Investigating the Influence of Vaccine Literacy, Vaccine Perception and Vaccine Hesitancy on Israeli Parents’ Acceptance of the COVID-19 Vaccine for Their Children: A Cross-Sectional Study
Abstract
:1. Introduction
2. Methods
2.1. Setting
2.2. Participants
2.3. Ethical Considerations
2.4. Measures
- Demographic data: age, gender, place of birth, area of residency, education, occupation, religious affiliation.
- Participants’ vaccination status—we asked the participants to indicate whether they had been vaccinated for COVID-19.
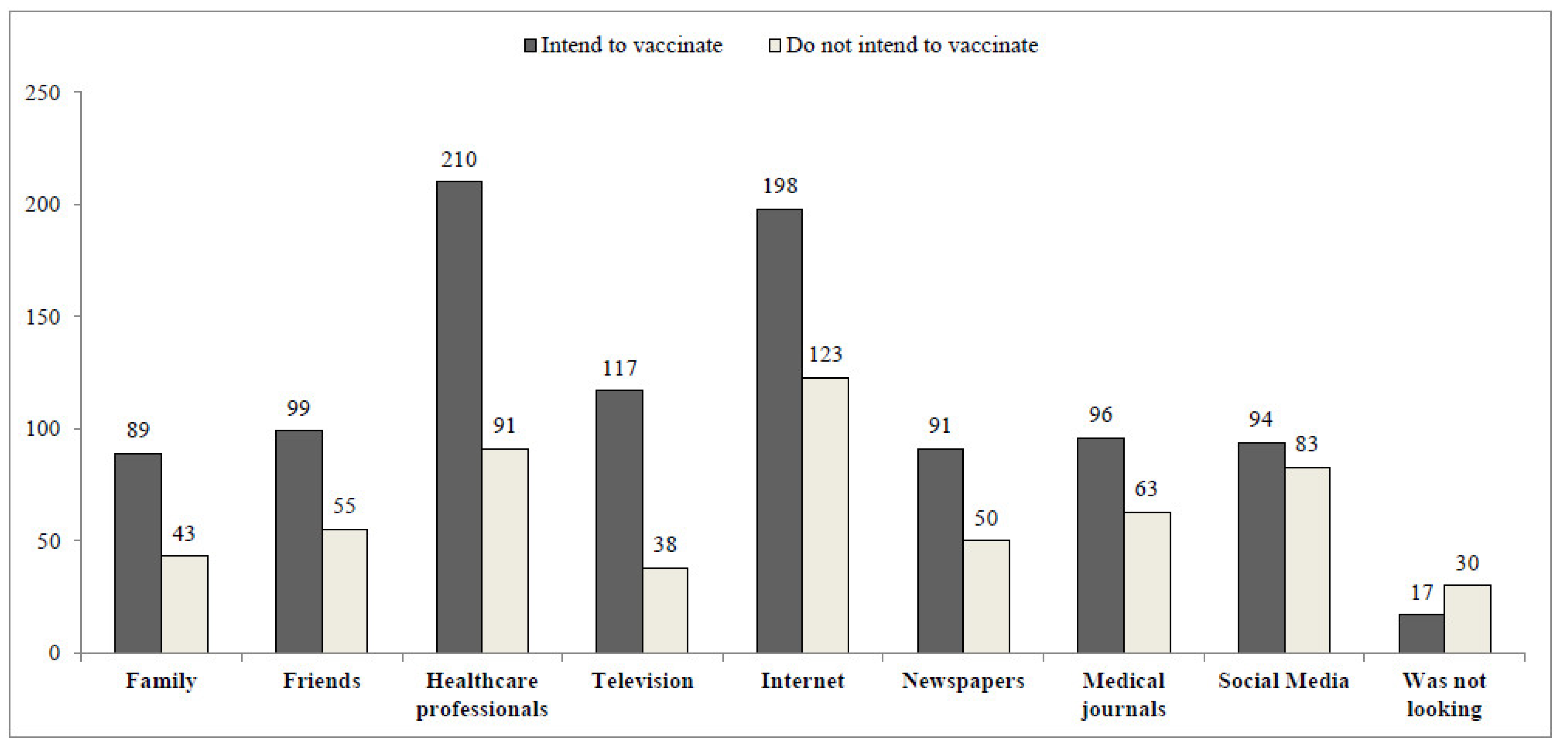
- Participants were asked to indicate which sources of information they had used while searching for information regarding the COVID-19 vaccine. Response options included: family, friends, healthcare professionals, television, internet, newspapers, medical journals, and social media, or “didn’t look for information” (multiple answers were accepted).
- Vaccine literacy was measured using a VL scale [23,27], composed of 12 Likert-type questions. Four items were aimed at assessing functional VL and eight items evaluated interactive-critical VL. Each response was rated with a 4-point Likert scale (4—never, 3—rarely, 2—sometimes, 1—often, for the functional questions; and 1—never, 2—rarely, 3—sometimes, 4—often, for the interactive-critical questions). The score was obtained from the mean value of the answers to each scale (a range of 1–4), a higher value corresponding to a higher VL level.
- COVID-19 vaccine perception was measured using seven Likert-type questions. Each response was rated with a 4-point Likert scale (1—strongly disagree, 4—strongly agree). Examples of items: “There is no need to vaccinate children against COVID-19, as herd immunity has already been achieved in Israel”; “There is no need to vaccinate children against the corona virus, as the disease in children is usually mild”. Mean score of items under each domain were computed, a higher value corresponding to a negative perception of the COVID-19 vaccine.
- Vaccination behavior was measured using a 15-item tool developed from a “5C model” of psychological antecedents to vaccination [19]. Each of the five antecedents, including confidence, complacency, constraints, calculation and collective responsibility, was assessed by three rating items on a 5-point scale (5—strongly agree, 1—strongly disagree). A mean score of items under each domain was computed, with a higher average score indicating stronger agreement regarding the corresponding domain.
- Perceived vaccine hesitancy was measured by a single item asking the participants to grade to what extent they are hesitating to vaccinate their children on an 11-point Likert scale (0 = not hesitant at all, 10 = very hesitant).
- COVID-19 vaccination intention was measured by two items: first we asked the participants if they would be willing to vaccinate their children against COVID-19 (very likely/somewhat likely/somewhat unlikely/definitely not), and then how likely they would be to vaccinate their children on an 11-point Likert scale (0 = definitely no, 10 = definitely yes). When a dichotomous division was required, we coded “very likely/somewhat likely” as “intent to vaccinate” and “somewhat unlikely/definitely not” as “does not intent to vaccinate”.
2.5. Data Analysis
3. Results
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Barouki, R.; Kogevinas, M.; Audouze, K.; Belesova, K.; Bergman, A.; Birnbaum, L.; Boekhold, S.; Denys, S.; Desseille, C.; Drakvik, E.; et al. The COVID-19 pandemic and global environmental change: Emerging research needs. Environ. Int. 2020, 146, 106272. [Google Scholar] [CrossRef]
- Israel: WHO Coronavirus Disease (COVID-19) Dashboard|WHO Coronavirus Disease (COVID-19) Dashboard [Internet]. Available online: https://covid19.who.int/region/euro/country/il (accessed on 16 November 2021).
- Kamidani, S.; Rostad, C.A.; Anderson, E.J. COVID-19 vaccine development: A pediatric perspective. Curr. Opin. Pediatr. 2020, 33, 144–151. [Google Scholar] [CrossRef]
- Yigit, M.; Ozkaya-Parlakay, A.; Senel, E. Evaluation of COVID-19 Vaccine Refusal in Parents. Pediatr. Infect. Dis. J. 2021, 40, e134–e136. [Google Scholar] [CrossRef]
- Leshem, E.; Wilder-Smith, A. COVID-19 vaccine impact in Israel and a way out of the pandemic. Lancet 2021, 397, 1783–1785. [Google Scholar] [CrossRef]
- Muhsen, K.; Cohen, D. COVID-19 vaccination in Israel. Clin Microbiol Infect [Internet]. Clin. Microbiol. Infect. 2021, 27, 1570–1574. [Google Scholar] [CrossRef]
- Glikman, D.; Stein, M.; Shinwell, E.S. Vaccinating children and adolescents against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)—The Israeli experience. Acta Paediatr. Int. J. Paediatr. 2021, 110, 2496–2498. [Google Scholar] [CrossRef]
- Bates, L.C.; Zieff, G.; Stanford, K.; Moore, J.B.; Kerr, Z.Y.; Hanson, E.D.; Barone Gibbs, B.; Kline, C.E.; Stoner, L. COVID-19 Impact on Behaviors across the 24-Hour Day in Children and Adolescents: Physical Activity, Sedentary Behavior, and Sleep. Children 2020, 7, 138. [Google Scholar] [CrossRef]
- COVID-19 Vaccine [Internet]. Available online: https://govextra.gov.il/ministry-of-health/covid19-vaccine/home-en/ (accessed on 9 August 2021).
- Opel, D.J.; Diekema, D.S.; Ross, L.F. Should We Mandate a COVID-19 Vaccine for Children? JAMA Pediatr. 2021, 175, 125–126. [Google Scholar] [CrossRef]
- Kwok, K.O.; Li, K.-K.; Wei, W.I.; Tang, A.; Wong, S.Y.S.; Lee, S.S. Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: A survey. Int. J. Nurs. Stud. 2021, 114, 103854. [Google Scholar] [CrossRef]
- World Health Organization. Ten Threats to Global Health in 2019. 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 10 September 2021).
- Szilagyi, P.G.; Shah, M.D.; Delgado, J.R.; Thomas, K.; Vizueta, N.; Cui, Y.; Vangala, S.; Shetgiri, R. Parents’ Intentions and Perceptions about COVID-19 Vaccination for Their Children: Results from a National Survey. Pediatrics 2021, 148, e2021052335. [Google Scholar] [CrossRef]
- Khubchandani, J.; Sharma, S.; Price, J.H.; Wiblishauser, M.J.; Sharma, M.; Webb, F.J. COVID-19 Vaccination Hesitancy in the United States: A Rapid National Assessment. J. Commun. Health 2021, 46, 270–277. [Google Scholar] [CrossRef]
- Saied, S.M.; Saied, E.M.; Kabbash, I.A.; Abdo, S.A.E. Vaccine hesitancy: Beliefs and barriers associated with COVID-19 vaccination among Egyptian medical students. J. Med. Virol. 2021, 93, 4280–4291. [Google Scholar] [CrossRef]
- Biasio, L.R.; Bonaccorsi, G.; Lorini, C.; Pecorelli, S. Assessing COVID-19 vaccine literacy: A preliminary online survey. Hum. Vaccines Immunother. 2020, 17, 1304–1312. [Google Scholar] [CrossRef]
- Larson, H.J.; Jarrett, C.; Schulz, W.S.; Chaudhuri, M.; Zhou, Y.; Dubé, E.; Schuster, M.; MacDonald, N.E.; Wilson, R. Measuring vaccine hesitancy: The development of a survey tool. Vaccine 2015, 33, 4165–4175. [Google Scholar] [CrossRef] [Green Version]
- Betsch, C.; Habersaat, K.B.; Deshevoi, S.; Heinemeier, D.; Briko, N.; Kostenko, N.; Kocik, J.; Böhm, R.; Zettler, I.; Wiysonge, C.S.; et al. Sample study protocol for adapting and translating the 5C scale to assess the psychological antecedents of vaccination. BMJ Open 2020, 10, e034869. [Google Scholar] [CrossRef] [Green Version]
- Betsch, C.; Schmid, P.; Heinemeier, D.; Korn, L.; Holtmann, C.; Böhm, R. Beyond confidence: Development of a measure assessing the 5C psychological antecedents of vaccination. PLoS ONE 2018, 13, e0208601. [Google Scholar] [CrossRef] [Green Version]
- Gusar, I.; Konjevoda, S.; Babić, G.; Hnatešen, D.; Čebohin, M.; Orlandini, R.; Dželalija, B. Pre-Vaccination COVID-19 Vaccine Literacy in a Croatian Adult Population: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 7073. [Google Scholar] [CrossRef]
- Nutbeam, D. Health literacy as a public health goal: A challenge for contemporary health education and communication strategies into the 21st century. Health Promot. Int. 2000, 15, 259–267. [Google Scholar] [CrossRef] [Green Version]
- Biasio, L.R. Vaccine literacy is undervalued. Hum. Vaccines Immunother. 2019, 15, 2552–2553. [Google Scholar] [CrossRef]
- Biasio, L.R.; Giambi, C.; Fadda, G.; Lorini, C.; Bonaccorsi, G.; D’Ancona, F. Validation of an Italian tool to assess vaccine literacy in adulthood vaccination: A pilot study. Ann. Ig. 2020, 32, 205–222. [Google Scholar]
- Goldman, R.D.; Yan, T.D.; Seiler, M.; Cotanda, C.P.; Brown, J.C.; Klein, E.J.; Hoeffe, J.; Gelernter, R.; Hall, J.E.; Davis, A.L.; et al. Caregiver willingness to vaccinate their children against COVID-19: Cross sectional survey. Vaccine 2020, 38, 7668–7673. [Google Scholar] [CrossRef]
- Zhang, K.C.; Fang, Y.; Cao, H.; Chen, H.; Hu, T.; Chen, Y.Q.; Zhou, X.; Wang, Z. Parental Acceptability of COVID-19 Vaccination for Children Under the Age of 18 Years: Cross-Sectional Online Survey. JMIR Pediatr. Parent. 2020, 3, e24827. [Google Scholar] [CrossRef]
- Gallè, F.; Sabella, E.; Roma, P.; De Giglio, O.; Caggiano, G.; Tafuri, S.; Da Molin, G.; Ferracuti, S.; Montagna, M.; Liguori, G.; et al. Knowledge and Acceptance of COVID-19 Vaccination among Undergraduate Students from Central and Southern Italy. Vaccines 2021, 9, 638. [Google Scholar] [CrossRef]
- Biasio, L.; Bonaccorsi, G.; Lorini, C.; Mazzini, D.; Pecorelli, S. Italian Adults’ Likelihood of Getting COVID-19 Vaccine: A Second Online Survey. Vaccines 2021, 9, 268. [Google Scholar] [CrossRef] [PubMed]
- Yılmaz, M.; Sahin, M.K. Parents’ willingness and attitudes concerning the COVID-19 vaccine: A cross-sectional study. Int. J. Clin. Pract. 2021, 75, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.; Tu, P.; Beitsch, L.M. Confidence and Receptivity for COVID-19 Vaccines: A Rapid Systematic Review. Vaccines 2020, 9, 16. [Google Scholar] [CrossRef] [PubMed]
- Akarsu, B.; Özdemir, D.C.; Baser, D.A.; Aksoy, H.; Fidancı, İ.; Cankurtaran, M. While studies on COVID-19 vaccine is ongoing, the public’s thoughts and attitudes to the future COVID-19 vaccine. Int. J. Clin. Pract. 2021, 75, 1–10. [Google Scholar] [CrossRef]
- Redmond, N.; Baer, H.J.; Clark, C.R.; Lipsitz, S.; Hicks, L.S. Sources of Health Information Related to Preventive Health Behaviors in a National Study. Am. J. Prev. Med. 2010, 38, 620–627.e2. [Google Scholar] [CrossRef] [Green Version]
- Rains, S.A. Perceptions of Traditional Information Sources and Use of the World Wide Web to Seek Health Information: Findings from the Health Information National Trends Survey. J. Health Commun. 2007, 12, 667–680. [Google Scholar] [CrossRef]
- Smith, D. Health care consumer’s use and trust of health information sources. J. Commun. Health 2011, 4, 200–210. [Google Scholar] [CrossRef]
- Aharon, A.A.; Nehama, H.; Rishpon, S.; Baron-Epel, O. Parents with high levels of communicative and critical health literacy are less likely to vaccinate their children. Patient Educ. Couns. 2017, 100, 768–775. [Google Scholar] [CrossRef]
- Patil, U.; Kostareva, U.; Hadley, M.; Manganello, J.; Okan, O.; Dadaczynski, K.; Massey, P.; Agner, J.; Sentell, T. Health Literacy, Digital Health Literacy, and COVID-19 Pandemic Attitudes and Behaviors in U.S. College Students: Implications for Interventions. Int. J. Environ. Res. Public Health 2021, 18, 3301. [Google Scholar] [CrossRef] [PubMed]
- Gorman, D.; Bielecki, K.; Larson, H.; Willocks, L.; Craig, J.; Pollock, K. Comparing vaccination hesitancy in Polish migrant parents who accept or refuse nasal flu vaccination for their children. Vaccine 2020, 38, 2795–2799. [Google Scholar] [CrossRef] [PubMed]
- Dubé, E.; Laberge, C.; Guay, M.; Bramadat, P.; Roy, R.; Bettinger, J. H_Dube_2013_Vaccine hesitancy overview. Hum. Vaccin. Immunother. 2013, 9, 1763–1773. [Google Scholar] [CrossRef] [PubMed]
- Sowa, P.; Kiszkiel, L.; Laskowski, P.; Alimowski, M.; Szczerbiński, L.; Paniczko, M.; Moniuszko-Malinowska, A.; Kamiński, K. COVID-19 Vaccine Hesitancy in Poland—Multifactorial Impact Trajectories. Vaccines 2021, 9, 876. [Google Scholar] [CrossRef]

| Predictor | COVID-19 Vaccination Acceptance | |||
|---|---|---|---|---|
| Number (%) | OR [95%CI] | p Value | ||
| Gender | Female | 401 (77.1) | 1.67 [0.92, 3.03] | 0.09 |
| Male | 119 (22.9) | [1] | ||
| Age, estimate for 1 year | Mean (±SD) | 44.76 (8.09) | 1.02 [0.98, 1.06] | 0.15 |
| Place of birth | Israel | 377 (72.5) | 1.19 [0.60, 2.36] | 0.94 |
| Other | 143 (27.5) | [1] | ||
| Area of residency | Central Israel | 251 (48.3) | 1.13 [0.65, 1.96] | 0.66 |
| Other | 269 (51.7) | [1] | ||
| Education | Academic | 383 (73.7) | 1.41 [0.63, 3.05] | 0.41 |
| Other | 137 (26.3) | [1] | ||
| Occupation | Healthcare workers | 179 (34.4) | 1.36 [0.87, 2.13] | 0.18 |
| Other | 341 (65.6) | [1] | ||
| Religious affiliation | Secular | 208 (40.0) | 1.05 [0.59, 1.86] | 0.87 |
| Other | 312 (60.0) | [1] | ||
| COVID-19 vaccination status | Yes | 395 (76.0) | 32.89 [13.11, 82.54] | <0.001 |
| No | 125 (24.0) | [1] |
| Parents’ Intention to Vaccinate Their Children | ||
|---|---|---|
| Yes | No | |
| Parents’ vaccination status (%) | ||
| Yes | 317 (61.0%) | 78 (15.0%) |
| No | 49 (9.4%) | 76 (14.6%) |
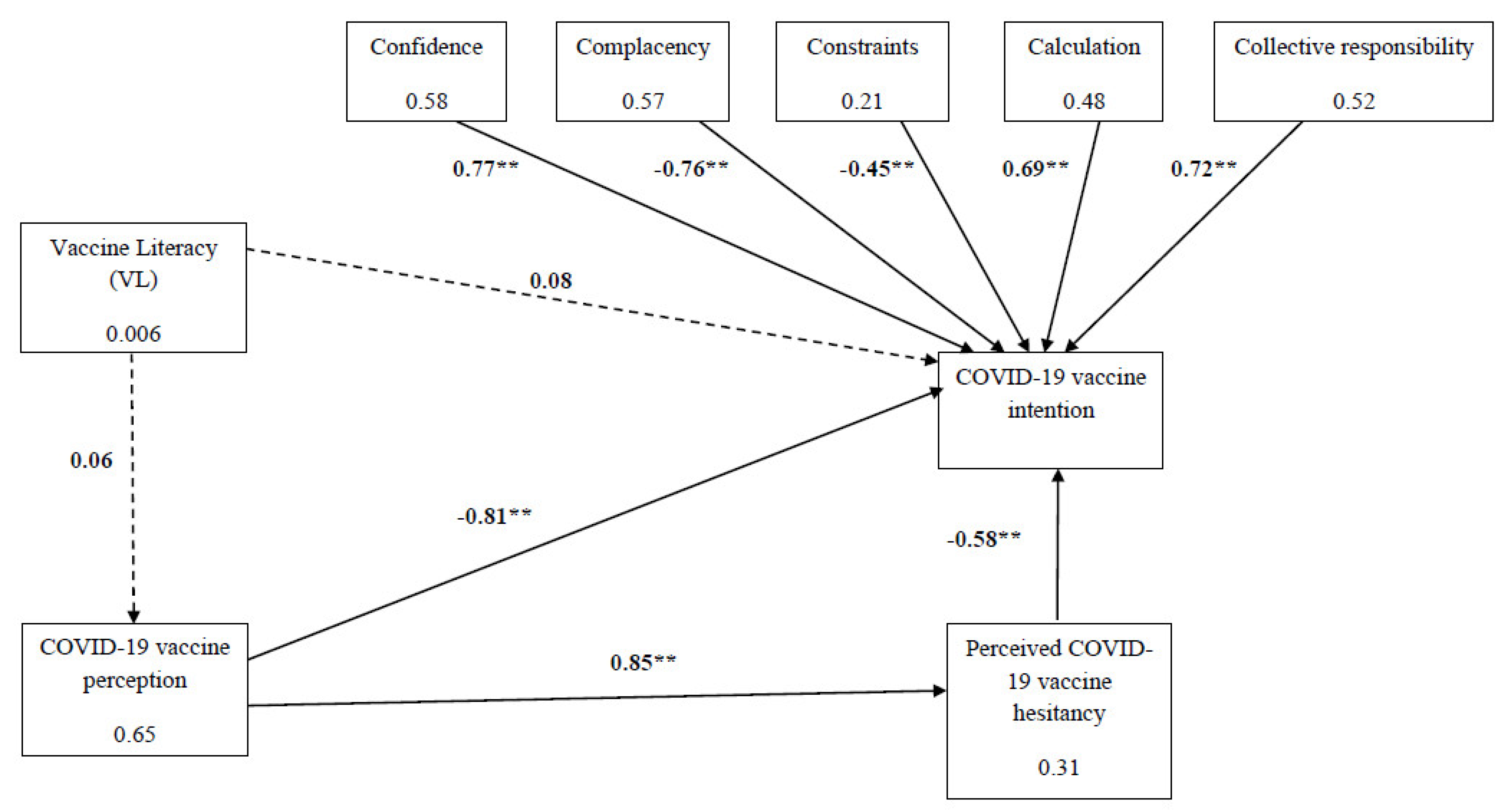
| Variable Mean Scores (±SD) | Likelihood to Vaccinate Their Children against COVID-19 | p Value | Cohen’s d | |
|---|---|---|---|---|
| Very Likely/Somewhat Likely (n = 366) | Very Unlikely/Definitely not (n = 154) | |||
| VL Functional skills | 3.27 (±0.61) | 3.18 (±0.60) | 0.13 | 0.15 |
| VL Interactive/critical skills | 2.86 (±0.66) | 2.80 (±0.62) | 0.31 | 0.09 |
| VL Total | 3.07 (±0.44) | 2.99 (±0.47) | 0.06 | 0.18 |
| COVID-19 vaccine perception | 2.26 (±0.75) | 3.44 (±0.68) | <0.001 | 1.68 |
| 5C Model: | ||||
| Confidence | 3.81 (±1.13) | 2.06 (±1.10) | <0.001 | 1.60 |
| Complacency | 2.17 (±1.08) | 3.86 (±1.09) | <0.001 | 1.56 |
| Constraints | 2.55 (±0.98) | 3.33 (±0.94) | <0.001 | 0.81 |
| Calculation | 3.19 (±0.95) | 1.88 (±0.84) | <0.001 | −1.43 |
| Collective responsibility | 3.96 (±1.04) | 2.51 (±1.06) | <0.001 | −1.39 |
| Perceived COVID-19 vaccine hesitancy | 4.68 (±2.71) | 7.53 (±2.37) | <0.001 | 1.09 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gendler, Y.; Ofri, L. Investigating the Influence of Vaccine Literacy, Vaccine Perception and Vaccine Hesitancy on Israeli Parents’ Acceptance of the COVID-19 Vaccine for Their Children: A Cross-Sectional Study. Vaccines 2021, 9, 1391. https://doi.org/10.3390/vaccines9121391
Gendler Y, Ofri L. Investigating the Influence of Vaccine Literacy, Vaccine Perception and Vaccine Hesitancy on Israeli Parents’ Acceptance of the COVID-19 Vaccine for Their Children: A Cross-Sectional Study. Vaccines. 2021; 9(12):1391. https://doi.org/10.3390/vaccines9121391
Chicago/Turabian StyleGendler, Yulia, and Lani Ofri. 2021. "Investigating the Influence of Vaccine Literacy, Vaccine Perception and Vaccine Hesitancy on Israeli Parents’ Acceptance of the COVID-19 Vaccine for Their Children: A Cross-Sectional Study" Vaccines 9, no. 12: 1391. https://doi.org/10.3390/vaccines9121391
APA StyleGendler, Y., & Ofri, L. (2021). Investigating the Influence of Vaccine Literacy, Vaccine Perception and Vaccine Hesitancy on Israeli Parents’ Acceptance of the COVID-19 Vaccine for Their Children: A Cross-Sectional Study. Vaccines, 9(12), 1391. https://doi.org/10.3390/vaccines9121391






