Intervention Strategies to Overcome HPV Vaccine Hesitancy Among Hispanic Immigrants in the USA: A Video-Based Approach
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Approval
2.2. Phase 1a: Focus Groups
2.3. Phase 1b: Video Creation
2.4. Phase 2: Assessing Effectiveness of Interventional Videos
2.5. Statistical Analysis
3. Results
3.1. Phase 1a: Focus Group Results
3.2. Phase 1b: Video Creation
3.3. Phase 2: Survey Results
3.3.1. Sociodemographic Characteristics
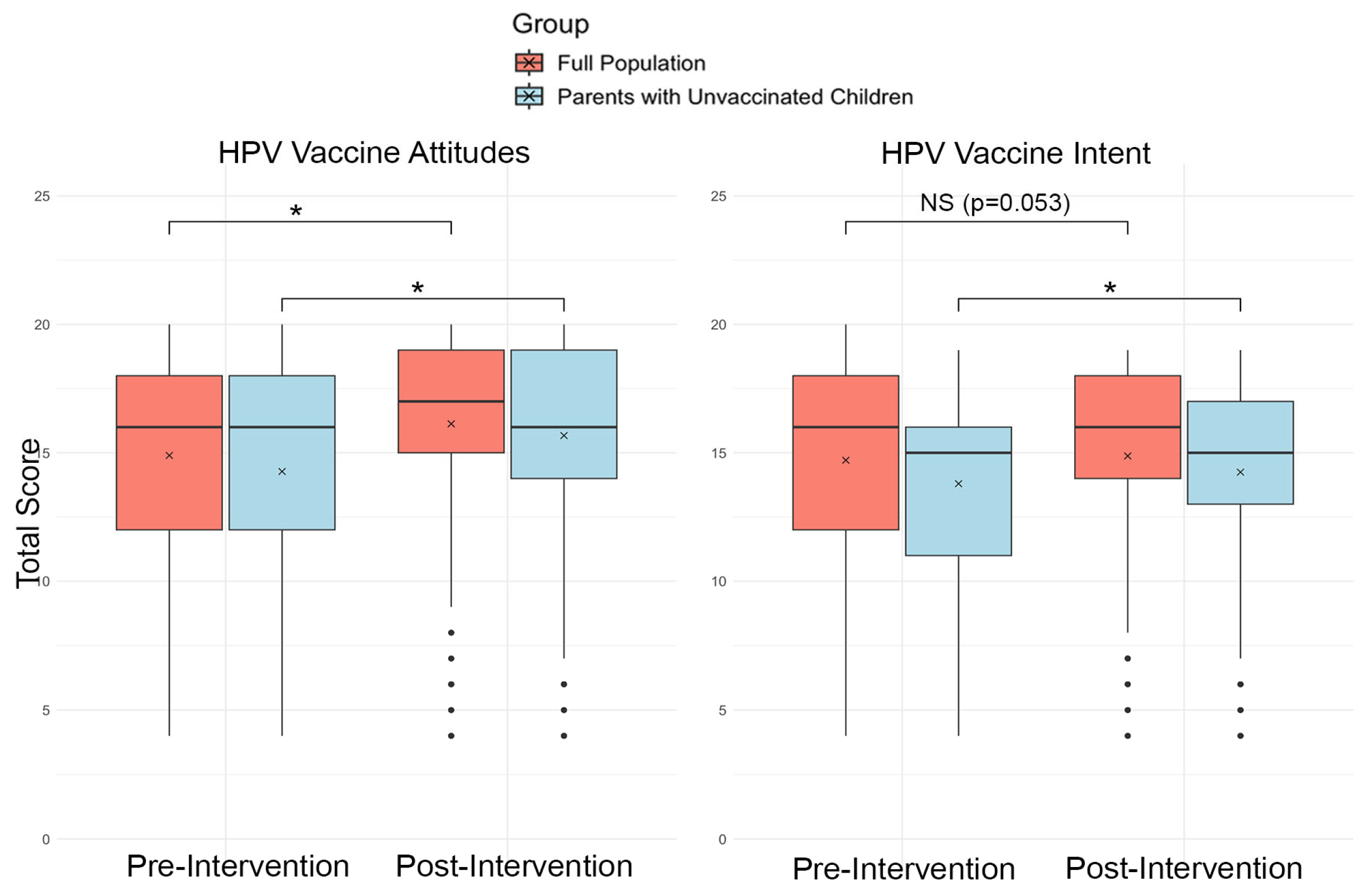
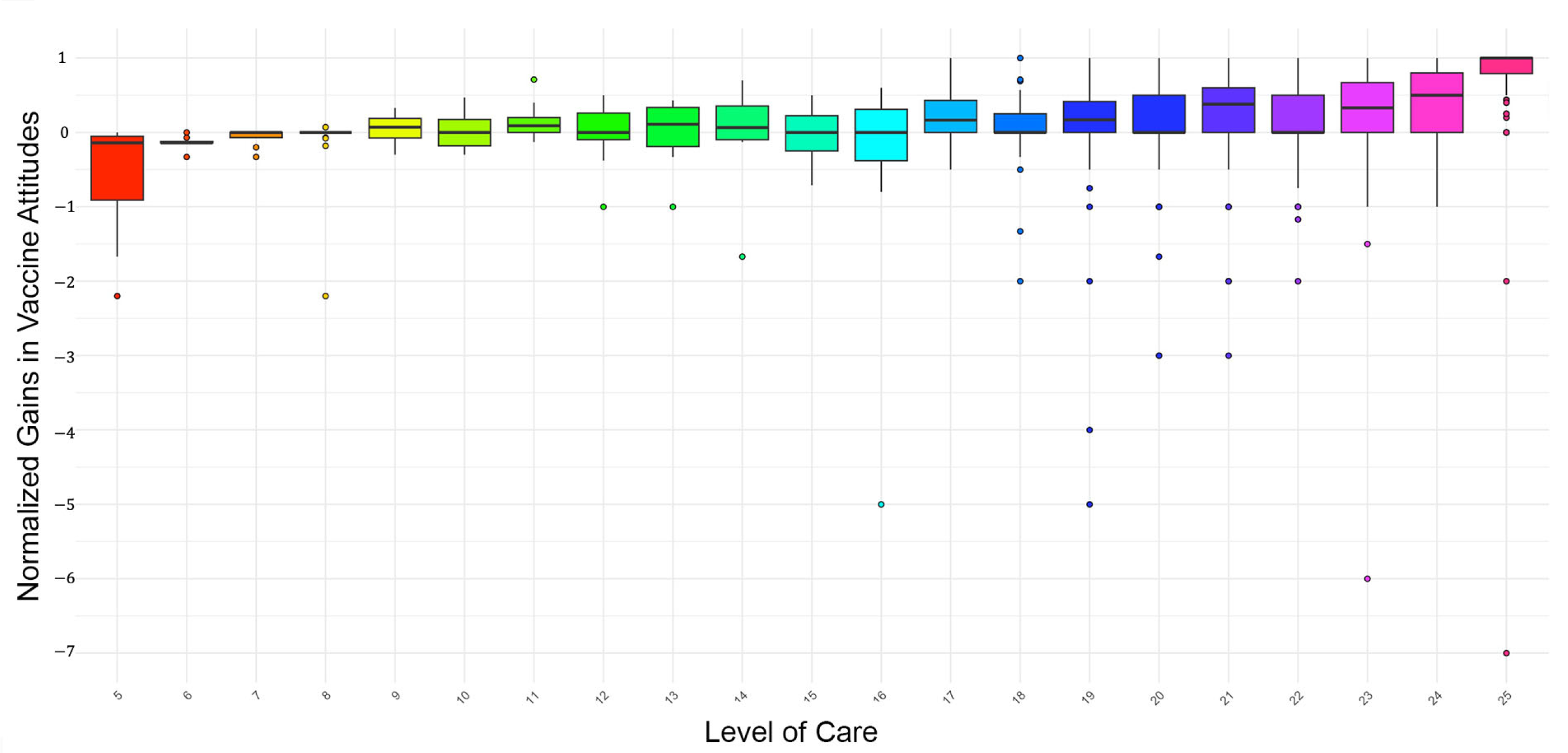
3.3.2. Attitudinal Data
4. Discussion
4.1. Community Engagement
4.2. Translating Community Feedback into Successful Educational Interventions
4.3. Limitations of Our Study
4.4. Implications for Health Communication
4.5. Implications for Public Health Policy, Insurance, and Government
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| HI | Hispanic Immigrant |
| HPV | Human Papilloma Virus |
| HBM | Health Belief Model |
| CDC | Centers for Disease Control and Prevention |
| CFA | Confirmatory Factor Analysis |
| TLI | Tucker–Lewis Index |
| CFI | Comparative Fit Index |
| RMSEA | Root Mean Square Error of Approximation |
| SRMSR | Standardized Root Mean Square Residual |
References
- Shattock, A.J.; Johnson, H.C.; Sim, S.Y.; Carter, A.; Lambach, P.; Hutubessy, R.C.W.; Thompson, K.M.; Badizadegan, K.; Lambert, B.; Ferrari, M.J.; et al. Contribution of vaccination to improved survival and health: Modelling 50 years of the Expanded Programme on Immunization. Lancet 2024, 403, 2307–2316. [Google Scholar] [CrossRef]
- Magno, H.; Golomb, B. Measuring the Benefits of Mass Vaccination Programs in the United States. Vaccines 2020, 8, 561. [Google Scholar] [CrossRef]
- Talbird, S.E.; Carrico, J.; La, E.M.; Carias, C.; Marshall, G.S.; Roberts, C.S.; Chen, Y.-T.; Nyaku, M.K. Impact of Routine Childhood Immunization in Reducing Vaccine-Preventable Diseases in the United States. Pediatrics 2022, 150, e2021056013. [Google Scholar] [CrossRef]
- MacDonald, N.E. SAGE Working Group on Vaccine Hesitancy Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Salmon, D.A.; Dudley, M.Z.; Glanz, J.M.; Omer, S.B. Vaccine hesitancy: Causes, consequences, and a call to action. Vaccine 2015, 33, D66–D71. [Google Scholar] [CrossRef]
- Fogel, B.; Schaefer, E.W.; Hicks, S.D. Early influenza vaccination rates decline in children during the COVID-19 pandemic. Vaccine 2021, 39, 4291–4295. [Google Scholar] [CrossRef]
- Redd, D.S.; Jensen, J.L.; Hughes, S.J.; Pogue, K.; Sloan-Aagard, C.D.; Miner, D.S.; Altman, J.D.; Crook, T.B.; Zentz, L.; Bodily, R.J.; et al. Effects of Religious Practice and Teachings about Sexual Behavior on Intent to Vaccinate against Human Papillomavirus. Vaccines 2022, 10, 397. [Google Scholar] [CrossRef]
- Arbyn, M.; Weiderpass, E.; Bruni, L.; de Sanjosé, S.; Saraiya, M.; Ferlay, J.; Bray, F. Estimates of incidence and mortality of cervical cancer in 2018: A worldwide analysis. Lancet Glob. Health 2020, 8, e191–e203. [Google Scholar] [CrossRef]
- Gargano, J.W. Trends in Cervical Precancers Identified Through Population-Based Surveillance—Human Papillomavirus Vaccine Impact Monitoring Project, Five Sites, United States, 2008–2022. MMWR Morb. Mortal. Wkly. Rep. 2025, 74, 96–101. [Google Scholar] [CrossRef]
- Jenco, M. HPV Vaccination Rate Stalls Again; 61% of Adolescents Up to Date. 22 August 2024. Available online: https://publications.aap.org/aapnews/news/29873/HPV-vaccination-rate-stalls-again-61-of (accessed on 15 May 2025).
- Berenson, A.B.; Laz, T.H.; Rahman, M. Reduction in Vaccine-Type Human Papillomavirus Prevalence Among Women in the United States, 2009–2012. J. Infect. Dis. 2016, 214, 1961–1964. [Google Scholar] [CrossRef]
- de Sanjose, S.; Brotons, M.; LaMontagne, D.S.; Bruni, L. Human papillomavirus vaccine disease impact beyond expectations. Curr. Opin. Virol. 2019, 39, 16–22. [Google Scholar] [CrossRef]
- Phillips, A.; Patel, C.; Pillsbury, A.; Brotherton, J.; Macartney, K. Safety of Human Papillomavirus Vaccines: An Updated Review. Drug Saf. 2018, 41, 329–346. [Google Scholar] [CrossRef]
- D’Souza, G.; Dempsey, A. The role of HPV in head and neck cancer and review of the HPV vaccine. Prev. Med. 2011, 53, S5–S11. [Google Scholar] [CrossRef]
- Lu, P.; Rodriguez-Lainz, A.; O’Halloran, A.; Greby, S.; Williams, W.W. Adult Vaccination Disparities Among Foreign-Born Populations in the U.S., 2012. Am. J. Prev. Med. 2014, 47, 722–733. [Google Scholar] [CrossRef]
- Hirth, J. Disparities in HPV vaccination rates and HPV prevalence in the United States: A review of the literature. Hum. Vaccines Immunother. 2019, 15, 146–155. [Google Scholar] [CrossRef]
- Sanchez, M.; Diez, S.; Fava, N.M.; Cyrus, E.; Ravelo, G.; Rojas, P.; Li, T.; Cano, M.A.; De La Rosa, M. Immigration Stress among Recent Latino Immigrants: The Protective Role of Social Support and Religious Social Capital. Soc. Work Public Health 2019, 34, 279–292. [Google Scholar] [CrossRef]
- Jeudin, P.; Liveright, E.; del Carmen, M.G.; Perkins, R.B. Race, Ethnicity, and Income Factors Impacting Human Papillomavirus Vaccination rates. Clin. Ther. 2014, 36, 24–37. [Google Scholar] [CrossRef]
- Mehta, N.; Raker, C.; Robison, K. Cervical Cancer Prevention: Screening Among Undocumented Hispanic Women Compared With Documented Hispanic Women. J. Low. Genit. Tract Dis. 2021, 25, 86. [Google Scholar] [CrossRef]
- Moreno, V.A.; Nogueira, D.L.; Delgado, D.; Valdez, M.J.; Lucero, D.; Hernandez Nieto, A.; Rodriguez-Cruz, N.; Lindsay, A.C. Misconceptions and knowledge gaps about HPV, cervical cancer, and HPV vaccination among Central American immigrant parents in the United States. Hum. Vaccines Immunother. 2025, 21, 2494452. [Google Scholar] [CrossRef]
- Hernandez, N.D.; Wilson, N.; Abah, T.; Contreras, O.; Franklin, C. Unveiling Cervical Cancer Inequities Among Georgia Immigrant Latinas: A Robust Qualitative Examination of the Facilitators and Barriers to Prevention, with Emphasis on the Impact of Community-Based Organizations. J. Cancer Educ. 2024. [Google Scholar] [CrossRef]
- Kim, K.; LeClaire, A.R. A systematic review of factors influencing human papillomavirus vaccination among immigrant parents in the United States. Health Care Women Int. 2017, 40, 696–718. Available online: https://www.tandfonline.com/doi/full/10.1080/07399332.2017.1404064#abstract (accessed on 15 May 2025). [CrossRef] [PubMed]
- Haviland, A.M.; Elliott, M.N.; Hambarsoomian, K.; Lurie, N. Immunization Disparities by Hispanic Ethnicity and Language Preference. Arch. Intern. Med. 2011, 171, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Larson, R.J.; Jensen, J.L.; Alvord, S.M.; Sloan-Aagard, C.; Skyles, T.; Davis, S.C.; Obray, A.M.; Pogue, K.; Poole, B.D. Effects of religious and cultural beliefs on vaccine attitudes in a Hispanic immigrant population in the United States. PLoS Glob. Public Health 2024, 4, e0003519. [Google Scholar] [CrossRef]
- Podolsky, R.; Cremer, M.; Atrio, J.; Hochman, T.; Arslan, A.A. HPV Vaccine Acceptability by Latino Parents: A Comparison of U.S. and Salvadoran Populations. J. Pediatr. Adolesc. Gynecol. 2009, 22, 205–215. [Google Scholar] [CrossRef] [PubMed]
- Nawas, G.T.; Zeidan, R.S.; Edwards, C.A.; El-Desoky, R.H. Barriers to COVID-19 Vaccines and Strategies to Improve Acceptability and Uptake. J. Pharm. Pract. 2023, 36, 900–904. [Google Scholar] [CrossRef]
- Lee, H.Y.; Luo, Y.; Neese, J.; Daniel, C.; Hahm, H.C. The Role of English Proficiency in HPV and HPV Vaccine Awareness: A Cross-Sectional Study Across Race/Ethnicity. Asian Pac. J. Cancer Prev. 2021, 22, 349–357. [Google Scholar] [CrossRef]
- Kohler, R.E.; Wagner, R.B.; Vega, J.; Rivera, Y.M.; Kantor, L.; Greene, K. HPV Vaccination Information Access, Needs, and Preferences Among Black and Hispanic Mothers. J. Health Commun. 2024, 29, 566–579. [Google Scholar] [CrossRef]
- Luque, J.; Raychowdhury, S.; Weaver, M. Health care provider challenges for reaching Hispanic immigrants with HPV vaccination in rural Georgia. Rural. Remote Health 2012, 12, 1975. [Google Scholar] [CrossRef]
- Mark, C.; Paul, N. Predicting Health Behaviour; McGraw-Hill Education: Maidenhead, UK, 2005; 403p. [Google Scholar]
- Rosenstock, I.M.; Strecher, V.J.; Becker, M.H. The Health Belief Model and HIV Risk Behavior Change. In Preventing AIDS; Springer: Boston, MA, USA, 1994; pp. 5–24. [Google Scholar]
- Sharma, M.; Romas, J.A. Theoretical Foundations of Health Education and Health Promotion; Jones & Bartlett Publishers: Burlington, MA, USA, 2010; 317p. [Google Scholar]
- Tarkang, E.E.; Zotor, F.B. Application of the Health Belief Model (HBM) in HIV Prevention: A Literature Review. Cent. Afr. J. Public Health 2015, 1, 1–8. [Google Scholar] [CrossRef]
- Yarbrough, S.S.; Braden, C.J. Utility of health belief model as a guide for explaining or predicting breast cancer screening behaviours. J. Adv. Nurs. 2001, 33, 677–688. [Google Scholar] [CrossRef]
- Zartaloudi, A. Health Belief Model (HBM) and vaccination during pandemics. Eur. Psychiatry 2022, 65, S308. [Google Scholar] [CrossRef]
- Donadiki, E.M.; Jiménez-García, R.; Hernández-Barrera, V.; Sourtzi, P.; Carrasco-Garrido, P.; López de Andrés, A.; Jimenez-Trujillo, I.; Velonakis, E.G. Health Belief Model applied to non-compliance with HPV vaccine among female university students. Public Health 2014, 128, 268–273. [Google Scholar] [CrossRef] [PubMed]
- Mehta, P.; Sharma, M.; Lee, R.C. Designing and Evaluating a Health Belief Model-Based Intervention to Increase Intent of HPV Vaccination among College Males. Int. Q. Community Health. Educ. 2014, 34, 101–117. [Google Scholar] [CrossRef]
- Grandahl, M.; Rosenblad, A.; Stenhammar, C.; Tydén, T.; Westerling, R.; Larsson, M.; Oscarsson, M.; Andrae, B.; Dalianis, T.; Nevéus, T. School-based intervention for the prevention of HPV among adolescents: A cluster randomised controlled study. BMJ Open 2016, 6, e009875. [Google Scholar] [CrossRef]
- Rodriguez, S.A.; Roncancio, A.M.; Savas, L.S.; Lopez, D.M.; Vernon, S.W.; Fernandez, M.E. Using Intervention Mapping to Develop and Adapt Two Educational Interventions for Parents to Increase HPV Vaccination Among Hispanic Adolescents. Front. Public Health 2018, 6, 164. [Google Scholar] [CrossRef]
- Larkey, L.K.; Hecht, M. A Model of Effects of Narrative as Culture-Centric Health Promotion. J. Health Commun. 2010, 15, 114–135. [Google Scholar] [CrossRef]
- Föcker, J.; Atkins, P.; Vantzos, F.-C.; Wilhelm, M.; Schenk, T.; Meyerhoff, H.S. Exploring the effectiveness of auditory, visual, and audio-visual sensory cues in a multiple object tracking environment. Atten. Percept. Psychophys. 2022, 84, 1611–1624. [Google Scholar] [CrossRef] [PubMed]
- Elo, S.; Kyngäs, H. The qualitative content analysis process. J. Adv. Nurs. 2008, 62, 107–115. [Google Scholar] [CrossRef]
- Pollard, M.S.; Davis, L.M. Decline in Trust in the Centers for Disease Control and Prevention During the COVID-19 Pandemic. Rand Health Q. 2022, 9, 23. [Google Scholar]
- Freed, G.L.; Clark, S.J.; Butchart, A.T.; Singer, D.C.; Davis, M.M. Parental Vaccine Safety Concerns in 2009. Pediatrics 2010, 125, 654–659. [Google Scholar] [CrossRef]
- CDC. Partnering for Vaccine Equity (P4VE) Program. Available online: https://www.cdc.gov/vaccine-equity/php/about/index.html (accessed on 15 May 2025).
- Johnson, D.K.; Mello, E.J.; Walker, T.D.; Hood, S.J.; Jensen, J.L.; Poole, B.D. Combating Vaccine Hesitancy with Vaccine-Preventable Disease Familiarization: An Interview and Curriculum Intervention for College Students. Vaccines 2019, 7, 39. [Google Scholar] [CrossRef] [PubMed]
- deRose, B.S. The Latino Immigrants’ Experience in Obtaining Required Childhood Vaccinations. J. Transcult. Nurs. 2018, 29, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Galletly, C.L.; Barreras, J.L.; Lechuga, J.; Glasman, L.R.; Cruz, G.; Dickson-Gomez, J.B.; Brooks, R.A.; Ruelas, D.M.; Stringfield, B.; Espinoza-Madrigal, I. US public charge policy and Latinx immigrants’ thoughts about health and healthcare utilization. Ethn. Health 2023, 28, 96–113. [Google Scholar] [CrossRef] [PubMed]
- Pedraza, F.I.; Nichols, V.C.; LeBrón, A.M.W. Cautious Citizenship: The Deterring Effect of Immigration Issue Salience on Health Care Use and Bureaucratic Interactions among Latino US Citizens. J. Health Polit. Policy Law 2017, 42, 925–960. [Google Scholar] [CrossRef]
- Ganev, K. New Content Formats in Digital Communications. Postmodernism Probl. 2023, 13, 332–340. [Google Scholar] [CrossRef]
- Massey, P.M.; Langellier, B.A.; Sentell, T.; Manganello, J. Nativity and language preference as drivers of health information seeking: Examining differences and trends from a U.S. population-based survey. Ethn. Health 2017, 22, 596–609. [Google Scholar] [CrossRef]
- Chu, J.N.; Sarkar, U.; Rivadeneira, N.A.; Hiatt, R.A.; Khoong, E.C. Impact of language preference and health literacy on health information-seeking experiences among a low-income, multilingual cohort. Patient Educ. Couns. 2022, 105, 1268–1275. [Google Scholar] [CrossRef]
- Smulian, E.A.; Mitchell, K.R.; Stokley, S. Interventions to increase HPV vaccination coverage: A systematic review. Hum. Vaccines Immunother. 2016, 12, 1566–1588. [Google Scholar] [CrossRef]
- Lott, B.E.; Okusanya, B.O.; Anderson, E.J.; Kram, N.A.; Rodriguez, M.; Thomson, C.A.; Rosales, C.; Ehiri, J.E. Interventions to increase uptake of Human Papillomavirus (HPV) vaccination in minority populations: A systematic review. Prev. Med. Rep. 2020, 19, 101163. [Google Scholar] [CrossRef]
- Brunson, E.K. How parents make decisions about their children’s vaccinations. Vaccine 2013, 31, 5466–5470. [Google Scholar] [CrossRef]
- Quadri, N.S.; Knowlton, G.; Vazquez Benitez, G.; Ehresmann, K.R.; LaFrance, A.B.; DeFor, T.A.; Smith, M.K.; Mann, E.M.; Alpern, J.D.; Stauffer, W.M. Evaluation of Preferred Language and Timing of COVID-19 Vaccine Uptake and Disease Outcomes. JAMA Netw. Open 2023, 6, e237877. [Google Scholar] [CrossRef]
- Applewhite, A.; Stancampiano, F.F.; Harris, D.M.; Manaois, A.; Dimuna, J.; Glenn, J.; Heckman, M.G.; Brushaber, D.E.; Sher, T.; Valery, J.R. A Retrospective Analysis of Gender-Based Difference in Adherence to Influenza Vaccination during the 2018–2019 Season. J. Prim. Care Community Health 2020, 11, 2150132720958532. [Google Scholar] [CrossRef] [PubMed]
- Adjei Boakye, E.; Tobo, B.B.; Rojek, R.P.; Mohammed, K.A.; Geneus, C.J.; Osazuwa-Peters, N. Approaching a decade since HPV vaccine licensure: Racial and gender disparities in knowledge and awareness of HPV and HPV vaccine. Hum. Vaccines Immunother. 2017, 13, 2713–2722. [Google Scholar] [CrossRef] [PubMed]
- Heimbecker, V.; Bordini, S.C.; Rodrigues, A.C.; de Alencar, N.M.; Blanco, N.S.; Fitz, F.; Moura, G.B.; Dumitru, M.; Mercadante, A.F.; Alvarenga, L.M.; et al. Gender Differences on the Awareness of Human Papillomavirus Infection and Vaccination. J. Cancer Educ. 2024, 39, 611–617. [Google Scholar] [CrossRef] [PubMed]
- Daniel-Ulloa, J.; Gilbert, P.A.; Parker, E.A. Human Papillomavirus Vaccination in the United States: Uneven Uptake by Gender, Race/Ethnicity, and Sexual Orientation. Am. J. Public Health 2016, 106, 746–747. [Google Scholar] [CrossRef]
- Rahman, M.; Islam, M.; Berenson, A.B. Differences in HPV Immunization Levels Among Young Adults in Various Regions of the United States. J. Community Health 2015, 40, 404–408. [Google Scholar] [CrossRef]
- Reimer, R.A.; Schommer, J.A.; Houlihan, A.E.; Gerrard, M. Ethnic and Gender Differences in HPV Knowledge, Awareness, and Vaccine Acceptability Among White and Hispanic Men and Women. J. Community Health 2014, 39, 274–284. [Google Scholar] [CrossRef]
- Yang, S.; Tao, R.; Bhattar, M.; Shen, L.; Jones, M.; Garbacz, A.; Passmore, S.R. Designing and testing social media campaign messages to promote COVID-19 vaccine confidence among rural adults: A community-engaged approach featuring rural community leader and clinician testimonials. Prev. Med. Rep. 2023, 36, 102508. [Google Scholar] [CrossRef]
- Cawkwell, P.B.; Oshinsky, D. Storytelling in the context of vaccine refusal: A strategy to improve communication and immunisation. Med. Humanit. 2016, 42, 31–35. [Google Scholar] [CrossRef]
- Jennings, F.J.; Leach, R.B.; Lawson, B.; Welch, E.; Gentry, A.; Buechner, S. Narrative or Facts: Two Paths to Vaccine Advocacy. J. Health Commun. 2024, 29, 644–653. [Google Scholar] [CrossRef]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Conner, M. Health Behaviors. In International Encyclopedia of the Social & Behavioral Sciences, 2nd ed.; Wright, J.D., Ed.; Elsevier: Oxford, UK, 2015; pp. 582–587. [Google Scholar]
- Green, M.C. Narratives and Cancer Communication. J. Commun. 2006, 56, S163–S183. [Google Scholar] [CrossRef]
- Baesler, E.J.; Burgoon, J.K. The Temporal Effects of Story and Statistical Evidence on Belief Change. Commun. Res. 1994, 21, 582–602. [Google Scholar] [CrossRef]
- Volkman, J.E. Narratives in Health and Risk Messaging. In Oxford Research Encyclopedia of Communication; Available online: https://oxfordre.com/communication/display/10.1093/acrefore/9780190228613.001.0001/acrefore-9780190228613-e-306 (accessed on 16 May 2025).
- Baumel, N.M.; Spatharakis, J.K.; Baumel, L.D.; Sellas, E.I. Disparity in Public Perception of Pfizer and Moderna COVID-19 Vaccines on TikTok. J. Adolesc. Health 2022, 70, 514. [Google Scholar] [CrossRef]
- Grimm, P. Social Desirability Bias. In Wiley International Encyclopedia of Marketing; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2010. [Google Scholar]
- Iwami, M.; Bouaddi, O.; Razai, M.S.; Mansour, R.; Morais, B.; Ali, N.M.; Crawshaw, A.F.; Bojang, S.; Seedat, F.; Deal, A.; et al. Defining drivers of human papillomavirus (HPV) vaccine uptake in migrant populations globally and strategies and interventions to improve coverage: A systematic review. medRxiv 2025. medRxiv:2025.01.31.25321303. [Google Scholar] [CrossRef]
- Lechuga, J.; Vera-Cala, L.; Martinez-Donate, A. HPV vaccine awareness, barriers, intentions, and uptake in Latina women. J. Immigr. Minor. Health 2016, 18, 173–178. [Google Scholar] [CrossRef]
- Sokale, I.; Montealegre, J.; Amuta, A.O.; Oluyomi, A.; Thrift, A.P. Racial and Ethnic Disparities in Human Papillomavirus Vaccination Among US-Born and Foreign-Born Adults Aged 18 to 26 Years in the United States. Vaccines 2025, 13, 98. [Google Scholar] [CrossRef]
| Section | Focus Group Questions |
|---|---|
| Vaccine Attitudes and Awareness | 1. What are your general feelings about vaccines? 2. Are you familiar with the HPV Vaccine? How likely are you to get your kids vaccinated? |
| Trust and Concerns in Vaccine Communication | 3. Who is the ideal person to communicate health information concerning vaccines? 4. What makes you more or less trusting of that individual? 5. Do you worry about providing documentation when you visit a healthcare provider? 6. Do you fear vaccines based on a lack of information? If so, what information is missing? |
| Specific Concerns and Influences on HPV Vaccination | 7. Are there any concerns you have specific to HPV vaccination that we have not covered above? 8. How much do your religious views impact your decisions about the HPV vaccine? 9. Besides going to a medical doctor, who do you go to for treatments? |
| Effective Communication Strategies for HPV Vaccine Education | 10. We are planning to produce educational materials (in the form of short videos) to help Spanish-speaking immigrants better understand the HPV vaccine. Based on what you have shared, we would like a little more feedback on what you think would be most effective for these videos. 11. Who should be the person speaking? 12. What kind of information would be helpful? 13. What format do you think is best (someone just relaying information to you vs. watching a conversation between a doctor and patient vs. a conversation between two parents)? 14. What makes you most comfortable listening to the information? |
| Emergent Theme | Example Quote |
|---|---|
| What Information is needed? | |
| Disease information | “And if there is a video on the complexity of the Papilloma issue, I think there are several factors that should be included, such as at least how it is acquired, who is directly affected, how to prevent it, what are the best, that is, the best resources to use for the vaccine”. (group 1) |
| Video Decision: | Included a video titled, “What is HPV?” that details the characteristics of the virus, how it is transmitted, and the consequences of infection. |
| Benefits/effectiveness of the vaccine | “Like for example…what percentage of effectiveness does it have [and] to know how much that vaccine affects them or how much that vaccine can help them or how much it can benefit them?” (group 2) |
| Video Decision: | Included a video titled, “How Do I Prevent HPV?” that explains how vaccines function to prevent disease, specifically highlighting the HPV vaccine. Additionally, we included a video titled, “Where did the Vaccine Come From?” that highlighted the long-term protection from and prevention of HPV-related cancers and consequences that the vaccine provides. |
| Side effects of the vaccine | “What are the effects? And after the vaccine? What is going to happen, tell us if the child is going to have a fever or something?” (group 1) |
| Video Decision: | Included a video titled, “Are there Side Effects of Getting Vaccinated?” that explains how safe the HPV vaccine is and what common side effects are seen. |
| Vaccine origin and manufacture | “How did it originate? How was it created? Who created it? Which laboratories?” (group 1) |
| Video Decision: | Included a video titled, “Where did the Vaccine Come From?” that highlighted both the approval process of the vaccine and safety statistics, as well as the long-term protection from and prevention of HPV-related cancers and consequences that the vaccine provides. |
| How and when to administer | “One question I have is what would be the right age to give the vaccine? Because we are talking about an age range that is possible, but as she explained to us it’s for a child of eight or nine years old. But we see that it is not necessary [for them] because they will not have the same concern we have about sexual relations. So what would be the right age to administer the vaccine?” (group 1) |
| Video Decision: | Included a video titled, “At What Age Should I Vaccinate My Children Against HPV?” that states the recommended age range and then explains why that age range is appropriate given the need to prevent infection prior to being sexually active. |
| Who should give the information? | |
| Medical Professionals/Research Scientists | “That you have the credentials to be able to prove what you’re saying…Because if they offer you a vaccine and they don’t know what it is, they haven’t studied it or they don’t know what it is, how are you going to trust that person? That’s what it’s like to have the basis, uh, to have studied. It doesn’t matter if it is a doctor or a nurse, but someone related to the field of the vaccine. Someone who knows how to clarify doubts”. (group 1) |
| Video Decision: | We chose to include an expert who is a university professor of microbiology to explain how HPV is transmitted. |
| Government/Center for Disease Control (CDC) | “As an example. This information comes from CDC”. (group 1) |
| Video Decision: | We chose to highlight the statement on the HPV vaccine directly from the Center for Disease Control and Prevention (CDC). We also highlighted the role of the US Food and Drug Administration (FDA) in the approval process of the vaccine. |
| Testimonials | “The experience of someone who’s been through it tells you about it, too. It helps, because you say hey, it’s real. It’s not nothing but a story. Like at the beginning of COVID when everybody started dying. Hey, let’s get vaccinated”. (group 1) |
| Video Decision: | We included a video, titled “Testimonials” highlighting three native Spanish-speaking women talking about their own experiences with the vaccine and their children. |
| Medical Professionals/Research Scientists | “That you have the credentials to be able to prove what you’re saying…Because if they offer you a vaccine and they don’t know what it is, they haven’t studied it or they don’t know what it is, how are you going to trust that person? That’s what it’s like to have the basis, uh, to have studied. It doesn’t matter if it is a doctor or a nurse, but someone related to the field of the vaccine. Someone who knows how to clarify doubts”. (group 1) |
| What format is appropriate? | |
| Engaging content | “Show pictures and make it didactic. How do you say, more fun? Fun is not just standing up and talking and giving a talk and that, because no, that’s not the idea. But doing, showing you the images, showing you the dialogues all of that kind of stuff, but talking to you directly”. (group 1) |
| Video Decision: | We chose to use a whiteboard animation application, “Video Scribe”, to create videos with animation, embedded videos of people, and both on-screen and voice-over text |
| Direct Communication | “Someone to talk to me directly, like this, to tell it all like it is. The information, the side effects”. (group 1) |
| Video Decision: | We used first-person format where all videos, and people in them, are talking directly to the viewer. |
| Short | “Imagine three min each with one for each point, it would be better”. Another speaker said, “Because I don’t have 20 min. Right, I don’t know about you guys, but we’re busy. We as dads don’t have time”. (both group 1) |
| Video Decision: | All videos (except “Testimonials”) were under 3 ½ min. The testimonial video was just under 8 min. |
| Engaging content | “Show pictures and make it didactic. How do you say, more fun? Fun is not just standing up and talking and giving a talk and that, because no, that’s not the idea. But doing, showing you the images, showing you the dialogues all of that kind of stuff, but talking to you directly”. (group 1) |
| Other: | |
| Language Barrier | “Sometimes we don’t take the interest, sometimes they put you a translator, but the translator doesn’t tell you things well as the doctor can tell you”. (group 2) |
| Video Decision: | All videos were filmed entirely in Spanish by native speakers or non-native speakers who have spent two years or more immersed in a Spanish-speaking environment. This includes all on-screen text, voice-over text, and person dialogue. |
| Means | Standard Deviations | t | p | |
|---|---|---|---|---|
| Pre-HPV vaccine intent | 14.73 | 3.89 | −1.94 | 0.053 |
| Post-HPV vaccine intent | 14.89 | 3.68 | ||
| Pre-HPV vaccine attitude | 14.90 | 4.18 | −13.61 | <0.001 |
| Post-HPV vaccine attitude | 16.13 | 4.05 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aduse-Poku, I.; Ardon, D.A.; Call, A.B.; Davis, S.C.; Evans, P.; Johanson, S.; Larson, R.J.; Rencher, J.; Woolley, I.A.; Poole, B.D.; et al. Intervention Strategies to Overcome HPV Vaccine Hesitancy Among Hispanic Immigrants in the USA: A Video-Based Approach. Vaccines 2025, 13, 574. https://doi.org/10.3390/vaccines13060574
Aduse-Poku I, Ardon DA, Call AB, Davis SC, Evans P, Johanson S, Larson RJ, Rencher J, Woolley IA, Poole BD, et al. Intervention Strategies to Overcome HPV Vaccine Hesitancy Among Hispanic Immigrants in the USA: A Video-Based Approach. Vaccines. 2025; 13(6):574. https://doi.org/10.3390/vaccines13060574
Chicago/Turabian StyleAduse-Poku, Isaiah, Diego A. Ardon, Alexis B. Call, Spencer C. Davis, Preston Evans, Spencer Johanson, Ruth J. Larson, James Rencher, Isaac A. Woolley, Brian D. Poole, and et al. 2025. "Intervention Strategies to Overcome HPV Vaccine Hesitancy Among Hispanic Immigrants in the USA: A Video-Based Approach" Vaccines 13, no. 6: 574. https://doi.org/10.3390/vaccines13060574
APA StyleAduse-Poku, I., Ardon, D. A., Call, A. B., Davis, S. C., Evans, P., Johanson, S., Larson, R. J., Rencher, J., Woolley, I. A., Poole, B. D., & Jensen, J. L. (2025). Intervention Strategies to Overcome HPV Vaccine Hesitancy Among Hispanic Immigrants in the USA: A Video-Based Approach. Vaccines, 13(6), 574. https://doi.org/10.3390/vaccines13060574







