Developing a Stabilizing Formulation of a Live Chimeric Dengue Virus Vaccine Dry Coated on a High-Density Microarray Patch
Abstract
:1. Introduction
2. Materials and Methods
2.1. Animal Ethics
2.2. Cell Lines
2.3. bDENV2 Chimeric Virus Propagation and Purification
2.4. C8-Antigen-Capture Enzyme-Linked Immunosorbent Assay (ELISA)
2.5. Excipient Screening Studies to Identify Stabilizing Excipient for Dry Down and Storage
2.5.1. Excipient Preparation
2.5.2. bDENV2 Drying and Storage
2.5.3. bDENV2 Reconstitution and Recovery for Analytical Testing
2.5.4. Recovery of bDENV2 Based on C8-Antigen-Capture ELISA
2.5.5. Recovery of bDENV2 Based on 50% Tissue Culture Infectious Dose (TCID50) Assay
2.5.6. Immunoplaque Staining
2.6. HD-MAPs Coating and Storage
2.7. Scanning Electron Microscopy (SEM) of HD-MAPs
2.8. Evaluation of Stored bDENV2-Coated HD-MAP
2.9. DENV-Specific IgG ELISA
2.10. DENV Plaque Reduction Neutralization Tests (PRNTs)
2.11. Optimization of Wear Time of HD-MAP after Application
2.12. Delivery Efficiencies of the Different Wear Times of HD-MAP
3. Results
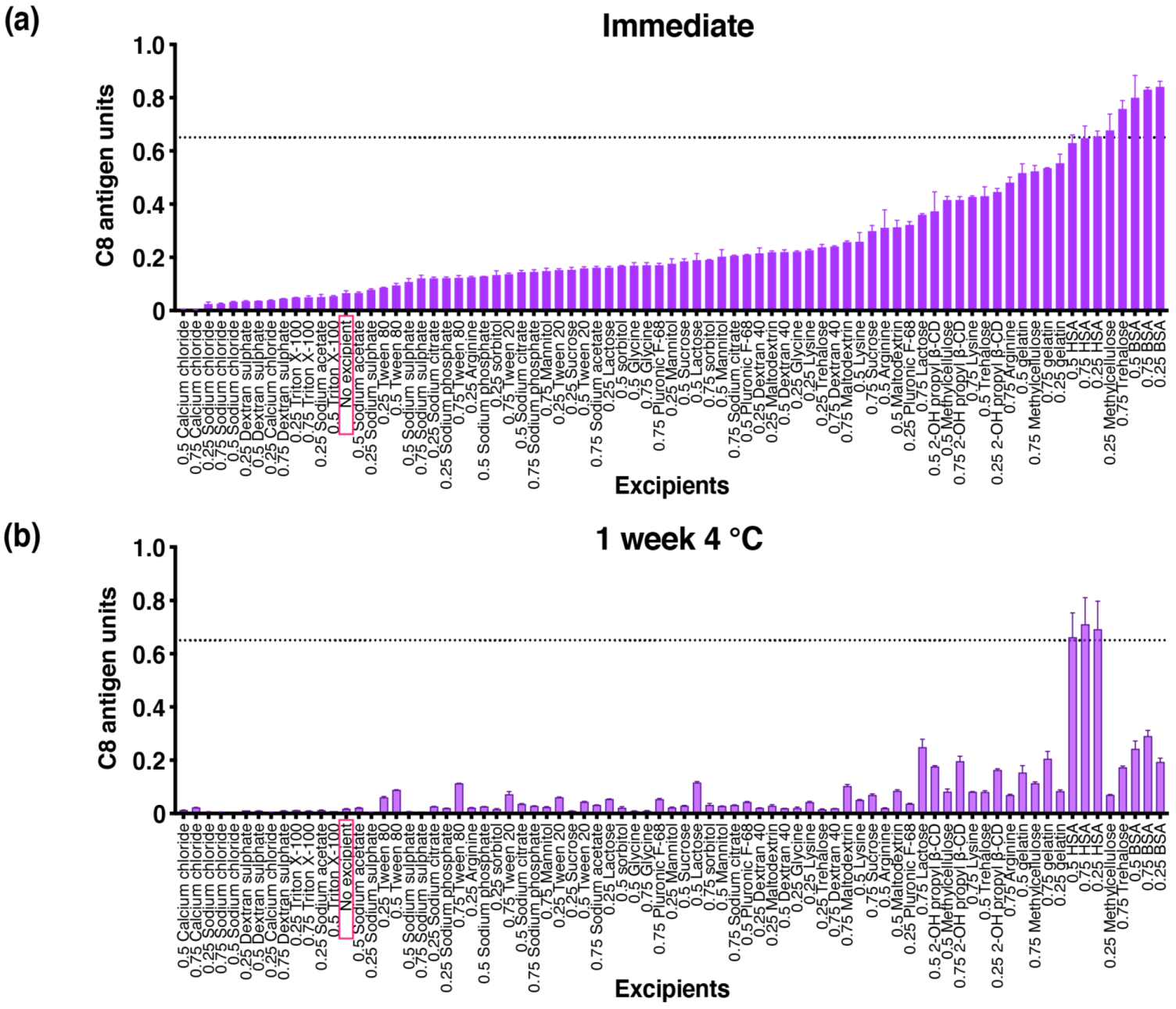
3.1. Initial Excipient Screening Studies to Identify Stabilizing Excipients for Dry-Down and Storage
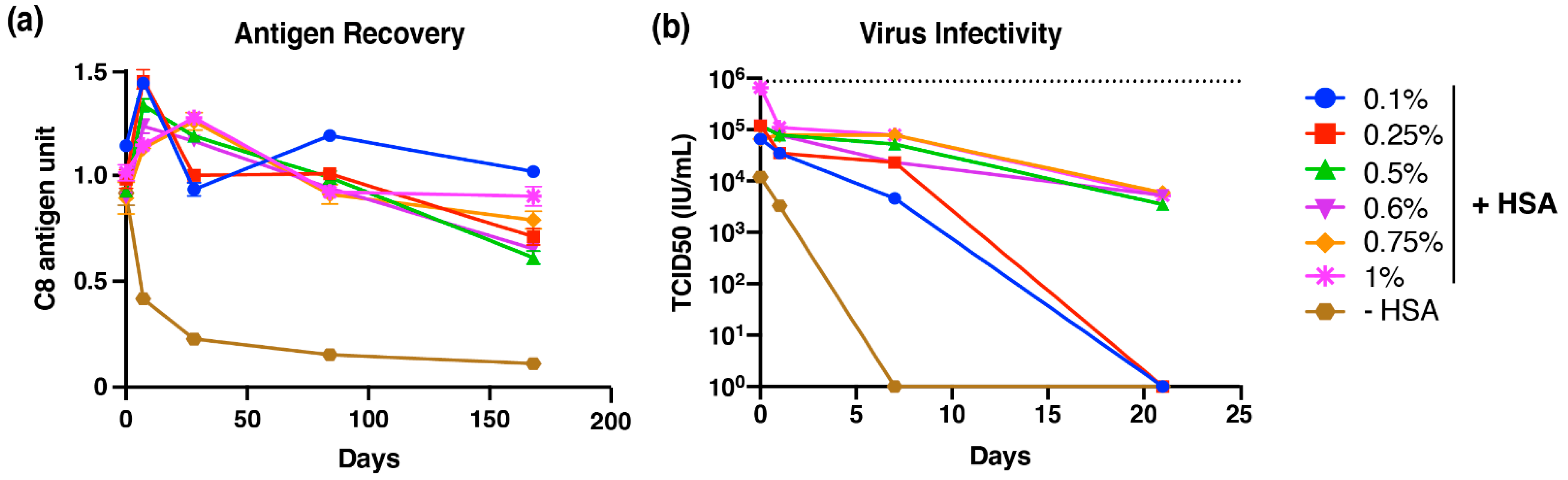
3.2. Optimizing Dry-Down and Reconstitution Buffers
3.3. Long-Term Stability of bDENV2 in a Dried State
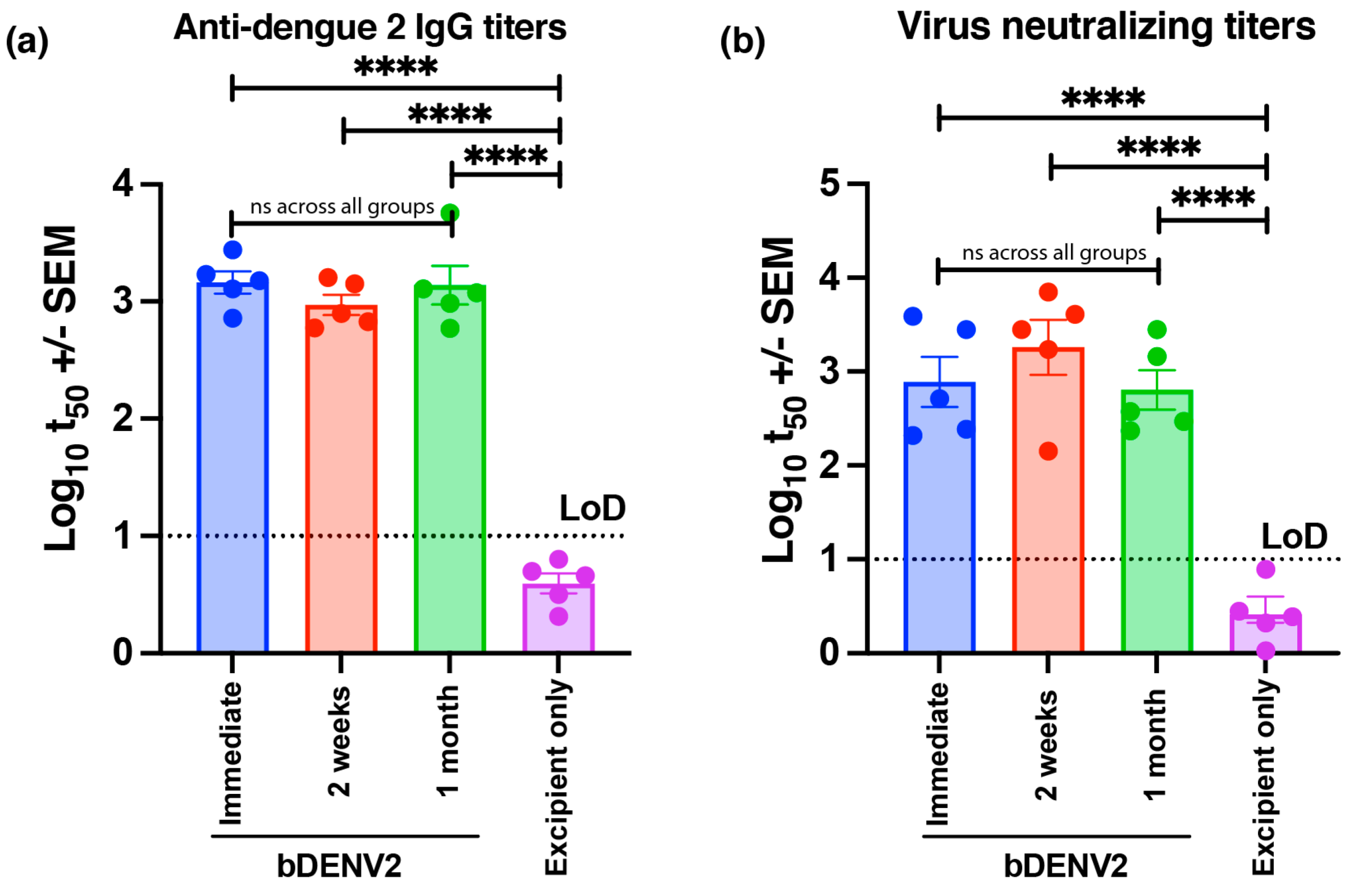
3.4. Store and Patch Study: The Delivery of Stable bDENV2 via HD-MAP
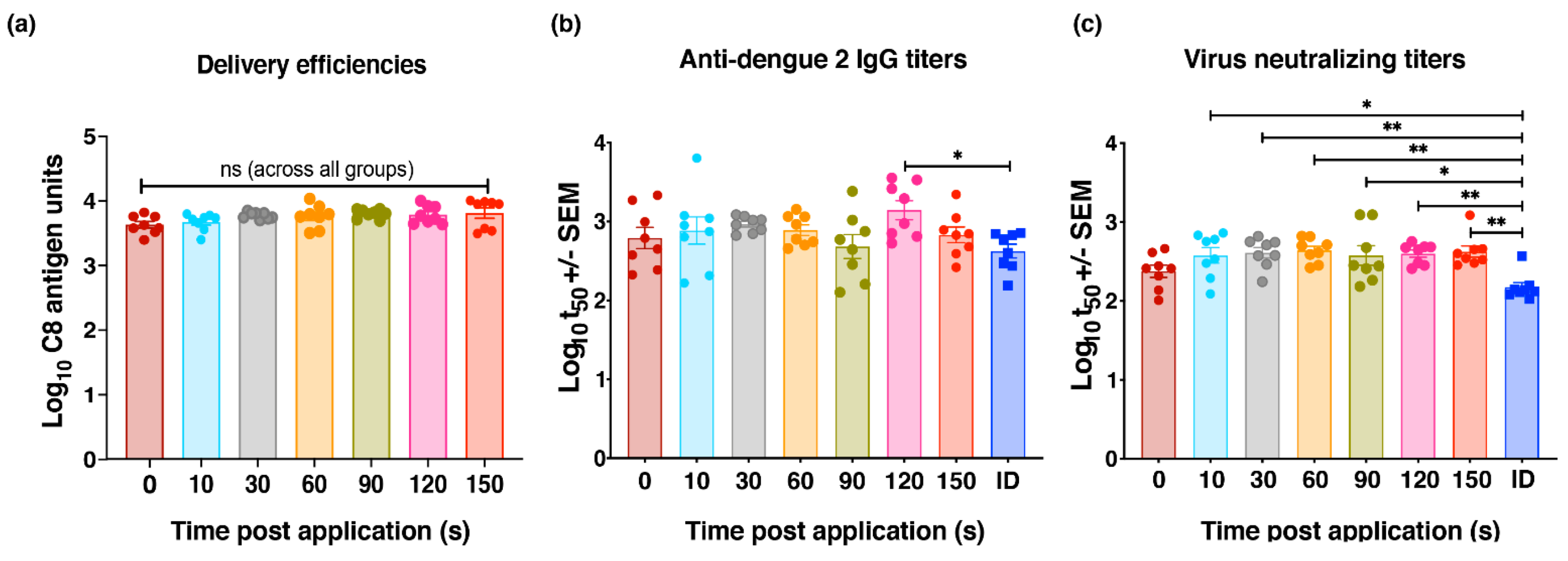
3.5. Optimization of HD-MAP Wear Time
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bhatt, S.; Gething, P.; Brady, O.; Messina, J.P.; Farlow, A.W.; Moyes, C.; Drake, J.; Brownstein, J.S.; Hoen, A.G.; Sankoh, O.; et al. The global distribution and burden of dengue. Nature 2013, 496, 504–507. [Google Scholar] [CrossRef]
- Holbrook, M.R. Historical Perspectives on Flavivirus Research. Viruses 2017, 9, 97. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guzman, M.G.; Gubler, D.J.; Izquierdo, A.; Martinez, E.; Halstead, S.B. Dengue infection. Nat. Rev. Dis. Prim. 2016, 2, 16055. [Google Scholar] [CrossRef] [PubMed]
- Islam, R.; Salahuddin, M.; Ayubi, S.; Hossain, T.; Majumder, A.; Taylor-Robinson, A.W.; Mahmud-Al-Rafat, A. Dengue epidemiology and pathogenesis: Images of the future viewed through a mirror of the past. Virol. Sin. 2015, 30, 326–343. [Google Scholar] [CrossRef] [PubMed]
- Messina, J.P.; Brady, O.; Scott, T.W.; Zou, C.; Pigott, D.; Duda, K.A.; Bhatt, S.; Katzelnick, L.; Howes, R.E.; Battle, K.; et al. Global spread of dengue virus types: Mapping the 70 year history. Trends Microbiol. 2014, 22, 138–146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Osorio, J.E.; Partidos, C.D.; Wallace, D.; Stinchcomb, D.T. Development of a recombinant, chimeric tetravalent dengue vaccine candidate. Vaccine 2015, 33, 7112–7120. [Google Scholar] [CrossRef]
- Collins, M.H.; Metz, S.W. Progress and Works in Progress: Update on Flavivirus Vaccine Development. Clin. Ther. 2017, 39, 1519–1536. [Google Scholar] [CrossRef] [Green Version]
- Durbin, A.P.; Kirkpatrick, B.D.; Pierce, K.K.; Elwood, D.; Larsson, C.J.; Lindow, J.; Tibery, C.; Sabundayo, B.P.; Shaffer, D.; Talaat, K.R.; et al. A Single Dose of Any of Four Different Live Attenuated Tetravalent Dengue Vaccines Is Safe and Immunogenic in Flavivirus-naive Adults: A Randomized, Double-blind Clinical Trial. J. Infect. Dis. 2013, 207, 957–965. [Google Scholar] [CrossRef] [PubMed]
- Limited, T.P.C. Takeda Begins Regulatory Submissions for Dengue Vaccine Candidate in EU and Dengue-Endemic Countries. Available online: https://www.takeda.com/newsroom/newsreleases/2021/takeda-begins-regulatory-submissions-for-dengue-vaccine-candidate-in-eu--and-dengue-endemic-countries/ (accessed on 24 October 2021).
- Combadiere, B.; Liard, C. Transcutaneous and intradermal vaccination. Hum. Vaccines 2011, 7, 811–827. [Google Scholar] [CrossRef] [Green Version]
- Nightingale, Z.D.; Patkar, C.; Rothman, A.L. Viral replication and paracrine effects result in distinct, functional responses of dendritic cells following infection with dengue 2 virus. J. Leukoc. Biol. 2008, 84, 1028–1038. [Google Scholar] [CrossRef]
- Laurent, P.E.; Bonnet, S.; Alchas, P.; Regolini, P.; Mikszta, J.A.; Pettis, R.; Harvey, N.G. Evaluation of the clinical performance of a new intradermal vaccine administration technique and associated delivery system. Vaccine 2007, 25, 8833–8842. [Google Scholar] [CrossRef] [PubMed]
- Levin, Y.; Kochba, E.; Hung, I.; Kenney, R. Intradermal vaccination using the novel microneedle device MicronJet600: Past, present, and future. Hum. Vaccines Immunother. 2015, 11, 991–997. [Google Scholar] [CrossRef] [Green Version]
- Depelsenaire, A.C.; Meliga, S.C.; McNeilly, C.L.; Pearson, F.E.; Coffey, J.W.; Haigh, O.L.; Flaim, C.J.; Frazer, I.H.; Kendall, M.A. Colocalization of Cell Death with Antigen Deposition in Skin Enhances Vaccine Immunogenicity. J. Investig. Dermatol. 2014, 134, 2361–2370. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fernando, G.J.; Chen, X.; Primiero, C.A.; Yukiko, S.R.; Fairmaid, E.J.; Corbett, H.J.; Frazer, I.H.; Brown, L.E.; Kendall, M.A. Nanopatch targeted delivery of both antigen and adjuvant to skin synergistically drives enhanced antibody responses. J. Control. Release 2012, 159, 215–221. [Google Scholar] [CrossRef]
- Fernando, G.; Chen, X.; Prow, T.; Crichton, M.; Fairmaid, E.J.; Roberts, M.; Frazer, I.; Brown, L.; Kendall, M.A.F. Potent Immunity to Low Doses of Influenza Vaccine by Probabilistic Guided Micro-Targeted Skin Delivery in a Mouse Model. PLoS ONE 2010, 5, e10266. [Google Scholar] [CrossRef]
- Forster, A.H.; Witham, K.; Depelsenaire, A.C.I.; Veitch, M.; Wells, J.W.; Wheatley, A.; Pryor, M.; Lickliter, J.D.; Francis, B.; Rockman, S.; et al. Safety, tolerability, and immunogenicity of influenza vaccination with a high-density microarray patch: Results from a randomized, controlled phase I clinical trial. PLoS Med. 2020, 17, e1003024. [Google Scholar] [CrossRef] [PubMed]
- Muller, D.A.; Depelsenaire, A.C.I.; Shannon, A.E.; Watterson, D.; Corrie, S.R.; Owens, N.S.; Agyei-Yeboah, C.; Cheung, S.T.M.; Zhang, J.; Fernando, G.J.P.; et al. Efficient Delivery of Dengue Virus Subunit Vaccines to the Skin by Microprojection Arrays. Vaccines 2019, 7, 189. [Google Scholar] [CrossRef] [Green Version]
- Muller, D.A.; Fernando, G.J.P.; Owens, N.S.; Agyei-Yeboah, C.; Wei, J.; Depelsenaire, A.; Forster, A.; Fahey, P.; Weldon, W.C.; Oberste, M.S.; et al. High-density microprojection array delivery to rat skin of low doses of trivalent inactivated poliovirus vaccine elicits potent neutralising antibody responses. Sci. Rep. 2017, 7, 1–10. [Google Scholar] [CrossRef]
- Muller, D.A.; Pearson, F.E.; Fernando, G.; Agyei-Yeboah, C.; Owens, N.S.; Corrie, S.; Crichton, M.; Wei, J.; Weldon, W.C.; Oberste, M.S.; et al. Inactivated poliovirus type 2 vaccine delivered to rat skin via high density microprojection array elicits potent neutralising antibody responses. Sci. Rep. 2016, 6, 22094. [Google Scholar] [CrossRef]
- Ng, H.-I.; Tuong, Z.K.; Fernando, G.J.P.; Depelsenaire, A.; Meliga, S.C.; Frazer, I.H.; Kendall, M.A.F. Microprojection arrays applied to skin generate mechanical stress, induce an inflammatory transcriptome and cell death, and improve vaccine-induced immune responses. npj Vaccines 2019, 4, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Ng, H.I.; Fernando, G.; Depelsenaire, A.; Kendall, M.A.F. Potent response of QS-21 as a vaccine adjuvant in the skin when delivered with the Nanopatch, resulted in adjuvant dose sparing. Sci. Rep. 2016, 6, 29368. [Google Scholar] [CrossRef]
- Ng, H.I.; Fernando, G.J.; Kendall, M.A. Induction of potent CD8+ T cell responses through the delivery of subunit protein vaccines to skin antigen-presenting cells using densely packed microprojection arrays. J. Control. Release 2012, 162, 477–484. [Google Scholar] [CrossRef] [PubMed]
- Fernando, G.J.; Hickling, J.; Flores, C.M.J.; Griffin, P.; Anderson, C.D.; Skinner, R.; Davies, C.; Witham, K.; Pryor, M.; Bodle, J.; et al. Safety, tolerability, acceptability and immunogenicity of an influenza vaccine delivered to human skin by a novel high-density microprojection array patch (Nanopatch™). Vaccine 2018, 36, 3779–3788. [Google Scholar] [CrossRef]
- Muller, D.A.; Henricson, J.; Ben Baker, S.; Togö, T.; Flores, C.M.J.; Lemaire, P.A.; Forster, A.; Anderson, C.D. Innate local response and tissue recovery following application of high density microarray patches to human skin. Sci. Rep. 2020, 10, 1–9. [Google Scholar] [CrossRef]
- McMillan, C.L.D.; Choo, J.J.Y.; Idris, A.; Supramaniam, A.; Modhiran, N.; Amarilla, A.A.; Isaacs, A.; Cheung, S.T.M.; Liang, B.; Bielefeldt-Ohmann, H.; et al. Complete protection by a single-dose skin patch–delivered SARS-CoV-2 spike vaccine. Sci. Adv. 2021, 7. [Google Scholar] [CrossRef]
- Choo, J.J.Y.; Vet, L.J.; McMillan, C.L.D.; Harrison, J.J.; Scott, C.A.P.; Depelsenaire, A.C.I.; Fernando, G.J.P.; Watterson, D.; Hall, R.A.; Young, P.R.; et al. A chimeric dengue virus vaccine candidate delivered by high density microarray patches protects against infection in mice. npj Vaccines 2021, 6, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Kolluru, C.; Gomaa, Y.; Prausnitz, M.R. Development of a thermostable microneedle patch for polio vaccination. Drug Deliv. Transl. Res. 2018, 9, 192–203. [Google Scholar] [CrossRef] [Green Version]
- Mistilis, M.J.; Bommarius, A.S.; Prausnitz, M.R. Development of a Thermostable Microneedle Patch for Influenza Vaccination. J. Pharm. Sci. 2015, 104, 740–749. [Google Scholar] [CrossRef] [Green Version]
- Wan, Y.; Gupta, V.; Bird, C.; Pullagurla, S.R.; Fahey, P.; Forster, A.; Volkin, D.B.; Joshi, S.B. Formulation Development and Improved Stability of a Combination Measles and Rubella Live-Viral Vaccine Dried for Use in the NanopatchTM Microneedle Delivery System. Hum. Vaccines Immunother. 2021, 17, 2501–2516. [Google Scholar] [CrossRef] [PubMed]
- Wan, Y.; Hickey, J.M.; Bird, C.; Witham, K.; Fahey, P.; Forster, A.; Joshi, S.B.; Volkin, D.B. Development of Stabilizing Formulations of a Trivalent Inactivated Poliovirus Vaccine in a Dried State for Delivery in the Nanopatch™ Microprojection Array. J. Pharm. Sci. 2018, 107, 1540–1551. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wong, Y.H.; Kumar, A.; Liew, C.W.; Tharakaraman, K.; Srinivasaraghavan, K.; Sasisekharan, R.; Verma, C.; Lescar, J. Molecular basis for dengue virus broad cross-neutralization by humanized monoclonal antibody 513. Sci. Rep. 2018, 8, 1–17. [Google Scholar] [CrossRef]
- Li, J.; Watterson, D.; Chang, C.-W.; Che, X.-Y.; Li, X.-Q.; Ericsson, D.; Qiu, L.-W.; Cai, J.-P.; Chen, J.; Fry, S.R.; et al. Structural and Functional Characterization of a Cross-Reactive Dengue Virus Neutralizing Antibody that Recognizes a Cryptic Epitope. Structure 2017, 26, 51–59.e4. [Google Scholar] [CrossRef] [Green Version]
- Reed, L.; Muench, H. A Simple Method of Estimating Fifty per Cent Endpoints12. Am. J. Epidemiol. 1938, 27, 493–497. [Google Scholar] [CrossRef]
- Edens, C.; Collins, M.L.; Goodson, J.L.; Rota, P.A.; Prausnitz, M.R. A microneedle patch containing measles vaccine is immunogenic in non-human primates. Vaccine 2015, 33, 4712–4718. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dejnirattisai, W.; Wongwiwat, W.; Supasa, S.; Zhang, X.; Dai, X.; Rouvinski, A.; Jumnainsong, A.; Edwards, C.; Quyen, N.T.H.; Duangchinda, T.; et al. A new class of highly potent, broadly neutralizing antibodies isolated from viremic patients infected with dengue virus. Nat. Immunol. 2014, 16, 170–177. [Google Scholar] [CrossRef] [Green Version]
- Beale, A.J.; Mason, P.J. The measurement of the D-antigen in poliovirus preparations. J. Hyg. 1962, 60, 113–121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Turvey, M.E.; Uppu, D.S.; Sharif, A.R.M.; Bidet, K.; Alonso, S.; Ooi, E.E.; Hammond, P.T. Microneedle-based intradermal delivery of stabilized dengue virus. Bioeng. Transl. Med. 2019, 4, e10127. [Google Scholar] [CrossRef] [PubMed]
- Arnemo, M.; Watle, S.S.V.; Schoultz, K.M.; Vainio, K.; Norheim, G.; Moorthy, V.; Fast, P.; Røttingen, J.-A.; Gjøen, T. Stability of a Vesicular Stomatitis Virus–Vectored Ebola Vaccine. J. Infect. Dis. 2015, 213, 930–933. [Google Scholar] [CrossRef]
- Faust, S.N.; Le Roy, M.; Pancharoen, C.; Weber, M.A.R.; Cathie, K.; Behre, U.; Bernatoniene, J.; Snape, M.D.; Helm, K.; Pech, C.E.M.; et al. Safety and immunogenicity of a varicella vaccine without human serum albumin (HSA) versus a HSA-containing formulation administered in the second year of life: A phase III, double-blind, randomized study. BMC Pediatr. 2019, 19, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Wiedmann, R.T.; Reisinger, K.S.; Hartzel, J.; Malacaman, E.; Senders, S.D.; Giacoletti, K.E.; Shaw, E.; Kuter, B.J.; Schödel, F.; Musey, L.K. M-M-R®II manufactured using recombinant human albumin (rHA) and M-M-R®II manufactured using human serum albumin (HSA) exhibit similar safety and immunogenicity profiles when administered as a 2-dose regimen to healthy children. Vaccine 2015, 33, 2132–2140. [Google Scholar] [CrossRef]
- Wiggan, O.; Livengood, J.A.; Silengo, S.J.; Kinney, R.M.; Osorio, J.E.; Huang, C.Y.-H.; Stinchcomb, D.T. Novel formulations enhance the thermal stability of live-attenuated flavivirus vaccines. Vaccine 2011, 29, 7456–7462. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raymond, C.R.; Paul, J.S.; Walter, G.C.; Marian, E.Q. Handbook of Pharmaceutical Excipients—7th Edition. Pharm. Dev. Technol. 2013, 18, 544. [Google Scholar] [CrossRef]
- Raphael, A.P.; Meliga, S.C.; Chen, X.; Fernando, G.J.; Flaim, C.; Kendall, M.A. Depth-resolved characterization of diffusion properties within and across minimally-perturbed skin layers. J. Control. Release 2013, 166, 87–94. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choo, J.J.Y.; McMillan, C.L.D.; Fernando, G.J.P.; Hall, R.A.; Young, P.R.; Hobson-Peters, J.; Muller, D.A. Developing a Stabilizing Formulation of a Live Chimeric Dengue Virus Vaccine Dry Coated on a High-Density Microarray Patch. Vaccines 2021, 9, 1301. https://doi.org/10.3390/vaccines9111301
Choo JJY, McMillan CLD, Fernando GJP, Hall RA, Young PR, Hobson-Peters J, Muller DA. Developing a Stabilizing Formulation of a Live Chimeric Dengue Virus Vaccine Dry Coated on a High-Density Microarray Patch. Vaccines. 2021; 9(11):1301. https://doi.org/10.3390/vaccines9111301
Chicago/Turabian StyleChoo, Jovin J. Y., Christopher L. D. McMillan, Germain J. P. Fernando, Roy A. Hall, Paul R. Young, Jody Hobson-Peters, and David A. Muller. 2021. "Developing a Stabilizing Formulation of a Live Chimeric Dengue Virus Vaccine Dry Coated on a High-Density Microarray Patch" Vaccines 9, no. 11: 1301. https://doi.org/10.3390/vaccines9111301
APA StyleChoo, J. J. Y., McMillan, C. L. D., Fernando, G. J. P., Hall, R. A., Young, P. R., Hobson-Peters, J., & Muller, D. A. (2021). Developing a Stabilizing Formulation of a Live Chimeric Dengue Virus Vaccine Dry Coated on a High-Density Microarray Patch. Vaccines, 9(11), 1301. https://doi.org/10.3390/vaccines9111301







