Childhood Influenza Vaccination Is Not a Priority for Parents: A National, Cross-Sectional Survey of Barriers to Childhood Influenza Vaccination in Australia
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Setting
2.3. Participants
2.4. Variables
2.5. Data Sources and Measurement
2.6. Bias
2.7. Study Size
2.8. Quantitative Variables
2.9. Statistical Analysis
2.10. Ethical Considerations
3. Results
3.1. Participant Characteristics
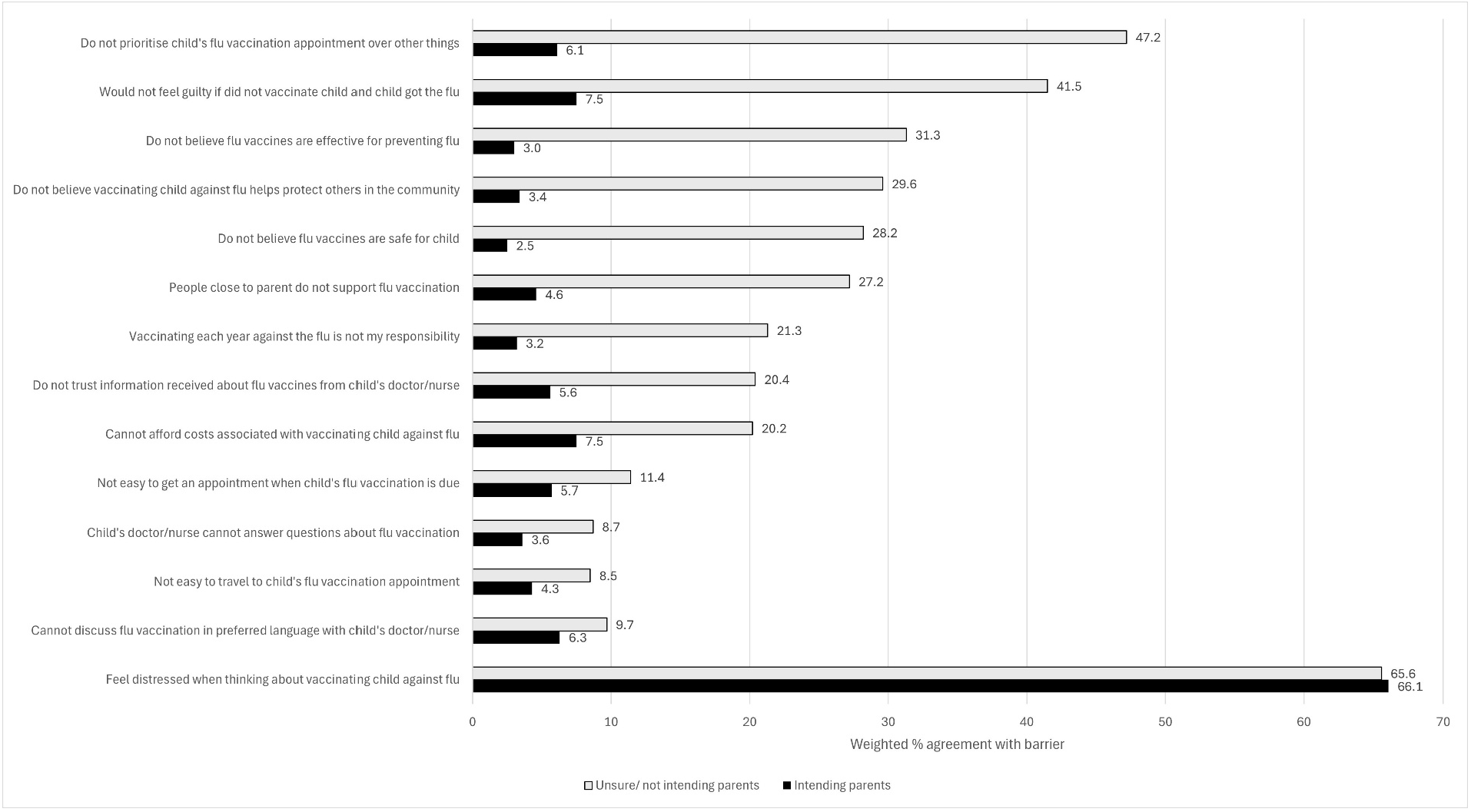
3.2. Prevalence of Influenza Vaccination Barriers
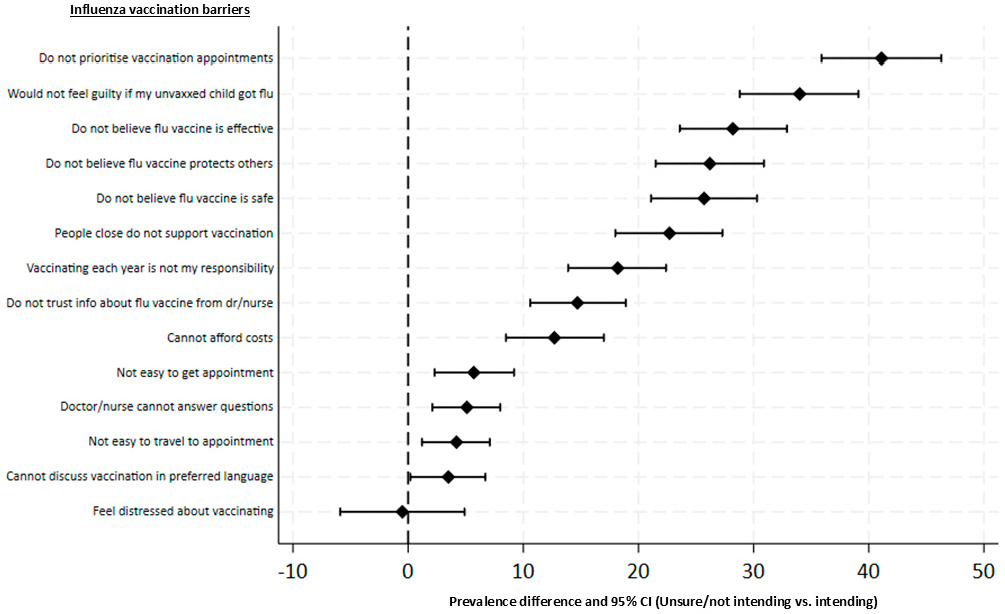
3.3. Comparing Influenza Vaccination Barriers by Parent’s Intention to Vaccinate
3.4. Comparing Influenza Vaccination Barriers by Key Demographic Variables
4. Discussion
4.1. Strengths and Limitations
4.2. Implications
4.3. Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Australian Technical Advisory Group on Immunisation (ATAGI). The Australian Immunisation Handbook; Australian Government Department of Health and Aged Care, 2022. Available online: https://immunisationhandbook.health.gov.au/ (accessed on 2 April 2025).
- NSW Ministry of Health. NSW Immunisation Strategy 2024–2028; 2024. Available online: https://www.health.nsw.gov.au/immunisation/Publications/strategy.pdf (accessed on 2 April 2025).
- National Centre for Immunisation Research and Surveillance (NCIRS). Influenza Vaccination Coverage Data (for the 2024 Influenza Season). NCIRS. Available online: https://ncirs.org.au/influenza-vaccination-coverage-data (accessed on 7 January 2025).
- Hull, B.; Hendry, A.; Dey, A.; McIntyre, P.; Macartney, K.; Beard, F. Annual Immunisation Coverage Report 2018. 2019. Available online: https://ncirs.org.au/sites/default/files/2019-11/NCIRS%20Annual%20Immunisation%20Coverage%20Report%202018_0.pdf (accessed on 2 April 2025).
- Hull, B.; Hendry, A.; Dey, A.; Macartney, K.; Beard, F. Annual Immunisation Coverage Report 2019. 2020. Available online: https://ncirs.org.au/sites/default/files/2020-11/NCIRS%20Annual%20Immunisation%20Coverage%20Report%202019%20Final.pdf (accessed on 2 April 2025).
- Walters, M.; Rhodes, A.; Hoq, M.; Measey, M.A. Caregiver’s intention and uptake of influenza vaccination for children in Australia before and after introduction of free vaccination. Public Health 2024, 237, 94–96. [Google Scholar] [CrossRef] [PubMed]
- Hull, B.; Hendry, A.; Dey, A.; Brotherton, J.; Macartney, K.; Beard, F. Annual Immunisation Coverage Report 2020. 2021. Available online: https://www.ncirs.org.au/sites/default/files/2022-07/NCIRS%20Annual%20Immunisation%20Coverage%20Report%202020.pdf (accessed on 2 April 2025).
- Centers for Disease Control (US Department of Health and Human Services). Influenza Vaccination Coverage, Children 6 Months Through 17 Years, United States. Available online: https://www.cdc.gov/fluvaxview/dashboard/children-vaccination-coverage.html (accessed on 2 April 2025).
- Irving, S.A.; Groom, H.C.; Belongia, E.A.; Crane, B.; Daley, M.F.; Goddard, K.; Jackson, L.A.; Kauffman, T.L.; Kenigsberg, T.A.; Kuckler, L.; et al. Influenza vaccination coverage among persons ages six months and older in the Vaccine Safety Datalink in the 2017–18 through 2022–23 influenza seasons. Vaccine 2023, 41, 7138–7146. [Google Scholar] [CrossRef]
- UK Department of Health and Social Care. Fingertips—Public Health Profiles. Available online: https://fingertips.phe.org.uk/search/flu%20vaccination (accessed on 2 April 2025).
- National Centre for Immunisation Research and Surveillance (NCIRS). Influenza Vaccines—Frequently Asked Questions. Available online: https://ncirs.org.au/influenza/influenza-vaccines-frequently-asked-questions-faqs (accessed on 2 April 2025).
- Patel, C.; Dey, A.; Wang, H.; McIntyre, P.; Macartney, K.; Beard, F. Summary of National Surveillance Data on Vaccine Preventable Diseases in Australia, 2016-2018 Final Report. Commun. Dis. Intell. 2022, 46, 1–112. [Google Scholar] [CrossRef]
- Norman, D.A.; Cheng, A.C.; Macartney, K.K.; Moore, H.C.; Danchin, M.; Seale, H.; McRae, J.; Clark, J.E.; Marshall, H.S.; Buttery, J.; et al. Influenza hospitalizations in Australian children 2010–2019: The impact of medical comorbidities on outcomes, vaccine coverage, and effectiveness. Influenza Other Respir. Viruses 2022, 16, 316–327. [Google Scholar] [CrossRef]
- Li-Kim-Moy, J.; Yin, J.K.; Blyth, C.C.; Kesson, A.; Booy, R.; Cheng, A.C.; Macartney, K. Influenza hospitalizations in Australian children. Epidemiol. Infect. 2017, 145, 1451–1460. [Google Scholar] [CrossRef]
- Teutsch, S.M.; Zurynski, Y.A.; Nunez, C.; Lester-Smith, D.; Festa, M.; Booy, R.; Elliott, E.J. Ten Years of National Seasonal Surveillance for Severe Complications of Influenza in Australian Children. Pediatr. Infect. Dis. J. 2021, 40, 191–198. [Google Scholar] [CrossRef]
- Blyth, C.C.; Jacoby, P.; Effler, P.V.; Kelly, H.; Smith, D.W.; Robins, C.; Willis, G.A.; Levy, A.; Keil, A.D.; Richmond, P.C. Effectiveness of trivalent flu vaccine in healthy young children. Pediatrics 2014, 133, e1218–e1225. [Google Scholar] [CrossRef]
- Boddington, N.L.; Pearson, I.; Whitaker, H.; Mangtani, P.; Pebody, R.G. Effectiveness of Influenza Vaccination in Preventing Hospitalization Due to Influenza in Children: A Systematic Review and Meta-analysis. Clin. Infect. Dis. 2021, 73, 1722–1732. [Google Scholar] [CrossRef]
- Zeno, E.E.; Nogareda, F.; Regan, A.; Couto, P.; Rondy, M.; Jara, J.; Voto, C.; Mena, M.P.R.; Katz, N.; del Valle Juarez, M.; et al. Interim Effectiveness Estimates of 2024 Southern Hemisphere Influenza Vaccines in Preventing Influenza-Associated Hospitalization—REVELAC-i Network, Five South American Countries, March–July 2024. MMWR Morb. Mortal. Wkly. Rep. 2024, 73, 861–868. [Google Scholar] [CrossRef]
- Eichner, M.; Schwehm, M.; Eichner, L.; Gerlier, L. Direct and indirect effects of influenza vaccination. BMC Infect. Dis. 2017, 17, 308. [Google Scholar] [CrossRef]
- Kaufman, J.; Tuckerman, J.; Bonner, C.; Durrheim, D.N.; Costa, D.; Trevena, L.; Thomas, S.; Danchin, M. Parent-level barriers to uptake of childhood vaccination: A global overview of systematic reviews. BMJ Glob. Health 2021, 6, e006860. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Understanding the behavioural and social drivers of vaccine uptake. WHO position paper—May 2022. Wkly. Epidemiol. Rec. 2022, 97, 209–224. [Google Scholar]
- Carlson, S.J.; Scanlan, C.; Marshall, H.S.; Blyth, C.C.; Macartney, K.; Leask, J. Attitudes about and access to influenza vaccination experienced by parents of children hospitalised for influenza in Australia. Vaccine 2019, 37, 5994–6001. [Google Scholar] [CrossRef]
- Biezen, R.; Grando, D.; Mazza, D.; Brijnath, B. Why do we not want to recommend influenza vaccination to young children? A qualitative study of Australian parents and primary care providers. Vaccine 2018, 36, 859–865. [Google Scholar] [CrossRef]
- Ruiz, H.; Halcomb, E.; Seale, H.; Horgan, A.; Rhee, J. Knowledge, beliefs and attitudes of general practitioners and general practice nurses regarding influenza vaccination for young children. Aust. J. Prim. Health 2021, 27, 276–283. [Google Scholar] [CrossRef]
- Tuckerman, J.; Crawford, N.W.; Marshall, H.S. Disparities in parental awareness of children’s seasonal influenza vaccination recommendations and influencers of vaccination. PLoS ONE 2020, 15, e0230425. [Google Scholar] [CrossRef]
- Kaufman, J.; Tuckerman, J.; Bonner, C.; Durrheim, D.N.; Costa, D.S.J.; Trevena, L.; Henseler, J.; Danchin, M. Development and validation of the Vaccine Barriers Assessment Tool for identifying drivers of under-vaccination in children under five years in Australia. Hum. Vaccines Immunother. 2024, 20, 2359623. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Smith, L.E.; Amlot, R.; Weinman, J.; Yiend, J.; Rubin, G.J. A systematic review of factors affecting vaccine uptake in young children. Vaccine 2017, 35, 6059–6069. [Google Scholar] [CrossRef]
- Rodriguez, V.J.; Kozlova, S.; LaBarrie, D.L.; Liu, Q. Parental anxiety and pediatric vaccine refusal in a US national sample of parents. Vaccine 2023, 41, 7072–7075. [Google Scholar] [CrossRef]
- Xu, Y.; Zhang, R.; Zhou, Z.; Fan, J.; Liang, J.; Cai, L.; Peng, L.; Ren, F.; Lin, W. Parental psychological distress and attitudes towards COVID-19 vaccination: A cross-sectional survey in Shenzhen, China. J. Affect. Disord. 2021, 292, 552–558. [Google Scholar] [CrossRef] [PubMed]
- Sampson, R.; Wong, L.; Macvicar, R. Parental reasons for non-uptake of influenza vaccination in young at-risk groups: A qualitative study. Br. J. Gen. Pract. 2011, 61, e386–e391. [Google Scholar] [CrossRef]
- Kempe, A.; Saville, A.W.; Albertin, C.; Zimet, G.; Breck, A.; Helmkamp, L.; Vangala, S.; Dickinson, L.M.; Rand, C.; Humiston, S.; et al. Parental Hesitancy About Routine Childhood and Influenza Vaccinations: A National Survey. Pediatrics 2020, 146, e20193852. [Google Scholar] [CrossRef]
- Offutt-Powell, T.N.; Ojha, R.P.; Qualls-Hampton, R.; Stonecipher, S.; Singh, K.P.; Cardarelli, K.M. Parental risk perception and influenza vaccination of children in daycare centres. Epidemiol. Infect. 2014, 142, 134–141. [Google Scholar] [CrossRef] [PubMed]
- Han, K.; Hou, Z.; Tu, S.; Liu, M.; Chantler, T.; Larson, H. Factors Influencing Childhood Influenza Vaccination: A Systematic Review. Vaccines 2024, 12, 233. [Google Scholar] [CrossRef]
- Frawley, J.E.; McManus, K.; McIntyre, E.; Seale, H.; Sullivan, E. Uptake of funded influenza vaccines in young Australian children in 2018; parental characteristics, information seeking and attitudes. Vaccine 2020, 38, 180–186. [Google Scholar] [CrossRef]
- Armstrong, P.K.; Dowse, G.K.; Effler, P.V.; Carcione, D.; Blyth, C.C.; Richmond, P.C.; Geelhoed, G.C.; Mascaro, F.; Scully, M.; Weeramanthri, T.S. Epidemiological study of severe febrile reactions in young children in Western Australia caused by a 2010 trivalent inactivated influenza vaccine. BMJ Open 2011, 1, e000016. [Google Scholar] [CrossRef]
- Blyth, C.C.; Richmond, P.C.; Jacoby, P.; Thornton, P.; Regan, A.; Robins, C.; Kelly, H.; Smith, D.W.; Effler, P.V. The impact of pandemic A(H1N1)pdm09 influenza and vaccine-associated adverse events on parental attitudes and influenza vaccine uptake in young children. Vaccine 2014, 32, 4075–4081. [Google Scholar] [CrossRef]
- Larson, H.J.; Clarke, R.M.; Jarrett, C.; Eckersberger, E.; Levine, Z.; Schulz, W.S.; Paterson, P. Measuring trust in vaccination: A systematic review. Hum. Vaccines Immunother. 2018, 14, 1599–1609. [Google Scholar] [CrossRef]
- Glanz, J.M.; Wagner, N.M.; Narwaney, K.J.; Shoup, J.A.; McClure, D.L.; McCormick, E.V.; Daley, M.F. A mixed methods study of parental vaccine decision making and parent-provider trust. Acad. Pediatr. 2013, 13, 481–488. [Google Scholar] [CrossRef]
- Smith, S.E.; Sivertsen, N.; Lines, L.; De Bellis, A. Decision making in vaccine hesitant parents and pregnant women—An integrative review. Int. J. Nurs. Stud. Adv. 2022, 4, 100062. [Google Scholar] [CrossRef]
- Goldenberg, M. Vaccine Hesitancy: Public Trust, Expertise, and the War on Science; University of Pittsburgh Press: Pittsburgh, PA, USA, 2021.
- Cologna, V.; Mede, N.G.; Berger, S.; Besley, J.; Brick, C.; Joubert, M.; Maibach, E.W.; Mihelj, S.; Oreskes, N.; Schäfer, M.S.; et al. Trust in scientists and their role in society across 68 countries. Nat. Hum. Behav. 2025, 9, 713–730. [Google Scholar] [CrossRef]
| Unweighted | Weighted | ABS Data on Australian Parents of Children <5 | ||
|---|---|---|---|---|
| n | (%) | (%) | % | |
| N | 2000 | - | - | - |
| Gender | ||||
| Woman | 1091 | (54.5%) | (52.3%) | 53.8% |
| Man | 901 | (45.1%) | (47.4%) | 46.3% |
| Non-binary | 3 | (0.1%) | (0.1%) | no data |
| Prefer not to say | 5 | (0.2%) | (0.2%) | - |
| Age (years) | ||||
| 18 to 24 | 32 | (1.6%) | (1.3%) | 3.4% |
| 25 to 29 | 153 | (7.6%) | (6.8%) | 12.9% |
| 30 to 34 | 742 | (37.1%) | (38.1%) | 29.9% |
| 35 to 39 | 743 | (37.1%) | (37.6%) | 32.4% |
| 40 to 44 | 291 | (14.5%) | (14.3%) | 15.1% |
| 45 to 49 | 29 | (1.5%) | (1.4%) | 4.1% |
| 50 to 54 | 7 | (0.4%) | (0.3%) | 1.2% |
| 55 to 59 | 3 | (0.1%) | (0.1%) | 0.5% |
| State or territory | ||||
| New South Wales | 612 | (30.6%) | (32.8%) | 32.0% |
| Victoria | 517 | (25.9%) | (27.3%) | 26.6% |
| Queensland | 404 | (20.2%) | (19.7%) | 19.3% |
| Western Australia | 217 | (10.8%) | (11.0%) | 10.8% |
| South Australia | 154 | (7.7%) | (6.6%) | 6.45% |
| Tasmania | 47 | (2.4%) | (0.4%) | 1.9% |
| Australian Capital Territory | 36 | (1.8%) | (2.0%) | 1.9% |
| Northern Territory | 13 | (0.7%) | (0.3%) | 1.0% |
| Regionality | ||||
| Metropolitan | 1458 | (72.9%) | (92.4%) | |
| Regional | 348 | (17.4%) | (4.8%) | |
| Rural | 159 | (8.0%) | (2.3%) | |
| Remote | 35 | (1.8%) | (0.5%) | |
| Aboriginal and Torres Strait Islander status | ||||
| Aboriginal | 57 | (2.9%) | (2.3%) | |
| Torres Strait Islander | 11 | (0.5%) | (0.4%) | |
| Both | 23 | (1.1%) | (0.8%) | |
| Neither | 1909 | (95.5%) | (96.5%) | |
| Education | ||||
| Less than high school | 13 | (0.7%) | (0.6%) | |
| High school or equivalent | 324 | (16.2%) | (14.3%) | |
| Trade cert/apprenticeship | 442 | (22.1%) | (20.6%) | |
| Bachelor’s degree | 879 | (44.0%) | (46.3%) | |
| Graduate degree | 342 | (17.1%) | (18.2%) | |
| Language used at home | ||||
| English only | 1739 | (87.0%) | (84.8%) | |
| Other language | 261 | (13.1%) | (15.2%) | |
| Number of children | ||||
| 1 | 1010 | (50.5%) | (53.3%) | |
| 2 | 697 | (34.8%) | (34.0%) | |
| 3+ | 293 | (14.6%) | (12.8%) | |
| Single parent or carer | ||||
| Yes | 1072 | (53.6%) | (55.8%) | |
| No | 928 | (46.4%) | (44.2%) | |
| Financial stress | ||||
| Yes | 726 | (36.3%) | (34.4%) | |
| No | 1274 | (63.7%) | (65.6%) | |
| Youngest child’s age | ||||
| <1 year | 192 | (9.6%) | (9.1%) | |
| 1 to <2 years | 359 | (17.9%) | (17.1%) | |
| 2 to <3 years | 507 | (25.4%) | (25.3%) | |
| 3 to <4 years | 519 | (25.9%) | (25.9%) | |
| 4 to <5 years | 423 | (21.1%) | (22.6%) | |
| Influenza Vaccination Barrier | PD | 95% CI Lower | Upper |
|---|---|---|---|
| Do not prioritise child’s flu vaccination appointment over other things | 41.1% | 35.9% | 46.3% |
| Would not feel guilty if they did not vaccinate child and child got the flu | 34.0% | 28.8% | 39.1% |
| Do not believe flu vaccines are effective for preventing flu | 28.2% | 23.6% | 32.9% |
| Do not believe vaccinating child against flu helps protect others in the community | 26.2% | 21.5% | 30.9% |
| Do not believe flu vaccines are safe for child | 25.7% | 21.1% | 30.3% |
| People close to parent do not support flu vaccination | 22.7% | 18.0% | 27.3% |
| Vaccinating each year against the flu is not parent’s responsibility | 18.2% | 13.9% | 22.4% |
| Do not trust information received about flu vaccines from child’s doctor/nurse | 14.7% | 10.6% | 18.9% |
| Cannot afford costs associated with vaccinating child against flu | 12.7% | 8.5% | 17.0% |
| Not easy to get an appointment when child’s flu vaccination is due | 5.7% | 2.3% | 9.2% |
| Child’s doctor/nurse cannot answer questions about flu vaccination | 5.1% | 2.1% | 8.0% |
| Not easy to travel to child’s flu vaccination appointment | 4.2% | 1.2% | 7.1% |
| Cannot discuss flu vaccination in preferred language with child’s doctor/nurse | 3.5% | 0.2% | 6.7% |
| Feel distressed when thinking about vaccinating child against flu | −0.5% | −5.9% | 4.9% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Steffens, M.S.; Kaufman, J.; Bolsewicz, K.T.; Vidmar, S.; Christou-Ergos, M.; Sabahelzain, M.M.; Leask, J.; Boxall, J.; Beard, F.; Danchin, M. Childhood Influenza Vaccination Is Not a Priority for Parents: A National, Cross-Sectional Survey of Barriers to Childhood Influenza Vaccination in Australia. Vaccines 2025, 13, 540. https://doi.org/10.3390/vaccines13050540
Steffens MS, Kaufman J, Bolsewicz KT, Vidmar S, Christou-Ergos M, Sabahelzain MM, Leask J, Boxall J, Beard F, Danchin M. Childhood Influenza Vaccination Is Not a Priority for Parents: A National, Cross-Sectional Survey of Barriers to Childhood Influenza Vaccination in Australia. Vaccines. 2025; 13(5):540. https://doi.org/10.3390/vaccines13050540
Chicago/Turabian StyleSteffens, Maryke S., Jessica Kaufman, Katarzyna T. Bolsewicz, Suzanna Vidmar, Maria Christou-Ergos, Majdi M. Sabahelzain, Julie Leask, Justin Boxall, Frank Beard, and Margie Danchin. 2025. "Childhood Influenza Vaccination Is Not a Priority for Parents: A National, Cross-Sectional Survey of Barriers to Childhood Influenza Vaccination in Australia" Vaccines 13, no. 5: 540. https://doi.org/10.3390/vaccines13050540
APA StyleSteffens, M. S., Kaufman, J., Bolsewicz, K. T., Vidmar, S., Christou-Ergos, M., Sabahelzain, M. M., Leask, J., Boxall, J., Beard, F., & Danchin, M. (2025). Childhood Influenza Vaccination Is Not a Priority for Parents: A National, Cross-Sectional Survey of Barriers to Childhood Influenza Vaccination in Australia. Vaccines, 13(5), 540. https://doi.org/10.3390/vaccines13050540





