A Retrospective Cohort Study of Safety Outcomes in New Zealand Infants Exposed to Tdap Vaccine in Utero
Abstract
1. Introduction
2. Methods
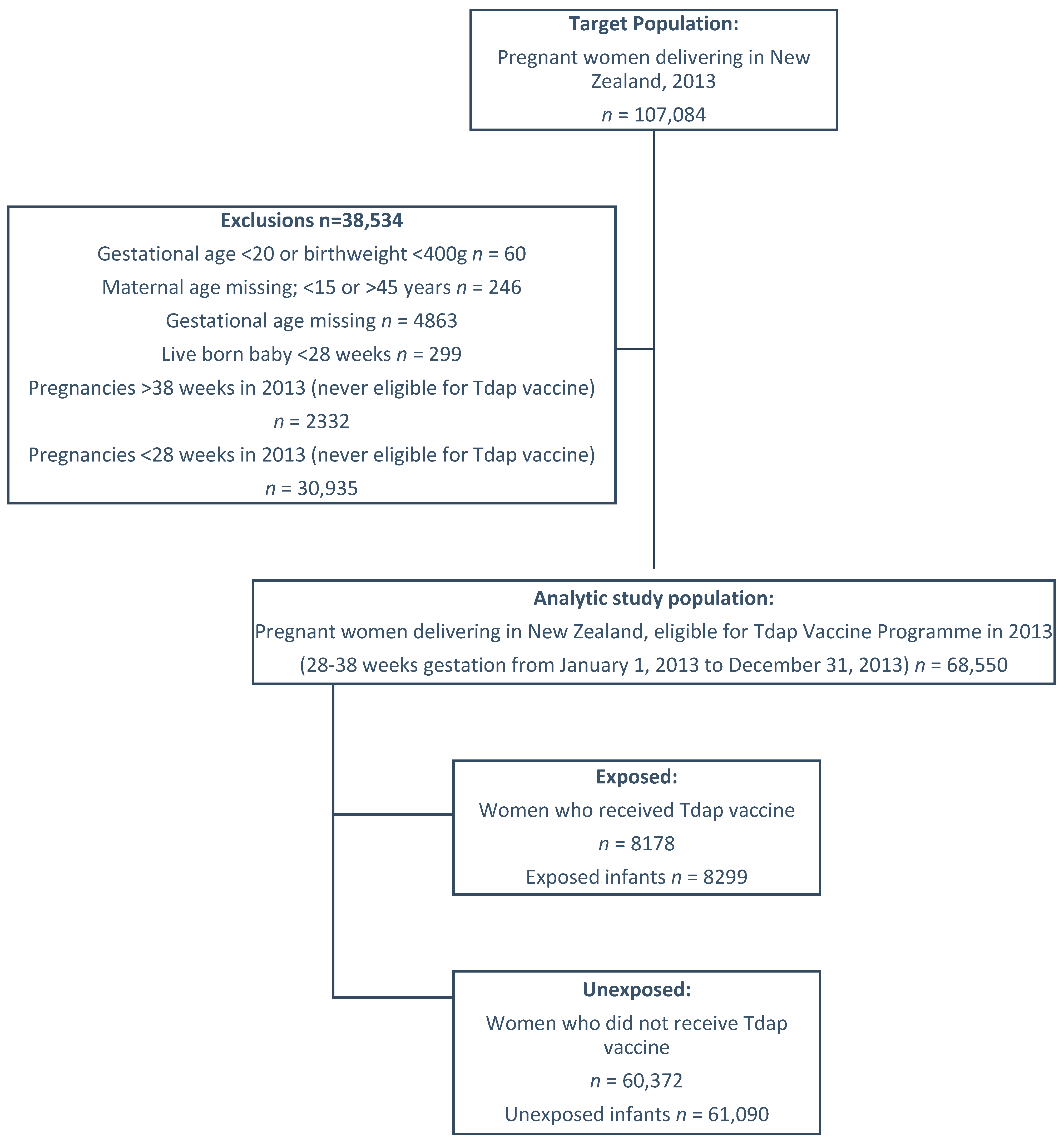
2.1. Study Population and Variables
2.2. Study Outcomes
2.3. Data Sources
2.4. Statistical Methods
3. Results
3.1. Study Cohort
3.2. Events of Delivery
3.3. Physical Examination and Anthropometric Measurements
3.4. Congenital Anomalies
3.5. Neonatal Conditions Classified by Organ System
3.6. Infant Death
4. Discussion
5. Interpretation
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Fulton, T.R.; Phadke, V.K.; Orenstein, W.A.; Hinman, A.R.; Johnson, W.D.; Omer, S.B. Protective effect of contemporary pertussis vaccines: A systematic review and meta-analysis. Clin. Infect. Dis. 2016, 62, 1100–1110. [Google Scholar] [CrossRef] [PubMed]
- Falleiros Arlant, L.H.; de Colsa, A.; Flores, D.; Brea, J.; Avila Aguero, M.L.; Hozbor, D.F. Pertussis in Latin America: Epidemiology and control strategies. Expert Rev. Anti-Infect. Ther. 2014, 12, 1265–1275. [Google Scholar] [CrossRef] [PubMed]
- Radke, S.; Petousis-Harris, H.; Watson, D.; Gentles, D.; Turner, N. Age-specific effectiveness following each dose of acellular pertussis vaccine among infants and children in New Zealand. Vaccine 2017, 35, 177–183. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Warfel, J.M.; Zimmerman, L.I.; Merkel, T.J. Acellular pertussis vaccines protect against disease but fail to prevent infection and transmission in a nonhuman primate model. Proc. Natl. Acad. Sci. USA 2014, 111, 787–792. [Google Scholar] [CrossRef] [PubMed]
- Althouse, B.M.; Scarpino, S.V. Asymptomatic transmission and the resurgence of Bordetella pertussis. BMC Med. 2015, 13, 146. [Google Scholar] [CrossRef] [PubMed]
- Blencowe, H.; Lawn, J.; Vandelaer, J.; Roper, M.; Cousens, S. Tetanus toxoid immunization to reduce mortality from neonatal tetanus. Int. J. Epidemiol. 2010, 39 (Suppl. 1), i102–i109. [Google Scholar] [CrossRef] [PubMed]
- Tapia, M.D.; Sow, S.O.; Tamboura, B.; Tégueté, I.; Pasetti, M.F.; Kodio, M.; Onwuchekwa, U.; Tennant, S.M.; Blackwelder, W.C.; Coulibaly, F.; et al. Maternal immunisation with trivalent inactivated influenza vaccine for prevention of influenza in infants in Mali: A prospective, active-controlled, observer-blind, randomised phase 4 trial. Lancet Infect. Dis. 2016, 16, 1026–1035. [Google Scholar] [CrossRef]
- Centers for Disease Control Prevention. Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine (Tdap) in pregnant women and persons who have or anticipate having close contact with an infant aged <12 months—Advisory Committee on Immunization Practices (ACIP), 2011. MMWR. Morb. Mortal. Wkly. Rep. 2011, 60, 1424–1426. [Google Scholar]
- Davies, S.C. Temporary Programme of Pertussis (Whooping Cough) Vaccination of Pregnant Women; Department of Health, Ed.; Department of Health: London, UK, 2012.
- Amirthalingam, G.; Andrews, N.; Campbell, H.; Ribeiro, S.; Kara, E.; Donegan, K.; Fry, N.K.; Miller, E.; Ramsay, M. Effectiveness of maternal pertussis vaccination in England: An observational study. Lancet 2014, 384, 1521–1528. [Google Scholar] [CrossRef]
- Dabrera, G.; Amirthalingam, G.; Andrews, N.; Campbell, H.; Ribeiro, S.; Kara, E.; Fry, N.K.; Ramsay, M. A case-control study to estimate the effectiveness of maternal pertussis vaccination in protecting newborn infants in England and Wales, 2012–2013. Clin. Infect. Dis. 2015, 60, 333–337. [Google Scholar] [CrossRef]
- Amirthalingam, G.; Campbell, H.; Ribeiro, S.; Fry, N.K.; Ramsay, M.; Miller, E.; Andrews, N. Sustained effectiveness of the maternal pertussis immunization program in England 3 years following introduction. Clin. Infect. Dis. 2016, 63 (Suppl. 4), S236–S243. [Google Scholar] [CrossRef]
- Baxter, R.; Bartlett, J.; Fireman, B.; Lewis, E.; Klein, N.P. Effectiveness of vaccination during pregnancy to prevent infant pertussis. Pediatrics 2017, 139, e20164091. [Google Scholar] [CrossRef] [PubMed]
- Keller-Stanislawski, B.; Englund, J.A.; Kang, G.; Mangtani, P.; Neuzil, K.; Nohynek, H.; Pless, R.; Lambach, P.; Zuber, P. Safety of immunization during pregnancy: A review of the evidence of selected inactivated and live attenuated vaccines. Vaccine 2014, 32, 7057–7064. [Google Scholar] [CrossRef] [PubMed]
- Griffin, J.B.; Yu, L.; Watson, D.; Turner, N.; Walls, T.; Howe, A.S.; Jiang, Y.; Petousis-Harris, H. Pertussis Immunisation in Pregnancy Safety (PIPS) Study: A retrospective cohort study of safety outcomes in pregnant women vaccinated with Tdap vaccine. Vaccine 2018, 36, 5173–5179. [Google Scholar] [CrossRef] [PubMed]
- Munoz, F.M.; Eckert, L.O.; Katz, M.A.; Lambach, P.; Ortiz, J.R.; Bauwens, J.; Bonhoeffer, J. Key terms for the assessment of the safety of vaccines in pregnancy: Results of a global consultative process to initiate harmonization of adverse event definitions. Vaccine 2015, 33, 6441–6452. [Google Scholar] [CrossRef] [PubMed]
- Sukumaran, L.; McCarthy, N.L.; Kharbanda, E.O.; Vazquez-Benitez, G.; Lipkind, H.S.; Jackson, L.; Klein, N.P.; Naleway, A.L.; McClure, D.L.; Hechter, R.C. Infant hospitalizations and mortality after maternal vaccination. Pediatrics 2018, 141, e20173310. [Google Scholar] [CrossRef] [PubMed]
- Kharbanda, E.O.; Vazquez-Benitez, G.; Lipkind, H.S.; Klein, N.P.; Cheetham, T.C.; Naleway, A.; Omer, S.B.; Hambidge, S.J.; Lee, G.M.; Jackson, M.L.; et al. Evaluation of the association of maternal pertussis vaccination with obstetric events and birth outcomes. JAMA 2014, 312, 1897–1904. [Google Scholar] [CrossRef] [PubMed]
- Sukumaran, L.; McCarthy, N.L.; Kharbanda, E.O.; Weintraub, E.S.; Vazquez-Benitez, G.; McNeil, M.M.; Li, R.; Klein, N.P.; Hambidge, S.J.; Naleway, A.L.; et al. Safety of Tetanus Toxoid, Reduced Diphtheria Toxoid, and Acellular Pertussis and Influenza Vaccinations in Pregnancy. Obstet. Gynecol. 2015, 126, 1069–1074. [Google Scholar] [CrossRef] [PubMed]
- Berenson, A.B.; Hirth, J.M.; Rahman, M.; Laz, T.H.; Rupp, R.E.; Sarpong, K.O. Maternal and infant outcomes among women vaccinated against pertussis during pregnancy. Hum. Vaccines Immunother. 2016, 12, 1965–1971. [Google Scholar] [CrossRef] [PubMed]
- Morgan, J.L.; Baggari, S.R.; McIntire, D.D.; Sheffield, J.S. Pregnancy outcomes after antepartum tetanus, diphtheria, and acellular pertussis vaccination. Obstet. Gynecol. 2015, 125, 1433–1438. [Google Scholar] [CrossRef] [PubMed]
- Donegan, K.; King, B.; Bryan, P. Safety of pertussis vaccination in pregnant women in UK: Observational study. BMJ 2014, 349, g4219. [Google Scholar] [CrossRef] [PubMed]
- Vazquez-Benitez, G.; Kharbanda, E.O.; Naleway, A.L.; Lipkind, H.; Sukumaran, L.; McCarthy, N.L.; Omer, S.B.; Qian, L.; Xu, S.; Jackson, M.L. Risk of preterm or small-for-gestational-age birth after influenza vaccination during pregnancy: Caveats when conducting retrospective observational studies. Am. J. Epidemiol. 2016, 184, 176–186. [Google Scholar] [CrossRef] [PubMed]
- DeSilva, M.; Vazquez-Benitez, G.; Nordin, J.D.; Lipkind, H.S.; Romitti, P.A.; DeStefano, F.; Kharbanda, E.O. Tdap vaccination during pregnancy and microcephaly and other structural birth defects in offspring. JAMA 2016, 316, 1823–1825. [Google Scholar] [CrossRef] [PubMed]
- Wiley, K.; Massey, P.; Cooper, S.; Wood, N.; Quinn, H.; Leask, J. Pregnant women’s intention to take up a post-partum pertussis vaccine, and their willingness to take up the vaccine while pregnant: A cross sectional survey. Vaccine 2013, 31, 3972–3978. [Google Scholar] [CrossRef] [PubMed]
| Mother Tdap Vaccination | Total | |||||
|---|---|---|---|---|---|---|
| Infants Exposed | Infants Unexposed | |||||
| N | % | N | % | N | % | |
| Total | 8299 | 12.0 | 61,090 | 88.0 | 69,389 | 100.0 |
| Infant characteristics | ||||||
| Gender | ||||||
| Male | 4249 | 51.2 | 31,283 | 51.2 | 35,532 | 51.2 |
| Female | 4050 | 48.8 | 29,805 | 48.8 | 33,855 | 48.8 |
| Missing | 0 | 0.0 | 2 | 0.0 | 2 | 0.0 |
| Infant ethnicity | ||||||
| Maori | 1098 | 13.2 | 17,271 | 28.3 | 18,369 | 26.5 |
| Pacific | 420 | 5.1 | 7022 | 11.5 | 7442 | 10.7 |
| Asian | 1216 | 14.7 | 8629 | 14.1 | 9845 | 14.2 |
| European/Other | 5563 | 67.0 | 28,142 | 46.1 | 33,705 | 48.6 |
| Missing | 2 | 0.0 | 26 | 0.0 | 28 | 0.0 |
| NZ Deprivation Index 2013 | ||||||
| 1–2 (least deprived) | 1805 | 21.7 | 7937 | 13.0 | 9742 | 14.0 |
| 3–4 | 1783 | 21.5 | 9216 | 15.1 | 10,999 | 15.9 |
| 5–6 | 1697 | 20.4 | 10,861 | 17.8 | 12,558 | 18.1 |
| 7–8 | 1751 | 21.1 | 14,106 | 23.1 | 15,857 | 22.9 |
| 9–10 (most deprived) | 1263 | 15.2 | 18,963 | 31.0 | 20,226 | 29.1 |
| Missing | 0 | 0.0 | 7 | 0.0 | 7 | 0.0 |
| Apgar score at 5 min after birth | ||||||
| Mean (SD) | 9.5 (0.9) | 9.5 (0.9) | 9.5 (0.9) | |||
| Median (Q1,Q3) | 10.0 (9.0,10.0) | 10.0 (9.0,10.0) | 10.0 (9.0,10.0) | |||
| Birth weight (g) | ||||||
| Mean (SD) | 3467.3 (532.5) | 3429.0 (592.5) | 3433.6 (585.6) | |||
| Median (Q1,Q3) | 3485.0 (3140.0,3800.0) | 3450.0 (3090.0,3795.0) | 3450.0 (3100.0,3800.0) | |||
| Mother characteristics | ||||||
| Age (years) at last menstrual period | ||||||
| Mean (SD) | 30.7 (5.4) | 28.3 (6.1) | 28.6 (6.1) | |||
| Median (Q1,Q3) | 31.0 (27.0,35.0) | 28.0 (24.0,33.0) | 29.0 (24.0,33.0) | |||
| Parity | ||||||
| 0 | 3642 | 43.9 | 21,916 | 35.9 | 25,558 | 36.8 |
| 1 | 2915 | 35.1 | 19,085 | 31.2 | 22,000 | 31.7 |
| 2 | 1023 | 12.3 | 8840 | 14.5 | 9863 | 14.2 |
| 3 | 266 | 3.2 | 3652 | 6.0 | 3918 | 5.6 |
| 4 | 71 | 0.9 | 1529 | 2.5 | 1600 | 2.3 |
| 5 | 25 | 0.3 | 783 | 1.3 | 808 | 1.2 |
| 6+ | 16 | 0.2 | 752 | 1.2 | 768 | 1.1 |
| Missing | 341 | 4.1 | 4533 | 7.4 | 4874 | 7.0 |
| History of stillbirth | ||||||
| Yes | 77 | 0.9 | 596 | 1.0 | 673 | 1.0 |
| No | 8222 | 99.1 | 60,494 | 99.0 | 68,716 | 99.0 |
| History of preterm birth | ||||||
| Yes | 214 | 2.6 | 1961 | 3.2 | 2175 | 3.1 |
| No | 8085 | 97.4 | 59,129 | 96.8 | 67,214 | 96.9 |
| History of chronic disease | ||||||
| Yes | 111 | 1.3 | 956 | 1.6 | 1067 | 1.5 |
| No | 8188 | 98.7 | 60,134 | 98.4 | 68,322 | 98.5 |
| History of antenatal care (no. of LMC visits) | ||||||
| Mean (SD) | 9.7 (3.5) | 9.2 (3.8) | 9.3 (3.8) | |||
| Median (Q1,Q3) | 10.0 (7.0,12.0) | 9.0 (7.0,12.0) | 9.0 (7.0,12.0) | |||
| Model of care | ||||||
| DHB | 325 | 3.9 | 3388 | 5.5 | 3713 | 5.4 |
| MWF | 6615 | 79.7 | 51,181 | 83.8 | 57,796 | 83.3 |
| GP | 111 | 1.3 | 442 | 0.7 | 553 | 0.8 |
| OBS | 1024 | 12.3 | 2878 | 4.7 | 3902 | 5.6 |
| Other | 13 | 0.2 | 28 | 0.0 | 41 | 0.1 |
| No LMC | 211 | 2.5 | 3173 | 5.2 | 3384 | 4.9 |
| Mother BMI | ||||||
| Mean (SD) | 25.4 (5.4) | 26.5 (6.2) | 26.3 (6.1) | |||
| Median (Q1,Q3) | 24.0 (22.0,28.0) | 25.0 (22.0,30.0) | 25.0 (22.0,29.0) | |||
| Current tobacco use | ||||||
| Yes | 550 | 6.6 | 11,823 | 19.4 | 12,373 | 17.8 |
| No | 7749 | 93.4 | 49,267 | 80.6 | 57,016 | 82.2 |
| Influenza vaccination | ||||||
| Yes | 3833 | 46.2 | 5187 | 8.5 | 9020 | 13.0 |
| No | 4466 | 53.8 | 55,903 | 91.5 | 60,369 | 87.0 |
| Outcome † | Description | Tdap (Exposed = 1, Unexposed = 0) | N (%) | Unadjusted OR ‡ (95% CI) | p Value | Adjusted OR ‡§ (95% CI) | p Value |
|---|---|---|---|---|---|---|---|
| Effects of delivery | |||||||
| P00 | Fetus and newborn affected by maternal conditions | 1 | 14 (0.2) | 1.085 (0.619,1.902) | 0.7760 | 1.062 (0.558,2.020) | 0.8550 |
| 0 | 95 (0.2) | ||||||
| P01 | Fetus and newborn affected by maternal complications of pregnancy | 1 | 19 (0.2) | 0.999 (0.618,1.614) | 0.9968 | 0.906 (0.526,1.561) | 0.7229 |
| 0 | 140 (0.2) | ||||||
| P02 | Fetus and newborn affected by abnormality of membranes | 1 | 27 (0.3) | 1.163 (0.774,1.746) | 0.4670 | 0.911 (0.557,1.490) | 0.7112 |
| 0 | 171 (0.3) | ||||||
| P03 | Fetus and newborn affected by complications of labor and delivery | 1 | 131 (1.6) | 1.169 (0.971,1.407) | 0.0999 | 0.931 (0.750,1.155) | 0.5141 |
| 0 | 827 (1.4) | ||||||
| Physical examination and anthropometric measurements | |||||||
| P05.12 | Small for gestational age (SGA) | 1 | 117 (1.4) | 0.711 (0.587,0.861) | 0.0005 | 0.721 (0.574,0.905) | 0.0047 |
| 0 | 1204 (2.0) | ||||||
| P05.29 | Other fetal malnutrition | 1 | 92 (1.1) | 0.832 (0.670,1.034) | 0.0969 | 1.036 (0.807,1.329) | 0.7833 |
| 0 | 812 (1.3) | ||||||
| P07.13 | Low birth weight (LBW): 1500 to <2500 g | 1 | 186 (2.2) | 0.755 (0.648,0.880) | 0.0003 | 0.784 (0.653,0.941) | 0.0089 |
| 0 | 1800 (2.9) | ||||||
| P07.323 | Moderate to late preterm: 32 to <37 weeks | 1 | 398 (4.8) | 0.852 (0.766,0.947) | 0.0031 | 0.831 (0.729,0.947) | 0.0055 |
| 0 | 3412 (5.6) | ||||||
| P08.0 | High birth weight | 1 | 45 (0.5) | 0.883 (0.647,1.204) | 0.4303 | 1.157 (0.824,1.625) | 0.3995 |
| 0 | 375 (0.6) | ||||||
| P08.1 | Large for gestational age infants | 1 | 31 (0.4) | 0.680 (0.470,0.983) | 0.0403 | 0.567 (0.359,0.894) | 0.0147 |
| 0 | 335 (0.5) | ||||||
| P12 | Scalp injury due to birth trauma | 1 | 84 (1.0) | 1.171 (0.929,1.475) | 0.1819 | 0.940 (0.720,1.228) | 0.6514 |
| 0 | 529 (0.9) | ||||||
| P15.4 | Birth trauma to face | 1 | 28 (0.3) | 1.079 (0.726,1.606) | 0.7063 | 0.772 (0.484,1.232) | 0.2781 |
| 0 | 191 (0.3) | ||||||
| P15.8 | Other specified birth trauma | 1 | 10 (0.1) | 0.775 (0.404,1.487) | 0.4430 | 0.670 (0.308,1.458) | 0.3122 |
| 0 | 95 (0.2) | ||||||
| Neonatal conditions classified by organ system | |||||||
| P20 | Intrauterine hypoxia | 1 | 28 (0.3) | 0.698 (0.473,1.029) | 0.0692 | 0.670 (0.429,1.047) | 0.0788 |
| 0 | 295 (0.5) | ||||||
| P21 | Asphyxia | 1 | 49 (0.6) | 1.135 (0.839,1.535) | 0.4104 | 1.374 (0.968,1.951) | 0.0751 |
| 0 | 318 (0.5) | ||||||
| P22.0 | Respiratory distress syndrome | 1 | 121 (1.5) | 0.635 (0.526,0.765) | <0.0001 | 0.652 (0.524,0.811) | 0.0001 |
| 0 | 1392 (2.3) | ||||||
| P22.1 | Transient tachypnea of newborn | 1 | 247 (3.0) | 0.891 (0.779,1.018) | 0.0906 | 0.839 (0.721,0.975) | 0.0224 |
| 0 | 2034 (3.3) | ||||||
| P22.89_P28.2589 | Respiratory distress | 1 | 230 (2.8) | 1.060 (0.921,1.219) | 0.4165 | 0.998 (0.850,1.171) | 0.9775 |
| 0 | 1600 (2.6) | ||||||
| P23 | Congenital pneumonia | 1 | 24 (0.3) | 0.870 (0.569,1.329) | 0.5192 | 1.010 (0.629,1.622) | 0.9675 |
| 0 | 203 (0.3) | ||||||
| P24.0 | Meconium aspiration syndrome | 1 | 11 (0.1) | 0.736 (0.396,1.369) | 0.3330 | 0.977 (0.497,1.921) | 0.9461 |
| 0 | 110 (0.2) | ||||||
| P25 | Interstitial emphysema and related conditions | 1 | 43 (0.5) | 1.344 (0.970,1.861) | 0.0754 | 1.240 (0.860,1.787) | 0.2495 |
| 0 | 236 (0.4) | ||||||
| P28.34 | Apnea | 1 | 70 (0.8) | 0.702 (0.549,0.899) | 0.0049 | 0.777 (0.585,1.031) | 0.0803 |
| 0 | 731 (1.2) | ||||||
| P29.1 | Tachycardia or bradycardia | 1 | 55 (0.7) | 0.785 (0.594,1.037) | 0.0888 | 0.691 (0.501,0.954) | 0.0245 |
| 0 | 515 (0.8) | ||||||
| P29.82 | Benign and innocent cardiac murmurs in newborn | 1 | 34 (0.4) | 1.193 (0.830,1.715) | 0.3415 | 1.098 (0.724,1.667) | 0.6598 |
| 0 | 210 (0.3) | ||||||
| P36.89 | Bacterial sepsis of newborn, specified or unspecified | 1 | 37 (0.4) | 0.803 (0.571,1.128) | 0.2052 | 0.872 (0.599,1.270) | 0.4763 |
| 0 | 339 (0.6) | ||||||
| P37.5 | Candidiasis | 1 | 17 (0.2) | 0.702 (0.427,1.156) | 0.1645 | 0.656 (0.381,1.131) | 0.1294 |
| 0 | 178 (0.3) | ||||||
| P38 | Omphalitis | 1 | 29 (0.3) | 1.180 (0.797,1.748) | 0.4085 | 1.399 (0.875,2.236) | 0.1606 |
| 0 | 181 (0.3) | ||||||
| P39.1 | Neonatal conjunctivitis and dacryocystitis | 1 | 82 (1.0) | 0.961 (0.763,1.211) | 0.7383 | 0.841 (0.641,1.103) | 0.2111 |
| 0 | 628 (1.0) | ||||||
| P39.4 | Neonatal skin infection | 1 | 13 (0.2) | 1.153 (0.642,2.070) | 0.6329 | 1.352 (0.706,2.593) | 0.3631 |
| 0 | 83 (0.1) | ||||||
| P54 | Neonatal hemorrhage | 1 | 18 (0.2) | 0.914 (0.560,1.492) | 0.7180 | 0.981 (0.571,1.683) | 0.9435 |
| 0 | 145 (0.2) | ||||||
| P55 | Haemolytic diseases | 1 | 39 (0.5) | 0.689 (0.496,0.957) | 0.0263 | 0.663 (0.444,0.990) | 0.0445 |
| 0 | 416 (0.7) | ||||||
| P59 | Other neonatal jaundice | 1 | 308 (3.7) | 0.827 (0.733,0.932) | 0.0019 | 0.869 (0.757,0.998) | 0.0466 |
| 0 | 2722 (4.5) | ||||||
| P61.0 | Thrombocytopenia | 1 | 13 (0.2) | 0.633 (0.359,1.116) | 0.1141 | 0.830 (0.440,1.567) | 0.5657 |
| 0 | 151 (0.2) | ||||||
| P61.234 | Anaemia | 1 | 20 (0.2) | 0.574 (0.364,0.905) | 0.0170 | 0.461 (0.270,0.786) | 0.0045 |
| 0 | 256 (0.4) | ||||||
| P70.0 | Syndrome of infant of mother with gestational diabetes | 1 | 50 (0.6) | 0.682 (0.510,0.912) | 0.0099 | 0.683 (0.487,0.960) | 0.0281 |
| 0 | 538 (0.9) | ||||||
| P70.1 | Syndrome of infant of a diabetic mother | 1 | 18 (0.2) | 0.633 (0.391,1.025) | 0.0631 | 0.601 (0.278,1.300) | 0.1957 |
| 0 | 209 (0.3) | ||||||
| P70.34 | Hypoglycemia | 1 | 236 (2.8) | 0.792 (0.691,0.907) | 0.0008 | 0.795 (0.681,0.929) | 0.0038 |
| 0 | 2178 (3.6) | ||||||
| P74.1 | Dehydration of newborn | 1 | 58 (0.7) | 1.155 (0.875,1.525) | 0.3091 | 1.093 (0.794,1.503) | 0.5868 |
| 0 | 370 (0.6) | ||||||
| P74.23 | Electrolyte anomalies (Na, K) | 1 | 57 (0.7) | 0.781 (0.594,1.028) | 0.0778 | 0.844 (0.621,1.147) | 0.2786 |
| 0 | 536 (0.9) | ||||||
| P80 | Hypothermia | 1 | 73 (0.9) | 0.861 (0.675,1.099) | 0.2297 | 0.964 (0.726,1.279) | 0.7996 |
| 0 | 623 (1.0) | ||||||
| P81 | Other disturbances of temperature regulation of newborn | 1 | 59 (0.7) | 1.287 (0.975,1.699) | 0.0744 | 1.297 (0.947,1.775) | 0.1052 |
| 0 | 338 (0.6) | ||||||
| P83.1 | Neonatal erythema toxicum | 1 | 47 (0.6) | 1.583 (1.154,2.171) | 0.0044 | 1.661 (1.163,2.372) | 0.0052 |
| 0 | 219 (0.4) | ||||||
| P83.5 | Congenital hydrocele | 1 | 11 (0.1) | 0.771 (0.414,1.436) | 0.4123 | 0.782 (0.396,1.543) | 0.4779 |
| 0 | 105 (0.2) | ||||||
| P83.89 | Other conditions of integument | 1 | 20 (0.2) | 0.909 (0.571,1.447) | 0.6862 | 0.986 (0.594,1.637) | 0.9572 |
| 0 | 162 (0.3) | ||||||
| P90 | Seizure | 1 | 18 (0.2) | 0.974 (0.596,1.594) | 0.9179 | 1.059 (0.602,1.862) | 0.8422 |
| 0 | 136 (0.2) | ||||||
| P91.6 | Hypoxic ischemic encephalopathy | 1 | 12 (0.1) | 0.874 (0.480,1.592) | 0.6606 | 0.786 (0.390,1.585) | 0.5011 |
| 0 | 101 (0.2) | ||||||
| P92.0 | Vomiting | 1 | 36 (0.4) | 1.228 (0.862,1.749) | 0.2549 | 0.928 (0.612,1.406) | 0.7231 |
| 0 | 216 (0.4) | ||||||
| P92.123589 | Difficulty feeding | 1 | 369 (4.4) | 1.239 (1.107,1.386) | 0.0002 | 1.054 (0.924,1.203) | 0.4344 |
| 0 | 2212 (3.6) | ||||||
| P94.2 | Congenital hypotonia | 1 | 15 (0.2) | 0.898 (0.525,1.535) | 0.6929 | 0.788 (0.413,1.504) | 0.4703 |
| 0 | 123 (0.2) | ||||||
| P96.81 | Jittery baby | 1 | 32 (0.4) | 1.197 (0.823,1.740) | 0.3473 | 1.104 (0.705,1.728) | 0.6666 |
| 0 | 197 (0.3) | ||||||
| Congenital anomalies | |||||||
| Q38.1 | Ankyloglossia | 1 | 221 (2.7) | 1.545 (1.334,1.789) | <0.0001 | 1.241 (1.044,1.474) | 0.0143 |
| 0 | 1063 (1.7) | ||||||
| Q66 | Talipes equinovarus, metatarsus varus, or other congenital deformities of feet | 1 | 33 (0.4) | 0.880 (0.613,1.263) | 0.4873 | 0.963 (0.612,1.516) | 0.8707 |
| 0 | 276 (0.5) | ||||||
| Outcome † | Tdap | N | Mean (SD) | Unadjusted Mean Difference (95% CI) | p Value | Adjusted Mean Difference (95% CI) | p Value |
|---|---|---|---|---|---|---|---|
| Apgar score at 5 min after birth | Exposed | 7660 | 9.537 (0.879) | 0.005 (−0.015,0.026) | 0.6246 | 0.000 (−0.022,0.023) | 0.9775 |
| Unexposed | 53,810 | 9.531 (0.870) | |||||
| Birthweight (g) | Exposed | 8063 | 3467 (532) | 38.275 (24.640,51.911) | <0.0001 | 35.585 (21.392,49.778) | <0.0001 |
| Unexposed | 58,337 | 3429 (592) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Petousis-Harris, H.; Jiang, Y.; Yu, L.; Watson, D.; Walls, T.; Turner, N.; Howe, A.S.; Griffin, J.B. A Retrospective Cohort Study of Safety Outcomes in New Zealand Infants Exposed to Tdap Vaccine in Utero. Vaccines 2019, 7, 147. https://doi.org/10.3390/vaccines7040147
Petousis-Harris H, Jiang Y, Yu L, Watson D, Walls T, Turner N, Howe AS, Griffin JB. A Retrospective Cohort Study of Safety Outcomes in New Zealand Infants Exposed to Tdap Vaccine in Utero. Vaccines. 2019; 7(4):147. https://doi.org/10.3390/vaccines7040147
Chicago/Turabian StylePetousis-Harris, Helen, Yannan Jiang, Lennex Yu, Donna Watson, Tony Walls, Nikki Turner, Anna S. Howe, and Jennifer B. Griffin. 2019. "A Retrospective Cohort Study of Safety Outcomes in New Zealand Infants Exposed to Tdap Vaccine in Utero" Vaccines 7, no. 4: 147. https://doi.org/10.3390/vaccines7040147
APA StylePetousis-Harris, H., Jiang, Y., Yu, L., Watson, D., Walls, T., Turner, N., Howe, A. S., & Griffin, J. B. (2019). A Retrospective Cohort Study of Safety Outcomes in New Zealand Infants Exposed to Tdap Vaccine in Utero. Vaccines, 7(4), 147. https://doi.org/10.3390/vaccines7040147





