., Liu, Y., & Cui, F. (2021). 12 Months Persistent Immunogenicity after Hepatitis B Vaccination in Patients with Type 2 Diabetes and Immunogenicity of Revaccination in Non-Responders: An Open-Label Randomized Controlled Trial. Vaccines, 9(12), 1407. https://doi.org/10.3390/vaccines9121407






