Determinants of COVID-19 Vaccine Acceptance among the Adult Population of Bangladesh Using the Health Belief Model and the Theory of Planned Behavior Model
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Settings and Participants
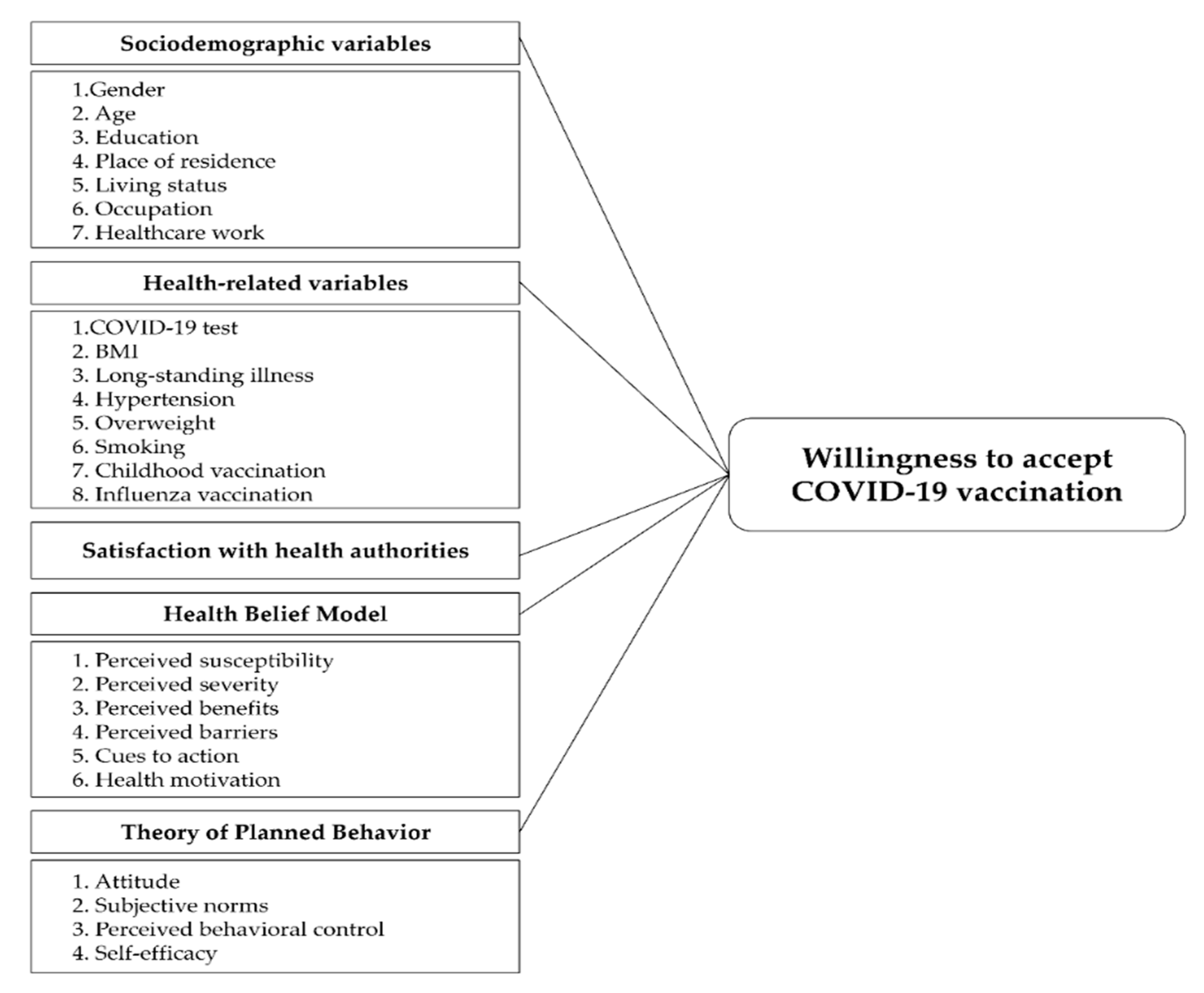
2.2. Measures
2.2.1. Willingness to Accept Vaccine and Reasons Not to Accept Vaccine
2.2.2. Trust/Satisfaction with Health Authorities
2.2.3. Health Belief Model (HBM) Variables
2.2.4. Theory of Planned Behavior (TPB) Variables
2.2.5. Sociodemographic and Health Variables
2.3. Statitical Analysis
3. Results
3.1. Sociodemographic Characteristics and COVID-19 Vaccine Acceptance
3.2. Univariate Analyses of Trust/Satisfaction with Authorities and Health Behavior Variables
3.3. Multivariate Analysis of Factors Associated with COVID-19 Vaccine Acceptance
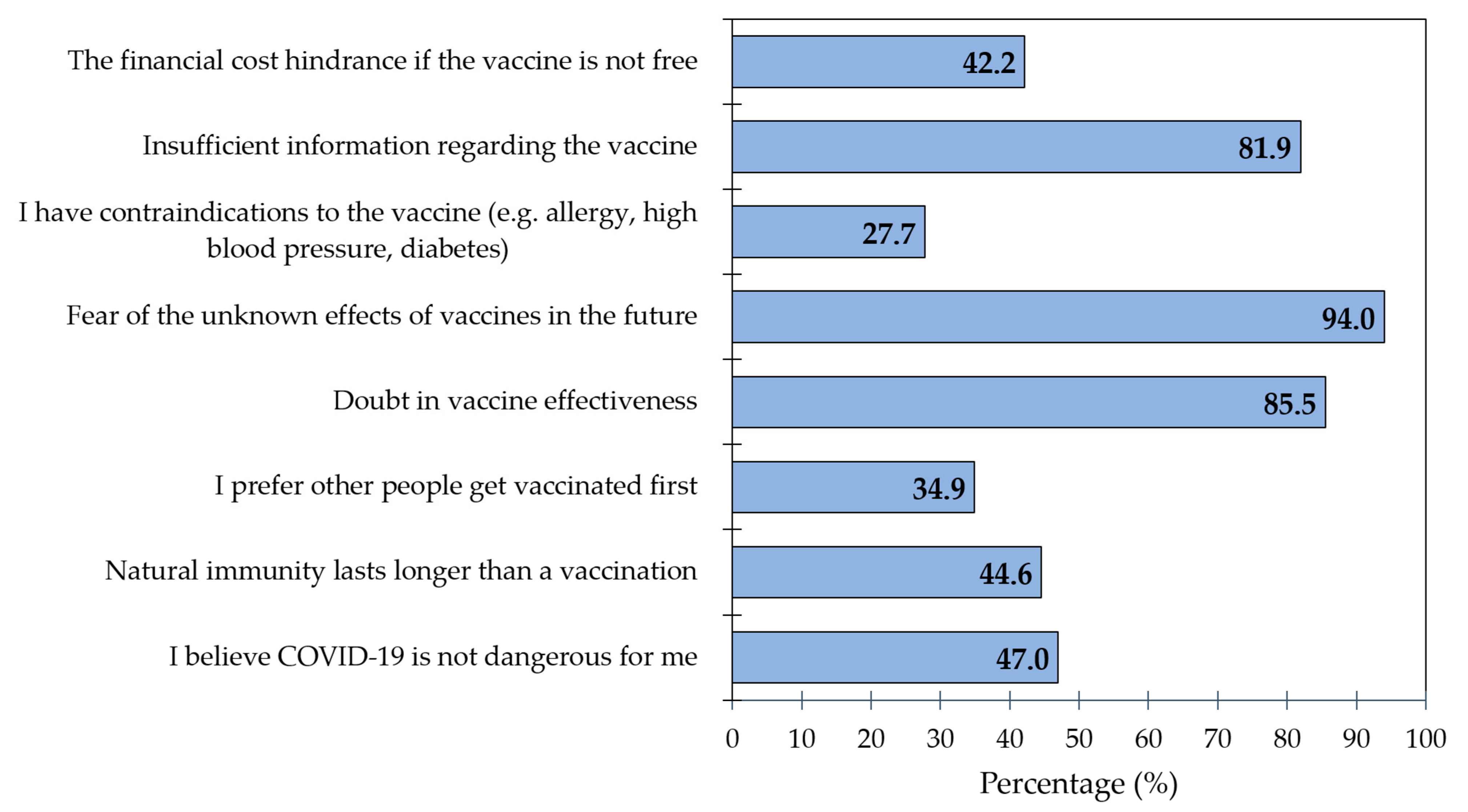
3.4. Reasons behind Unwillingness/Indecision with Getting Vaccinated
4. Discussion
4.1. Implications
4.2. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. COVID 19 Public Health Emergency of International Concern (PHEIC) Global Research and Innovation Forum. Available online: https://www.who.int/publications/m/item/covid-19-public-health-emergency-of-international-concern-(pheic)-global-research-and-innovation-forum (accessed on 30 November 2020).
- Worldometer, S. Covid-19 Coronavirus Pandemic: Worldometer. 2020. Available online: https://www.worldometers.info/coronavirus/ (accessed on 11 June 2021).
- Hossain, M.S.; Ferdous, S.; Siddiqee, M.H. Mass panic during Covid-19 outbreak- A perspective from Bangladesh as a high-risk country. J. Biomed. Anal. 2020, 3, 1–3. [Google Scholar] [CrossRef]
- Haug, N.; Geyrhofer, L.; Londei, A.; Dervic, E.; Desvars-Larrive, A.; Loreto, V.; Pinior, B.; Thurner, S.; Klimek, P. Ranking the effectiveness of worldwide COVID-19 government interventions. Nat. Hum. Behav. 2020, 4, 1303–1312. [Google Scholar] [CrossRef] [PubMed]
- Viana, J.; van Dorp, C.H.; Nunes, A.; Gomes, M.C.; van Boven, M.; Kretzschmar, M.E.; Veldhoen, M.; Rozhnova, G. Controlling the pandemic during the SARS-CoV-2 vaccination rollout. Nat. Commun. 2021, 12, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Krammer, F. SARS-CoV-2 vaccines in development. Nature 2020, 586, 516–527. [Google Scholar] [CrossRef]
- Tumban, E. Lead SARS-CoV-2 Candidate Vaccines: Expectations from Phase III Trials and Recommendations Post-Vaccine Approval. Viruses 2020, 13, 54. [Google Scholar] [CrossRef] [PubMed]
- Ruma, P. ‘The Wait is Over’: Bangladesh Begins COVID-19 Vaccinations. Available online: https://www.reuters.com/article/us-health-coronavirus-bangladesh-vaccine-idUSKBN2A70I0 (accessed on 28 December 2020).
- Sallam, M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef]
- DeRoo, S.S.; Pudalov, N.J.; Fu, L.Y. Planning for a COVID-19 Vaccination Program. JAMA 2020, 323, 2458. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2021, 27, 225–228. [Google Scholar] [CrossRef]
- Gallè, F.; Sabella, E.A.; Roma, P.; Da Molin, G.; Diella, G.; Montagna, M.T.; Ferracuti, S.; Liguori, G.; Orsi, G.B.; Napoli, C. Acceptance of COVID-19 Vaccination in the Elderly: A Cross-Sectional Study in Southern Italy. Vaccines 2021, 9, 1222. [Google Scholar] [CrossRef]
- Gallè, F.; Sabella, E.; Roma, P.; De Giglio, O.; Caggiano, G.; Tafuri, S.; Da Molin, G.; Ferracuti, S.; Montagna, M.; Liguori, G.; et al. Knowledge and Acceptance of COVID-19 Vaccination among Undergraduate Students from Central and Southern Italy. Vaccines 2021, 9, 638. [Google Scholar] [CrossRef]
- Al-Mohaithef, M.; Padhi, B.K. Determinants of COVID-19 Vaccine Acceptance in Saudi Arabia: A Web-Based National Survey. J. Multidiscip. Health 2020, 13, 1657–1663. [Google Scholar] [CrossRef]
- Harapan, H.; Wagner, A.L.; Yufika, A.; Winardi, W.; Anwar, S.; Gan, A.K.; Setiawan, A.M.; Rajamoorthy, Y.; Sofyan, H.; Mudatsir, M. Acceptance of a COVID-19 Vaccine in Southeast Asia: A Cross-Sectional Study in Indonesia. Front. Public Health 2020, 8, 381. [Google Scholar] [CrossRef]
- Reiter, P.L.; Pennell, M.L.; Katz, M.L. Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine 2020, 38, 6500–6507. [Google Scholar] [CrossRef] [PubMed]
- Taylor, S.; Landry, C.A.; Paluszek, M.M.; Groenewoud, R.; Rachor, G.S.; Asmundson, G.J.G. A Proactive Approach for Managing COVID-19: The Importance of Understanding the Motivational Roots of Vaccination Hesitancy for SARS-CoV2. Front. Psychol. 2020, 11, 575950. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Jing, R.; Lai, X.; Zhang, H.; Lyu, Y.; Knoll, M.D.; Fang, H. Acceptance of COVID-19 Vaccination during the COVID-19 Pandemic in China. Vaccines 2020, 8, 482. [Google Scholar] [CrossRef]
- Paul, A.; Sikdar, D.; Mahanta, J.; Ghosh, S.; Jabed, A.; Paul, S.; Yeasmin, F.; Sikdar, S.; Chowdhury, B.; Nath, T.K. Peoples’ understanding, acceptance, and perceived challenges of vaccination against COVID-19: A cross-sectional study in Bangladesh. PLoS ONE 2021, 16, e0256493. [Google Scholar] [CrossRef]
- Abedin, M.; Islam, M.A.; Rahman, F.N.; Reza, H.M.; Hossain, M.Z.; Arefin, A.; Hossain, A. Willingness to vaccinate against COVID-19 among Bangladeshi adults: Understanding the strategies to optimize vaccination coverage. PLoS ONE 2021, 16, e0250495. [Google Scholar] [CrossRef]
- Kalam, A.; Davis, T.P., Jr.; Shano, S.; Uddin, N.; Islam, A.; Kanwagi, R.; Hassan, M.M.; Larson, H.J. Exploring the behavioral determinants of COVID-19 vaccine acceptance among an urban population in Bangladesh: Implications for behavior change interventions. PLoS ONE 2021, 16, e0256496. [Google Scholar] [CrossRef]
- Arce, J.S.S.; Warren, S.S.; Meriggi, N.F.; Scacco, A.; McMurry, N.; Voors, M.; Syunyaev, G.; Malik, A.A.; Aboutajdine, S.; Adeojo, O.; et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat. Med. 2021, 27, 1385–1394. [Google Scholar] [CrossRef]
- Sallam, M.; Dababseh, D.; Eid, H.; Al-Mahzoum, K.; Al-Haidar, A.; Taim, D.; Yaseen, A.; Ababneh, N.A.; Bakri, F.G.; Mahafzah, A. High Rates of COVID-19 Vaccine Hesitancy and Its Association with Conspiracy Beliefs: A Study in Jordan and Kuwait among Other Arab Countries. Vaccines 2021, 9, 42. [Google Scholar] [CrossRef]
- Sallam, M.; Dababseh, D.; Eid, H.; Hasan, H.; Taim, D.; Al-Mahzoum, K.; Al-Haidar, A.; Yaseen, A.; Ababneh, N.; Assaf, A.; et al. Low COVID-19 Vaccine Acceptance Is Correlated with Conspiracy Beliefs among University Students in Jordan. Int. J. Environ. Res. Public Health 2021, 18, 2407. [Google Scholar] [CrossRef]
- MacDonald, N.E.; Sage Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Larson, H.J.; Clarke, R.M.; Jarrett, C.; Eckersberger, E.; Levine, Z.; Schulz, W.S.; Paterson, P. Measuring trust in vaccination: A systematic review. Hum. Vaccines Immunother. 2018, 14, 1599–1609. [Google Scholar] [CrossRef]
- Larson, H.J.; De Figueiredo, A.; Xiahong, Z.; Schulz, W.S.; Verger, P.; Johnston, I.G.; Cook, A.R.; Jones, N.S. The State of Vaccine Confidence 2016: Global Insights Through a 67-Country Survey. EBioMedicine 2016, 12, 295–301. [Google Scholar] [CrossRef] [Green Version]
- Seale, H.; Heywood, A.E.; Leask, J.; Sheel, M.; Thomas, S.; Durrheim, D.N.; Bolsewicz, K.; Kaur, R. COVID-19 is rapidly changing: Examining public perceptions and behaviors in response to this evolving pandemic. PLoS ONE 2020, 15, e0235112. [Google Scholar] [CrossRef]
- Regmi, K.; Lwin, C. Factors Associated with the Implementation of Non-Pharmaceutical Interventions for Reducing Coronavirus Disease 2019 (COVID-19): A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 4274. [Google Scholar] [CrossRef]
- Han, E.; Tan, M.M.J.; Turk, E.; Sridhar, D.; Leung, G.M.; Shibuya, K.; Asgari, N.; Oh, J.; García-Basteiro, A.L.; Hanefeld, J.; et al. Lessons learnt from easing COVID-19 restrictions: An analysis of countries and regions in Asia Pacific and Europe. Lancet 2020, 396, 1525–1534. [Google Scholar] [CrossRef]
- Gabriel, E.H.; Hoch, M.C.; Cramer, R.J. Health Belief Model Scale and Theory of Planned Behavior Scale to assess attitudes and perceptions of injury prevention program participation: An exploratory factor analysis. J. Sci. Med. Sport 2019, 22, 544–549. [Google Scholar] [CrossRef] [PubMed]
- Shmueli, L. Predicting intention to receive COVID-19 vaccine among the general population using the health belief model and the theory of planned behavior model. BMC Public Health 2021, 21, 804. [Google Scholar] [CrossRef] [PubMed]
- Zampetakis, L.A.; Melas, C. The health belief model predicts vaccination intentions against COVID-19: A survey experiment approach. Appl. Psychol. Health Well-Being 2021, 13, 469–484. [Google Scholar] [CrossRef] [PubMed]
- Wong, L.P.; Alias, H.; Wong, P.-F.; Lee, H.Y.; Abubakar, S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum. Vaccines Immunother. 2020, 16, 1232–1238. [Google Scholar] [CrossRef]
- Wong, M.C.S.; Wong, E.L.Y.; Huang, J.; Cheung, A.W.L.; Law, K.; Chong, M.K.C.; Ng, R.W.Y.; Lai, C.K.C.; Boon, S.S.; Lau, J.T.F.; et al. Acceptance of the COVID-19 vaccine based on the health belief model: A population-based survey in Hong Kong. Vaccine 2021, 39, 1148–1156. [Google Scholar] [CrossRef] [PubMed]
- Moona, A.; Daria, S.; Asaduzzaman, M.; Islam, R. Bangladesh reported delta variant of coronavirus among its citizen: Actionable items to tackle the potential massive third wave. Infect. Prev. Pr. 2021, 3, 100159. [Google Scholar] [CrossRef] [PubMed]
- Statulator. Statulator: A Free on-Line Statistical Calculator. Available online: https://statulator.com/ (accessed on 17 November 2021).
- Janz, N.K.; Becker, M.H. The Health Belief Model: A Decade Later. Health Educ. Q. 1984, 11, 1–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Godin, G.; Kok, G. The Theory of Planned Behavior: A Review of its Applications to Health-Related Behaviors. Am. J. Health Promot. 1996, 11, 87–98. [Google Scholar] [CrossRef] [PubMed]
- Fan, C.-W.; Chen, I.-H.; Ko, N.-Y.; Yen, C.-F.; Lin, C.-Y.; Griffiths, M.D.; Pakpour, A.H. Extended theory of planned behavior in explaining the intention to COVID-19 vaccination uptake among mainland Chinese university students: An online survey study. Hum. Vaccines Immunother. 2021, 17, 3413–3420. [Google Scholar] [CrossRef]
- Chinn, S. A simple method for converting an odds ratio to effect size for use in meta-analysis. Stat. Med. 2000, 19, 3127–3131. [Google Scholar] [CrossRef]
- Al-Sanafi, M.; Sallam, M. Psychological Determinants of COVID-19 Vaccine Acceptance among Healthcare Workers in Kuwait: A Cross-Sectional Study Using the 5C and Vaccine Conspiracy Beliefs Scales. Vaccines 2021, 9, 701. [Google Scholar] [CrossRef] [PubMed]
- Goruntla, N.; Chintamani, S.H.; Bhanu, P.; Samyuktha, S.; Veerabhadrappa, K.V.; Bhupalam, P.; Ramaiah, J.D. Predictors of acceptance and willingness to pay for the COVID-19 vaccine in the general public of India: A health belief model approach. Asian Pac. J. Trop. Med. 2021, 14, 165. [Google Scholar] [CrossRef]
- Borriello, A.; Master, D.; Pellegrini, A.; Rose, J.M. Preferences for a COVID-19 vaccine in Australia. Vaccine 2021, 39, 473–479. [Google Scholar] [CrossRef]
- Detoc, M.; Bruel, S.; Frappe, P.; Tardy, B.; Botelho-Nevers, E.; Gagneux-Brunon, A. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine 2020, 38, 7002–7006. [Google Scholar] [CrossRef]
- Tao, L.; Wang, R.; Han, N.; Liu, J.; Yuan, C.; Deng, L.; Han, C.; Sun, F.; Liu, M.; Liu, J. Acceptance of a COVID-19 vaccine and associated factors among pregnant women in China: A multi-center cross-sectional study based on health belief model. Hum. Vaccines Immunother. 2021, 17, 2378–2388. [Google Scholar] [CrossRef] [PubMed]
- Gagneux-Brunon, A.; Detoc, M.; Bruel, S.; Tardy, B.; Rozaire, O.; Frappe, P.; Botelho-Nevers, E. Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: A cross-sectional survey. J. Hosp. Infect. 2020, 108, 168–173. [Google Scholar] [CrossRef]
- World Health Organization (WHO) Bangladesh. Morbidity and Mortality Weekly Update (MMWU) No49. Available online: https://cdn.who.int/media/docs/default-source/searo/bangladesh/covid-19-who-bangladesh-situation-reports/who_covid-19-update_49_20210201.pdf?sfvrsn=a365c489_9 (accessed on 30 October 2021).
- Mahmud, S.; Mohsin, M.; Khan, I.A.; Mian, A.U.; Zaman, M.A. Knowledge, beliefs, attitudes and perceived risk about COVID-19 vaccine and determinants of COVID-19 vaccine acceptance in Bangladesh. PLoS ONE 2021, 16, e0257096. [Google Scholar] [CrossRef] [PubMed]
- Hossain, M.B.; Alam, M.Z.; Islam, M.S.; Sultan, S.; Faysal, M.M.; Rima, S.; Hossain, M.A.; Mamun, A.A. COVID-19 Vaccine Hesitancy among the Adult Population in Bangladesh: A Nationally Representative Cross-sectional Survey. medRxiv 2021. [Google Scholar] [CrossRef]
- Islam, M.S.; Siddique, A.B.; Akter, R.; Tasnim, R.; Sujan, M.S.H.; Ward, P.R.; Sikder, M.T. Knowledge, attitudes and perceptions towards COVID-19 vaccinations: A cross-sectional community survey in Bangladesh. BMC Public Health 2021, 21, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Tabassum, M.; Parvej, I.; Sultana, S.; Mannan, S.E.; Ahmed, F. Determinants of COVID-19 vaccine acceptance and encountered side-effects among the vaccinated in Bangladesh. Asian Pac. J. Trop. Med. 2021, 14, 341. [Google Scholar] [CrossRef]
- Yan, E.; Lai, D.; Lee, V. Predictors of Intention to Vaccinate against COVID-19 in the General Public in Hong Kong: Findings from a Population-Based, Cross-Sectional Survey. Vaccines 2021, 9, 696. [Google Scholar] [CrossRef]
- Cerda, A.A.; García, L.Y. Hesitation and Refusal Factors in Individuals’ Decision-Making Processes Regarding a Coronavirus Disease 2019 Vaccination. Front. Public Health 2021, 9, 626852. [Google Scholar] [CrossRef]
- Alam, A.M.; Majumder, A.A.; Haque, M.; Ashraf, F.; Khondoker, M.U.; Mashreky, S.R.; Wahab, A.; Siddiqui, T.H.; Uddin, A.; Joarder, T.; et al. Disproportionate COVID-19 vaccine acceptance rate among healthcare professionals on the eve of nationwide vaccine distribution in Bangladesh. Expert Rev. Vaccines 2021, 20, 1167–1175. [Google Scholar] [CrossRef]
- Ali, M.; Hossain, A. What is the extent of COVID-19 vaccine hesitancy in Bangladesh? A cross-sectional rapid national survey. BMJ Open 2021, 11, e050303. [Google Scholar] [CrossRef]
- Haque, M.M.A.; Rahman, M.L.; Hossian, M.; Matin, K.F.; Nabi, M.H.; Saha, S.; Hasan, M.; Manna, R.M.; Barsha, S.Y.; Hasan, S.; et al. Acceptance of COVID-19 vaccine and its determinants: Evidence from a large sample study in Bangladesh. Heliyon 2021, 7, e07376. [Google Scholar] [CrossRef] [PubMed]
- The Daily Star. University Students to be Vaccinated Soon. Available online: https://www.thedailystar.net/backpage/news/univ-students-be-vaccinated-soon-2102461 (accessed on 30 October 2021).
- Jackson, S.E.; Paul, E.; Brown, J.; Steptoe, A.; Fancourt, D. Negative Vaccine Attitudes and Intentions to Vaccinate Against Covid-19 in Relation to Smoking Status: A Population Survey of UK Adults. Nicotine Tob. Res. 2021, 23, 1623–1628. [Google Scholar] [CrossRef] [PubMed]
- Alqudeimat, Y.; Alenezi, D.; AlHajri, B.; Alfouzan, H.; Almokhaizeem, Z.; Altamimi, S.; Almansouri, W.; Alzalzalah, S.; Ziyab, A.H. Acceptance of a COVID-19 Vaccine and Its Related Determinants among the General Adult Population in Kuwait. Med. Princ. Pract. 2021, 30, 262–271. [Google Scholar] [CrossRef] [PubMed]
- Mangtani, P.; Breeze, E.; Kovats, S.; Ng, E.S.; Roberts, J.A.; Fletcher, A. Inequalities in influenza vaccine uptake among people aged over 74 years in Britain. Prev. Med. 2005, 41, 545–553. [Google Scholar] [CrossRef]
- Wada, K.; Smith, D. Influenza Vaccination Uptake among the Working Age Population of Japan: Results from a National Cross-Sectional Survey. PLoS ONE 2013, 8, e59272. [Google Scholar] [CrossRef] [Green Version]
- Herbec, A.; Brown, J.; Jackson, S.; Kale, D.; Zatonski, M.; Garnett, C.; Chadborn, T.; Shahab, L. Perceived Risk Factors for Severe Covid-19 Symptoms and their Association with Health Behaviours: Findings from the HEBECO Study; PsyArXiv Preprints: Ithaca, NY, USA, 2020. [Google Scholar] [CrossRef]
- Freeman, D.; Loe, B.S.; Chadwick, A.; Vaccari, C.; Waite, F.; Rosebrock, L.; Jenner, L.; Petit, A.; Lewandowsky, S.; Vanderslott, S.; et al. COVID-19 vaccine hesitancy in the UK: The Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol. Med. 2020, 1–15. [Google Scholar] [CrossRef]
- Vallis, M.; Glazer, S. Protecting Individuals Living with Overweight and Obesity: Attitudes and Concerns Towards COVID-19 Vaccination in Canada. Obesity 2021, 29, 1128–1137. [Google Scholar] [CrossRef]
- Heidi Ledford. How Obesity Could Create Problems for a COVID Vaccine. Available online: https://www.nature.com/articles/d41586-020-02946-6 (accessed on 30 December 2020).
- Townsend, M.J.; Kyle, T.K.; Stanford, F.C. COVID-19 Vaccination and Obesity: Optimism and Challenges. Obesity 2021, 29, 634–635. [Google Scholar] [CrossRef]
- Banik, R.; Islam, S.; Pranta, M.U.R.; Rahman, Q.M.; Rahman, M.; Pardhan, S.; Driscoll, R.; Hossain, S.; Sikder, T. Understanding the determinants of COVID-19 vaccination intention and willingness to pay: Findings from a population-based survey in Bangladesh. BMC Infect. Dis. 2021, 21, 1–15. [Google Scholar] [CrossRef]
- Kerr, J.R.; Schneider, C.R.; Recchia, G.; Dryhurst, S.; Sahlin, U.; Dufouil, C.; Arwidson, P.; Freeman, A.L.; van der Linden, S. Correlates of intended COVID-19 vaccine acceptance across time and countries: Results from a series of cross-sectional surveys. BMJ Open 2021, 11, e048025. [Google Scholar] [CrossRef]
- Alhalaseh, L.; Fayoumi, H.; Khalil, B. The Health Belief Model in predicting healthcare workers’ intention for influenza vaccine uptake in Jordan. Vaccine 2020, 38, 7372–7378. [Google Scholar] [CrossRef] [PubMed]
- Coe, A.B.; Elliott, M.H.; Gatewood, S.B.; Goode, J.-V.R.; Moczygemba, L.R. Perceptions and predictors of intention to receive the COVID-19 vaccine. Res. Soc. Adm. Pharm. 2021. [Google Scholar] [CrossRef] [PubMed]
- Kabir, R.; Mahmud, I.; Chowdhury, M.; Vinnakota, D.; Jahan, S.; Siddika, N.; Isha, S.; Nath, S.; Apu, E.H. COVID-19 Vaccination Intent and Willingness to Pay in Bangladesh: A Cross-Sectional Study. Vaccines 2021, 9, 416. [Google Scholar] [CrossRef] [PubMed]
- Jennings, W.; Stoker, G.; Bunting, H.; Valgarðsson, V.; Gaskell, J.; Devine, D.; McKay, L.; Mills, M. Lack of Trust, Conspiracy Beliefs, and Social Media Use Predict COVID-19 Vaccine Hesitancy. Vaccines 2021, 9, 593. [Google Scholar] [CrossRef]
- Thaker, J. The Persistence of Vaccine Hesitancy: COVID-19 Vaccination Intention in New Zealand. J. Health Commun. 2021, 26, 104–111. [Google Scholar] [CrossRef]
- Machingaidze, S.; Wiysonge, C.S. Understanding COVID-19 vaccine hesitancy. Nat. Med. 2021, 27, 1338–1339. [Google Scholar] [CrossRef]
- Troiano, G.; Nardi, A. Vaccine hesitancy in the era of COVID-19. Public Health 2021, 194, 245–251. [Google Scholar] [CrossRef]
- Mo, P.K.H.; Lau, J.T.F. Influenza vaccination uptake and associated factors among elderly population in Hong Kong: The application of the Health Belief Model. Health Educ. Res. 2015, 30, 706–718. [Google Scholar] [CrossRef] [Green Version]
- Wolff, K. COVID-19 Vaccination Intentions: The Theory of Planned Behavior, Optimistic Bias, and Anticipated Regret. Front. Psychol. 2021, 12, 648289. [Google Scholar] [CrossRef]
- Yahaghi, R.; Ahmadizade, S.; Fotuhi, R.; Taherkhani, E.; Ranjbaran, M.; Buchali, Z.; Jafari, R.; Zamani, N.; Shahbazkhania, A.; Simiari, H.; et al. Fear of COVID-19 and Perceived COVID-19 Infectability Supplement Theory of Planned Behavior to Explain Iranians’ Intention to Get COVID-19 Vaccinated. Vaccines 2021, 9, 684. [Google Scholar] [CrossRef] [PubMed]
- Wells, A. Meta-Cognition and Worry: A Cognitive Model of Generalized Anxiety Disorder. Behav. Cogn. Psychother. 1995, 23, 301–320. [Google Scholar] [CrossRef]
- Kazi Asequl, A.; Anwar, H.; Md, H.A.R. Factor Affecting COVID-19 Vaccine Hesitancy in Bangladesh: An Empirical Investigation. Res. Sq. 2021, preprint. [Google Scholar] [CrossRef]
- Kanozia, R.; Arya, R. “Fake news”, religion, and COVID-19 vaccine hesitancy in India, Pakistan, and Bangladesh. Media Asia 2021, 48, 313–321. [Google Scholar] [CrossRef]
- Bhattacherjee, S.; Dasgupta, P.; Mukherjee, A.; Dasgupta, S. Vaccine hesitancy for childhood vaccinations in slum areas of Siliguri, India. Indian J. Public Health 2018, 62, 253–258. [Google Scholar] [CrossRef]
| Variables | Total N = 543 (%) | COVID-19 Vaccine Acceptance | χ2 | p Value | |
|---|---|---|---|---|---|
| Intended (n = 460) (%) | Undecided/Unwilling (n = 83) (%) | ||||
| Sociodemographic characteristics | |||||
| Gender | 0.264 | 0.607 | |||
| Male | 210 (38.67) | 180 (39.13) | 30 (36.14) | ||
| Female | 333 (61.33) | 280 (60.87) | 53 (63.86) | ||
| Age | 24.29 (±3.67) | 24.14 (±2.92) | 25.13 (±6.35) | 36.494 | 0.019 |
| Education | 2.670 | 0.263 | |||
| Less than college education | 42 (7.73) | 32 (6.96) | 10 (12.05) | ||
| Bachelor’s degree | 272 (50.09) | 231 (50.21) | 41 (49.40) | ||
| Beyond Bachelor’s degree | 229 (42.17) | 197 (42.83) | 32 (38.55) | ||
| Administrative division | 4.680 | 0.699 | |||
| Barishal | 26 (4.79) | 24 (5.22) | 2 (2.41) | ||
| Chittagong | 35 (6.45) | 29 (6.30) | 6 (7.23) | ||
| Dhaka | 134 (24.68) | 111 (24.13) | 23 (27.71) | ||
| Khulna | 285 (52.49) | 243 (52.83) | 42 (50.60) | ||
| Mymensingh | 8 (1.47) | 8 (1.74) | 0 (0.00) | ||
| Rajshahi | 27 (4.97) | 21 (4.57) | 6 (7.23) | ||
| Rangpur | 25 (4.60) | 21 (4.57) | 4 (4.82) | ||
| Sylhet | 3 (0.55) | 3 (0.65) | 0 (0.00) | ||
| Place of residence | 0.547 | 0.460 | |||
| Urban | 353 (65.01) | 302 (65.65) | 51 (61.45) | ||
| Rural | 190 (34.99) | 158 (34.35) | 32 (38.55) | ||
| Living status | 2.955 | 0.228 | |||
| With family members | 420 (77.35) | 360 (78.26) | 60 (72.29) | ||
| With non-family members | 84 (15.47) | 66 (14.35) | 18 (21.69) | ||
| Alone | 39 (7.18) | 34 (7.39) | 5 (6.02) | ||
| Occupation | 9.969 | 0.044 | |||
| Unemployed | 84 (15.46) | 64 (13.91) | 20 (24.10) | ||
| Student | 375 (69.06) | 328 (71.30) | 47 (56.62) | ||
| Public sector | 7 (1.29) | 7 (1.52) | 0 (0.00) | ||
| Private sector | 39 (1.18) | 31 (6.74) | 8 (9.64) | ||
| Self-employed | 38 (7.00) | 30 (6.52) | 8 (9.64) | ||
| Healthcare worker | 1.697 | 0.428 | |||
| No | 499 (91.90) | 421 (91.52) | 78 (93.98) | ||
| Healthcare student | 35 (6.45) | 30 (6.52) | 5 (6.02) | ||
| Healthcare professional | 9 (1.66) | 9 (1.96) | 0 (0.00) | ||
| Health related characteristics | |||||
| Tested positive for COVID-19 | 0.553 | 0.457 | |||
| No | 269 (49.54) | 231 (50.52) | 38 (45.78) | ||
| Yes | 274 (50.46) | 229 (49.78) | 45 (54.22) | ||
| BMI | 8.244 | 0.041 | |||
| Underweight | 49 (9.02) | 45 (9.78) | 4 (4.82) | ||
| Normal weight | 370 (68.14) | 310 (67.39) | 60 (72.29) | ||
| Overweight | 88 (16.21) | 79 (17.17) | 9 (10.84) | ||
| Obesity | 36 (6.63) | 26 (5.65) | 10 (12.05) | ||
| Long-standing illness(es) | 0.006 | 0.938 | |||
| No | 290 (53.41) | 246 (53.48) | 44 (53.01) | ||
| Yes | 253 (46.59) | 214 (46.52) | 39 (46.99) | ||
| Hypertension | 2.484 | 0.115 | |||
| No | 516 (95.03) | 440 (96.65) | 76 (91.57) | ||
| Yes | 27 (4.97) | 20 (4.35) | 7 (8.43) | ||
| Overweight | 0.048 | 0.826 | |||
| No | 487 (89.69) | 412 (89.57) | 75 (90.36) | ||
| Yes | 56 (10.31) | 48 (10.43) | 8 (9.64) | ||
| Smoking | 4.363 | 0.037 | |||
| No | 415 (76.42) | 359 (78.04) | 56 (67.46) | ||
| Yes | 128 (23.58) | 101 (21.96) | 27 (32.54) | ||
| Childhood vaccination(s) | 5.426 | 0.020 | |||
| No | 17 (3.13) | 11 (2.39) | 6 (7.23) | ||
| Yes | 526 (96.87) | 449 (97.61) | 77 (92.77) | ||
| Seasonal influenza vaccination | 1.355 | 0.852 | |||
| Never | 140 (25.78) | 122 (26.52) | 18 (21.69) | ||
| Last year | 5 (0.92) | 4 (0.87) | 1 (1.20) | ||
| Current flu season | 2 (0.37) | 2 (0.43) | 0 (0.00) | ||
| Annually | 11 (2.03) | 9 (1.6) | 2 (2.41) | ||
| Can’t remember | 385 (70.90) | 323 (70.22) | 62 (74.70) | ||
| Variables | Total (N = 543) | COVID-19 Vaccine Acceptance | χ2 a | p Value | |
|---|---|---|---|---|---|
| Intended (n = 460) | Undecided/Unwilling (n = 283) | ||||
| Mean (SD) | Mean (SD) | Mean (SD) | |||
| Trust/satisfaction with authorities | 1.01 (0.83) | 1.07 (0.84) | 0.66 (0.67) | 14.56 | 0.000 *** |
| HBM | |||||
| Perceived susceptibility | 3.44 (1.01) | 3.58 (0.97) | 2.69 (0.87) | 57.11 | 0.000 *** |
| Perceived severity | 3.60 (0.87) | 3.64 (0.89) | 3.39 (0.73) | 9.97 | 0.002 ** |
| Perceived benefits | 3.45 (0.87) | 3.56 (0.83) | 2.83 (0.84) | 54.04 | 0.000 *** |
| Perceived barriers (reverse coded) | 3.40 (0.85) | 3.35 (0.83) | 2.72 (0.89) | 14.54 | 0.000 *** |
| Cues to action | 3.19 (0.84) | 3.30 (0.83) | 2.59 (0.68) | 57.03 | 0.000 *** |
| Health motivation | 3.28 (0.91) | 3.28 (0.91) | 3.30 (0.95) | 0.14 | 0.712 |
| TPB | |||||
| Attitude | 2.52 (1.05) | 2.48 (1.07) | 2.80 (0.91) | 10.02 | 0.002 ** |
| Subjective norms | 3.57 (0.89) | 3.64 (0.89) | 3.16 (0.76) | 29.66 | 0.000 *** |
| Perceived behavioral control | 3.89 (0.96) | 3.89 (0.95) | 3.92 (0.99) | 0.04 | 0.834 |
| Self-efficacy (reverse coded) | 2.50 (1.01) | 2.39 (1.01) | 3.10 (0.79) | 40.63 | 0.000 *** |
| Predictors | Odds Ratio (95% Confidence Interval), Effect Size § | ||||
|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
| Sociodemographic factors | |||||
| Age | 0.96 (0.90–1.03), −0.42 | 0.96 (0.89–1.01), −0.04 | 0.95 (0.89–1.02), −0.04 | 0.99 (0.92–1.07), −0.01 | 0.99 (0.91–1.07), −0.01 |
| Occupation | |||||
| Unemployed | Ref. | Ref. | Ref. | Ref. | Ref. |
| Student | 2.01 * (1.10–3.67), 0.69 | 2.06 * (1.11–3.83), 0.72 | 1.89 * (1.00–3.55), 0.63 | 2.41 * (1.12–5.18), 0.88 | 2.56 * (1.16–5.67), 0.94 |
| Public sector | 3.34 (0.00–6.98), 0.78 | 4.2 (0.00–4.65), 0.83 | 4.8 (0.20–5.67), 0.79 | 5.67 (0.00–9.78), 0.75 | 4.23 (0.01–10.09), 0.82 |
| Private sector | 1.28 (0.50–3.24), 0.25 | 1.40 (0.54–3.65), 0.34 | 1.38 (0.52–3.65), 0.32 | 0.86 (0.28–2.59), −0.15 | 0.99 (0.31–3.16), −0.01 |
| Self-employed | 1.41 (0.53–3.79), 0.35 | 1.71 (0.63–4.64), 0.54 | 1.62 (0.59–4.51), 0.48 | 2.25 (0.65-7.79), 0.81 | 3.02 (0.82–11.20), 1.10 |
| Health related factors | |||||
| BMI | |||||
| Underweight | Ref. | Ref. | Ref. | Ref. | |
| Normal weight | 0.54 (0.18–1.59), −0.61 | 0.56 (0.18–1.69), −0.57 | 0.40 (0.12–1.36), −0.91 | 0.41 (0.12–1.45), −0.89 | |
| Overweight | 0.97 (0.27–3.42), −0.03 | 0.97 (0.27–3.49), −0.27 | 0.64 (0.15–2.67), −0.45 | 0.60 (0.14–2.71), −0.50 | |
| Obesity | 0.25 * (0.06–0.89), −1.40 | 0.25* (0.06–0.91), −1.39 | 0.17* (0.04–0.76), −1.78 | 0.14 * (0.02–0.68), −1.98 | |
| Smoking | |||||
| No | Ref. | Ref. | Ref. | Ref. | |
| Yes | 0.56 * (0.33–0.96), −0.57 | 0.58 * (0.34–0.99), −0.54 | 0.66 (0.35–1.24), −0.41 | 0.73 (0.37–1.41), −0.31 | |
| Childhood vaccination | |||||
| No | Ref. | Ref. | Ref. | Ref. | |
| Yes | 3.24 * (1.12–9.32), 1.17 | 3.72 * (1.22–11.35), 1.31 | 2.62 (0.70–9.74), 0.96 | 2.18 (0.53–8.83), 0.78 | |
| Satisfaction with authorities | 1.95 *** (1.39–2.75), 0.67 | 1.32 (0.89–1.96), 0.28 | 1.51 (0.98–2.29), 0.41 | ||
| HBM Dimensions | |||||
| Perceived susceptibility | 1.78 ** (1.26–2.45), 0.57 | 1.73 ** (1.20–2.51), 0.55 | |||
| Perceived severity | 0.68 (0.44–1.06), −0.38 | 0.67 (0.42–1.06), −0.40 | |||
| Perceived benefits | 2.00 ** (1.29–3.09), 0.69 | 2.02 ** (1.26–3.25), 0.71 | |||
| Perceived barriers | 0.49 *** (0.34–0.71), −0.70 | 0.63 * (0.42–0.93), −0.46 | |||
| Cues to action | 2.05 ** (1.3–3.17), 0.72 | 1.98 ** (1.21–3.26), 0.68 | |||
| TPB Dimensions | |||||
| Attitude | 0.89 (0.67–1.21), −0.11 | ||||
| Subjective norms | 1.21 (0.78–1.88), 0.19 | ||||
| Self-efficacy | 0.45 *** (0.33–0.64), −0.80 | ||||
| Model Fit Statistics | |||||
| Cox and Snell pseudo R2 | 0.02 | 0.05 | 0.08 | 0.21 | 0.25 |
| Nagelkerke pseudo R2 | 0.04 | 0.09 | 0.14 | 0.37 | 0.44 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Patwary, M.M.; Bardhan, M.; Disha, A.S.; Hasan, M.; Haque, M.Z.; Sultana, R.; Hossain, M.R.; Browning, M.H.E.M.; Alam, M.A.; Sallam, M. Determinants of COVID-19 Vaccine Acceptance among the Adult Population of Bangladesh Using the Health Belief Model and the Theory of Planned Behavior Model. Vaccines 2021, 9, 1393. https://doi.org/10.3390/vaccines9121393
Patwary MM, Bardhan M, Disha AS, Hasan M, Haque MZ, Sultana R, Hossain MR, Browning MHEM, Alam MA, Sallam M. Determinants of COVID-19 Vaccine Acceptance among the Adult Population of Bangladesh Using the Health Belief Model and the Theory of Planned Behavior Model. Vaccines. 2021; 9(12):1393. https://doi.org/10.3390/vaccines9121393
Chicago/Turabian StylePatwary, Muhammad Mainuddin, Mondira Bardhan, Asma Safia Disha, Mehedi Hasan, Md. Zahidul Haque, Rabeya Sultana, Md. Riad Hossain, Matthew H. E. M. Browning, Md. Ashraful Alam, and Malik Sallam. 2021. "Determinants of COVID-19 Vaccine Acceptance among the Adult Population of Bangladesh Using the Health Belief Model and the Theory of Planned Behavior Model" Vaccines 9, no. 12: 1393. https://doi.org/10.3390/vaccines9121393
APA StylePatwary, M. M., Bardhan, M., Disha, A. S., Hasan, M., Haque, M. Z., Sultana, R., Hossain, M. R., Browning, M. H. E. M., Alam, M. A., & Sallam, M. (2021). Determinants of COVID-19 Vaccine Acceptance among the Adult Population of Bangladesh Using the Health Belief Model and the Theory of Planned Behavior Model. Vaccines, 9(12), 1393. https://doi.org/10.3390/vaccines9121393











