The Potential Adjuvanticity of CAvant®SOE for Foot-and-Mouth Disease Vaccine
Abstract
1. Introduction
2. Materials and Methods
2.1. Preparation of the Vaccines
2.2. Immunization in Mice
2.3. Immunization and FMDV Challenge in Pigs
2.4. Enzyme-Linked Immunosorbent Assay (ELISA)
2.5. Splenocytes Isolation and Cell-Mediated Immune Responses
2.6. Virus Neutralization Test
2.7. Analysis of FMD Replication in Pigs
2.8. Statistical Analysis
3. Results
3.1. CAvant®SOE Enhances FMDV-Specific Humoral Immune Responses in Mice
3.2. CAvant®SOE Balances FMDV-Specific Th1 and Th2 Immune Responses in Mice
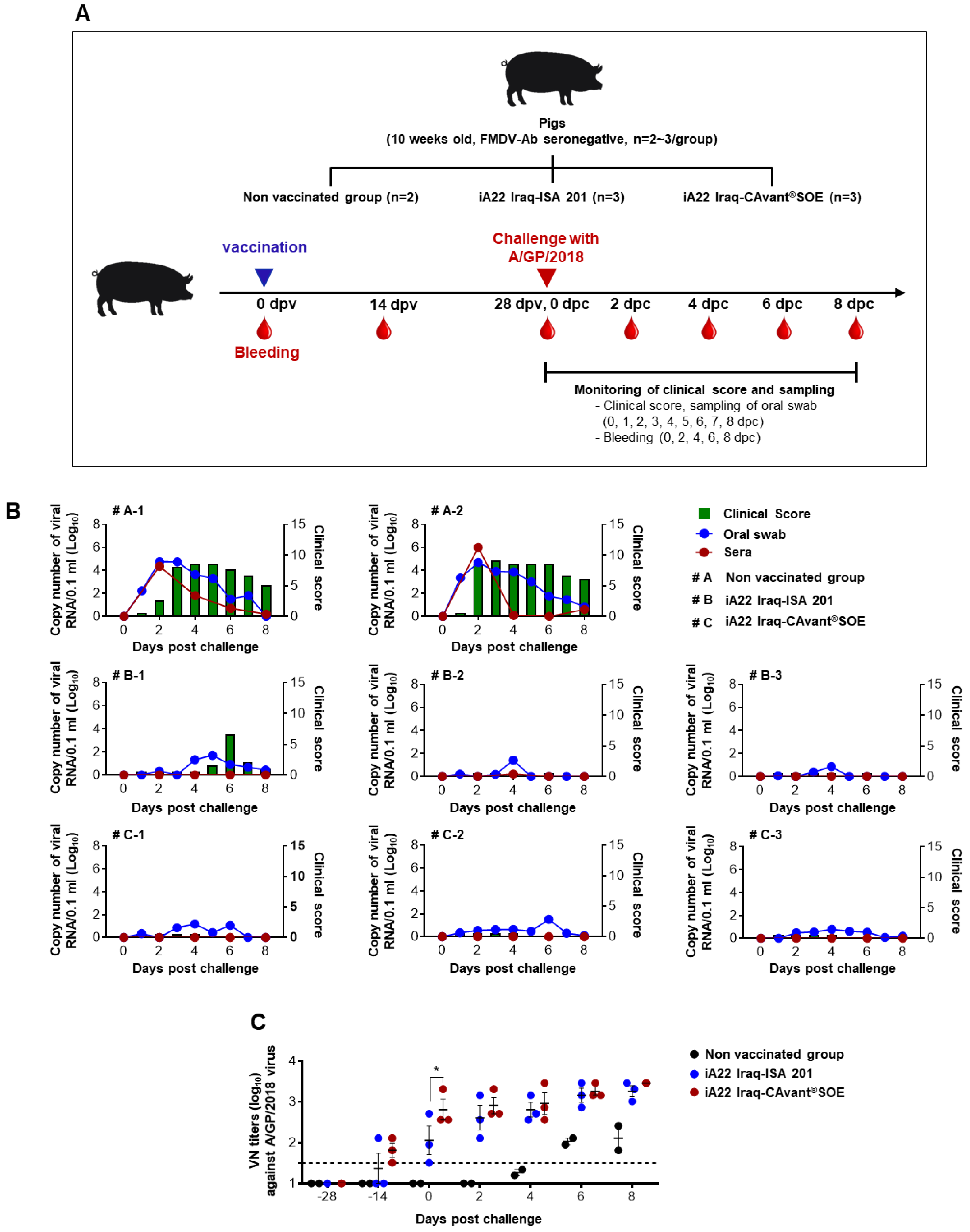
3.3. The CAvant®SOE Adjuvant Increases Protection from Challenge with FMDV in Pigs
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grubman, M.J.; Baxt, B. Foot-and-mouth disease. Clin. Microbiol. Rev. 2004, 17, 465–493. [Google Scholar] [CrossRef]
- Knowles, N.; Samuel, A. Molecular epidemiology of foot-and-mouth disease virus. Virus Res. 2003, 91, 65–80. [Google Scholar] [CrossRef]
- Feng, S.; Patton, M.; Davis, J. Market Impact of Foot-and-Mouth Disease Control Strategies: A UK Case Study. Front. Vet. Sci. 2017, 4, 129. [Google Scholar] [CrossRef] [PubMed]
- Yoon, H.; Jeong, W.; Han, J.-H.; Choi, J.; Kang, Y.-M.; Kim, Y.-S.; Park, H.-S.; Carpenter, T.E. Financial Impact of Foot-and-mouth disease outbreaks on pig farms in the Republic of Korea, 2014/2015. Prev. Vet. Med. 2018, 149, 140–142. [Google Scholar] [CrossRef]
- World Organisation for Animal Health. OIE-Listed Diseases, Infections and Infestations in Force in 2018; World Organisation for Animal Health: Paris, France, 2018. [Google Scholar]
- Saeed, A.; Kanwal, S.; Arshad, M.; Ali, M.; Shaikh, R.S.; Abubakar, M. Foot-and-mouth disease: Overview of motives of disease spread and efficacy of available vaccines. J. Anim. Sci. Technol. 2015, 57, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Lu, Z.; Liu, Z. Foot-and-mouth disease vaccines: Progress and problems. Expert Rev. Vaccines 2016, 15, 783–789. [Google Scholar] [CrossRef]
- Forth, L.F.; Höper, D.; Beer, M.; Eschbaumer, M. High-Resolution Composition Analysis of an Inactivated Polyvalent Foot-and-Mouth Disease Vaccine. Pathogens 2020, 9, 63. [Google Scholar] [CrossRef] [PubMed]
- Parida, S. Vaccination against foot-and-mouth disease virus: Strategies and effectiveness. Expert Rev. Vaccines 2009, 8, 347–365. [Google Scholar] [CrossRef]
- Kamel, M.; El-Sayed, A.; Vazquez, H.C. Foot-and-mouth disease vaccines: Recent updates and future perspectives. Arch. Virol. 2019, 164, 1501–1513. [Google Scholar] [CrossRef]
- Barnard, A.L.; Arriens, A.; Cox, S.; Barnett, P.; Kristensen, B.; Summerfield, A.; McCullough, K.C. Immune response characteristics following emergency vaccination of pigs against foot-and-mouth disease. Vaccine 2005, 23, 1037–1047. [Google Scholar] [CrossRef]
- Horsington, J.; Zhang, Z.; Bittner, H.; Hole, K.; Singanallur, N.; Alexandersen, S.; Vosloo, W. Early protection in sheep against intratypic heterologous challenge with serotype O foot-and-mouth disease virus using high-potency, emergency vaccine. Vaccine 2014, 33, 422–429. [Google Scholar] [CrossRef]
- Singh, R.K.; Sharma, G.K.; Mahajan, S.; Dhama, K.; Basagoudanavar, S.H.; Hosamani, M.; Sreenivasa, B.; Chaicumpa, W.; Gupta, V.K.; Sanyal, A. Foot-and-Mouth Disease Virus: Immunobiology, Advances in Vaccines and Vaccination Strategies Addressing Vaccine Failures—An Indian Perspective. Vaccines 2019, 7, 90. [Google Scholar] [CrossRef] [PubMed]
- Dar, P.; Kalaivanan, R.; Sied, N.; Mamo, B.; Kishore, S.; Suryanarayana, V.; Kondabattula, G. Montanide ISA™ 201 adjuvanted FMD vaccine induces improved immune responses and protection in cattle. Vaccine 2013, 31, 3327–3332. [Google Scholar] [CrossRef] [PubMed]
- Lyons, N.A.; Lyoo, Y.S.; King, D.; Paton, D.J. Challenges of Generating and Maintaining Protective Vaccine-Induced Immune Responses for Foot-and-Mouth Disease Virus in Pigs. Front. Vet. Sci. 2016, 3, 102. [Google Scholar] [CrossRef] [PubMed]
- Park, M.-E.; Lee, S.-Y.; Kim, R.-H.; Ko, M.-K.; Park, J.-N.; Lee, K.-N.; Kim, S.-M.; Choi, J.-H.; You, S.-H.; Kim, B.; et al. Altered adjuvant of foot-and-mouth disease vaccine improves immune response and protection from virus challenge. Trials Vaccinol. 2016, 5, 97–104. [Google Scholar] [CrossRef]
- Pattnaik, B.; Subramanaim, S.; Sanyal, A.; Mohapatra, J.K.; Dash, B.B.; Ranjan, R.; Rout, M. Foot-and-mouth Disease: Global Status and Future Road Map for Control and Prevention in India. Agric. Res. 2012, 1, 132–147. [Google Scholar] [CrossRef]
- Cao, Y. Adjuvants for foot-and-mouth disease virus vaccines: Recent progress. Expert Rev. Vaccines 2014, 13, 1377–1385. [Google Scholar] [CrossRef]
- Çokçalışkan, C.; Türkoğlu, T.; Sareyyüpoğlu, B.; Uzunlu, E.; Babak, A.; Özbilge, B.B.; Gülyaz, V. QS-21 enhances the early antibody response to oil adjuvant foot-and-mouth disease vaccine in cattle. Clin. Exp. Vaccine Res. 2016, 5, 138–147. [Google Scholar] [CrossRef]
- Doel, T. Optimisation of the immune response to foot-and-mouth disease vaccines. Vaccine 1999, 17, 1767–1771. [Google Scholar] [CrossRef]
- Cloete, M.; Dungu, B.; Van Staden, L.; Ismail-Cassim, N.; Vosloo, W. Evaluation of different adjuvants for foot-and-mouth disease vaccine containing all the SAT serotypes. Onderstepoort J. Vet. Res. 2008, 75, 17–31. [Google Scholar] [CrossRef]
- Iyer, A.; Ghosh, S.; Singh, S.; Deshmukh, R. Evaluation of three ‘ready to formulate’oil adjuvants for foot-and-mouth disease vaccine production. Vaccine 2000, 19, 1097–1105. [Google Scholar] [CrossRef]
- Khorasani, A.; Madadgar, O.; Soleimanjahi, H.; Keyvanfar, H.; Mahravani, H. Evaluation of the efficacy of a new oil-based adjuvant ISA 61 VG FMD vaccine as a potential vaccine for cattle. Iran J. Vete. Res. 2016, 17, 8–12. [Google Scholar]
- Stenfeldt, C.; Segundo, F.E.-S.; Santos, T.E.L.; Rodriguez, L.L.; Earzt, J. The Pathogenesis of Foot-and-Mouth Disease in Pigs. Front. Vet. Sci. 2016, 3, 41. [Google Scholar] [CrossRef]
- Barnett, P.; Pullen, L.; Williams, L.; Doel, T. International bank for foot-and-mouth disease vaccine: Assessment of Montanide ISA 25 and ISA 206, two commercially available oil adjuvants. Vaccine 1996, 14, 1187–1198. [Google Scholar] [CrossRef]
- Park, M.-E.; Lee, S.-Y.; Kim, R.-H.; Ko, M.-K.; Lee, K.-N.; Kim, S.-M.; Kim, B.-K.; Lee, J.-S.; Kim, B.; Park, J.-H. Enhanced immune responses of foot-and-mouth disease vaccine using new oil/gel adjuvant mixtures in pigs and goats. Vaccine 2014, 32, 5221–5227. [Google Scholar] [CrossRef]
- Sadir, A.M.; Schudel, A.A.; Laporte, O.; Braun, M.; Margni, R.A. Response to foot-and-mouth disease vaccines in newborn calves. Influence of age, colostral antibodies and adjuvants. Epidemiol. Infect. 1988, 100, 135–144. [Google Scholar] [CrossRef] [PubMed]
- Späth, E.; Smitsaart, E.; Casaro, A.; Fondevila, N.; Fernández, F.; Leunda, M.; Compaired, D.; Buffarini, M.; Pessi, H. Immune response of calves to foot-and-mouth disease virus vaccine emulsified with oil adjuvant. Strategies of vaccination. Vaccine 1995, 13, 909–914. [Google Scholar] [CrossRef]
- Li, D.; Zhou, C.; She, D.; Li, P.; Sun, P.; Bai, X.; Chen, Y.; Xie, B.; Liu, Z. The comparison of the efficacy of swine FMD vaccine emulsified with oil adjuvant of ISA 201 VG or ISA 206 VG. J. Biosci. Med. 2013, 1, 22–25. [Google Scholar] [CrossRef][Green Version]
- Ibrahim, E.E.-S.; Gamal, W.M.; Hassan, A.I.; Mahdy, S.E.-D.; Hegazy, A.Z.; Abdel-Atty, M.M. Comparative study on the immunopotentiator effect of ISA 201, ISA 61, ISA 50, ISA 206 used in trivalent foot and mouth disease vaccine. Vet. World 2015, 8, 1189–1198. [Google Scholar] [CrossRef]
- Mowat, N. Vaccine Manual: The Production and Quality Control of Veterinary Vaccines for Use in Developing Countries; Daya Books: New Delhi, India, 1999. [Google Scholar]
- McKercher, P.D.; Graves, J.H. A review of the current status of oil adjuvants in foot-and-mouth disease vaccines. Dev. Boil. Stand. 1976, 35, 107–112. [Google Scholar]
- Park, J.-N.; Lee, S.-Y.; Chu, J.-Q.; Lee, Y.-J.; Kim, R.-H.; Lee, K.-N.; Kim, S.-M.; Tark, D.-S.; Kim, B.; Park, J.-H. Protection to homologous and heterologous challenge in pigs immunized with vaccine against foot-and-mouth disease type O caused an epidemic in East Asia during 2010/2011. Vaccine 2014, 32, 1882–1889. [Google Scholar] [CrossRef] [PubMed]
- Alves, M.P.; Guzylack-Piriou, L.; Juillard, V.; Audonnet, J.-C.; Doel, T.; Dawson, H.; Golde, W.T.; Gerber, H.; Peduto, N.; McCullough, K.C.; et al. Innate Immune Defenses Induced by CpG Do Not Promote Vaccine-Induced Protection against Foot-and-Mouth Disease Virus in Pigs. Clin. Vaccine Immunol. 2009, 16, 1151–1157. [Google Scholar] [CrossRef] [PubMed]
- Oem, J.; Yeh, M.; McKenna, T.; Hayes, J.; Rieder, E.; Giuffre, A.; Robida, J.; Lee, K.; Cho, I.; Fang, X.; et al. Pathogenic Characteristics of the Korean 2002 Isolate of Foot-and-Mouth Disease Virus Serotype O in Pigs and Cattle. J. Comp. Pathol. 2008, 138, 204–214. [Google Scholar] [CrossRef] [PubMed]
- Golde, W.T.; Pacheco, J.M.; Duque, H.; Doel, T.; Penfold, B.; Ferman, G.S.; Gregg, D.R.; Rodriguez, L.L. Vaccination against foot-and-mouth disease virus confers complete clinical protection in 7 days and partial protection in 4 days: Use in emergency outbreak response. Vaccine 2005, 23, 5775–5782. [Google Scholar] [CrossRef]
- Kenneth, C.; McCullough, S.F. Immunology of foot and mouth disease. In Foot and Mouth Disease; Current Perspectives; CRC Press: Boca Raton, FL, USA, 2004. [Google Scholar]
- London, C.A.; Abbas, A.K.; Kelso, A. Helper T cell subsets: Heterogeneity, functions and development. Vet. Immunol. Immunopathol. 1998, 63, 37–44. [Google Scholar] [CrossRef]
- Oh, Y.; Fleming, L.; Statham, B.; Hamblin, P.; Barnett, P.; Paton, D.J.; Park, J.-H.; Joo, Y.S.; Parida, S. Interferon-γ Induced by In Vitro Re-Stimulation of CD4+ T-Cells Correlates with In Vivo FMD Vaccine Induced Protection of Cattle against Disease and Persistent Infection. PLoS ONE 2012, 7, e44365. [Google Scholar] [CrossRef]
- Chen, Z.; Zhang, S.; Li, Z.; Ma, G.; Su, Z. Construction of a stable w/o nano-emulsion as a potential adjuvant for foot and mouth disease virus vaccine. Artif. Cells Nanomed. Biotechnol. 2016, 45, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.-B.; Xu, J. Better Adjuvants for Better Vaccines: Progress in Adjuvant Delivery Systems, Modifications, and Adjuvant–Antigen Codelivery. Vaccines 2020, 8, 128. [Google Scholar] [CrossRef]
- McCullough, K.C.; Crowther, J.R.; Butcher, R.N.; Carpenter, W.C.; Brocchi, E.; Capucci, L.; De Simone, F. Immune protection against foot-and-mouth disease virus studied using virus-neutralizing and non-neutralizing concentrations of monoclonal antibodies. Immunology 1986, 58, 421–428. [Google Scholar] [PubMed]
- McCullough, K.C.; De Simone, F.; Brocchi, E.; Capucci, L.; Crowther, J.R.; Kihm, U. Protective immune response against foot-and-mouth disease. J. Virol. 1992, 66, 1835–1840. [Google Scholar] [CrossRef]
- Cribbs, D.H.; Ghochikyan, A.; Vasilevko, V.; Tran, M.; Petrushina, I.; Sadzikava, N.; Babikyan, D.; Kesslak, P.; Kieber-Emmons, T.; Cotman, C.W. Adjuvant-dependent modulation of Th1 and Th2 responses to immunization with β-amyloid. Int. Immunol. 2003, 15, 505–514. [Google Scholar] [CrossRef] [PubMed]
- Da Cunha, C.E.P.; Moreira, C.; Rocha, A.D.S.R.; Finger, P.F.; Magalhães, C.G.; Ferreira, M.R.A.; Dellagostin, O.A.; Moreira, N.; Conceição, F.R. Parenteral adjuvant potential of recombinant B subunit of Escherichia coli heat-labile enterotoxin. Mem. Inst. Oswaldo Cruz 2017, 112, 812–816. [Google Scholar] [CrossRef] [PubMed]


| Protein | aa Position | aa Sequence |
|---|---|---|
| A22 Iraq VP1 | 139–158 | GGTGRRGDLGPLAARVAAQL |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahn, Y.-H.; Chathuranga, W.A.G.; Shim, Y.-J.; Haluwana, D.K.; Kim, E.-H.; Yoon, I.-J.; Lim, Y.-T.; Shin, S.H.; Jo, H.; Hwang, S.Y.; et al. The Potential Adjuvanticity of CAvant®SOE for Foot-and-Mouth Disease Vaccine. Vaccines 2021, 9, 1091. https://doi.org/10.3390/vaccines9101091
Ahn Y-H, Chathuranga WAG, Shim Y-J, Haluwana DK, Kim E-H, Yoon I-J, Lim Y-T, Shin SH, Jo H, Hwang SY, et al. The Potential Adjuvanticity of CAvant®SOE for Foot-and-Mouth Disease Vaccine. Vaccines. 2021; 9(10):1091. https://doi.org/10.3390/vaccines9101091
Chicago/Turabian StyleAhn, Young-Hoon, W. A. Gayan Chathuranga, Young-Jung Shim, D. K. Haluwana, Eun-Hee Kim, In-Joong Yoon, Yong-Taik Lim, Sung Ho Shin, Hyundong Jo, Seong Yun Hwang, and et al. 2021. "The Potential Adjuvanticity of CAvant®SOE for Foot-and-Mouth Disease Vaccine" Vaccines 9, no. 10: 1091. https://doi.org/10.3390/vaccines9101091
APA StyleAhn, Y.-H., Chathuranga, W. A. G., Shim, Y.-J., Haluwana, D. K., Kim, E.-H., Yoon, I.-J., Lim, Y.-T., Shin, S. H., Jo, H., Hwang, S. Y., Kim, H. M., Lee, M. J., Park, J.-H., Yoo, S.-S., & Lee, J.-S. (2021). The Potential Adjuvanticity of CAvant®SOE for Foot-and-Mouth Disease Vaccine. Vaccines, 9(10), 1091. https://doi.org/10.3390/vaccines9101091






