Immunization Coverage, Equity, and Access for Children with Disabilities: A Scoping Review of Challenges, Strategies, and Lessons Learned to Reduce the Number of Zero-Dose Children
Abstract
1. Introduction
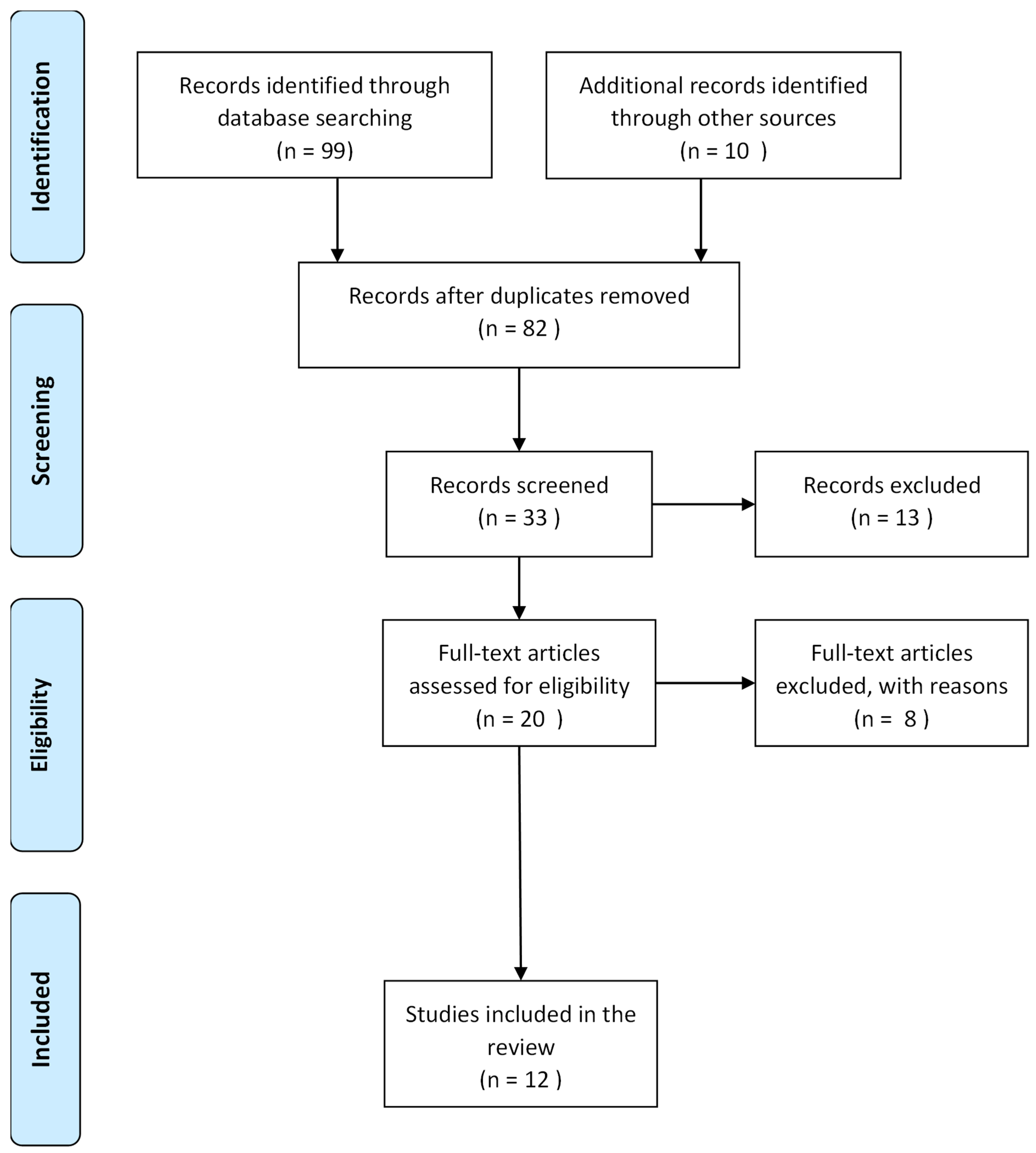
2. Methods
2.1. Study Design
2.2. Research Question and Study Eligibility
2.3. Literature Sources
2.4. Inclusion Criteria
2.4.1. Operational Criteria
2.4.2. Handling Varied Definitions During Screening
2.4.3. Rationale
2.5. Search Strategy
2.6. Title, Abstract, and Full-Text Screening
2.7. Data Abstraction and Analysis
2.8. Justification of Exclusion Criteria
3. Results
3.1. Characteristics of Included Studies
3.2. Barriers and Systemic Factors That Contribute to Inequities in Immunization Coverage for Children with Disabilities
- A.
- Barriers related to healthcare systems and social factors
- B.
- The influence of education, stigma, and misconceptions
3.3. Strategies That Have Been Identified or Implemented to Ensure Children with Disabilities Are Reached by Immunization Programs, and How These Can Be Scaled or Improved
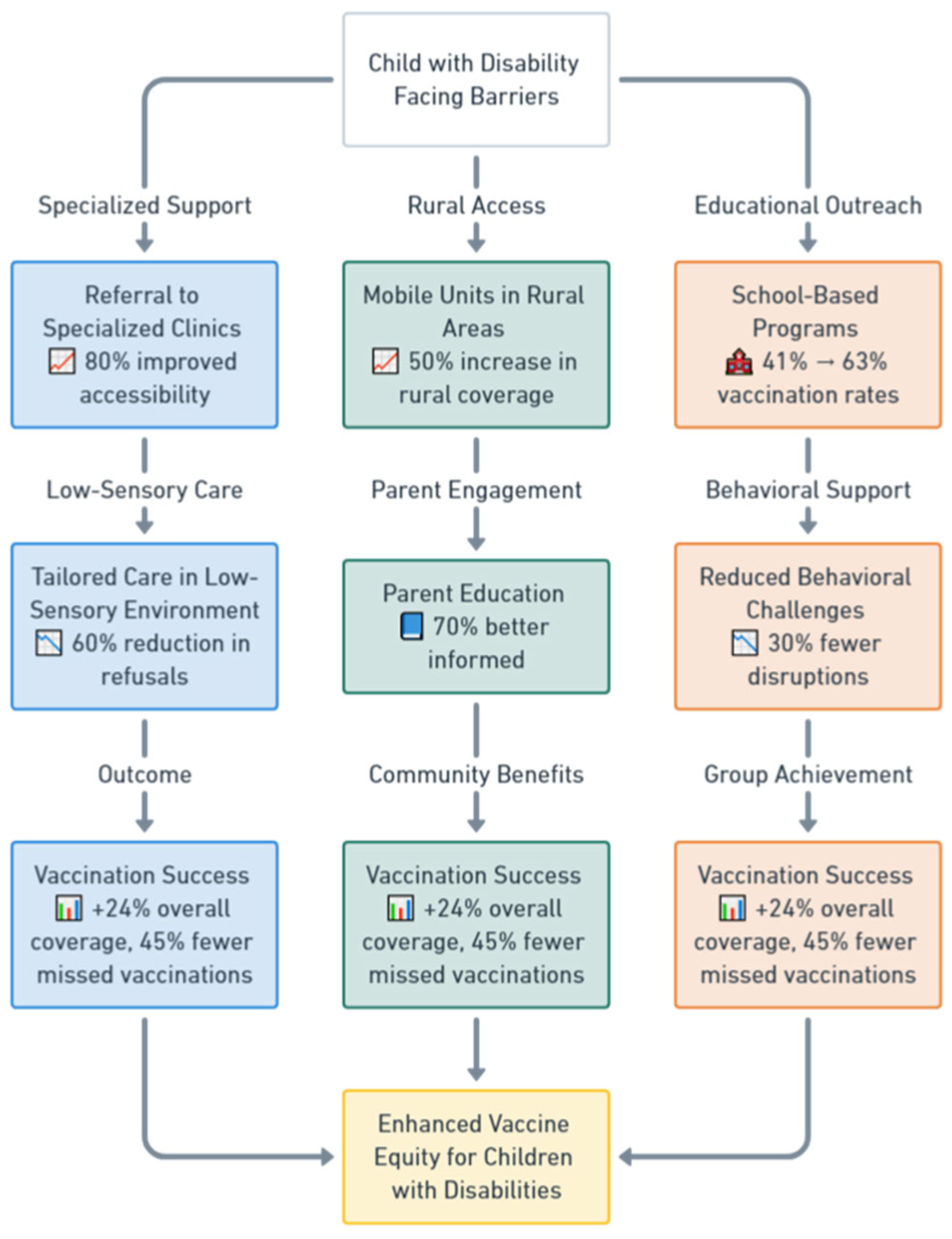
- A.
- Enhancing healthcare accessibility and service delivery
- B.
- Implementing tailored interventions for children with disabilities
- C.
- Addressing societal factors like stigma and education
3.4. Lessons Learned in Ensuring Equitable Access for Children with Disabilities
- A.
- Creating supportive and inclusive environments
- B.
- Empowering families and children
- C.
- Tailoring immunization services to individual needs
4. Discussion
4.1. Intersecting Stigma, Socioeconomic Disparities, and Disability
4.2. Practical Implementation, Scaling, and Evaluation of Identified Strategies
4.2.1. Tailored Interventions
4.2.2. Mobile Vaccination Units
4.2.3. Community Engagement
4.2.4. School-Based Vaccination Programs
4.2.5. Adapting High-Income Country Strategies for Low- and Middle-Income Countries
4.2.6. Monitoring and Evaluation (M&E)
4.2.7. Funding and Policy Advocacy
4.3. Limitations of the Study
- A.
- Addressing data gaps
- B.
- Methodological limitations and potential biases
- C.
- Broader methodological discussion
- D.
- Inconsistencies in definitions
4.4. Future Research Directions
- A.
- Longitudinal and Rigorous Study Designs
- B.
- Understudied Disability Types
- C.
- Participatory and Community-Engaged Methods
- D.
- Standardization of Definitions and Outcome Measures
5. Conclusions
Call to Action for Inclusive Immunization
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Feikin, D.R.; Karron, R.A.; Saha, S.K.; Sparrow, E.; Srikantiah, P.; Weinberger, D.M.; Zar, H.J. The full value of immunisation against respiratory syncytial virus for infants younger than 1 year: Effects beyond prevention of acute respiratory illness. Lancet Infect. Dis. 2024, 24, e318–e327. [Google Scholar] [PubMed]
- Zhu, J.; Cole, C.B.; Fihman, J.; Adjagba, A.; Dasic, M.; Cernuschi, T. Opportunities to accelerate immunization progress in middle-income countries. Vaccine 2024, 42, S98–S106. [Google Scholar]
- Thaheem, A.K.; Qureshi, A.U.; Sarkar, A.; Liu, G. The Ripple Effect of Vaccines: Health, Economic, and Social Dimensions. J. Soc. Inform. Glob. Health 2023, 2, 40–48. [Google Scholar]
- Rice, I.; Opondo, C.; Nyesigomwe, L.; Ekude, D.; Magezi, J.; Kalanzi, A.; Kerac, M.; Hayes, J.; Robello, M.; Halfman, S. Children with disabilities lack access to nutrition, health and WASH services: A secondary data analysis. Matern. Child Nutr. 2024, 20, e13642. [Google Scholar]
- Mwangi, L.W.; Abuga, J.A.; Cottrell, E.; Kariuki, S.M.; Kinyanjui, S.M.; Newton, C.R. Barriers to access and utilization of healthcare by children with neurological impairments and disability in low-and middle-income countries: A systematic review. Wellcome Open Res. 2022, 6, 61. [Google Scholar]
- O’Neill, J.; Newall, F.; Antolovich, G.; Lima, S.; Danchin, M. Vaccination in people with disability: A review. Hum. Vaccines Immunother. 2020, 16, 7–15. [Google Scholar]
- Thota, A.B.; Mogo, E.I.; Igbelina, C.D.; Sheaf, G.S.; Mustafa, R.; Bakrania, S.; Encalada, A.V.; Wood, G.A. Inclusion Matters: Inclusive Interventions for Children with Disabilities—An Evidence and Gap Map from Low-and Middle-Income Countries; UNICEF Office of Research-Innocenti: Florence, Italy, 2022. [Google Scholar]
- Emerson, E.; Robertson, J.; Baines, S.; Hatton, C. Vaccine coverage among children with and without intellectual disabilities in the UK: Cross sectional study. BMC Public Health 2019, 19, 748. [Google Scholar]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 349, g7647. [Google Scholar]
- Akers, J.; Aguiar-Ibáñez, R.; Baba-Akbari, A. Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Health Care; Centre for Reviews and Dissemination, University of York: York, UK, 2009. [Google Scholar]
- Robertson-Malt, S. JBI’s systematic reviews: Presenting and interpreting findings. AJN Am. J. Nurs. 2014, 114, 49–54. [Google Scholar]
- Kostanjsek, N.F.I. Use of The International Classification of Functioning, Disability and Health (ICF) as a conceptual framework and common language for disability statistics and health information systems. BMC Public Health 2011, 11, S3. [Google Scholar]
- Leonardi, M.; Lee, H.; Kostanjsek, N.; Fornari, A.; Raggi, A.; Martinuzzi, A.; Yáñez, M.; Almborg, A.-H.; Fresk, M.; Besstrashnova, Y. 20 years of ICF—International classification of functioning, disability and health: Uses and applications around the world. Int. J. Environ. Res. Public Health 2022, 19, 11321. [Google Scholar] [CrossRef]
- Team, T.E. EndNote, EndNote X9; Clarivate: Philadelphia, PA, USA, 2013. [Google Scholar]
- Covidence Systematic Review Software, Veritas Health Innovation, Melbourne, Australia. Available online: www.covidence.org (accessed on 3 January 2025).
- Lin, J.-D.; Lin, P.-Y.; Lin, L.-P. Universal hepatitis B vaccination coverage in children and adolescents with intellectual disabilities. Res. Dev. Disabil. 2010, 31, 338–344. [Google Scholar]
- Tuckerman, J.; Mohamed, Y.; Justice, F.; Andersson, T.; Wyatt, K.; Broun, K.; Bastable, A.; Overmars, I.; Kaufman, J.; Danchin, M. Stakeholder perspectives of immunisation delivery for adolescents with disability in specialist schools in Victoria, Australia:‘we need a vaccination pathway’. BMC Public Health 2024, 24, 1973. [Google Scholar]
- Ong, N.; Brogan, D.; Lucien, A.; Wolman, S.; Campbell, D.; Deng, L.; Koirala, A.; Garg, P.; Sharma, K. The development and evaluation of a vaccination pathway for children with intellectual and developmental disability and needle fear. Paediatr. Neonatal Pain 2024, 6, 1–9. [Google Scholar] [PubMed]
- Rosenberg, R.E.; Law, J.K.; Anderson, C.; Samango-Sprouse, C.; Law, P.A. Survey of vaccine beliefs and practices among families affected by autism spectrum disorders. Clin. Pediatr. 2013, 52, 871–874. [Google Scholar]
- Fong, E.; Adil, D.; Mesterman, R. 28 Vaccination experiences for children with special needs-An examination of the impact of behaviours on vaccine uptake. Paediatr. Child Health 2024, 29, e12. [Google Scholar]
- Bray, A. Vaccination Strategies to Keep Children with Special Needs Healthy. 2022. Available online: https://www.clinicaladvisor.com/features/vaccinating-children-with-special-needs/ (accessed on 1 December 2024).
- Okoro, J.; Ojinnaka, N.; Ikefuna, A.; Onyenwe, N. Sociodemographic influences on immunization of children with chronic neurological disorders in Enugu, Nigeria. Trials Vaccinol. 2015, 4, 9–13. [Google Scholar] [CrossRef]
- O’Neill, J.; Newall, F.; Antolovich, G.; Lima, S.; Danchin, M. The uptake of adolescent vaccinations through the school immunisation program in specialist schools in Victoria, Australia. Vaccine 2019, 37, 272–279. [Google Scholar] [CrossRef]
- Mactaggart, I.; Kuper, H.; Murthy, G.V.; Sagar, J.; Oye, J.; Polack, S. Assessing health and rehabilitation needs of people with disabilities in Cameroon and India. Disabil. Rehabil. 2016, 38, 1757–1764. [Google Scholar] [CrossRef]
- United Nations Children’s Fund and Leonard Cheshire Disability and Inclusive Development Centre. Disability Prevention Efforts and Disability Rights: Finding Common Ground on Immunization Efforts; UNICEF: New York, NY, USA, 2020; Available online: https://www.unicef.org/sites/default/files/2022-10/GIP02115_UNICEF_Children-with-Disabilities-Factsheet-final%20-%20accessible.pdf (accessed on 3 January 2025).
- United Nations Children’s Fund. UNICEF Humanitarian Action for Children 2024 Overview. Available online: https://www.unicef.org/media/149906/file/Humanitarian-Action-for-Children-2024-Overview.pdf (accessed on 15 January 2025).
- United Nations Children’s Fund. Children with Disabilities: UNICEF Data 2013. Available online: https://data.unicef.org/wp-content/uploads/2015/12/SOWC_2013_75.pdf (accessed on 15 January 2025).
- United Nations Children’s Fund. The State of World’s Children 2023. Available online: https://www.unicef.org/eca/reports/sowc2023-eca (accessed on 15 January 2025).
- Wang, E.; Clymer, J.; Davis-Hayes, C.; Buttenheim, A. Nonmedical exemptions from school immunization requirements: A systematic review. Am. J. Public Health 2014, 104, e62–e84. [Google Scholar]
- Elias, E.R.; Murphy, N.A.; Liptak, G.S.; Adams, R.C.; Burke, R.; Friedman, S.L.; Houtrow, A.; Kalichman, M.; Kuo, D. Home care of children and youth with complex health care needs and technology dependencies. Pediatrics 2012, 129, 996–1005. [Google Scholar]
- Ashfield, S.; Donelle, L. Parental online information access and childhood vaccination decisions in North America: Scoping review. J. Med. Internet Res. 2020, 22, e20002. [Google Scholar]
- Healy, C.M.; Pickering, L.K. How to communicate with vaccine-hesitant parents. Pediatrics 2011, 127, S127–S133. [Google Scholar] [PubMed]
- Leask, J.; Chapman, S.; Hawe, P.; Burgess, M. What maintains parental support for vaccination when challenged by anti-vaccination messages? A qualitative study. Vaccine 2006, 24, 7238–7245. [Google Scholar]
- Helps, C.; Leask, J.; Barclay, L.; Carter, S. Understanding non-vaccinating parents’ views to inform and improve clinical encounters: A qualitative study in an Australian community. BMJ Open 2019, 9, e026299. [Google Scholar]
- Ward, K.; Quinn, H.E.; Bachelor, M.A.; Bryant, V.; Campbell-Lloyd, S.; Newbound, A.; Scully, M.; Webby, R.J.; McIntyre, P.B. Adolescent school-based vaccination in Australia. Commun. Dis. Intell. Q. Rep. 2013, 37, E156–E167. [Google Scholar]
- Krause, T.G.; Jakobsen, S.S.; Haarh, M.; Mølbak, K. The Danish vaccination register. Euro Surveill. Bull. Eur. Sur Les Mal. Transm. Eur. Commun. Dis. Bull. 2012, 17, 20155. [Google Scholar]
- Murthy, N.C.; Rodgers, L.E.; Pabst, L.J.; Fiebelkorn, A.P.; Ng, T. Progress in Childhood Vaccination Data in Immunization Information Systems—United States, 2013–2016. Morb. Mortal. Wkly. Rep. 2017, 66, 1178–1181. [Google Scholar]
- Carter, A.; Klinner, C.; Young, A.; Strnadová, I.; Wong, H.; Vujovich-Dunn, C.; Newman, C.E.; Davies, C.; Skinner, S.R.; Danchin, M. “I Thought It Was Better to Be Safe than Sorry”: Factors Influencing Parental Decisions on HPV and Other Adolescent Vaccinations for Students with Intellectual Disability and/or Autism in New South Wales, Australia. Vaccines 2024, 12, 922. [Google Scholar] [CrossRef]
- Bruce, J.; Chantler, T.; Kumakech, E.; Mawanda, A.; Olorunsaiye, C.Z.; Schmucker, L.; Kiapi, L.; Landegger, J.; Webster, J. Evaluation of a data-informed community engagement strategy to increase immunisation coverage in northern Uganda: A cluster-randomised controlled trial with an embedded process evaluation. Lancet Glob. Health 2018, 6, S15. [Google Scholar]
- van der Mark, E.J.; Zuiderent-Jerak, T.; Dedding, C.W.M.; Conradie, I.M.; Broerse, J.E.W. Connecting relational wellbeing and participatory action research: Reflections on ‘unlikely’ transformations among women caring for disabled children in South Africa. J. Glob. Ethics 2023, 19, 80–104. [Google Scholar] [CrossRef]
| Criteria | Operational Definition |
| Population | Children with disabilities
|
| Concept | Immunization coverage and equity
|
| Context |
|
| Study Authors | Country/Region | Economic Setting | Method | Study Period | Total Sample | Population | Participants | Themes |
|---|---|---|---|---|---|---|---|---|
| Lin et al. (2010) [16] | Taiwan | HICs | Cross-sectional | NA | 495 | Primary caregivers of children and adolescents with ID | 3–24 years | Theme 3 |
| Tuckerman et al. (2024) [17] | Australia | HIC | Qualitative cross-sectional study | June and September 2022 | 32 | Stakeholders linked to adolescents with disability in specialist schools in Victoria, Australia | Principal/Vice Principal, n = 6 Other school staff, n = 7 Council staff, n = 10 Parent, n = 7 Adolescent, n = 2 | Themes 1, 2, and 3 |
| Ong et al. (2023) [18] | Australia | HIC | Qualitative cross-sectional study | September 2017 to February 2020 | 36 | Children with intellectual and developmental disability and needle fear | Persons who took the children to vaccination | Themes 1, 2, and 3 |
| Rosenberg et al. (2013) [19] | US | HIC | Not specified | January 14 to October 15 2009 | 10,000 diagnosed with ASD and 20,000 direct family members | Autism spectrum disorder (ASD) | Consented affected participants between 4 and 18 years who had completed primary history questionnaires and their consented younger siblings aged above 4.5 years and born after family concern about index development (n = 486 families) | Theme 1 |
| Fong et al. (2024) [20] | Canada | HIC | Cross-sectional survey | November 2022–April 2023 | 109 | Children diagnosed with Autism spectrum disorder (ASD), intellectual disorder (ID), and/or global developmental delay (GDD) aged 6–17 years, seen through outpatient clinics at the Ron Joyce Children’s Health Centre of McMaster Children’s hospital in Hamilton | Families with children aged 6–17 years | Themes 1 and 2 |
| Bray (2022) [21] | General | All settings | Information from expert | Not applicable | Not applicable | Children with special needs Healthy | Not applicable | Themes 1, 2, and 3 |
| Okoro et al. (2015) [22] | Nigeria | HIC | Cross-sectional | NA | 168 | children with neurological disorders | 6 months to 5 years | Themes 1, 2, and 3 |
| Mactaggart et al. (2016) [24] | Cameroon and India | LMIC | Case–control study | February–April 2014 | 1548 | People with disabilities | India: 508 cases and 337 controls Cameroon: 429 cases and 274 controls | Theme 1 |
| UNICEF and Leonard Cheshire Disability (2020) [25] | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | People with disabilities | Not applicable | Themes 2 and 3 |
| UNICEF (2024) [26] | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Children with disabilities | Not applicable | Themes 1, 2, and 3 |
| UNICEF (2013) [27] | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Children with disabilities | Not applicable | Themes 2 and 3 |
| UNICEF (2023) [28] | Indonesia | UMIC | Mixed-method | 2022 | 68 | Key policymakers and implementers | Government: 55 OPD: 11 Civil Society: 1 Academic Institution: 1 | Themes 1, 2, and 3 |
| S/N | Subthemes | Authors | Findings |
|---|---|---|---|
| 1.1 | Barriers related to healthcare systems and social factors | Tuckerman et al. (2024) [17] | Some children do not deliver consent paperwork to their parents, failing to obtain parental or guardian consent for vaccinating. Furthermore, some parents do not trust school workers to deliver immunizations, complicating the process and not providing consent. Schools may also have insufficient resources to assist vaccination efforts, which adds logistical challenges successfully. The level of comfort with disability and assistance received during immunizations significantly impact the vaccination outcome. Meeting the individualized needs of children with disabilities can be difficult, especially when staff have little expertise managing children’s anxiety and disruptive behavior during immunization. Furthermore, the lack of a defined follow-up protocol and parents’ inadequate information regarding sedation choices create further impediments. Inappropriate follow-up settings that are not parent-friendly impede good communication and care, making it difficult to guarantee a smooth and supportive immunization procedure for these children. |
| Fong et al. (2024) [20] | Vaccine administration failure due to children’s behavior. | ||
| Okoro et al. (2015) [22] | The type of chronic neurological disorder also significantly affects the immunization coverage of children. | ||
| Mactaggart et al. (2016) [24] | Most individuals who seek care at healthcare facilities present with illness, leading to failure to accommodate the special needs of children with disabilities. This is exacerbated by the geographical and financial constraints. which limit the families’ access to essential services like immunization. | ||
| UNICEF (2024) [26] | Humanitarian efforts predominantly fail to make provisions for the special needs of children with disabilities, preventing them from accessing essential services like vaccination campaigns that are generally held in schools or child-friendly venues. | ||
| UNICEF (2023) [28] | Essential health services, such as immunization, are not reaching rural areas and do not take into consideration the unique needs of children with disabilities when accessing them, despite the progress that has been made in healthcare in general. | ||
| 1.2 | The influence of education, stigma, and misconceptions | Tuckerman et al. (2024) [17] | Concerns regarding potential HPV vaccine reactions, as well as preferences for some vaccines over others, impact vaccination follow-up and completion rates, and this is more evident among caregivers with high education status. |
| Rosenberg et al. (2013) [19] | Vaccination may be delayed due to the misconceptions about vaccines causing autism. | ||
| Mactaggart et al. (2016) [24] | There was a low level of knowledge about rehabilitation services, which impacted the access to those services. | ||
| Fong et al. (2024) [20] | Parent’s perspective about the influence of the children‘s behavior on vaccination success. | ||
| Bray (2022) [21] | Parents may be hesitant to vaccinate children with special needs with a history of antimicrobial allergies. | ||
| Okoro et al. (2015) [22] | The mother’s educational attainment and father’s occupation were observed to significantly affect the immunization coverage of children with chronic neurological disorders. Children with obvious neurological deficits whose mothers have low educational attainment are at risk of low immunization coverage. Furthermore, stigma also plays a role in lowering the immunization coverage. | ||
| UNICEF (2023) [28] | The belief in a relationship between the vaccination and autism influenced the decision of the mothers, leading to delaying or omitting some vaccinations that were supposed to be taken in early childhood. |
| S/N | Subthemes | Authors | Findings |
|---|---|---|---|
| 2.1 | Enhancing healthcare accessibility and service delivery | Tuckerman et al. (2024) [17] | A focus is placed on adapting information specific to students with disabilities, reassuring parents about safe vaccination spaces and ensuring staff are equipped with basic knowledge to explain the vaccination process. |
| Ong et al. (2023) [18] | The parents wished that services were provided closer to their residential area, which suggests that there is a need for temporally or mobile clinics. | ||
| UNICEF and Leonard Cheshire Disability (2020) [25] | Encouragement for incorporating disability-inclusive policies into national immunization programs in order to guarantee that healthcare facilities are accessible and equipped to serve children with different disabilities. | ||
| Fong et al. (2024) [20] | Administering the vaccine in a low-sensory environment, decreasing wait time for vaccination, and ensuring clinic staff have experience in caring for children with special needs. | ||
| Okoro et al. (2015) [22] | Planners and implementers of immunization programs must make greater efforts to understand the sociodemographic factors affecting immunization of children in order to extend coverage to unreached children, reduce dropout rates, and build sustainable programs. | ||
| 2.2 | Implementing tailored interventions for children with disabilities | Tuckerman et al. (2024) [17] | On vaccination day, a safe and structured environment should be created with distraction techniques, individualized spaces, and support staff to assist students. |
| Ong et al. (2023) [18] | Distraction and sedation techniques should be included in difficult to vaccinate strategies with the aim of reducing the anxiety among children with disabilities during immunization. | ||
| Bray (2022) [21] | The American Academy of Pediatrics (AAP) recommends vaccinating children with special needs following the same CDC immunization schedule as healthy children unless medically contraindicated. However, health-care providers may consider specific physical and psychosocial challenges when immunizing children with special needs to employ various distraction technics, including but not limited to using handheld devices for entertainment, music therapy, or squeezing soft objects, as they have proven effective in reducing anxiety. | ||
| Okoro et al. (2015) [22] | Parental involvement in the immunization program enhances the immunization program, as it helps to reduce children’s anxiety by boosting children’s security and contributing toward an informed decision process for the parents. | ||
| UNICEF and Leonard Cheshire Disability (2020) [25] | Collaboration with local disability-focused groups and non-governmental organizations can boost the consideration of a child’s unique physical, cognitive, or sensory needs, providing a more inclusive approach to healthcare. | ||
| UNICEF (2024) [26] | Reasonable adjustments appropriate to the age of the child with a disability need to be made to ensure that they are given physical access to services and support for psychosocial disabilities. Also, careful identification of the need for vaccination and fighting stigma that children with disabilities or their parents may face is required. | ||
| UNICEF (2023) [28] | The child with disabilities requires special accommodations to access the health services. | ||
| 2.3 | Addressing societal factors like stigma and education | Tuckerman et al. (2024) [17] | Providing information and consent forms in multiple languages and simplifying communication for parents with culturally and linguistically diverse backgrounds using visuals and tailored formats. Schools are encouraged to better educate parents on the importance of vaccination through resources, information sessions, and school communication channels like newsletters. |
| Okoro et al. (2015) [22] | Healthcare workers may identify some signs and symptoms as contradictions for vaccination. Measures to reduce socioeconomic disparities also need to be taken, as they influence vaccination uptake. | ||
| UNICEF (2013) [27] | Including children with disabilities in promotion materials, like posters for immunization programs, can raise awareness and enhance the understanding of the community on the need for vaccination uptake among children with disabilities. | ||
| UNICEF (2023) [28] | Involvement of civil society, community members, children with disabilities, and organizations advocating for people with disabilities is instrumental in ensuring that the policies are inclusive and respond to the stigma. |
| S/N | Subthemes | Authors | Findings |
|---|---|---|---|
| 3.1 | Creating supportive and inclusive environments | Tuckerman et al. (2024) [17] | Children with disabilities are very sensitive to environment, and anything that goes wrong can turn things around easily. The right physical environment with adequate infrastructure and distraction toys for children has a positive impact on the day of vaccination. The necessary efforts must be implemented to ensure that vaccination is successful at the first visit, as repeating the procedure requires extra effort. Some parents request information about alternative information that is outside the knowledge of school staff. |
| Ong et al. (2023) [18] | The seduction pathway needs to be implemented in case vaccination with the distraction method is unsuccessful. | ||
| Bray (2022) [21] | Positive techniques exist to assist the pediatric provider. It is essential to consider positioning and restraining the child with special needs during immunization procedures. Rather than lying down, sitting upright during immunizations increases a child’s comfort level and sense of control. | ||
| UNICEF and Leonard Cheshire Disability (2020) [25] | Healthcare facilities should be inclusive to take into consideration adolescents and children in the immunization program, and the message delivered for immunization need to be disability friendly to minimize the stigma that children with disabilities frequently confront. | ||
| UNICEF (2023) [28] | The integration of immunization services for children with disabilities among the usual immunization programs that take place at school contributed to the uptake of vaccination among children with disabilities in Indonesia. Further children with disabilities need to be considered in health-sector plans and budgets at the national and sub-national levels. | ||
| 3.2 | Empowering families and children | Tuckerman et al. (2024) [17] | Parents need to be informed about the vaccination date and given the opportunity to attend, fostering a more inclusive and supportive immunization process. Anxiety is common, and some adolescents are scared before being vaccinated. |
| Ong et al. (2023) [27] | Having a positive experience among the parents through involvement led to empowerment of these children. | ||
| Okoro et al. (2015) [22] | There is a need to sustain regular health education aimed at emphasizing the benefits of vaccination and dispelling false concerns about the side effects of immunizations. | ||
| Lin et al. (2010) [16] | Health income influenced the uptake level of vaccination, and sensitivity toward the families of children with disabilities is essential for ensuring that they are aware of the benefits of vaccination. | ||
| Bray (2022) [21] | Adequate communication with clear and concise information from healthcare professionals for parents is fundamental in highlighting and convincing the parent to ensure that their child with disabilities adheres to the CDC-recommended immunization schedule. | ||
| UNICEF (2024) [26] | Communicating the rights of children with disabilities to access health services, including immunization, is important to boost the immunization uptake. | ||
| 3.3 | Tailoring immunization services to individual needs | Tuckerman et al. (2024) [17] | The need for more parent information sessions about options and additional support for vaccination outside of the school program was raised by the parents. The immunization program in special schools was perceived as convenient; however, preparing students for vaccination day and catering to individual student needs were important for the vaccination outcome. |
| Ong et al. (2023) [18] | Children with needle phobias were prepared through discussion to help them deal with anxiety, and this led to a good outcome. This was complimented by a mock trial with a nitrous mask to sedate the child, and the preparation of the parents through adequate information sharing was taken into consideration a priori. This shows how individual needs were employed. | ||
| Bray (2022) [21] | Healthcare providers, like pediatric providers, need to have knowledge related to the specific needs of children with conditions such as autism to ensure that they are given sufficient information and vaccinated. | ||
| UNICEF and Leonard Cheshire Disability (2020) [25] | Girls with disabilities are less likely to access health services in comparison to boys with disabilities; therefore, additional attention is required to tailor the immunization program to facilitate an increase in uptake in the mentioned group. | ||
| UNICEF (2013) [27] | Immunization services for children with disabilities require special consideration to ensure their inclusiveness. | ||
| UNICEF (2023) [28] | The MoH Regulation No. 25/2014 on Child Health Efforts covers the provision of health services for children with disabilities, whereby they may receive healthcare beyond the healthcare facilities in place, including specialized schools, inclusive education schools, households, and other institutions. In this regulation, the health centers near specialized schools are obliged to provide immunization services at those schools. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Musuka, G.; Cuadros, D.F.; Miller, F.D.; Mukandavire, Z.; Dhliwayo, T.; Iradukunda, P.G.; Mano, O.; Dzinamarira, T. Immunization Coverage, Equity, and Access for Children with Disabilities: A Scoping Review of Challenges, Strategies, and Lessons Learned to Reduce the Number of Zero-Dose Children. Vaccines 2025, 13, 377. https://doi.org/10.3390/vaccines13040377
Musuka G, Cuadros DF, Miller FD, Mukandavire Z, Dhliwayo T, Iradukunda PG, Mano O, Dzinamarira T. Immunization Coverage, Equity, and Access for Children with Disabilities: A Scoping Review of Challenges, Strategies, and Lessons Learned to Reduce the Number of Zero-Dose Children. Vaccines. 2025; 13(4):377. https://doi.org/10.3390/vaccines13040377
Chicago/Turabian StyleMusuka, Godfrey, Diego F. Cuadros, F. DeWolfe Miller, Zindoga Mukandavire, Tapiwa Dhliwayo, Patrick Gad Iradukunda, Oscar Mano, and Tafadzwa Dzinamarira. 2025. "Immunization Coverage, Equity, and Access for Children with Disabilities: A Scoping Review of Challenges, Strategies, and Lessons Learned to Reduce the Number of Zero-Dose Children" Vaccines 13, no. 4: 377. https://doi.org/10.3390/vaccines13040377
APA StyleMusuka, G., Cuadros, D. F., Miller, F. D., Mukandavire, Z., Dhliwayo, T., Iradukunda, P. G., Mano, O., & Dzinamarira, T. (2025). Immunization Coverage, Equity, and Access for Children with Disabilities: A Scoping Review of Challenges, Strategies, and Lessons Learned to Reduce the Number of Zero-Dose Children. Vaccines, 13(4), 377. https://doi.org/10.3390/vaccines13040377











