Opposing Mechanisms Involving Perceived Benefits versus Safety Partially Explained an Increase in COVID-19 Vaccination Intention among Unvaccinated Chinese Adults during a Post-Rollout Period: Results of Two Serial Surveys
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Data Collection
2.2. Measures
2.2.1. Background Factors
2.2.2. Behavioral Intention of COVID-19 Vaccination
2.2.3. Perceived Benefits and Severe Side Effects of COVID-19 Vaccination
2.3. Data Analysis
3. Results
3.1. Comparing the Two Sample’s Characteristics
3.2. Associations between Background Factors/Perceptions Related to Vaccination and Vaccination Intention
3.3. Testing the Differences in Two Surveys’ Prevalence of Vaccination Intention and Levels of Perceptions Related to Vaccination
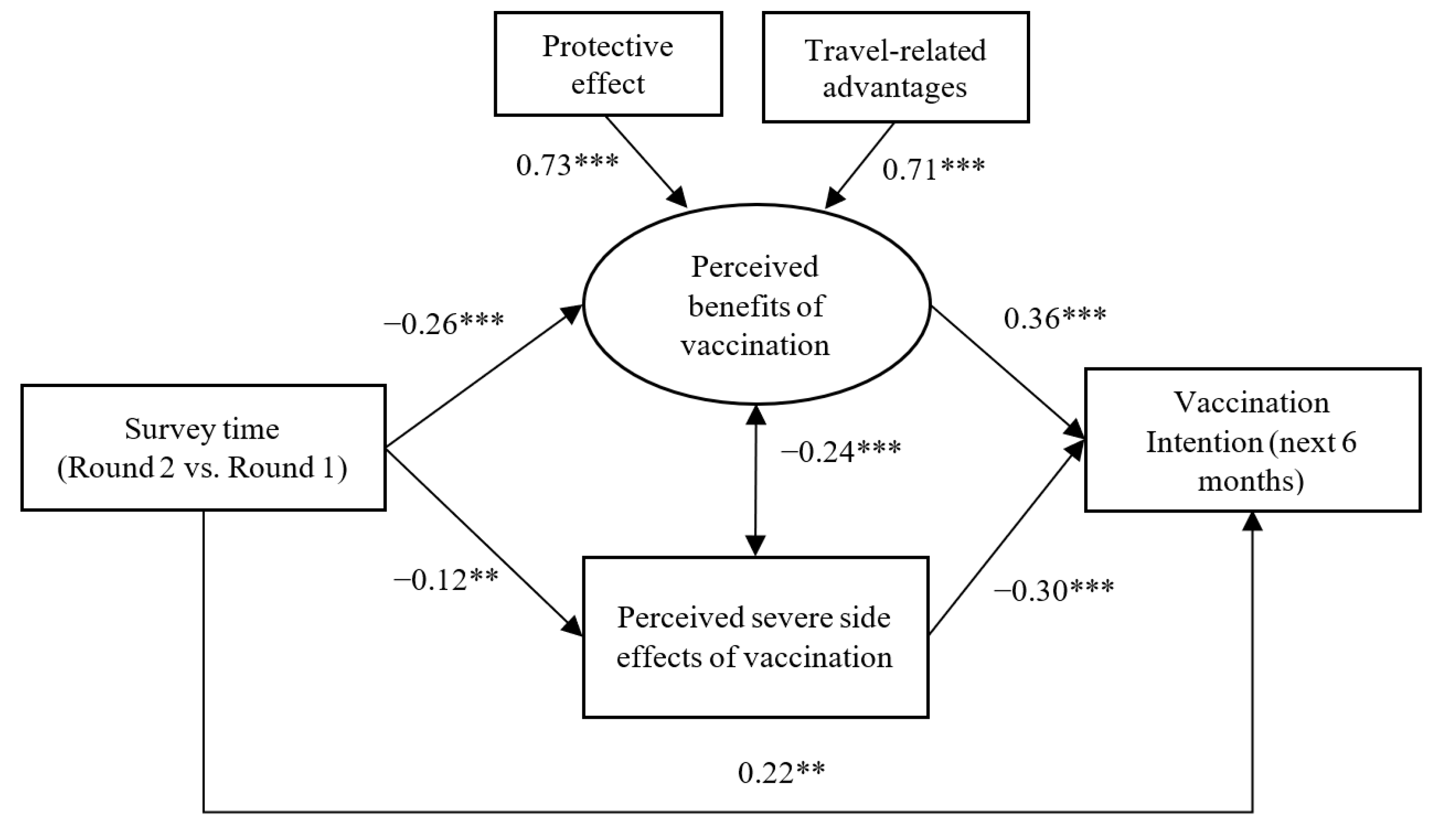
3.4. Testing Mediation/Suppression between Survey Time and COVID-19 Vaccination Intention
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bartsch, S.M.; O’Shea, K.J.; Ferguson, M.C.; Bottazzi, M.E.; Wedlock, P.T.; Strych, U.; McKinnell, J.A.; Siegmund, S.S.; Cox, S.N.; Hotez, P.J. Vaccine efficacy needed for a COVID-19 coronavirus vaccine to prevent or stop an epidemic as the sole intervention. Am. J. Prev. Med. 2020, 59, 493–503. [Google Scholar] [CrossRef]
- Al-Amer, R.; Maneze, D.; Everett, B.; Montayre, J.; Villarosa, A.R.; Dwekat, E.; Salamonson, Y. COVID-19 vaccination intention in the first year of the pandemic: A systematic review. J. Clin. Nurs. 2021. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M. COVID-19 vaccine hesitancy worldwide: A concise systematic review of vaccine acceptance rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef]
- Bloomberg. Vaccine Tracker. Available online: https://www.bloomberg.com/graphics/covid-vaccine-tracker-global-distribution/ (accessed on 25 June 2021).
- Centers for Disease Control and Prevention of U.S.A. Science Brief: COVID-19 Vaccines and Vaccination. Available online: https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/fully-vaccinated-people.html (accessed on 1 November 2021).
- Yu, Y.; Lau, M.; Lau, J.T.-F. Positive Association between Individualism and Vaccination Resistance against COVID-19 Vaccination among Chinese Adults: Mediations via Perceived Personal and Societal Benefits. Vaccines 2021, 9, 1225. [Google Scholar] [CrossRef] [PubMed]
- Fridman, A.; Gershon, R.; Gneezy, A. COVID-19 and vaccine hesitancy: A longitudinal study. PLoS ONE 2021, 16, e0250123. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Wong, E.L.-Y.; Ho, K.-F.; Cheung, A.W.-L.; Yau, P.S.-Y.; Dong, D.; Wong, S.Y.-S.; Yeoh, E.-K. Change of willingness to accept COVID-19 vaccine and reasons of vaccine hesitancy of working people at different waves of local epidemic in Hong Kong, China: Repeated cross-sectional surveys. Vaccines 2021, 9, 62. [Google Scholar] [CrossRef]
- Wani, T.A.; Ali, S. Innovation diffusion theory. J. Gen. Manag. Res. 2015, 3, 101–118. [Google Scholar]
- Mo, P.K.H.; Luo, S.; Wang, S.; Zhao, J.; Zhang, G.; Li, L.; Li, L.; Xie, L.; Lau, J.T. Intention to receive the COVID-19 vaccination in China: Application of the diffusion of innovations theory and the moderating role of openness to experience. Vaccines 2021, 9, 129. [Google Scholar] [CrossRef]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Janz, N.K.; Becker, M.H. The health belief model: A decade later. Health Educ. Q. 1984, 11, 1–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bandura, A. Social cognitive theory of self-regulation. Organ. Behav. Hum. Decis. Process. 1991, 50, 248–287. [Google Scholar] [CrossRef]
- Gul, F.; Pesendorfer, W. Temptation and self-control. Econometrica 2001, 69, 1403–1435. [Google Scholar] [CrossRef]
- Yu, Y.; Lau, J.T.F.; Lau, M.M.C.; Wong, M.C.S.; Chan, P.K.S. Understanding the Prevalence and Associated Factors of Behavioral Intention of COVID-19 Vaccination Under Specific Scenarios Combining Effectiveness, Safety, and Cost in the Hong Kong Chinese General Population. Int. J. Health Policy Manag. 2021. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Lu, X.; Lai, X.; Lyu, Y.; Zhang, H.; Fenghuang, Y.; Jing, R.; Li, L.; Yu, W.; Fang, H. The changing acceptance of COVID-19 vaccination in different epidemic phases in China: A longitudinal study. Vaccines 2021, 9, 191. [Google Scholar] [CrossRef]
- Wong, M.C.S.; Wong, E.L.Y.; Cheung, A.W.L.; Huang, J.; Lai, C.K.C.; Yeoh, E.K.; Chan, P.K.S. COVID-19 Vaccine Hesitancy in a City with Free Choice and Sufficient Doses. Vaccines 2021, 9, 1250. [Google Scholar] [CrossRef]
- Yu, Y.; Lau, M.; Jiang, H.; Lau, J.T. Prevalence and Factors of the Performed or Scheduled COVID-19 Vaccination in a Chinese Adult General Population in Hong Kong. Vaccines 2021, 9, 847. [Google Scholar] [CrossRef]
- BBC News. COVID Infection Protection Waning in Double Jabbed. Available online: https://www.bbc.com/news/health-58322882 (accessed on 1 November 2021).
- World Health Organization. Side Effects of COVID-19 Vaccines. Available online: https://www.who.int/news-room/feature-stories/detail/side-effects-of-covid-19-vaccines (accessed on 23 April 2021).
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Marc, G.P.; Moreira, E.D.; Zerbini, C. Safety and efficacy of the BNT162b2 mRNA COVID-19 vaccine. N. Engl. J. Med. 2020, 38, 2603–2615. [Google Scholar] [CrossRef]
- Kow, C.S.; Hasan, S.S. Real-world effectiveness of BNT162b2 mRNA vaccine: A meta-analysis of large observational studies. Inflammopharmacology 2021, 29, 1075–1090. [Google Scholar] [CrossRef]
- Abu-Raddad, L.J.; Chemaitelly, H.; Butt, A.A. Effectiveness of the BNT162b2 COVID-19 Vaccine against the B. 1.1. 7 and B. 1.351 Variants. N. Engl. J. Med. 2021, 385, 187–189. [Google Scholar] [CrossRef]
- Hitchings, M.D.; Ranzani, O.T.; Torres, M.S.S.; de Oliveira, S.B.; Almiron, M.; Said, R.; Borg, R.; Schulz, W.L.; de Oliveira, R.D.; da Silva, P.V. Effectiveness of CoronaVac in the setting of high SARS-CoV-2 P. 1 variant transmission in Brazil: A test-negative case-control study. medRxiv 2021. [Google Scholar] [CrossRef]
- Jara, A.; Undurraga, E.A.; González, C.; Paredes, F.; Fontecilla, T.; Jara, G.; Pizarro, A.; Acevedo, J.; Leo, K.; Leon, F. Effectiveness of an inactivated SARS-CoV-2 vaccine in Chile. N. Engl. J. Med. 2021, 385, 875–884. [Google Scholar] [CrossRef] [PubMed]
- Hong Kong Special Administrative Region Government. Hong Kong Vaccination Dashboard. Available online: https://www.covidvaccine.gov.hk/en/ (accessed on 25 June 2021).
- Office of the Communication Authority, H. Key Communication Statistics. Available online: https://www.ofca.gov.hk/en/news_info/data_statistics/key_stat/ (accessed on 3 November 2021).
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Academic Press: Cambridge, MA, USA, 2013. [Google Scholar]
- Hoyle, R.H. Structural Equation Modeling: Concepts, Issues, and Applications; Sage: Thousand Oaks, CA, USA, 1995. [Google Scholar]
- Fairchild, A.J.; MacKinnon, D.P.; Taborga, M.P.; Taylor, A.B. R2 effect-size measures for mediation analysis. Behav. Res. Methods 2009, 41, 486–498. [Google Scholar] [CrossRef] [Green Version]
- Wong, M.C.; Wong, E.L.; Huang, J.; Cheung, A.W.; Law, K.; Chong, M.K.; Ng, R.W.; Lai, C.K.; Boon, S.S.; Lau, J.T. Acceptance of the COVID-19 vaccine based on the health belief model: A population-based survey in Hong Kong. Vaccine 2021, 39, 1148–1156. [Google Scholar] [CrossRef]
- Kwok, K.O.; Li, K.K.; Tang, A.; Tsoi, M.T.F.; Chan, E.Y.Y.; Tang, J.W.T.; Wong, A.; Wei, W.I.; Wong, S.Y.S. Psychobehavioral Responses and Likelihood of Receiving COVID-19 Vaccines during the Pandemic, Hong Kong. Emerg. Infect. Dis. 2021, 27, 1802–1810. [Google Scholar] [CrossRef]
- World Health Organization. The Effects of Virus Variants on COVID-19 Vaccines. Available online: https://www.who.int/news-room/feature-stories/detail/the-effects-of-virus-variants-on-covid-19-vaccines?gclid=EAIaIQobChMIhdXepaOy8QIVi38rCh0pAw7MEAAYASAAEgK6wPD_BwE (accessed on 25 June 2021).
- Centers for Disease Control and Prevention of U.S.A. COVID Data Tracker. Available online: https://covid.cdc.gov/covid-data-tracker/#rates-by-vaccine-status (accessed on 27 November 2021).
- Yu, Y.; Lau, J.T.F.; She, R.; Chen, X.; Li, L.; Li, L.; Chen, X. Prevalence and associated factors of intention of COVID-19 vaccination among healthcare workers in China: Application of the Health Belief Model. Hum. Vaccines Immunother. 2021, 17, 2894–2902. [Google Scholar] [CrossRef]
- Martin, A.; Goryakin, Y.; Suhrcke, M. Does active commuting improve psychological wellbeing? Longitudinal evidence from eighteen waves of the British Household Panel Survey. Prev. Med. 2014, 69, 296–303. [Google Scholar] [CrossRef]
- O’donoghue, G.; Perchoux, C.; Mensah, K.; Lakerveld, J.; Van Der Ploeg, H.; Bernaards, C.; Chastin, S.F.; Simon, C.; O’gorman, D.; Nazare, J.-A. A systematic review of correlates of sedentary behaviour in adults aged 18–65 years: A socio-ecological approach. BMC Public Health 2016, 16, 163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. COVID-19 Advice for the Public: Getting Vaccinated. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines/advice (accessed on 29 June 2021).
- Sherman, S.M.; Smith, L.E.; Sim, J.; Amlôt, R.; Cutts, M.; Dasch, H.; Rubin, G.J.; Sevdalis, N. COVID-19 vaccination intention in the UK: Results from the COVID-19 vaccination acceptability study (CoVAccS), a nationally representative cross-sectional survey. Hum. Vaccines Immunother. 2021, 17, 1612–1621. [Google Scholar] [CrossRef]
- Abdallah, D.A.; Lee, C.M. Social norms and vaccine uptake: College students’ COVID vaccination intentions, attitudes, and estimated peer norms and comparisons with influenza vaccine. Vaccine 2021, 39, 2060–2067. [Google Scholar]
- Betsch, C.; Böhm, R. Moral values do not affect prosocial vaccination. Nat. Hum. Behav. 2018, 2, 881–882. [Google Scholar] [CrossRef]
- Census and Statistics Department, Hong Kong Special Administrative Region Goverment. Women and Men in Hong Kong Key Statistics; Hong Kong Special Administrative Region Government: Hong Kong, China, 2019.
| Round 1 n (%) | Round 2 n (%) | p of Chi-Square Test | |
|---|---|---|---|
| Overall | 358 | 145 | |
| Background factors | |||
| Sex | 0.409 | ||
| Females | 223 (62.3) | 96 (66.2) | |
| Males | 135 (37.7) | 49 (33.8) | |
| Educational level | <0.001 | ||
| Below college | 301 (84.1) | 97 (66.9) | |
| College or above | 57 (15.9) | 48 (33.1) | |
| Marital status | 0.534 | ||
| Others | 135 (37.7) | 59 (40.7) | |
| Married | 223 (62.3) | 86 (59.3) | |
| Chronic disease status | 0.023 | ||
| No/Do not know | 279 (77.9) | 99 (68.3) | |
| Yes | 79 (22.1) | 46 (31.7) | |
| Behavioral intention of COVID-19 vaccination in the next 6 months | 0.026 | ||
| Low intention | 306 (85.5) | 112 (77.2) | |
| High intention | 52 (14.5) | 33 (22.8) |
| Behavioral Intention of COVID-19 Vaccination | ||
|---|---|---|
| ORc (95% CI) | p | |
| Age | 1.01 (0.99–1.03) | 0.440 |
| Sex | ||
| Females | Ref = 1.0 | |
| Males | 0.79 (0.49–1.27) | 0.335 |
| Educational level | ||
| Below college | Ref = 1.0 | |
| College or above | 1.17 (0.65–2.11) | 0.610 |
| Marital status | ||
| Others | Ref = 1.0 | |
| Married | 1.08 (0.67–1.73) | 0.766 |
| Chronic disease status | ||
| No/Do not know | Ref = 1.0 | |
| Yes | 0.94 (0.55–1.60) | 0.809 |
| Behavioral Intention of COVID-19 Vaccination | ||
|---|---|---|
| ORa (95% CI) | p | |
| Survey time (Round 2 versus Round 1) | 1.86 (1.12–3.08) | 0.016 |
| Perceived benefits | ||
| Protective effect | 1.80 (1.27–2.55) | 0.001 |
| Travel advantages | 1.48 (1.05–2.08) | 0.026 |
| Perceived severe side effects | 0.47 (0.33–0.68) | <0.001 |
| Round 1 | Round 2 | ||||
|---|---|---|---|---|---|
| Range | Mean, SD | Mean, SD | p of t-Test | Cohen’s d | |
| Perceived benefits | |||||
| Protective effect | 1–5 | 3.3, 0.9 | 3.0, 0.7 | 0.001 | 0.34 |
| Travel advantages | 1–5 | 3.6, 1.0 | 3.2, 1.0 | <0.001 | 0.42 |
| Perceived severe side effects | 1–5 | 3.8, 0.9 | 3.5, 0.8 | 0.001 | 0.31 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, Y.; Lau, J.T.F.; Lau, M.M.C. Opposing Mechanisms Involving Perceived Benefits versus Safety Partially Explained an Increase in COVID-19 Vaccination Intention among Unvaccinated Chinese Adults during a Post-Rollout Period: Results of Two Serial Surveys. Vaccines 2021, 9, 1414. https://doi.org/10.3390/vaccines9121414
Yu Y, Lau JTF, Lau MMC. Opposing Mechanisms Involving Perceived Benefits versus Safety Partially Explained an Increase in COVID-19 Vaccination Intention among Unvaccinated Chinese Adults during a Post-Rollout Period: Results of Two Serial Surveys. Vaccines. 2021; 9(12):1414. https://doi.org/10.3390/vaccines9121414
Chicago/Turabian StyleYu, Yanqiu, Joseph T. F. Lau, and Mason M. C. Lau. 2021. "Opposing Mechanisms Involving Perceived Benefits versus Safety Partially Explained an Increase in COVID-19 Vaccination Intention among Unvaccinated Chinese Adults during a Post-Rollout Period: Results of Two Serial Surveys" Vaccines 9, no. 12: 1414. https://doi.org/10.3390/vaccines9121414
APA StyleYu, Y., Lau, J. T. F., & Lau, M. M. C. (2021). Opposing Mechanisms Involving Perceived Benefits versus Safety Partially Explained an Increase in COVID-19 Vaccination Intention among Unvaccinated Chinese Adults during a Post-Rollout Period: Results of Two Serial Surveys. Vaccines, 9(12), 1414. https://doi.org/10.3390/vaccines9121414







