Usp18 Expression in CD169+ Macrophages is Important for Strong Immune Response after Vaccination with VSV-EBOV
Abstract
:1. Introduction
2. Material and Methods
2.1. Mice
2.2. Virus
2.3. Neutralization Antibody Assay
2.4. Immunohistofluorescense
2.5. RNA Extraction, cDNA Synthesis and qRT-PCR
2.6. Statistical Analysis
3. Results
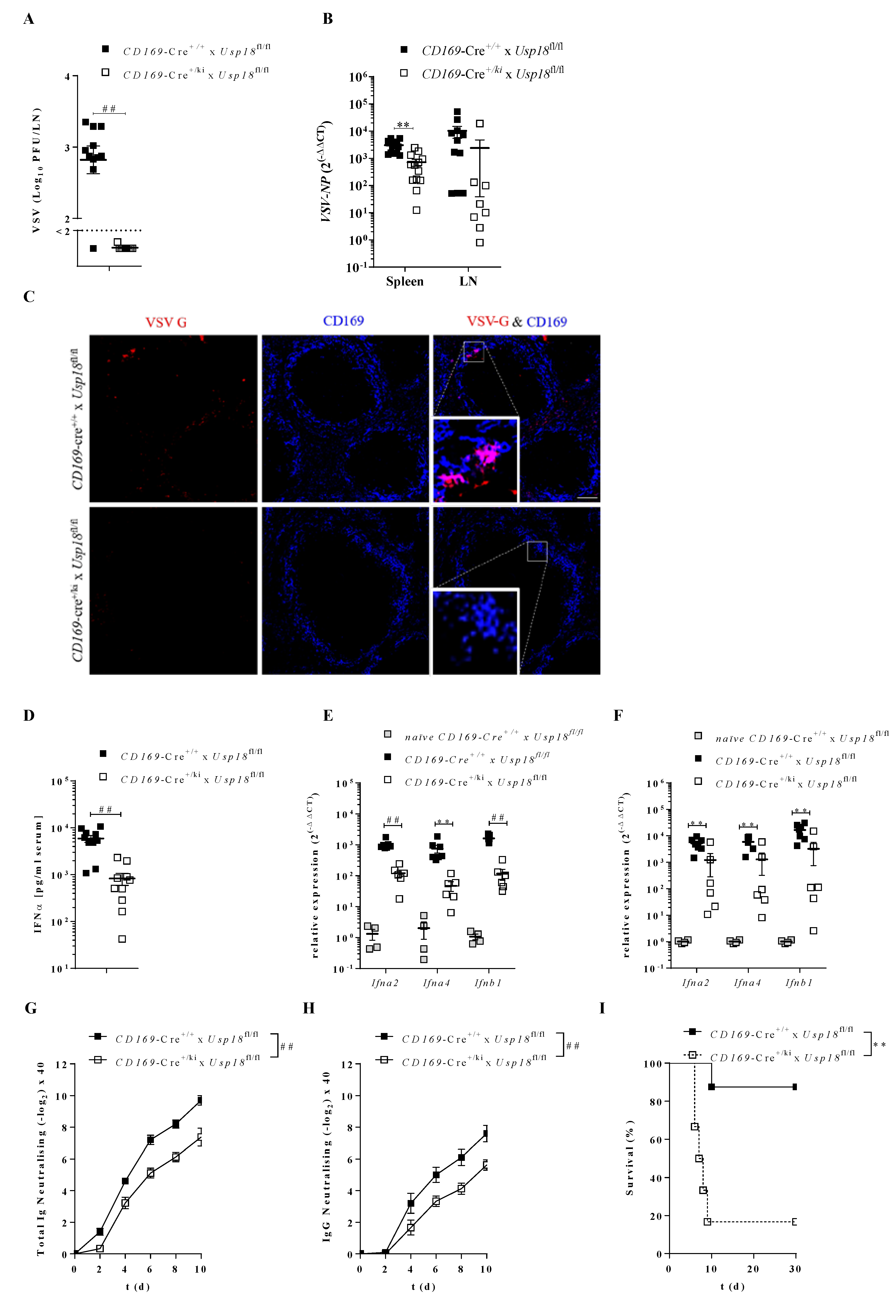
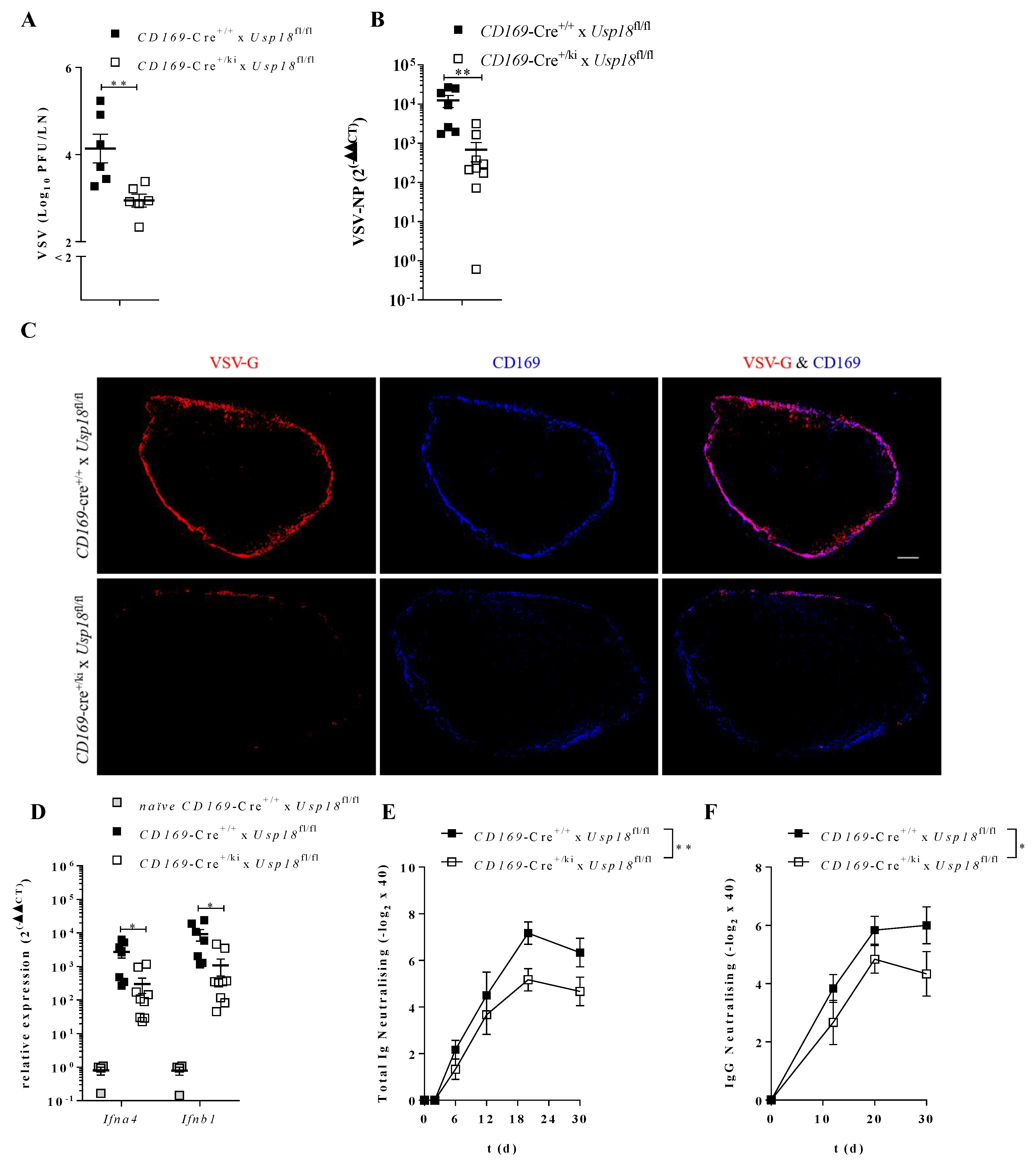
3.1. Usp18 Enforces Viral Replication in CD169+ Macrophages and Promotes Immune Activation
3.2. Enforced Replication Activates Immunity in dLN
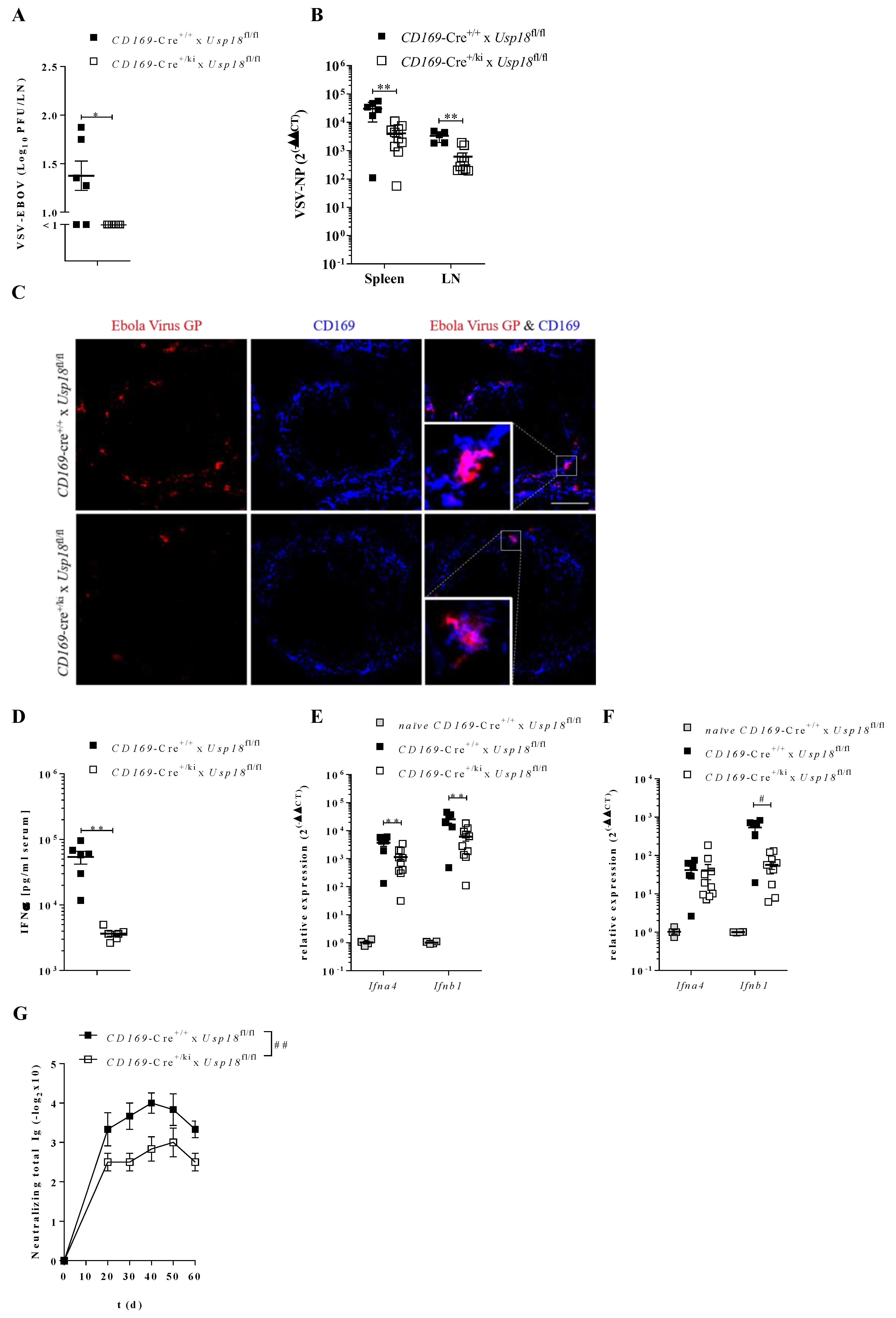
3.3. Enforced Virus Replication Actives Immunity upon Systemic VSV-EBOV Administration
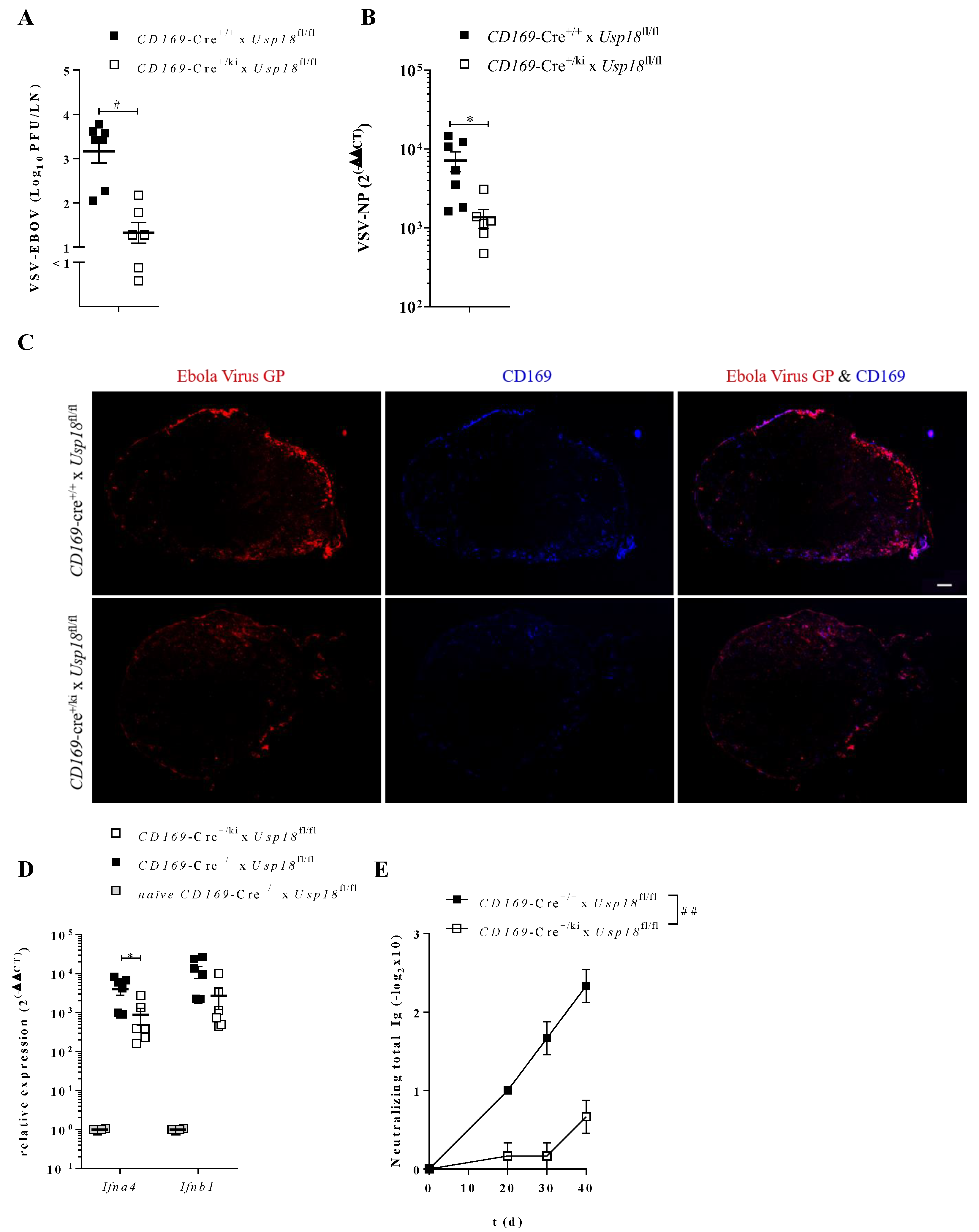
3.4. Enforced Virus Replication is Essential for Vaccination Success
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Volchkov, V.; Volchkova, V.A.; Muhlberger, E.; Kolesnikova, L.V.; Weik, M.; Dolnik, O.; Klenk, H.-D. Recovery of Infectious Ebola Virus from Complementary DNA: RNA Editing of the GP Gene and Viral Cytotoxicity. Science 2001, 291, 1965–1969. [Google Scholar] [CrossRef] [PubMed]
- Malvy, D.; McElroy, A.K.; de Clerck, H.; Günther, S.; van Griensven, J. Ebola virus disease. Lancet 2019, 393, 936–948. [Google Scholar] [CrossRef] [Green Version]
- Geisbert, T.W.; Daddario-DiCaprio, K.M.; Lewis, M.G.; Geisbert, J.B.; Grolla, A.; Leung, A.; Paragas, J.; Matthias, L.; Smith, M.A.; Jones, S.M.; et al. Vesicular Stomatitis Virus-Based Ebola Vaccine Is Well-Tolerated and Protects Immunocompromised Nonhuman Primates. PLoS Pathog. 2008, 4, e1000225. [Google Scholar] [CrossRef] [PubMed]
- Marzi, A.; Robertson, S.J.; Haddock, E.; Feldmann, F.; Hanley, P.W.; Scott, D.P.; Strong, J.E.; Kobinger, G.; Best, S.M.; Feldmann, H. EBOLA VACCINE. VSV-EBOV rapidly protects macaques against infection with the 2014/15 Ebola virus outbreak strain. Science 2015, 349, 739–742. [Google Scholar] [CrossRef] [Green Version]
- Suder, E.; Furuyama, W.; Feldmann, H.; Marzi, A.; De Wit, E. The vesicular stomatitis virus-based Ebola virus vaccine: From concept to clinical trials. Hum. Vaccines Immunother. 2018, 14, 2107–2113. [Google Scholar] [CrossRef] [Green Version]
- Poetsch, J.H.; Dahlke, C.; Zinser, M.E.; Kasonta, R.; Lunemann, S.; Rechtien, A.; Ly, M.L.; Stubbe, H.C.; Krähling, V.; Biedenkopf, N.; et al. Detectable Vesicular Stomatitis Virus (VSV)–Specific Humoral and Cellular Immune Responses Following VSV–Ebola Virus Vaccination in Humans. J. Infect. Dis. 2018, 219, 556–561. [Google Scholar] [CrossRef]
- EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/ervebo (accessed on 3 March 2020).
- Menicucci, A.R.; Jankeel, A.; Feldmann, H.; Marzi, A.; Messaoudi, I. Antiviral Innate Responses Induced by VSV-EBOV Vaccination Contribute to Rapid Protection. mBio 2019, 10, e00597-19. [Google Scholar] [CrossRef] [Green Version]
- Müller, S.; Hunziker, L.; Enzler, S.; Bühler-Jungo, M.; Di Santo, J.P.; Zinkernagel, R.M.; Mueller, C. Role of an Intact Splenic Microarchitecture in Early Lymphocytic Choriomeningitis Virus Production. J. Virol. 2002, 76, 2375–2383. [Google Scholar] [CrossRef] [Green Version]
- Gonzalez, N.A.; Guillen, J.; Gallardo, G.; Díaz, M.; De La Rosa, J.V.; Hernández, I.; Casanova-Acebes, M.; Lopez, F.; Tabraue, C.; Beceiro, S.; et al. The nuclear receptor LXRα controls the functional specialization of splenic macrophages. Nat. Immunol. 2013, 14, 831–839. [Google Scholar] [CrossRef] [Green Version]
- Habbeddine, M.; Verthuy, C.; Rastoin, O.; Chasson, L.; Bebien, M.; Bajenoff, M.; Adriouch, S.; Haan, J.D.; Penninger, J.M.; Lawrence, T. Receptor Activator of NF-κB Orchestrates Activation of Antiviral Memory CD8 T Cells in the Spleen Marginal Zone. Cell Rep. 2017, 21, 2515–2527. [Google Scholar] [CrossRef] [Green Version]
- Moseman, E.A.; Iannacone, M.; Bosurgi, L.; Tonti, E.; Chevrier, N.; Tumanov, A.; Fu, Y.-X.; Hacohen, N.; Von Andrian, U.H. B Cell Maintenance of Subcapsular Sinus Macrophages Protects against a Fatal Viral Infection Independent of Adaptive Immunity. Immun. 2012, 36, 415–426. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schulz, O.; Hammerschmidt, S.I.; Moschovakis, G.L.; Förster, R. Chemokines and Chemokine Receptors in Lymphoid Tissue Dynamics. Annu. Rev. Immunol. 2016, 34, 203–242. [Google Scholar] [CrossRef]
- Chã¡vez-Galã¡n, L.; Olleros, M.L.; Vesin, M.; Garcia, I. Much More than M1 and M2 Macrophages, There are also CD169+ and TCR+ Macrophages. Front. Immunol. 2015, 6, 263. [Google Scholar] [CrossRef] [PubMed]
- Eloranta, M.L.; Alm, G.V. Splenic Marginal Metallophilic Macrophages and Marginal Zone Macrophages are the Major Interferon-α/β Producers in Mice upon Intravenous Challenge with Herpes Simplex Virus. Scand. J. Immunol. 1999, 49, 391–394. [Google Scholar] [CrossRef] [PubMed]
- Iannacone, M.; Moseman, E.A.; Tonti, E.; Bosurgi, L.; Junt, T.; Henrickson, S.E.; Whelan, S.P.; Guidotti, L.G.; Von Andrian, U.H. Subcapsular sinus macrophages prevent CNS invasion on peripheral infection with a neurotropic virus. Nature 2010, 465, 1079–1083. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Junt, T.; Moseman, E.A.; Iannacone, M.; Massberg, S.; Lang, P.A.; Boes, M.; Fink, K.; Henrickson, S.E.; Shayakhmetov, D.M.; Di Paolo, N.C.; et al. Subcapsular sinus macrophages in lymph nodes clear lymph-borne viruses and present them to antiviral B cells. Nature 2007, 450, 110–114. [Google Scholar] [CrossRef] [PubMed]
- Honke, N.; Shaabani, N.; Cadeddu, G.; Sorg, U.R.; Zhang, N.-E.; Trilling, M.; Klingel, K.; Sauter, M.; Kandolf, R.; Gailus, N.; et al. Enforced viral replication activates adaptive immunity and is essential for the control of a cytopathic virus. Nat. Immunol. 2011, 13, 51–57. [Google Scholar] [CrossRef]
- Malakhova, O.A.; Kim, K.; Luo, J.-K.; Zou, W.; Kumar, K.G.S.; Fuchs, S.Y.; Shuai, K.; Zhang, D.-E. UBP43 is a novel regulator of interferon signaling independent of its ISG15 isopeptidase activity. EMBO J. 2006, 25, 2358–2367. [Google Scholar] [CrossRef]
- Samuel, C.E. Antiviral Actions of Interferons. Clin. Microbiol. Rev. 2001, 14, 778–809. [Google Scholar] [CrossRef] [Green Version]
- Zhou, Q.; Lavorgna, A.; Bowman, M.; Hiscott, J.; Harhaj, E.W. Aryl Hydrocarbon Receptor Interacting Protein Targets IRF7 to Suppress Antiviral Signaling and the Induction of Type I Interferon*. J. Boil. Chem. 2015, 290, 14729–14739. [Google Scholar] [CrossRef] [Green Version]
- Stark, G.R.; Kerr, I.M.; Williams, B.R.; Silverman, R.H.; Schreiber, R.D. HOW CELLS RESPOND TO INTERFERONS. Annu. Rev. Biochem. 1998, 67, 227–264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kastenmüller, W.; Torabi-Parizi, P.; Subramanian, N.; Lämmermann, T.; Germain, R.N. A Spatially-Organized Multicellular Innate Immune Response in Lymph Nodes Limits Systemic Pathogen Spread. Cell 2012, 150, 1235–1248. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garcia, Z.; Lemaître, F.; Van Rooijen, N.; Albert, M.L.; Levy, Y.; Schwartz, O.; Bousso, P. Subcapsular sinus macrophages promote NK cell accumulation and activation in response to lymph-borne viral particles. Blood 2012, 120, 4744–4750. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williamson, L.E.; Flyak, A.I.; Kose, N.; Bombardi, R.; Branchizio, A.; Reddy, S.; Davidson, E.; Doranz, B.J.; Fusco, M.L.; Saphire, E.O.; et al. Early Human B Cell Response to Ebola Virus in Four U.S. Survivors of Infection. J. Virol. 2019, 93, 01439-18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kalinke, U.; Oxenius, A.; López-Macías, C.; Zinkernagel, R.M.; Hengartner, H. Virus neutralization by germ-line vs. hypermutated antibodies. Proc. Natl. Acad. Sci. USA 2000, 97, 10126–10131. [Google Scholar] [CrossRef] [Green Version]
- Steinhoff, U.; Müller, U.; Schertler, A.; Hengartner, H.; Aguet, M.; Zinkernagel, R.M. Antiviral protection by vesicular stomatitis virus-specific antibodies in alpha/beta interferon receptor-deficient mice. J. Virol. 1995, 69, 2153–2158. [Google Scholar] [CrossRef] [Green Version]
- Goldmann, T.; Zeller, N.; Raasch, J.; Kierdorf, K.; Frenzel, K.; Ketscher, L.; Basters, A.; Staszewski, O.; Brendecke, S.M.; Spiess, A.; et al. USP 18 lack in microglia causes destructive interferonopathy of the mouse brain. EMBO J. 2015, 34, 1612–1629. [Google Scholar] [CrossRef] [Green Version]
- Asano, K.; Takahashi, N.; Ushiki, M.; Monya, M.; Aihara, F.; Kuboki, E.; Moriyama, S.; Iida, M.; Kitamura, H.; Qiu, C.-H.; et al. Intestinal CD169+ macrophages initiate mucosal inflammation by secreting CCL8 that recruits inflammatory monocytes. Nat. Commun. 2015, 6, 7802. [Google Scholar] [CrossRef]
- Honke, N.; Shaabani, N.; Zhang, N.-E.; Iliakis, G.; Xu, H.C.; Häussinger, D.; Recher, M.; Löhning, M.; Lang, P.A.; Lang, K.S. Usp18 Driven Enforced Viral Replication in Dendritic Cells Contributes to Break of Immunological Tolerance in Autoimmune Diabetes. PLoS Pathog. 2013, 9, e1003650. [Google Scholar] [CrossRef] [Green Version]
- Schutsky, K.; Curtis, D.; Bongiorno, E.K.; Barkhouse, D.A.; Kean, R.B.; Dietzschold, B.; Hooper, D.; Faber, M. Intramuscular Inoculation of Mice with the Live-Attenuated Recombinant Rabies Virus TriGAS Results in a Transient Infection of the Draining Lymph Nodes and a Robust, Long-Lasting Protective Immune Response against Rabies. J. Virol. 2012, 87, 1834–1841. [Google Scholar] [CrossRef] [Green Version]
- Baccala, R.; Kono, D.H.; Theofilopoulos, A.N. Interferons as pathogenic effectors in autoimmunity. Immunol. Rev. 2005, 204, 9–26. [Google Scholar] [CrossRef]
- Cembrzyńska-Nowak, M.; Liebhart, J.; Bieńkowska-Haba, M.; Liebhart, E.; Kulczak, A.; Siemieniec, I.; Dobek, R.; Dor, A.; Barg, W.; Panaszek, B. The overproduction of nitric oxide associated with neutrophilic predominance is relevant to airway mycotic infections in asthmatics undergoing prolonged glucocorticoid treatment. Cell. Mol. Boil. Lett. 2005, 10, 677–687. [Google Scholar]
- Elson, C.O.; Cong, Y.; McCracken, V.; Dimmitt, R.A.; Lorenz, R.; Weaver, C.T. Experimental models of inflammatory bowel disease reveal innate, adaptive, and regulatory mechanisms of host dialogue with the microbiota. Immunol. Rev. 2005, 206, 260–276. [Google Scholar] [CrossRef]
- Jung, D.Y.; Lee, H.; Jung, B.-Y.; Ock, J.; Lee, M.-S.; Lee, W.-H.; Suk, K. TLR4, but not TLR2, signals autoregulatory apoptosis of cultured microglia: A critical role of IFN-beta as a decision maker. J. Immunol. 2005, 174, 6467–6476. [Google Scholar] [CrossRef]
- Lehnardt, S.; Massillon, L.; Follett, P.; Jensen, F.E.; Ratan, R.; Rosenberg, P.A.; Volpe, J.J.; Vartanian, T. Activation of innate immunity in the CNS triggers neurodegeneration through a Toll-like receptor 4-dependent pathway. Proc. Natl. Acad. Sci. USA 2003, 100, 8514–8519. [Google Scholar] [CrossRef] [Green Version]
- Zhou, S.; Kurt-Jones, E.A.; Fitzgerald, K.A.; Wang, J.P.; Cerny, A.M.; Chan, M.; Finberg, R.W. Role of MyD88 in route-dependent susceptibility to vesicular stomatitis virus infection. J. Immunol. 2007, 178, 5173–5181. [Google Scholar] [CrossRef]
- Honke, N.; Shaabani, N.; Zhang, N.-E.; Hardt, C.; Lang, K.S. Multiple functions of USP18. Cell Death Dis. 2016, 7, e2444. [Google Scholar] [CrossRef] [Green Version]
- Cong, X.-L.; Lo, M.-C.; Reuter, B.A.; Yan, M.; Fan, J.-B.; Zhang, D.-E. Usp18 promotes conventional CD11b+ dendritic cell development. J. Immunol. 2012, 188, 4776–4781. [Google Scholar] [CrossRef] [Green Version]
- Garbutt, M.; Liebscher, R.; Wahl, V.; Jones, S.; Möller, P.; Wagner, R.; Volchkov, V.; Klenk, H.-D.; Feldmann, H.; Ströher, U. Properties of Replication-Competent Vesicular Stomatitis Virus Vectors Expressing Glycoproteins of Filoviruses and Arenaviruses. J. Virol. 2004, 78, 5458–5465. [Google Scholar] [CrossRef] [Green Version]
- Perez-Zsolt, D.; Erkizia, I.; Pino, M.; García-Gallo, M.; Martin, M.T.; Benet, S.; Chojnacki, J.; Fernández-Figueras, M.T.; Guerrero, D.; Urrea, V.; et al. Anti-Siglec-1 antibodies block Ebola viral uptake and decrease cytoplasmic viral entry. Nat. Microbiol. 2019, 4, 1558–1570. [Google Scholar] [CrossRef]
- Bucasas, K.L.; Franco, L.M.; Shaw, C.; Bray, M.S.; Wells, J.M.; Niño, D.; Arden, N.; Quarles, J.M.; Couch, R.B.; Belmont, J.W. Early Patterns of Gene Expression Correlate with the Humoral Immune Response to Influenza Vaccination in Humans. J. Infect. Dis. 2011, 203, 921–929. [Google Scholar] [CrossRef] [Green Version]
- Haralambieva, I.H.; Simon, W.L.; Kennedy, R.B.; Ovsyannikova, I.G.; Warner, N.D.; Grill, D.; Poland, G.A. Profiling of Measles-Specific Humoral Immunity in Individuals Following Two Doses of MMR Vaccine Using Proteome Microarrays. Viruses 2015, 7, 1113–1133. [Google Scholar] [CrossRef] [Green Version]
- Marzi, A.; Engelmann, F.; Feldmann, F.; Haberthur, K.; Shupert, W.L.; Brining, U.; Scott, D.P.; Geisbert, T.W.; Kawaoka, Y.; Katze, M.G.; et al. Antibodies are necessary for rVSV/ZEBOV-GP–mediated protection against lethal Ebola virus challenge in nonhuman primates. Proc. Natl. Acad. Sci. USA 2013, 110, 1893–1898. [Google Scholar] [CrossRef] [Green Version]
- Emanuel, J.; Callison, J.; Dowd, K.A.; Pierson, T.C.; Feldmann, H.; Marzi, A. A VSV-based Zika virus vaccine protects mice from lethal challenge. Sci. Rep. 2018, 8, 11043. [Google Scholar] [CrossRef]
- Rose, J.K.; Clarke, D.K.; Pattnaik, A.K.; Whitt, M.A. RHABDOVIRUSES AS VACCINE VECTORS: FROM INITIAL DEVELOPMENT TO CLINICAL TRIALS. In Biology and Pathogenesis of Rhabdo- and Filoviruses; World Scientific Pub Co Pte Lt.: Singapore, 2014; pp. 199–230. [Google Scholar]
- Müller, U.; Steinhoff, U.; Reis, L.; Hemmi, S.; Pavlovic, J.; Zinkernagel, R.; Aguet, M. Functional role of type I and type II interferons in antiviral defense. Sci. 1994, 264, 1918–1921. [Google Scholar] [CrossRef]
- Trottier, M.D.; Palian, B.M.; Reiss, C.S. VSV replication in neurons is inhibited by type I IFN at multiple stages of infection. Virol. 2005, 333, 215–225. [Google Scholar] [CrossRef] [Green Version]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Friedrich, S.-K.; Schmitz, R.; Bergerhausen, M.; Lang, J.; Cham, L.B.; Duhan, V.; Häussinger, D.; Hardt, C.; Addo, M.; Prinz, M.; et al. Usp18 Expression in CD169+ Macrophages is Important for Strong Immune Response after Vaccination with VSV-EBOV. Vaccines 2020, 8, 142. https://doi.org/10.3390/vaccines8010142
Friedrich S-K, Schmitz R, Bergerhausen M, Lang J, Cham LB, Duhan V, Häussinger D, Hardt C, Addo M, Prinz M, et al. Usp18 Expression in CD169+ Macrophages is Important for Strong Immune Response after Vaccination with VSV-EBOV. Vaccines. 2020; 8(1):142. https://doi.org/10.3390/vaccines8010142
Chicago/Turabian StyleFriedrich, Sarah-Kim, Rosa Schmitz, Michael Bergerhausen, Judith Lang, Lamin B. Cham, Vikas Duhan, Dieter Häussinger, Cornelia Hardt, Marylyn Addo, Marco Prinz, and et al. 2020. "Usp18 Expression in CD169+ Macrophages is Important for Strong Immune Response after Vaccination with VSV-EBOV" Vaccines 8, no. 1: 142. https://doi.org/10.3390/vaccines8010142
APA StyleFriedrich, S.-K., Schmitz, R., Bergerhausen, M., Lang, J., Cham, L. B., Duhan, V., Häussinger, D., Hardt, C., Addo, M., Prinz, M., Asano, K., Lang, P. A., & Lang, K. S. (2020). Usp18 Expression in CD169+ Macrophages is Important for Strong Immune Response after Vaccination with VSV-EBOV. Vaccines, 8(1), 142. https://doi.org/10.3390/vaccines8010142






