Attitudes and Perception of Healthcare Workers Concerning Influenza Vaccination during the 2019/2020 Season: A Survey of Sicilian University Hospitals
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Statistical Analysis
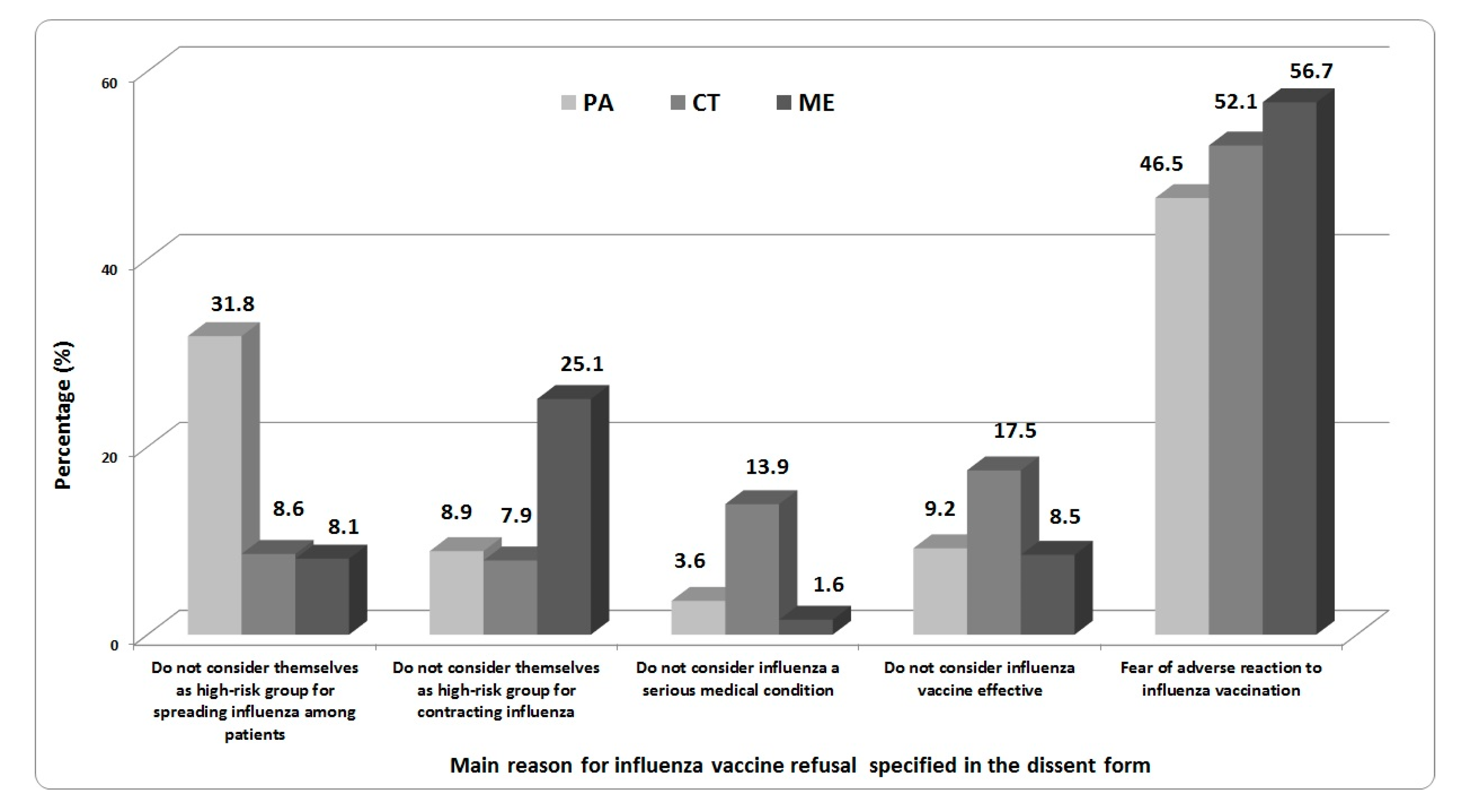
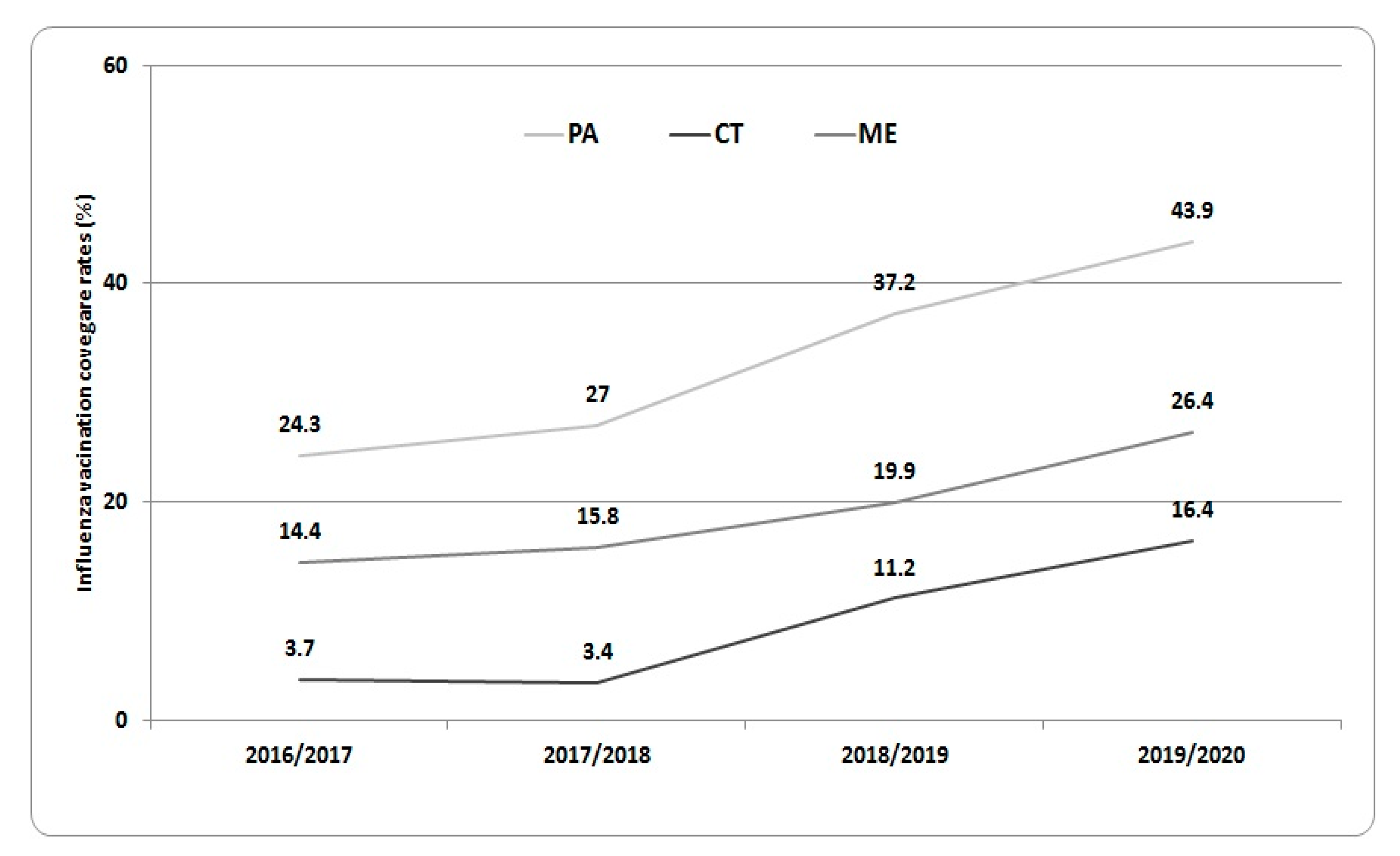
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Nair, H.; Brooks, W.A.; Katz, M.; Roca, A.; Berkley, J.A.; Madhi, S.A.; Simmerman, J.M.; Gordon, A.; Sato, M.; Howie, S.; et al. Global burden of respiratory infections due to seasonal influenza in young children: A systematic review and meta-analysis. Lancet 2011, 378, 1917–1930. [Google Scholar] [CrossRef]
- Costantino, C.; Vitale, F. Influenza vaccination in high-risk groups: A revision of existing guidelines and rationale for an evidence-based preventive strategy. J. Prev. Med. Hyg. 2016, 57, E13–E18. [Google Scholar] [PubMed]
- Center for Disease Control and Prevention. Disease burden of Influenza. Available online: https://www.cdc.gov/flu/about/burden/index.html (accessed on 13 October 2020).
- Italian ministry of Health. Influenza Vaccination Coverage Rates from 2018/2019 Season. Available online: http://www.salute.gov.it/imgs/C_17_tavole_19_1_19_file.pdf (accessed on 13 October 2020).
- Genovese, C.; La Fauci, V.; Costa, G.B.; Buda, A.; Nucera, S.; Antonuccio, G.M.; Alessi, V.; Carnuccio, S.; Carnuccio, P.; Laudani, N.; et al. A potential outbreak of Measles and chickenpox among healthcare workers of a university Hospital. EuroMediterr. Biomed. J. 2019, 14, 45–48. [Google Scholar]
- Montagna, M.T.; Mascipinto, S.; Pousis, C.; Bianchi, F.P.; Caggiano, G.; Carpagnano, L.F.; Giglio, O.D.; Barbuti, G.; Auxilia, F.; Destrebecq, A.; et al. Knowledge, experiences, and attitudes toward Mantoux test among medical and health professional students in Italy: A cross-sectional study. Ann. Ig. 2018, 30, 86–98. [Google Scholar] [PubMed]
- Restivo, V.; Costantino, C.; Mammina, C.; Vitale, F. Influenza like Illness among Medical Residents Anticipates Influenza Diffusion in General Population: Data from a National Survey among Italian Medical Residents. PLoS ONE 2016, 11, e0168546. [Google Scholar] [CrossRef][Green Version]
- Rapisarda, V.; Ledda, C.; Maltezou, H.C. Vaccination in healthcare workers: Risk assessment, planning, strategy of intervention and legal implications. Future Microbiol. 2019, 14, 1–3. [Google Scholar] [CrossRef]
- Costantino, C.; Casuccio, A.; Caracci, F.; Bono, S.; Calamusa, G.; Calamusa, G.; Maida, C.M.; Vitale, F.; Restivo, V. Impact of Communicative and Informative Strategies on Influenza Vaccination Adherence and Absenteeism from Work of Health Care Professionals Working at the University Hospital of Palermo, Italy: A Quasi-Experimental Field Trial on Twelve Influenza Seasons. Vaccines 2019, 8, 5. [Google Scholar] [CrossRef]
- Maltezou, H.C.; Botelho-Nevers, E.; Brantsæter, A.B.; Carlsson, R.M.; Heininger, U.; Hübschen, J.M.; Josefsdottirg, K.S.; Kassianos, G.; Kyncl, J.; Ledda, C.; et al. Vaccination of healthcare personnel in europe: Update to current policies. Vaccine 2019, 37, 7576–7584. [Google Scholar] [CrossRef]
- Italian Ministry of Health. National Vaccination Prevention Plan 2017–2019. Available online: www.salute.gov.it/portale/documentazione/p6_2_2_1.jsp?lingua=italiano&id=2571 (accessed on 13 October 2020).
- Genovese, C.; Picerno, I.A.M.; Trimarchi, G.; Cannavo, G.; Egitto, G.; Cosenza, B.; Merlina, V.; Icardi, G.; Panatto, D.; Amicizia, A.; et al. Vaccination coverage in healthcare workers: A multicenter cross-sectional study in Italy. J. Prev. Med. Hyg. 2019, 60, E12–E17. [Google Scholar]
- Costantino, C.; Ledda, C.; Genovese, C.; Contrino, E.; Vitale, E.; Maida, C.M.; Squeri, R.; Squeri, F.; Rapisarda, V. Immunization Status against Measles of Health-Care Workers Operating at Three Sicilian University Hospitals: An Observational Study. Vaccines 2019, 7, 175. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Seasonal Influenza Vaccination and Antiviral Use in EU/EEA Member States—Overview of Vaccine Recommendations for 2017–2018 and Vaccination Coverage Rates for 2015–2016 and 2016–2017 Influenza Seasons. Available online: https://www.ecdc.europa.eu/en/publications-data/seasonal-influenza-vaccination-antiviral-use-eu-eea-member-states (accessed on 13 October 2020).
- Public Health England. Seasonal Influenza Vaccine Uptake in Healthcare Workers (HCWs) in England: Winter Season 2018 to 2019. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/804885/Seasonal_influenza_vaccine_uptake-HCWs-2018_Final.pdf (accessed on 13 October 2020).
- Panatto, D.; Lai, P.L.; Mosca, S.; Lecini, E.; Orsi, A.; Signori, A.; Castaldi, S.; Pariani, E.; Pellegrinelli, L.; Galli, C.; et al. Influenza Vaccination in Italian Healthcare Workers (2018–2019 Season): Strengths and Weaknesses. Results of a Cohort Study in Two Large Italian Hospitals. Vaccines 2020, 8, 119. [Google Scholar] [CrossRef] [PubMed]
- Napolitano, F.; Bianco, A.; D’Alessandro, A.; Papadopoli, R.; Angelillo, I.F. Healthcare workers’ knowledge, beliefs, and coverage regarding vaccinations in critical care units in Italy. Vaccine 2019, 37, 6900–6906. [Google Scholar] [CrossRef] [PubMed]
- Costantino, C.; Amodio, E.; Calamusa, G.; Vitale, F.; Mazzucco, W. Could university training and a proactive attitude of coworkers be associated with influenza vaccination compliance? A multicentre survey among Italian medical residents. BMC Med. Educ. 2016, 29, 16–38. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Squeri, R.; La Fauci, V.; Picerno, I.A.M.; Trimarchi, G.; Cannavò, G.; Egitto, G.; Cosenza, B.; Merlina, V.; Genovese, C. Evaluation of Vaccination Coverages in the Health Care Workers of a University Hospital in Southern Italy. Ann. Ig. 2019, 31, 13–24. [Google Scholar]
- Sicilian Health Department. Decree n.1829 of the 20 September 2019: Recommendations for Influenza Vaccination Campaign 2019/2020. Available online: https://www.vaccinarsinsicilia.org/assets/uploads/files/d.a.-n.-1829-del-20-settembre-2019-campagna-antinfluenzale.pdf (accessed on 13 October 2020).
- Sicilian Health Department. Decree n.1649 of the 19 September 2018: Recommendations for Influenza Vaccination Campaign 2018/2019. Available online: http://pti.regione.sicilia.it/portal/page/portal/PIR_PORTALE/PIR_LaStrutturaRegionale/PIR_AssessoratoSalute/PIR_Infoedocumenti/PIR_DecretiAssessratoSalute/PIR_DecretiAssessoriali/PIR_DecretiAssessorialianno2018/D.A.%20n.%201646%20del%2019%20settembre%202018%20%20pdf%20a.pdf (accessed on 13 October 2020).
- Fortunato, F.; Tafuri, S.; Cozza, V.; Martinelli, D.; Prato, R. Low vaccination coverage among italian healthcare workers in 2013: Contributing to the voluntary vs. mandatory vaccination debate. Hum. Vaccines Immunother. 2015, 11, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Costantino, C.; Battaglia, A.; D’Asta, M.; Furnari, R.; Gimigliano, A.; Guaccero, A.; Mallamace, N.; Marcantoni, C.; Maringhini, G.; Marsala, M.G.L.; et al. Knowledge, attitudes and behaviors regarding influenza vaccination among hygiene and preventive medicine residents in Calabria and Sicily. EuroMediterr. Biomed. J. 2012, 7, 77–83. [Google Scholar]
- Mereckiene, J.; Cotter, S.; Nicoll, A.; Lopalco, P.; Noori, T.; Weber, J.T.; D’Ancona, F.; Levy-Bruhl, D.; Dematte, L.; Giambi, C.; et al. Seasonal influenza immunisation in europe. Overview of recommendations and vaccination coverage for threeseasons: Pre-pandemic (2008/09), pandemic (2009/10) and post-pandemic (2010/11). Eurosurveillance 2014, 19, 20780. [Google Scholar] [CrossRef]
- Sydnor, E.; Perl, T.M. Healthcare providers as sources of vaccine-preventable diseases. Vaccine 2014, 32, 4814–4822. [Google Scholar] [CrossRef]
- Maltezou, H.C.; Poland, G.A. Vaccination policies for healthcare workers in europe. Vaccine 2014, 32, 4876–4880. [Google Scholar] [CrossRef]
- Restivo, V.; Orsi, A.; Ciampini, S.; Messano, G.A.; Trucchi, C.; Ventura, G.; Casuccio, A.; Vitale, F. How should vaccination services be planned, organized, and managed? Results from a survey on the Italian vaccination services. Ann. Ig. 2019, 31, 45–53. [Google Scholar]
- Pereira, M.; Williams, S.; Restrick, L.; Cullinan, P.; Hopkinson, N.S.; London Respiratory Network. Healthcare worker influenza vaccination and sickness absence—An ecological study. Clin. Med. (Lond.) 2017, 17, 484–489. [Google Scholar] [CrossRef] [PubMed]
- Amodio, E.; Restivo, V.; Firenze, A.; Mammina, C.; Tramuto, F.; Vitale, F. Can influenza vaccination coverage among healthcare workers influence the risk of nosocomial influenza-like illness in hospitalized patients? J. Hosp. Infect. 2014, 86, 182–187. [Google Scholar] [CrossRef]
- Costantino, C.; Amodio, E.; Vitale, F.; Di Pasquale, M.; Gelsomino, V.; Morici, M.; Palmeri, A.; Termini, S.; Firenze, A.; Massenti, M.F.; et al. Attitudes, behaviours and perceptions of Italian General Practitioner trainees towards influenza vaccination in Western Sicily (Italy). Ital. J. Public Health 2012, 9, 33–39. [Google Scholar]
- Bellia, C.; Setbon, M.; Zylberman, P.; Flahault, A. Healthcare worker compliance with seasonal and pandemic influenza vaccination. Influ. Other. Respir. Viruses 2013, 7, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Riphagen-Dalhuisen, J.; Gefenaite, G.; Hak, E. Predictors of seasonal influenza vaccination among healthcare workers in hospitals: A descriptive meta-analysis. Occup. Environ. Med. 2012, 69, 230–235. [Google Scholar] [CrossRef]
- Bonaccorsi, G.; Lorini, C.; Santomauro, F.; Guarducci, S.; Pellegrino, E.; Puggelli, F.; Balli, M.; Bonanni, P. Predictive factors associated with the acceptance of pandemic and seasonal influenza vaccination in health care workers and students in tuscany, central italy. Hum. Vaccines Immunother. 2013, 9, 2603–2612. [Google Scholar] [CrossRef]
- Lehmann, B.A.; Ruiter, R.A.C.; Chapman, G.; Kok, G. The intention to get vaccinated against influenza and actual vaccination uptake of dutch healthcare personnel. Vaccine 2014, 32, 6986–6991. [Google Scholar] [CrossRef]
- Barbadoro, P.; Marigliano, A.; Di Tondo, E.; Chiatti, C.; Di Stanislao, F.; D’Errico, M.M.; Prospero, E. Determinants of influenza vaccination uptake among italian healthcare workers. Hum. Vaccines Immunother. 2013, 9, 911–916. [Google Scholar] [CrossRef]
- Hollmeyer, H.G.; Hayden, F.; Poland, G.; Buchholz, U. Influenza vaccination of health care workers in hospitals: A review of studies on attitudes and predictors. Vaccine 2009, 27, 3935–3944. [Google Scholar] [CrossRef]
- Yue, X.; Black, C.; Ball, S.; Donahue, S.; De Perio, M.A.; Laney, A.S.; Greby, S. Workplace interventions associated with influenza vaccination coverage among health care personnel in ambulatory care settings during the 2013–2014 and 2014–2015 influenza seasons. Am. J. Infect. Control. 2017, 45, 1243–1248. [Google Scholar] [CrossRef]
- Costantino, C.; Restivo, V.; Gaglio, V.; Lanza, G.L.M.; Marotta, C.; Maida, C.M.; Mazzucco, W.; Casuccio, A.; Torregrossa, M.V.; Vitale, F. Effectiveness of an educational intervention on seasonal influenza vaccination campaign adherence among healthcare workers of the Palermo University Hospital, Italy. Ann. Ig. 2019, 31, 35–44. [Google Scholar] [PubMed]
- Marotta, C.; Raia, D.D.; Ventura, G.; Casuccio, N.; Dieli, F.; D’Angelo, C.; Restivo, V.; Costantino, C.; Vitale, F.; Casuccio, A. Improvement in vaccination knowledge among health students following an integrated extra curricular intervention, an explorative study in the University of Palermo. J. Prev. Med. Hyg. 2017, 58, E93–E98. [Google Scholar] [PubMed]
- MacDougall, D.M.; McCarthy, A.E. Seasonal influenza vaccination campaigns for health care personnel: Systematic review. CMAJ 2010, 182, E542–E548. [Google Scholar]
- Schmidt, S.; Saulle, R.; Di Thiene, D.; Boccia, A.; La Torre, G. Do the quality of the trials and the year of publication affect the efficacy of intervention to improve seasonal influenza vaccination among healthcare workers? Results of a systematic review. Hum. Vaccines Immunother. 2013, 9, 349–361. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Vaccine Hesitancy among Healthcare Workers and Their Patients in Europe: A Qualitative Study. Available online: https://www.ecdc.europa.eu/en/publications-data/vaccine-hesitancy-among-healthcare-workers-and-their-patients-europe (accessed on 13 October 2020).
- Costantino, C.; Caracci, F.; Brandi, M.; Bono, S.E.; Ferro, A.; Sannasardo, C.E.; Scarpitta, F.; Siddu, A.; Vella, C.; Ventura, G.; et al. Determinants of vaccine hesitancy and effectiveness of vaccination counseling interventions among a sample of the general population in Palermo, Italy. Hum. Vaccin. Immunother. 2020, 18, 1–7. [Google Scholar] [CrossRef]
- Maltezou, H.C.; Theodoridou, K.; Ledda, C.; Rapisarda, V.; Theodoridou, M. Vaccination of healthcare workers: Is mandatory vaccination needed? Expert. Rev. Vaccines 2019, 18, 5–13. [Google Scholar] [CrossRef]
- Costantino, C.; Restivo, V.; Tramuto, F.; Casuccio, A.; Vitale, F. Influenza vaccination of healthcare workers in Italy: Could mandatory vaccination be a solution to protect patients? Future Microbiol. 2019, 14, 45–49. [Google Scholar] [CrossRef]
- Amato, M.; Werba, J.P.; Frigerio, B.; Coggi, D.; Sansaro, D.; Ravani, A.; Ferrante, P.; Veglia, F.; Tremoli, E.; Baldassarre, D. Relationship between Influenza Vaccination Coverage Rate and COVID-19 Outbreak: An Italian Ecological Study. Vaccines 2020, 8, 535. [Google Scholar] [CrossRef]
- Costantino, C.; Cannizzaro, E.; Alba, D.; Conforto, A.; Cimino, L.; Mazzucco, W. Sars-Cov-2 Pandemic In The Mediterranean Area: Epidemiology And Perspectives. EuroMediterr. Biomed. J. 2020, 15, 102–106. [Google Scholar]
| Variables | Palermo UH (n = 1169) * | Messina UH (n = 440) * | Catania UH (n = 747) * | p-Value |
|---|---|---|---|---|
| Mean age ± Standard deviation | 33.5 ± 13.1 | 29.1 ± 10.8 | 39.3 ± 12.6 | <0.001 |
| Median age (Interquartile range) | 28 (25–40) | 25 (22–32) | 33 (29–50) | <0.001 |
| Gender, n (%) | ||||
| - male | 477 (40.9) | 176 (40.0) | 344 (46.1) | >0.05 |
| - female | 690 (59.1) | 264 (60.0) | 403 (53.9) | |
| HCW type, n (%) | ||||
| - medical doctor | 429 (38.1) | 134 (30.5) | 514 (68.8) | <0.001 |
| - nurse/healthcare assistant | 195 (17.3) | 45 (10.2) | 233 (31.2) | |
| - student/trainee | 501 (44.5) | 261 (59.3) | 0 (0.0) | |
| Hospital unit, n (%) | ||||
| - at risk | 448 (71.1) | 75 (74.3) | 528 (70.7) | <0.76 |
| - not at risk | 182 (28.9) | 26 (25.7) | 219 (29.3) |
| Variables | Palermo UH (n = 1168) * | Messina UH (n = 440) * | Catania UH (n = 747) * | p-Value |
|---|---|---|---|---|
| Daily washing of hands, n (%) | ||||
| - ≤3 times a day | 25 (2.1) | 13 (2.9) | 28 (3.7) | <0.001 |
| - 4–6 times a day | 462 (39.5) | 196 (44.7) | 142 (19.0) | |
| - ≥7 times a day | 681 (58.4) | 230 (52.4) | 577 (77.3) | |
| Vaccination adherence during last five seasons, n (%) | ||||
| - Never vaccinated | 500 (43.1) | 136 (30.9) | 569 (76.3) | <0.001 |
| - Vaccinated 1 or 2 times | 337 (29.1) | 213 (48.4) | 81 (10.8) | |
| - Regularly vaccinated (3–5 times) | 323 (27.8) | 91 (20.7) | 97 (12.9) | |
| Self-perceived risk of contracting influenza in comparison with general population, n (%) | ||||
| - Equal | 333 (28.8) | 108 (24.5) | 502 (67.3) | <0.001 |
| - Higher | 768 (66.4) | 306 (69.6) | 239 (31.9) | |
| - Lower | 56 (4.8) | 26 (5.9) | 6 (0.8) | |
| Considering themselves as a high-risk group to infect patients with influenza virus, n (%) | ||||
| - Yes | 352 (30.5) | 123 (27.9) | 94 (12.6) | <0.001 |
| - Yes, partially | 556 (48.1) | 200 (45.5) | 150 (20.1) | |
| - No | 247 (21.4) | 117 (26.6) | 503 (67.3) | |
| Main reason for influenza vaccination adherence, n (%) | ||||
| - To protect themselves | 375 (32.2) | 142 (32.3) | 151 (49.8) | <0.001 |
| - To protect patients | 775 (66.5) | 290 (65.9) | 152 (50.2) | |
| - To avoid compulsory mask wearing | 15 (1.3) | 8 (1.8) | 0 (0.0) | |
| Attitude to recommending influenza vaccination to patients, n (%) | ||||
| - Yes | 988 (85.3) | 384 (87.3) | 278 (37.2) | <0.001 |
| - No | 171 (14.7) | 56 (12.7) | 469 (62.8) | |
| Variables | Crude OR | CI 95% | p-Value | Adj OR | CI 95% | p-Value |
|---|---|---|---|---|---|---|
| Gender | ||||||
| - Male | ref | 0.09 | ref | 0.12 | ||
| - Female | 0.70 | (0.52–1.05) | 0.86 | (0.75–1.22) | ||
| Age in years | 1.45 | (0.92–2.60) | 0.08 | 1.59 | (0.86–2.03) | 0.15 |
| HCWs type | ||||||
| - nurse/healthcare assistant | ref | 0.06 | ref | 0.18 | ||
| - medical doctor | 0.84 | (0.6–1.01) | 0.77 | (0.52–1.12) | ||
| Self-perceived risk of contracting influenza in comparison with general population | ||||||
| - Equal or Lower | ref | <0.001 | ref | <0.01 | ||
| - Higher | 3.4 | (2.6–4.3) | 2.65 | (1.89–3.65) | ||
| Hospital Unit | ||||||
| - Not at risk | ref | 0.15 | ref | 0.54 | ||
| - At risk | 0.8 | (0.6–1.0) | 0.91 | (0.64–1.26) | ||
| Daily washing of hands | ||||||
| - ≤6 times a day | ref | 0.95 | ||||
| - ≥7 times a day | 0.1 | (0.8–1.3) | ||||
| Main reason for influenza vaccination adherence | ||||||
| - To protect themselves/ To avoid mask wearing | ref | 0.06 | ref | 0.54 | ||
| - To protect patients | 0.8 | (0.6–1.01) | 1.09 | (0.81–1.48) | ||
| Attitude to recommending influenza vaccination to patients | ||||||
| - No | ref | <0.001 | ref | <0.001 | ||
| - Yes | 6.35 | (4.69–15.2) | 3.45 | (1.78–5.63) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Costantino, C.; Ledda, C.; Squeri, R.; Restivo, V.; Casuccio, A.; Rapisarda, V.; Graziano, G.; Alba, D.; Cimino, L.; Conforto, A.; et al. Attitudes and Perception of Healthcare Workers Concerning Influenza Vaccination during the 2019/2020 Season: A Survey of Sicilian University Hospitals. Vaccines 2020, 8, 686. https://doi.org/10.3390/vaccines8040686
Costantino C, Ledda C, Squeri R, Restivo V, Casuccio A, Rapisarda V, Graziano G, Alba D, Cimino L, Conforto A, et al. Attitudes and Perception of Healthcare Workers Concerning Influenza Vaccination during the 2019/2020 Season: A Survey of Sicilian University Hospitals. Vaccines. 2020; 8(4):686. https://doi.org/10.3390/vaccines8040686
Chicago/Turabian StyleCostantino, Claudio, Caterina Ledda, Raffaele Squeri, Vincenzo Restivo, Alessandra Casuccio, Venerando Rapisarda, Giorgio Graziano, Davide Alba, Livia Cimino, Arianna Conforto, and et al. 2020. "Attitudes and Perception of Healthcare Workers Concerning Influenza Vaccination during the 2019/2020 Season: A Survey of Sicilian University Hospitals" Vaccines 8, no. 4: 686. https://doi.org/10.3390/vaccines8040686
APA StyleCostantino, C., Ledda, C., Squeri, R., Restivo, V., Casuccio, A., Rapisarda, V., Graziano, G., Alba, D., Cimino, L., Conforto, A., Costa, G. B., D’Amato, S., Mazzitelli, F., Vitale, F., & Genovese, C. (2020). Attitudes and Perception of Healthcare Workers Concerning Influenza Vaccination during the 2019/2020 Season: A Survey of Sicilian University Hospitals. Vaccines, 8(4), 686. https://doi.org/10.3390/vaccines8040686











