Predictors of COVID-19 Vaccine Acceptance and Hesitancy among Healthcare Workers in Southern California: Not Just “Anti” vs. “Pro” Vaccine
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample and Recruitment Strategy
2.2. Data Collection Process
2.3. Measures
2.4. Analysis
3. Results
3.1. Sample Characteristics
3.2. Predictors of Vaccination Intentions
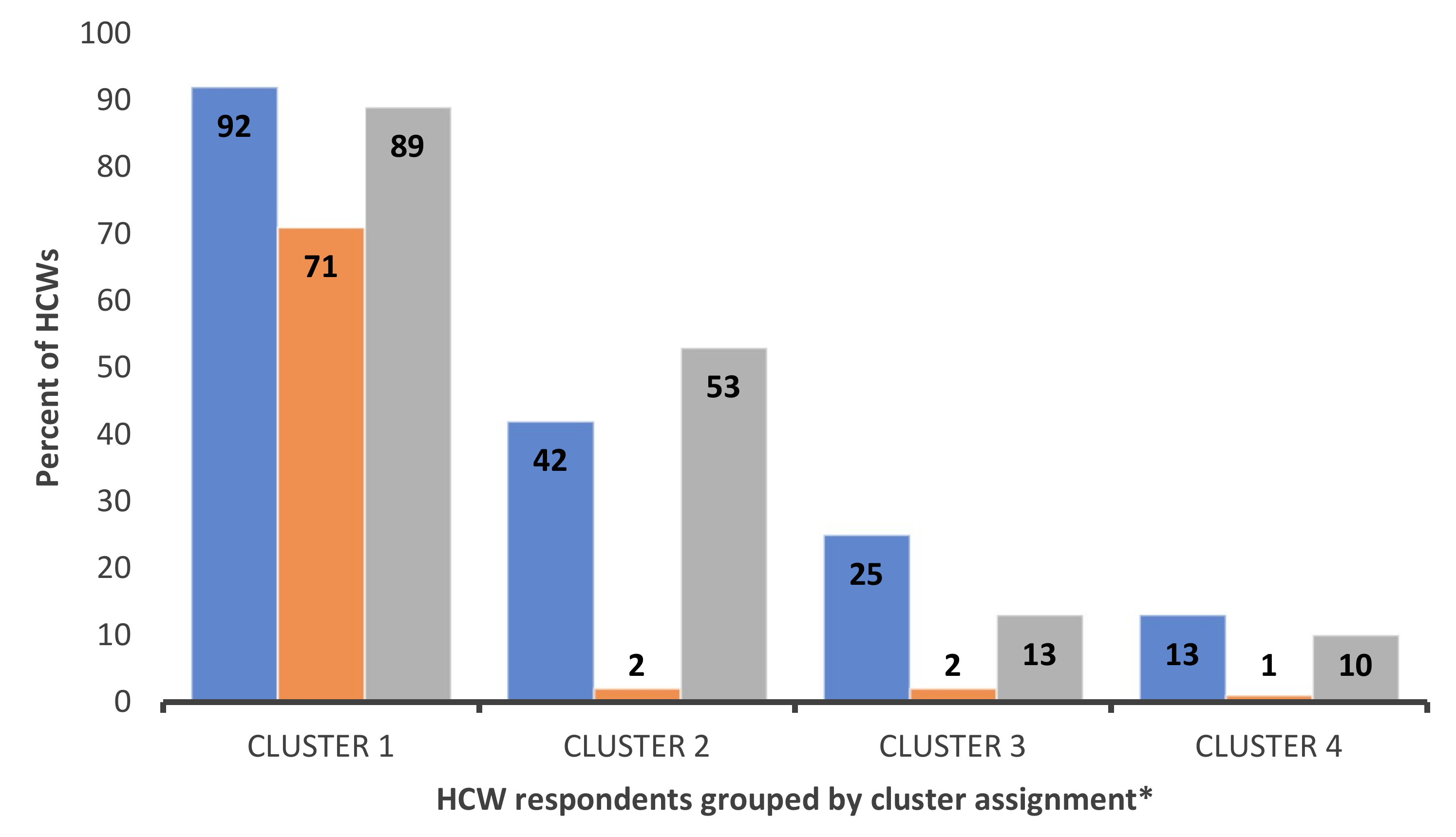
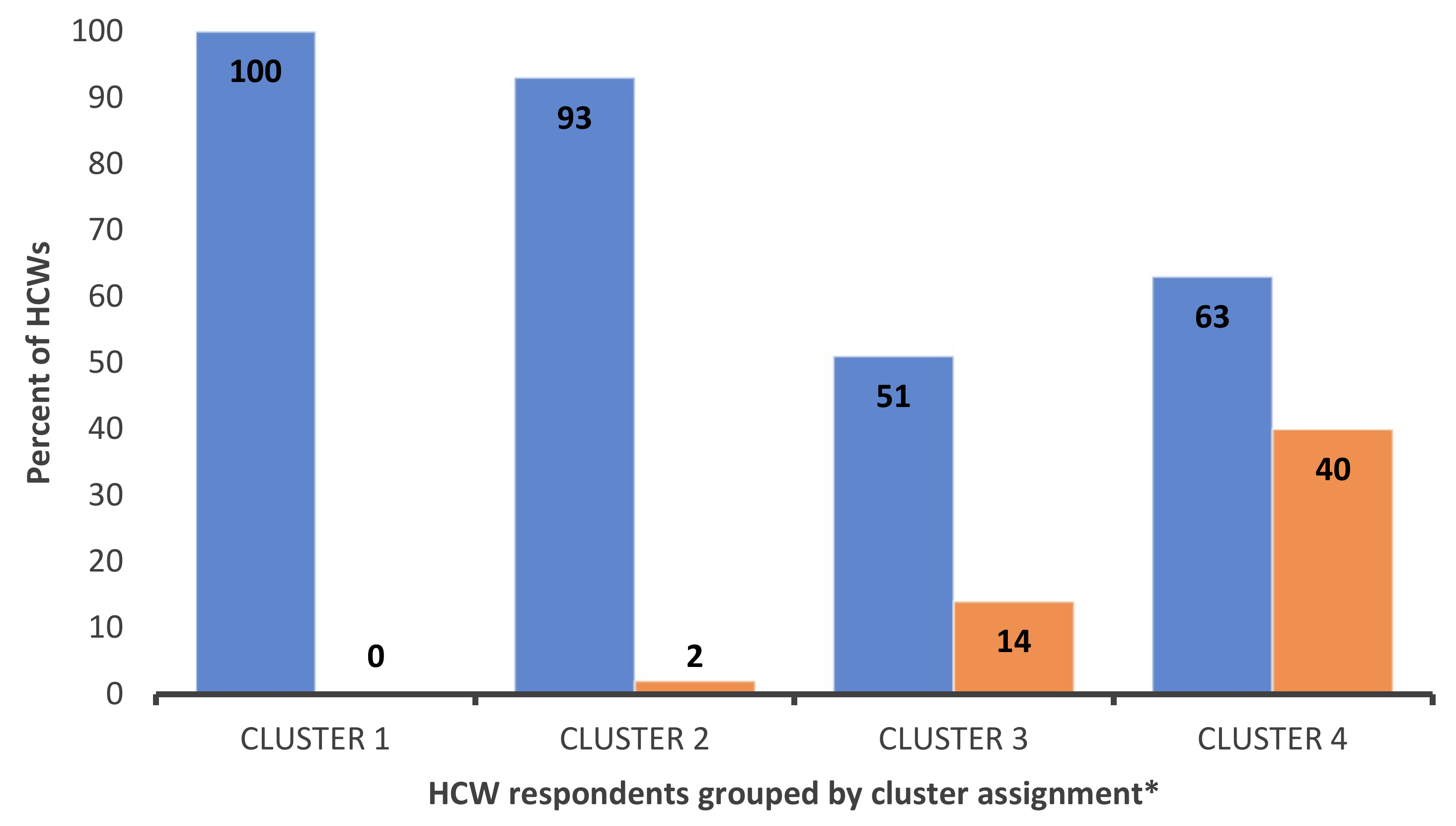
3.3. K-Means Cluster Analysis
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Coronavirus Disease 2019 (COVID-19) Situation Reports. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (accessed on 17 August 2021).
- Food and Drug Administration. COVID-19 Vaccines. Available online: https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/covid-19-vaccines (accessed on 17 August 2021).
- World Health Organization. Ten Threats to Global Health in 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 17 August 2021).
- Dror, A.A.; Eisenbach, N.; Taiber, S.; Morozov, N.G.; Mizrachi, M.; Zigron, A.; Srouji, S.; Sela, E. Vaccine hesitancy: The next challenge in the fight against COVID-19. Eur. J. Epidemiol. 2020, 35, 775–779. [Google Scholar] [CrossRef]
- Shekhar, R.; Sheikh, A.B.; Upadhyay, S.; Singh, M.; Kottewar, S.; Mir, H.; Barrett, E.; Pal, S. COVID-19 Vaccine Acceptance among Health Care Workers in the United States. Vaccines 2021, 9, 119. [Google Scholar] [CrossRef]
- Fontanet, A.; Cauchemez, S. COVID-19 herd immunity: Where are we. Nat. Rev. Immunol. 2020, 20, 583–584. [Google Scholar] [CrossRef] [PubMed]
- Paterson, P.; Meurice, F.; Stanberry, L.R.; Glismann, S.; Rosenthal, S.L.; Larson, H.J. Vaccine hesitancy and healthcare providers. Vaccine 2016, 34, 6700–6706. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jamieson, K.H.; Albarracin, D. The Relation between Media Consumption and Misinformation at the Outset of the SARS-CoV-2 Pandemic in the US. Harv. Kennedy Sch. Misinf. Rev. 2020. [Google Scholar] [CrossRef]
- Kirzinger, A.; Munana, C.; Brodie, M. Vaccine Hesitancy in Rural America. Available online: https://www.kff.org/coronaviruscovid-19/poll-finding/vaccine-hesitancy-in-rural-america/ (accessed on 17 August 2021).
- Li, M.; Luo, Y.; Watson, R.; Zheng, Y.; Ren, J.; Tang, J.; Chen, Y. Healthcare workers’ (HCWs) attitudes and related factors towards COVID-19 vaccination: A rapid systematic review. Postgrad. Med. J. 2021. [Google Scholar] [CrossRef]
- Biswas, N.; Mustapha, T.; Khubchandani, J.; Price, J.H. The Nature and Extent of COVID-19 Vaccination Hesitancy in Healthcare Workers. J. Community Health 2021, 46, 1244–1251. [Google Scholar] [CrossRef]
- American Medical Association. AMA Survey Shows Over 96% of Doctors Fully Vaccinated against COVID-19. Available online: www.ama-assn.org/press-center/press-releases/ama-survey-shows-over-96-doctors-fully-vaccinated-against-covid-19 (accessed on 17 August 2021).
- Gharpure, R.; Guo, A.; Bishnoi, C.K.; Patel, U.; Gifford, D.; Tippins, A.; Jaffe, A.; Shulman, E.; Stone, N.; Mungai, E.; et al. Early COVID-19 First-Dose Vaccination Coverage among Residents and Staff Members of Skilled Nursing Facilities Participating in the Pharmacy Partnership for Long-Term Care Program-United States, December 2020–January 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 178–182. [Google Scholar] [CrossRef]
- Gilboa, M.; Tal, I.; Levin, E.G.; Segal, S.; Belkin, A.; Zilberman-Daniels, T.; Biber, A.; Rubin, C.; Rahav, G.; Regev-Yochay, G. Coronavirus disease 2019 (COVID-19) vaccination uptake among healthcare workers. Infect. Control Hosp. Epidemiol. 2021, 46, 1–6. [Google Scholar] [CrossRef]
- Burden, S.; Henshall, C.; Oshikanlu, R. Harnessing the nursing contribution to COVID-19 mass vaccination programmes: Addressing hesitancy and promoting confidence. J. Adv. Nurs. 2021, 77, e16–e20. [Google Scholar] [CrossRef]
- SteelFisher, G.K.; Blendon, R.J.; Caporello, H. An Uncertain Public-Encouraging Acceptance of Covid-19 Vaccines. N. Engl. J. Med. 2021, 384, 1483–1487. [Google Scholar] [CrossRef] [PubMed]
- Tabachnick, B.G.; Fiddell, L.S. Using Multivariate Statistics, 7th ed.; Pearson: New York, NY, USA, 2007; Volume 5, pp. 481–498. ISBN 978-0134790541. [Google Scholar]
- Milligan, G.W. A Monte-Carlo study of 30 internal criterion measures for cluster-analysis. Psychometrika 1981, 46, 187–195. [Google Scholar] [CrossRef]
- Krolak-Schwedt, S.; Eckes, T. A Graph Theoretic Criterion for Determining the Number of Clusters in a Data Set. Multivar. Behav. Res. 1992, 27, 541–565. [Google Scholar] [CrossRef]
- Milligan, G.W.; Cooper, M.C. An examination of procedures for determining the number of clusters in a data set. Psychometrika 1985, 50, 159–179. [Google Scholar] [CrossRef]
- Ciardi, F.; Menon, V.; Jensen, J.L.; Shariff, M.A.; Pillai, A.; Venugopal, U.; Kasubhai, M.; Dimitrov, V.; Kanna, B.; Poole, B.D. Knowledge, Attitudes and Perceptions of COVID-19 Vaccination among Healthcare Workers of an Inner-City Hospital in New York. Vaccines 2021, 9, 516. [Google Scholar] [CrossRef]
- Grochowska, M.; Ratajczak, A.; Zdunek, G.; Adamiec, A.; Waszkiewicz, P.; Feleszko, W. A Comparison of the Level of Acceptance and Hesitancy towards the Influenza Vaccine and the Forthcoming COVID-19 Vaccine in the Medical Community. Vaccines 2021, 9, 475. [Google Scholar] [CrossRef] [PubMed]
- Gadoth, A.; Halbrook, M.; Martin-Blais, R.; Gray, A.; Tobin, N.H.; Ferbas, K.G.; Aldrovandi, G.M.; Rimoin, A.W. Cross-sectional Assessment of COVID-19 Vaccine Acceptance Among Health Care Workers in Los Angeles. Ann. Intern. Med. 2021, 174, 882–885. [Google Scholar] [CrossRef] [PubMed]
- Oliver, K.; Raut, A.; Pierre, S.; Silvera, L.; Boulos, A.; Gale, A.; Baum, A.; Chory, A.; Davis, N.; D’Souza, D.; et al. Factors associated with COVID-19 vaccine receipt at two integrated healthcare systems in New York City: A Cross sectional study of healthcare workers. medRxiv 2021. [Google Scholar] [CrossRef]
- Milligan, M.A.; Hoyt, D.L.; Gold, A.K.; Hiserodt, M.; Otto, M.W. COVID-19 vaccine acceptance: Influential roles of political party and religiosity. Psychol. Health Med. 2021, 46, 1–11. [Google Scholar] [CrossRef]
- Weisel, O. Vaccination as a social contract: The case of COVID-19 and US political partisanship. Proc. Natl. Acad. Sci. USA 2021, 118, e2026745118. [Google Scholar] [CrossRef]
- Ruiz, J.B.; Bell, R.A. Predictors of intention to vaccinate against COVID-19: Results of a nationwide survey. Vaccine 2021, 39, 1080–1086. [Google Scholar] [CrossRef] [PubMed]
- Hudson, A.; Montelpare, W.J. Predictors of vaccine hesitancy: Implications for COVID-19 public health messaging. Int. J. Environ. Res. Public Health 2021, 18, 8054. [Google Scholar] [CrossRef]
- Fisher, K.A.; Bloomstone, S.J.; Walder, J.; Crawford, S.; Fouayzi, H.; Mazor, K.M. Attitudes Toward a Potential SARS-CoV-2 Vaccine: A Survey of U.S. Adults. Ann. Intern. Med. 2020, 173, 964–973. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Dobalian, A.; Ward, K.D. COVID-19 Vaccine Hesitancy and Its Determinants among Adults with a History of Tobacco or marijuana use. J. Community Health 2021, 46, 1090–1098. [Google Scholar] [CrossRef]
- Stolle, L.B.; Nalamasu, R.; Pergolizzi, J.V.; Varrassi, G.; Magnusson, P.; LeQuang, J.; Breve, F. Fact vs. fallacy: The anti-vaccine Discussion Reloaded. Adv. Ther. 2020, 37, 4481–4490. [Google Scholar] [CrossRef]
- Pan, W.; Liu, D.; Fang, J. An Examination of Factors Contributing to the Acceptance of Online Health Misinformation. Front. Psychol. 2021, 12, 524. [Google Scholar] [CrossRef]
- Moniz, M.H.; Townsel, C.; Wagner, A.L.; Zikmund-Fisher, B.J.; Hawley, S.; Jiang, C.; Stout, M.J. COVID-19 Vaccine Acceptance Among Healthcare Workers in a United States Medical Center. medRxiv 2021. [Google Scholar] [CrossRef]
- Ball, P.; Maxmen, A. The epic battle against coronavirus misinformation and conspiracy theories. Nature 2020, 581, 371–374. [Google Scholar] [CrossRef] [PubMed]
- Chou, W.S.; Budenz, A. Considering emotion in COVID-19 vaccine communication: Addressing vaccine hesitancy and fostering vaccine confidence. Health Commun. 2020, 35, 1718–1722. [Google Scholar] [CrossRef] [PubMed]
- Latkin, C.; Dayton, L.A.; Yi, G.; Konstantopoulos, A.; Park, J.; Maulsby, C.; Kong, X. COVID-19 vaccine intentions in the United States, a social-ecological framework. Vaccine 2021, 39, 2288–2294. [Google Scholar] [CrossRef]
- Islam, M.S.; Kamal, A.M.; Kabir, A.; Southern, D.L.; Khan, S.H.; Hasan, S.M.M.; Sarkar, T.; Sharmin, S.; Das, S.; Roy, T.; et al. COVID-19 vaccine rumors and conspiracy theories: The need for cognitive inoculation against misinformation to improve vaccine adherence. PLoS ONE 2021, 16, e0251605. [Google Scholar] [CrossRef] [PubMed]
- Klompas, M.; Pearson, M.; Morris, C. The Case for Mandating COVID-19 Vaccines for Health Care Workers. Ann. Intern. Med. 2021, 174, 1305–1307. [Google Scholar] [CrossRef] [PubMed]
- Dzieciolowska, S.; Hamel, D.; Gadio, S.; Dionne, M.; Gagnon, D.; Robitaille, L.; Cook, E.; Caron, I.; Talib, A.; Parkes, L.; et al. Covid-19 vaccine acceptance, hesitancy, and refusal among Canadian healthcare workers: A multicenter survey. Am. J. Infect. Control. 2021, 49, 1152–1157. [Google Scholar] [CrossRef] [PubMed]
- Palm, R.; Bolsen, T.; Kingsland, J.T. The Effect of Frames on COVID-19 Vaccine Resistance. Front. Political Sci. 2021, 3, 41. [Google Scholar] [CrossRef]
- Korn, L.; Böhm, R.; Meier, N.W.; Betsch, C. Vaccination as a social contract. Proc. Natl. Acad. Sci. USA 2020, 117, 14890–14899. [Google Scholar] [CrossRef]
- Bruine de Bruin, W.; Parker, A.M.; Galesic, M.; Vardavas, R. Reports of social circles’ and own vaccination behavior: A national longitudinal survey. Health Psychol. 2019, 38, 975–983. [Google Scholar] [CrossRef] [Green Version]
- Allen, J.D.; Mohllajee, A.P.; Shelton, R.C.; Othus, M.K.; Fontenot, H.B.; Hanna, R. Stage of adoption of the human papillomavirus vaccine among college women. Prev. Med. 2009, 48, 420–425. [Google Scholar] [CrossRef]
- Centers for Disease Control. Building Confidence in COVID-19 Vaccines Among Your Patients. Available online: https://www.cdc.gov/vaccines/covid-19/downloads/VaccinateWConfidence-TipsForHCTeams_508.pptx (accessed on 17 August 2021).
- World Health Organization. Conversations to Build Trust in Vaccination. A Training Module. Available online: https://www.who.int/immunization/programmes_systems/TrainingModule_ConversationGuide_final.pptx?ua=1 (accessed on 17 August 2021).
- Pennycook, G.; McPhetres, J.; Zhang, Y.; Lu, J.G.; Rand, D.G. Fighting COVID-19 Misinformation on Social Media: Experimental Evidence for a Scalable Accuracy-Nudge Intervention. Psychol. Sci. 2020, 31, 770–780. [Google Scholar] [CrossRef]
- Chevallier, C.; Hacquin, A.S.; Mercier, H. COVID-19 Vaccine Hesitancy: Shortening the Last Mile. Trends Cogn. Sci. 2021, 25, 331–333. [Google Scholar] [CrossRef]
- Strickland, J.C.; Reed, D.D.; Hursh, S.R.; Schwartz, L.P.; Foster, R.N.S.; Gelino, B.W.; Le Comte, R.S.; Oda, F.S.; Salzer, A.R.; Latkin, C.; et al. Integrating Operant and Cognitive Behavioral Economics to Inform Infectious Disease Response: Prevention, Testing, and Vaccination in the COVID-19 Pandemic. medRxiv 2021. [Google Scholar] [CrossRef]
- Rutten, L.J.F.; Zhu, X.; Leppin, A.L.; Ridgeway, J.L.; Swift, M.D.; Griffin, J.M.; St Sauver, J.L.; Virk, A.; Jacobson, R.M. Evidence-Based Strategies for Clinical Organizations to Address COVID-19 Vaccine Hesitancy. Mayo Clin. Proc. 2021, 96, 699–707. [Google Scholar] [CrossRef] [PubMed]
- Hamel, L.; Lopes, L.; Kearney, A.; Sparks, G.; Stokes, M.; Brodie, M. KFF COVID-19 Vaccine Monitor. Available online: https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-june-2021/ (accessed on 17 August 2021).
- Paul, E.; Steptoe, A.; Fancourt, D. Attitudes towards vaccines and intention to vaccinate against COVID-19: Implications for public health communications. Lancet Reg. Health Eur. 2021, 1, 100012. [Google Scholar] [CrossRef] [PubMed]
| Number of Clusters | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|
| Variance ratio value | 2.8167 | 4.7548 | 4.2031 | 3.8492 | 2.9618 |
| N (%) | |
|---|---|
| Gender | |
| Male | 618 (24.81) |
| Female | 1.867 (74.95) |
| Other/non-binary | 6 (0.24) |
| Age | |
| 1946–1964 | 615 (24.94) |
| 1965–1980 | 800 (32.44) |
| 1981–1996 | 998 (40.47) |
| After 1996 | 53 (2.15) |
| Race | |
| White | 1.815 (72.86) |
| Black or African American | 123 (4.94) |
| Asian American | 438 (17.58) |
| Pacific Islander | 47 (1.89) |
| Native American | 68 (2.73) |
| Ethnicity | |
| Hispanic/Latinx | 570 (22.88) |
| Non-Hispanic/Latinx | 1.921 (77.12) |
| Education | |
| Some college | 326 (13.09) |
| Associate degree | 319 (12.18) |
| Bachelor’s degree | 823 (33.05) |
| Graduate degree | 397 (15.94) |
| Doctoral degree | 525 (25.10) |
| Household income level | |
| Less than USD 50,000 | 124 (4.98) |
| USD 50,000–100,000 | 526 (21.12) |
| USD 101,000–150,000 | 624 (25.05) |
| USD 150,000–200,000 | 405 (16.26) |
| USD 201,000–250,000 | 261 (10.48) |
| Greater than USD 250,000 | 365 (14.65) |
| Decline to respond | 186 (7.47) |
| Political Affiliation | |
| Democrat/lean Democrat | 1.158 (46.49) |
| Republican/lean Republican | 743 (29.83) |
| No lean | 590 (23.69) |
| Occupation | |
| Physician | 473 (18.99) |
| Attending | 348 (13.97) |
| Resident | 108 (4.34) |
| Fellow | 17 (0.68) |
| Nurse | 869 (34.89) |
| Nurse practitioner/Physician Assistant | 83 (3.33) |
| Pharmacist | 61 (2.45) |
| Respiratory Therapist | 91 (3.65) |
| Administrator | 176 (7.07) |
| Patient care assistant | 738 (29.63) |
| Clinical area | |
| ICU | 604 (24.25) |
| Non-ICU | 853 (34.24) |
| Emergency Department | 177 (7.11) |
| Outpatient | 808 (32.44) |
| Clinical Specialty | |
| Critical care | 187 (7.51) |
| Adult | 104 (4.18) |
| Pediatric | 83 (3.33) |
| General Medicine | 486 (19.51) |
| Adult | 375 (15.05) |
| Pediatric | 111 (4.46) |
| Subspecialty | 975 (39.14) |
| Adult | 744 (29.87) |
| Pediatric | 231 (9.27) |
| Surgery | 310 (12.44) |
| Emergency | 163 (6.54) |
| Not medical | 370 (14.85) |
| Contact with COVID-19 patients | |
| Frequent * | 698 (28.02) |
| Intermittent ** | 838 (33.64) |
| No contact | 955 (38.34) |
| Recent flu vaccination | |
| Yes | 2.285 (91.73) |
| No | 206 (8.27) |
| Vaccinated | Hesitant | Not Vaccinated | ||||
|---|---|---|---|---|---|---|
| Mean or % | SE | Mean or % | SE | Mean or % | SE | |
| Male | 91.10% | 6.10% | 2.80% | |||
| Latinx | 83.20% | 11.40% | 5.40% | |||
| Black | 74.80% | 17.90% | 7.30% | |||
| Asian | 93.20% | 5.70% | 1.10% | |||
| Age | ||||||
| <25 years | 77.40% | 20.80% | 1.90% | |||
| 25–40 years | 81.90% | 11.90% | 6.20% | |||
| 41–55 years | 87.00% | 8.90% | 4.20% | |||
| 56–75 years | 91.50% | 4.60% | 3.90% | |||
| Education Level | ||||||
| Some College | 85.30% | 8.60% | 6.10% | |||
| Associate Degree | 80.60% | 12.20% | 7.20% | |||
| Bachelor’s Degree | 81.90% | 12.40% | 5.70% | |||
| Graduate Degree | 85.90% | 9.60% | 4.50% | |||
| Doctorate Degree | 94.40% | 3.70% | 1.90% | |||
| Chronic Illness | 87.80% | 8.10% | 4.10% | |||
| Household Size | 2.94 | 0.03 | 3.31 | 0.08 | 3.33 | 0.12 |
| Income | ||||||
| <USD 50,000 | 86.30% | 9.70% | 4.00% | |||
| USD 50,000–100,000 | 81.60% | 12.70% | 5.70% | |||
| USD 101,000–150,000 | 84.00% | 11.10% | 5.00% | |||
| USD 151,000–200,000 | 86.40% | 9.10% | 4.40% | |||
| USD 201,000–250,000 | 87.40% | 8.00% | 4.60% | |||
| >USD 250,000 | 93.40% | 2.50% | 4.10% | |||
| Occupation | ||||||
| Nurse | 80.80% | 7.60% | 3.60% | |||
| Physician | 96.60% | 2.10% | 1.30% | |||
| NP/PA | 94.00% | 3.60% | 2.40% | |||
| Administration | 93.20% | 5.70% | 1.10% | |||
| Clinical area | ||||||
| Intensive Care Unit | 82.00% | 11.80% | 6.30% | |||
| Emergency Department | 84.70% | 11.30% | 4.00% | |||
| Outpatient | 90.60% | 5.80% | 3.60% | |||
| Specialty area | ||||||
| Adult Critical Care | 80.80% | 12.50% | 6.70% | |||
| Adult Specialty Care | 86.60% | 8.60% | 4.80% | |||
| Peds Critical Care | 80.70% | 9.60% | 9.60% | |||
| Peds Specialty Care | 80.50% | 13.00% | 6.50% | |||
| COVID conspiracies | ||||||
| COVID is manmade | 4.02 | 0.03 | 3 | 0.09 | 2.65 | 0.13 |
| COVID is a hoax | 4.85 | 0.02 | 4.53 | 0.06 | 4.16 | 0.12 |
| COVID impact is exaggerated | 4.61 | 0.02 | 3.84 | 0.09 | 2.99 | 0.13 |
| COVID vs. Flu | ||||||
| Flu is more contagious | 2.69 | 0.03 | 2.90 | 0.07 | 3.00 | 0.11 |
| History of Flu vaccine | 88.90% | 7.60% | 3.50% | |||
| Recent Flu vaccine | 89.70% | 7.50% | 2.80% | |||
| COVID impact | ||||||
| Financial impact | 82.90% | 10.90% | 6.20% | |||
| Someone close had COVID | 83.00% | 10.30% | 6.70% | |||
| Someone close was hospitalized | 85.30% | 9.90% | 4.80% | |||
| Someone close died | 88.60% | 8.20% | 3.10% | |||
| Estimated COVID mortality | ||||||
| Underestimate | 71.10% | 14.60% | 14.30% | |||
| Overestimate | 89.50% | 8.00% | 2.50% | |||
| Likelihood of dying from COVID | ||||||
| High | 73.40% | 15.70% | 11.00% | |||
| Low | 93.40% | 5.10% | 1.60% | |||
| COVID vaccine knowledge | ||||||
| Underestimate efficacy | 58.10% | 25.10% | 16.80% | |||
| Prior COVID diagnosis | ||||||
| Recovered from COVID | 71.60% | 20.20% | 8.30% | |||
| Contact with COVID patients | ||||||
| Frequent | 84.10% | 10.70% | 5.20% | |||
| Intermittent | 85.60% | 9.70% | 4.77% | |||
| No contact | 87.60% | 7.75% | 4.61% | |||
| Political party affiliation | ||||||
| Democratic | 93.90% | 4.50% | 1.60% | |||
| Republican | 78.60% | 13.20% | 8.20% | |||
| Social media use | ||||||
| Well connected | 3.86 | 0.02 | 3.73 | 0.07 | 3.83 | 0.1 |
| News sources | ||||||
| Cable news | 87.90% | 8.00% | 4.10% | |||
| Mainstream news | 91.10% | 5.70% | 3.20% | |||
| Social media | 85.70% | 10.20% | 4.10% | |||
| Family or friends | 73.00% | 19.70% | 7.40% | |||
| Not Vaccinated | Hesitant | |||||
|---|---|---|---|---|---|---|
| aOR [95% CI] | B | p-Value | aOR [95% CI] | B | p-Value | |
| Demographics | ||||||
| Male | 0.66 [0.32,1.37] | −0.41 | 0.240 | 0.91 [0.57,1.45] | −0.09 | 0.701 |
| Latinx | 0.58 [0.30,1.10] | −0.55 | 0.100 | 0.75 [0.49,1.12] | 0.75 | 0.194 |
| Black | 1.07 [0.42,2.71] | 0.07 | 0.740 | 1.6 [0.85,3.02] | 1.6 | 0.149 |
| Asian | 0.10 [0.03,0.31] | −2.28 | <0.001 | 0.44 [0.25,0.75] | 0.44 | <0.001 |
| Age | 1.55 [1.08,2.22] | 0.43 | 0.010 | 1.83 [1.42,2.36] | 1.83 | <0.001 |
| Education level | 1.02 [0.77,1.36] | 0.02 | 0.810 | 1.33 [1.11,1.59] | 1.33 | <0.001 |
| Chronic illness | 1.60 [0.89,2.85] | 0.47 | 0.120 | 1.44 [0.98,2.14] | 1.44 | 0.070 |
| Household size | 1.17 [0.95,1.44] | 0.16 | 0.100 | 1.19 [1.04,1.37] | 1.19 | 0.013 |
| Income | 1.04 [0.89,1.22] | 0.04 | 0.590 | 0.89 [0.80,0.99] | 0.89 | 0.045 |
| Occupation | ||||||
| Nurse | 1.54 [0.85,2.70] | 0.43 | 0.150 | 1.03 [0.70,1.54] | 0.03 | 0.867 |
| Physician | 1.14 [0.31,4.15] | 0.13 | 0.810 | 0.29 [0.12,0.67] | −1.25 | 0.004 |
| NP/PA | 0.78 [0.12,4.82] | −0.26 | 0.730 | 0.3 [0.08,1.14] | −1.21 | 0.077 |
| Administration | 0.35 [0.07,1.81] | −1.06 | 0.170 | 0.65 [0.30,1.44] | −0.43 | 0.287 |
| Clinical area | ||||||
| Intensive Care Unit | 0.87 [0.42,1.80] | −0.14 | 0.600 | 0.92 [0.57,1.48] | −0.09 | 0.725 |
| Emergency Department | 1.11 [0.19,6.50] | 0.1 | 0.830 | 0.63 [0.20,2.04] | −0.46 | 0.442 |
| Outpatient | 0.42 [0.21,0.83] | −0.87 | 0.009 | 0.5 [0.31,0.79] | −0.70 | <0.001 |
| Specialty area | ||||||
| Adult Critical Care | 0.73 [0.21,2.50] | −0.32 | 0.610 | 0.78 [0.34,1.81] | −0.24 | 0.569 |
| Adult Specialty Care | 0.98 [0.52,1.85] | −0.02 | 0.960 | 1 [0.65,1.55] | 0.01 | 0.976 |
| Peds Critical Care | 1.21 [0.34,4.37] | 0.19 | 0.770 | 0.76 [0.29,1.98] | −0.28 | 0.570 |
| Peds Specialty Care | 0.92 [0.37,2.33] | −0.08 | 0.870 | 1.18 [0.64,2.17] | 0.17 | 0.591 |
| COVID conspiracies | ||||||
| COVID is manmade | 1.37 [1.12,1.68] | 0.32 | 0.002 | [1.19,1.55] | 0.31 | <0.001 |
| COVID is a hoax | 0.82 [0.62,1.10] | −0.19 | 0.195 | [0.68,1.10] | −0.14 | 0.235 |
| COVID impact is exaggerated | 1.66 [1.33,2.01] | 0.51 | <0.001 | [1.01,1.41] | 0.17 | 0.043 |
| COVID vs. Flu | ||||||
| Flu is more contagious | 0.68 [0.52,0.89] | −0.40 | 0.005 | 0.91 [0.76,1.08] | −0.10 | 0.261 |
| History of Flu vaccine | 0.47 [0.23,0.93] | −0.77 | 0.032 | 0.33 [0.20,0.55] | −1.12 | <0.001 |
| Recent Flu vaccine | 0.09 [0.04,0.17] | −2.47 | <0.001 | 0.29 [0.17,0.50] | −1.23 | <0.001 |
| COVID impact | ||||||
| Financial impact | 1.66 [1.00,2.76] | 0.51 | 0.05 | 1.29 [0.91,1.81] | 0.25 | 0.148 |
| Someone close had COVID | 1.83 [0.27,12.4] | 0.6 | 0.537 | 6.4 [0.74,55.01] | 1.86 | 0.09 |
| Someone close was hospitalized | 1.49 [0.21,10.6] | 0.4 | 0.691 | 5.68 [0.65,49.77] | 1.74 | 0.116 |
| Someone close died | 1.18 [0.17,8.14] | 0.17 | 0.867 | 4.74 [0.55,40.88] | 1.56 | 0.157 |
| Estimated COVID mortality | ||||||
| Underestimate | 1.10 [0.56,2.17] | 0.09 | 0.782 | 0.97 [0.56,2.17] | −0.03 | 0.915 |
| Overestimate | 1.34 [0.67,2.68] | 0.29 | 0.415 | 1.34 [0.67,2.68] | 0.29 | 0.188 |
| Likelihood of dying from COVID | ||||||
| High | 2.91 [1.57,5.37] | −1.07 | <0.001 | 2.3 [1.52,3.48] | −0.83 | <0.001 |
| Low | 0.56 [0.22,1.45] | −0.58 | 0.230 | 0.61 [0.36,1.05] | −0.49 | 0.077 |
| COVID vaccine knowledge | ||||||
| Underestimate efficacy | 13.9 [7.92,24.4] | 2.63 | <0.001 | 7.08 [4.85,10.35] | 1.96 | <0.001 |
| Prior COVID diagnosis | ||||||
| Recovered from COVID | 1.88 [1.01,3.52] | 0.63 | 0.047 | 2.58 [1.73,3.85] | 0.95 | <0.001 |
| Contact with COVID patients | ||||||
| Frequent | 1 [0.71,1.44] | 0.01 | 0.961 | 1.04 [0.82,1.33] | 0.04 | 0.735 |
| Political party affiliation | ||||||
| Democratic | 0.45 [0.22,0.95] | −0.79 | 0.035 | 0.47 [0.29,0.75] | −0.76 | 0.002 |
| Republican | 1.34 [0.72,2.47] | 0.29 | 0.354 | 1.19 [0.77,1.83] | 0.17 | 0.429 |
| Social media use | ||||||
| Well connected | 1 [0.78,1.30] | 0.01 | 0.977 | 0.85 [0.72,1.01] | −0.16 | 0.061 |
| News sources | ||||||
| Cable news | 1.39 [0.67,2.87] | 0.33 | 0.380 | 1.14 [0.69,1.89] | 0.14 | 0.598 |
| Mainstream news | 1.77 [0.76,4.13] | 0.57 | 0.184 | 1.29 [0.72,2.28] | 0.25 | 0.392 |
| Social media | 0.50 [0.19,1.31] | −0.69 | 0.159 | 0.72 [0.39,1.32] | −0.33 | 0.287 |
| Family or friends | 0.69 [0.24,1.96] | −0.38 | 0.481 | 1.09 [0.55,2.20] | 0.09 | 0.800 |
| Total (n = 304) | Group 1 (n = 38) | Group 2 (n = 94) | Group 3 (n = 86) | Group 4 (n = 86) | |
|---|---|---|---|---|---|
| Gender | |||||
| Male | 53 (17) | 10 (27) | 14 (15) | 16 (19) | 13 (15) |
| Female | 251 (83) | 28 (73) | 80 (85) | 70 (81) | 73 (85) |
| Age | |||||
| 1946–1964 | 50 (16) | 16 (42) | 18 (19) | 9 (10) | 7 (8) |
| 1965–1980 | 87 (29) | 10 (26) | 29 (31) | 28 (33) | 20 (23) |
| 1981–1996 | 155 (51) | 11 (29) | 46 (49) | 46 (53) | 52 (61) |
| After 1996 | 12 (4) | 1 (3) | 1 (1) | 3 (4) | 7 (8) |
| Race | |||||
| White | 242 (80) | 29 (77) | 76 (81) | 72 (84) | 65 (75) |
| African American | 27 (9) | 2 (5) | 8 (9) | 6 (7) | 11 (13) |
| Asian American | 19 (6) | 4 (10) | 5 (5) | 6 (7) | 4 (5) |
| Pacific Islander | 4 (1) | 0 (0) | 1 (1) | 1 (1) | 2 (2) |
| Native American | 12 (4) | 3 (8) | 4 (4) | 1 (1) | 4 (5) |
| Ethnicity | |||||
| Hispanic | 98 (32) | 13 (34) | 44 (47) | 21 (24) | 20 (23) |
| Non-Hispanic | 206 (68) | 25 (66) | 50 (53) | 65 (76) | 66 (77) |
| Education | |||||
| Some college | 40 (13) | 3 (8) | 28 (30) | 7 (8) | 2 (2) |
| Associate degree | 56 (18) | 4 (10) | 28 (30) | 16 (19) | 9 (10) |
| Bachelor’s degree | 128 (42) | 15 (39) | 31 (33) | 46 (53) | 36 (42) |
| Graduate degree | 48 (16) | 9 (24) | 5 (5) | 10 (12) | 24 (28) |
| Doctoral degree | 31 (10) | 7 (18) | 2 (2) | 7 (8) | 15 (17) |
| Political Affiliation | |||||
| Democratic | 54 (18) | 2 (5) | 8 (9) | 6 (7) | 38 (44) |
| Republican | 155 (51) | 26 (68) | 44 (47) | 52 (60) | 33 (38) |
| No lean | 95 (31) | 10 (27) | 42 (44) | 28 (33) | 15 (18) |
| Occupation | |||||
| Physician | 11 (4) | 2 (5) | 0 (0) | 2 (2) | 7 (8) |
| Nurse | 144 (47) | 20 (54) | 31 (33) | 49 (57) | 44 (51) |
| NP/PA | 5 (2) | 2 (5) | 0 (0) | 1 (1) | 2 (2) |
| Pharmacist | 4 (1) | 0 (0) | 1 (1) | 0 (0) | 3 (3) |
| CRT/RRT | 23 (7) | 2 (5) | 5 (5) | 14 (16) | 2 (2) |
| Administrator | 11 (4) | 5 (13) | 1 (1) | 3 (3) | 2 (2) |
| Allied health | 106 (35) | 7 (18) | 56 (60) | 17 (20) | 26 (30) |
| Clinical Area | |||||
| ICU | 95 (32) | 14 (37) | 20 (21) | 43 (51) | 18 (21) |
| Non-ICU | 116 (38) | 10 (27) | 41 (44) | 25 (29) | 40 (47) |
| Emergency room | 25 (8) | 5 (13) | 2 (2) | 9 (10) | 9 (10) |
| Outpatient | 68 (22) | 9 (23) | 31 (33) | 9 (10) | 19 (22) |
| Willingness to receive COVID-19 vaccine | |||||
| Definitely not | 121 (40) | 26 (69) | 56 (60) | 17 (20) | 22 (26) |
| Probably not | 102 (33) | 12 (31) | 31 (33) | 27 (31) | 32 (37) |
| Not sure | 81 (27) | 0 (0) | 7 (7) | 42 (49) | 32 (37) |
| Willingness to recommend COVID-19 vaccine | |||||
| Definitely not | 55 (18) | 22 (58) | 24 (25) | 8 (9) | 1 (1) |
| Probably not | 98 (32) | 14 (37) | 41 (44) | 25 (29) | 18 (21) |
| Not sure | 103 (39) | 2 (5) | 27 (29) | 41 (48) | 33 (38) |
| Probably yes | 35 (11) | 0 (0) | 2 (2) | 7 (8) | 26 (31) |
| Definitely yes | 13 (4) | 0 (0) | 0 (0) | 5 (6) | 8 (9) |
| Knowledge of COVID-19 vaccine efficacy | |||||
| Accurate | 119 (39) | 6 (16) | 24 (25) | 40 (47) | 49 (57) |
| Underestimate | 185 (61) | 32 (84) | 70 (75) | 46 (53) | 37 (43) |
| Recent Flu vaccination receipt | |||||
| Yes | 195 (64) | 12 (41) | 62 (66) | 53 (61) | 68 (79) |
| No | 109 (36) | 26 (59) | 32 (34) | 33 (39) | 18 (21) |
| Perceived likelihood of dying from COVID-19 | |||||
| Low | 261 (86) | 33 (87) | 90 (96) | 63 (73) | 75 (87) |
| Average | 21 (7) | 3 (8) | 2 (2) | 12 (14) | 4 (5) |
| High | 22 (7) | 2 (5) | 2 (2) | 11 (13) | 7 (8) |
| Estimated mortality from COVID-19 | |||||
| Underestimate | 137 (45) | 29 (76) | 55 (58) | 31 (36) | 22 (26) |
| Accurate | 119 (39) | 8 (21) | 29 (31) | 38 (44) | 44 (51) |
| High | 48 (16) | 1 (3) | 10 (11) | 17 (20) | 20 (23) |
| Seasonal flu is more contagious than COVID-19 | |||||
| Yes | 68 (22) | 30 (79) | 18 (19) | 12 (14) | 8 (9) |
| No | 93 (31) | 2 (5) | 19 (20) | 31 (36) | 41 (48) |
| Not sure | 142 (47) | 6 (16) | 57 (61) | 43 (50) | 37 (43) |
| Seasonal flu is deadlier than COVID-19 | |||||
| Yes | 48 (16) | 24 (63) | 15 (16) | 5 (6) | 4 (5) |
| No | 136 (45) | 4 (10) | 19 (20) | 66 (77) | 47 (55) |
| Not sure | 120 (39) | 10 (26) | 60 (64) | 15 (17) | 35 (40) |
| COVID-19 is a manmade virus | |||||
| Yes | 108 (35) | 35 (92) | 40 (42) | 22 (25) | 11 (13) |
| No | 94 (31) | 2 (5) | 17 (18) | 13 (15) | 62 (72) |
| Not sure | 102 (34) | 1 (3) | 37 (40) | 51 (60) | 13 (15) |
| COVID-19 is a hoax | |||||
| Yes | 32 (10) | 27 (71) | 2 (2) | 2 (2) | 1 (1) |
| No | 238 (78) | 5 (13) | 69 (73) | 79 (92) | 85 (99) |
| Not sure | 33 (11) | 6 (16) | 22 (25) | 5 (6) | 0 (0) |
| The impact of COVID-19 is exaggerated | |||||
| Yes | 104 (33) | 34 (89) | 50 (53) | 11 (13) | 9 (10) |
| No | 153 (50) | 1 (3) | 24 (25) | 60 (70) | 68 (80) |
| Not sure | 47 (15) | 3 (8) | 20 (22) | 15 (17) | 9 (10) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dubov, A.; Distelberg, B.J.; Abdul-Mutakabbir, J.C.; Beeson, W.L.; Loo, L.K.; Montgomery, S.B.; Oyoyo, U.E.; Patel, P.; Peteet, B.; Shoptaw, S.; et al. Predictors of COVID-19 Vaccine Acceptance and Hesitancy among Healthcare Workers in Southern California: Not Just “Anti” vs. “Pro” Vaccine. Vaccines 2021, 9, 1428. https://doi.org/10.3390/vaccines9121428
Dubov A, Distelberg BJ, Abdul-Mutakabbir JC, Beeson WL, Loo LK, Montgomery SB, Oyoyo UE, Patel P, Peteet B, Shoptaw S, et al. Predictors of COVID-19 Vaccine Acceptance and Hesitancy among Healthcare Workers in Southern California: Not Just “Anti” vs. “Pro” Vaccine. Vaccines. 2021; 9(12):1428. https://doi.org/10.3390/vaccines9121428
Chicago/Turabian StyleDubov, Alex, Brian J. Distelberg, Jacinda C. Abdul-Mutakabbir, W. Lawrence Beeson, Lawrence K. Loo, Susanne B. Montgomery, Udochukwu E. Oyoyo, Pranjal Patel, Bridgette Peteet, Steven Shoptaw, and et al. 2021. "Predictors of COVID-19 Vaccine Acceptance and Hesitancy among Healthcare Workers in Southern California: Not Just “Anti” vs. “Pro” Vaccine" Vaccines 9, no. 12: 1428. https://doi.org/10.3390/vaccines9121428
APA StyleDubov, A., Distelberg, B. J., Abdul-Mutakabbir, J. C., Beeson, W. L., Loo, L. K., Montgomery, S. B., Oyoyo, U. E., Patel, P., Peteet, B., Shoptaw, S., Tavakoli, S., & Chrissian, A. A. (2021). Predictors of COVID-19 Vaccine Acceptance and Hesitancy among Healthcare Workers in Southern California: Not Just “Anti” vs. “Pro” Vaccine. Vaccines, 9(12), 1428. https://doi.org/10.3390/vaccines9121428







