1. Introduction
Foot-and-mouth disease (FMD) is highly contagious and caused by the FMD virus (FMDV), the type species of the
Aphthovirus genus of the
Picornaviridae, a family of small, single-stranded positive-sense RNA viruses. The FMDV genome is encased in an icosahedral capsid formed by 60 copies each of four structural proteins (VP1–VP4). The outer capsid is formed by VP1–VP3; VP1 surrounds the icosahedral 5-fold symmetry axes, while VP2 and VP3 alternate around the 3-fold symmetry axes [
1,
2]. To initiate an infection, the capsid proteins interact with cellular receptors. In vivo, FMDV field strains preferentially target epithelial cells, and use the epithelial cell-restricted integrin αvβ6 as the principal receptor [
3,
4,
5,
6,
7]. FMDV binds αvβ6 via a conserved arginine-glycine-aspartic acid (RGD) motif in the GH-loop of VP1 and can also use other RGD-dependent integrins (αvβ1, αvβ3, and αvβ8) to initiate infection [
8,
9,
10], but the role of these integrins in vivo is unclear.
FMD is endemic in many regions of the world and affects several wildlife species and also domesticated livestock, such as cattle, sheep, goats, and pigs [
11,
12]. FMD is associated with significant economic losses as a result of reduced productivity and trade restrictions imposed on affected countries [
13]; thus, the impacts are likely to be greater for countries where FMD is endemic. For disease-free countries, the costs of maintaining a disease-free status can also be high, and they can also incur enormous financial losses as the consequence of a sporadic incursion [
14]. Vaccination is important for controlling FMD in endemic regions and for lessening the effects of an outbreak in FMD-free countries [
15]. FMDV exists as seven serotypes (O, A, C, Asia-1, and the Southern African Territories [SAT] serotypes, SAT-1, SAT-2, and SAT-3). This complicates efforts to control FMD via vaccination, as different vaccines are required for each serotype. Furthermore, within each serotype a large number of constantly evolving antigenic variants exist, which can lead to the emergence of novel strains [
16,
17]. This further complicates FMD control, as animals vaccinated with a specific strain may not be protected from infection by another virus of the same serotype, and new emerging strains may evade the immunity induced by the current vaccines [
18]. Consequently, vaccines need to be a close antigenic match for the outbreak virus, which can necessitate the need to rapidly develop new vaccine strains to protect against emerging variants for which the existing vaccines are a poor match.
The current FMDV vaccines are chemically inactivated virus preparations produced in mammalian cell cultures in large industrial-scale fermenters. Baby hamster kidney cells (BHK-21 clone 13), that grow in suspension [
19], are commonly used for vaccine production. However, BHK cells lack the αvβ6 integrin and can produce low yields of vaccine virus [
7]. Thus, FMDV field strains may need to be adapted by serial passage to grow efficiently in BHK cell systems. The adaptation process is driven in part by the availability of cell surface receptors, and often selects for variants with amino acid (aa) changes on the outer surfaces of the capsids that allow the use of alternative, non-integrin receptors, such as heparan sulphate (HS), for cell attachment and entry [
20,
21,
22,
23,
24,
25,
26,
27,
28,
29].
Knowledge of the changes in the viral capsid that permit the use of non-integrin receptors could allow for the rational design of vaccine viruses that do not need to be adapted to BHK cells. Adaptation to HS receptors was first demonstrated for FMDV O1BFS [
24], and subsequent studies identified the residue at VP3-56 as important for HS binding [
27,
30]. The structure of O1BFS bound to heparin (a structural analogue of HS) [
30] showed that the HS binding site (here called the canonical HS binding site) is formed by a shallow depression in the outer capsid surface [
30]. In the complex, heparin makes multiple contacts with all three outer capsid proteins, with the most prominent contacts made with R residues at VP3-56 and VP2-135 and a histidine (H) at VP1-195 [
30]. In the FMDV field strain O1Kcar
2, which does not bind HS, VP3-56 is H, while the other main heparin contact residues are conserved between O1BFS and O1Kcar
2. Thus, for type O FMDV, the switch to HS binding appears to arise from only a small number of residue changes (including at VP3-56) that result in a net gain in positive charge in the depression that forms the HS binding site [
27,
30]. The structure of another cell-culture-adapted strain of FMDV, A1061, also in a complex with heparin, revealed a HS binding site in the same location on the capsid that is structurally very similar to that of O1BFS [
22]. This suggests a common mechanism for cell culture adaptation; however, although the depression that forms the HS binding site is a conserved feature of FMDV capsids [
2,
22,
31], other type A viruses, and viruses representative of other FMDV serotypes, do not appear to acquire the ability to bind HS at this site. Instead, cell culture adaptation selects for aa changes at other locations, in particular at a “hotspot” at the icosahedral, 5-fold symmetry axes of the capsid [
25,
26,
28,
32,
33,
34,
35]. The aa substitutions at the 5-fold symmetry axes that are associated with altered receptor usage and improved virus growth in cell cultures often occur in the βF-βG (residues 83–85) and βD-βE (residues 108–112) loops of VP1 and involve positively charged aa substitutions. As five copies of VP1 surround the 5-fold symmetry axes, this creates a dense patch of positive charge on the outer capsid surface, which is thought to facilitate interactions with cell surface receptors. For example, a single glutamine (Q) to lysine (K) change at VP1-109 acquired during BHK cell passage enabled integrin-independent infection of CHO cells (which lack expression of the integrins used as receptors by FMDV) and improved virus growth in cell cultures by a virus with the capsid proteins from the A/Turkey/2/2006 field isolate [
32]. Importantly, this same aa change also allowed for integrin-independent infection of CHO cells and improved virus growth in cell culture when it was introduced into FMDVs that had the capsids of type O (OUKG/35/2001) or Asia-1 (Asia-1/Bar/9/2009) field viruses [
32]. Similarly for the SAT viruses, the acquisition of positively charged aa at VP1 110-112 and VP1 83-85 is associated with altered receptor usage and improved virus growth in cell cultures [
25,
26].
Adaptation of FMDV field strains to BHK cells can be time consuming, costly, and prove difficult for some viruses, and thus complicates efforts to develop a new vaccine to novel emerging strains. Here, we attempt to bypass the need for cell culture adaptation by generating chimeric FMDVs with capsids derived from field viruses (representative of type O, A, Asia-1, and SAT2) that include aa changes that occur during cell culture passage and characterise their growth in adherent and suspension BHK cells. The purpose of this approach is to improve virus growth under vaccine manufacturing conditions by the introduction of targeted amino acid changes to the capsid, rather than by protracted serial passage.
Our results show that the introduced changes increased the rate of virus growth in both adherent and suspension BHK cells. Importantly, we also show that for viruses that grow poorly in BHK cells, some aa changes can greatly improve yields of 146S (Svedberg units) intact virus particles under vaccine manufacturing conditions. In addition, we show that the stability and antigenicity of selected viruses was not adversely affected by the introduced changes. This approach has the potential to greatly expedite the production of new vaccine strains by eliminating the need for time-consuming and expensive cell culture adaptation. It may also reduce the need for extraneous agent testing, since viruses are produced in vitro rather than being isolated from field samples.
2. Materials and Methods
2.1. Cell Culture
Adherent baby hamster kidney (BHK-21 clone 13) cells (Pirbright Institute, Woking, UK) and IBRS-2 cells (Pirbright Institute, Woking, UK) were cultured in Glasgow’s modified Eagle’s medium (GMEM) (Sigma, Gillingham, UK) and Chinese hamster ovary (CHO) cells (ATCC CCL-61) in Ham’s F-12 (Sigma, Gillingham, UK), each supplemented with 10% foetal calf serum (FCS), 20 mM glutamine, penicillin (100 SI units/mL), and streptomycin (100 μg/mL). Primary bovine thyroid (BTY) cells and primary pig kidney cells were prepared and cultivated as described previously [
36,
37]. Boehringer–Ingelheim suspension baby hamster kidney (BHK-21) cells were cultured in a 5 L UniVessel
® Glass Bioreactor controlled by a BIOSTAT B controller (Sartorius Stedim Biotech, Aubagne, France), with a working volume of 2–4 L in BI Gibco Glasgow medium (GMEM) supplemented with 5% adult bovine serum (ABS). Cells were maintained under pH and dO2 control (pH 7.3, 40% dO2, 37 °C) and stirred continuously (450–800 rpm).
2.2. Infectious Copy Plasmids and Rescue of Recombinant Viruses
All of the infectious copy plasmids used in this study were based on pT7S3 [
38], which contains a cDNA copy of the full-length viral RNA (vRNA) of FMDV O1Kaufbeuren (O1K). Chimeric viruses with wt capsids were generated by replacing the coding regions for VP2, VP3, VP1 and 2A of O1K with the corresponding region of a field virus. The construction of the infectious copy plasmids for viruses with wt capsids of A-Turkey/2/2006, Asia-1/Bar/9/2009 or OUKG/35/2001 (here called O1K-A WT, O1K-Asia WT and O1K-O WT, respectively) has been described previously [
32]. Plasmids for the O1K-A KK, O1K-A RK, O1K-Asia KK, O1K-O KK and O1K-O RK viruses were generated by QuikChange Lightning site-directed mutagenesis (Agilent Technologies, Didcot, UK) using the appropriate infectious copy plasmid as the template and primer pairs, as described previously [
32]. The infectious copy plasmids for the O1K-A HS, O1K-Asia RK, O1K-Asia HS, O
1K-O HS, O1K-SAT2 WT, O1K-SAT2 KGR, O1K-SAT2 KKR, O1K-SAT2 KHR and O1K-SAT2 HS viruses were constructed for this study and were based on a modified pT7S3 (pT7S3-SpeI) that was modified to remove an SpeI site in the plasmid backbone such that it contained unique AflII and SpeI restriction enzyme sites in the regions encoding for L
pro and 2B, respectively. For each of the above infectious copy plasmids, DNA sequences covering the AflII site and the SpeI site and including the appropriate aa changes (as shown in
Table 1,
Table 2 and
Table 3) were synthesised by Geneart. The synthesised DNA was initially cloned into pCR Blunt II-TOPO (Life Technologies, Paisley, UK) via blunt-end topisomerase cloning. The fragment containing the capsid region was recovered by double restriction digestion with AflII and SpeI and then ligated into similarly digested pT7S3-SpeI.
2.3. Virus Recovery
Infectious copy plasmids were linearised using HpaI and used as the template to synthesise full-length vRNA using an Ambion Megascript T7 kit (Life Technologies, Paisley, UK). Due to the presence of multiple HpaI sites, RNA was synthesised from the O1K-Asia WT and O1K-Asia KK plasmids without linearisation. The synthesised RNA (6.5 μg) was transfected into BHK-21 cells in 25 cm2 tissue culture flasks using Trans-IT mRNA transfection reagent (Mirus). Transfected BHK-21 cells were incubated at 37 °C for 24 hours (h) and then cell lysates were prepared by freeze-thawing. Viruses with wt capsids were subsequently passaged on BTY cells to minimise the chances of cell culture adaptation during recovery. All other viruses were passaged on adherent BHK-21 cells.
2.4. Viral Genome Sequencing
Clarified infected-cell lysates (0.5 mL) were added to 0.5 mL of trizol reagent (Life Technologies, Paisley, UK) and total RNA extracted as per the manufacturer’s instructions. The extracted RNA was converted to double-stranded cDNA, as described previously [
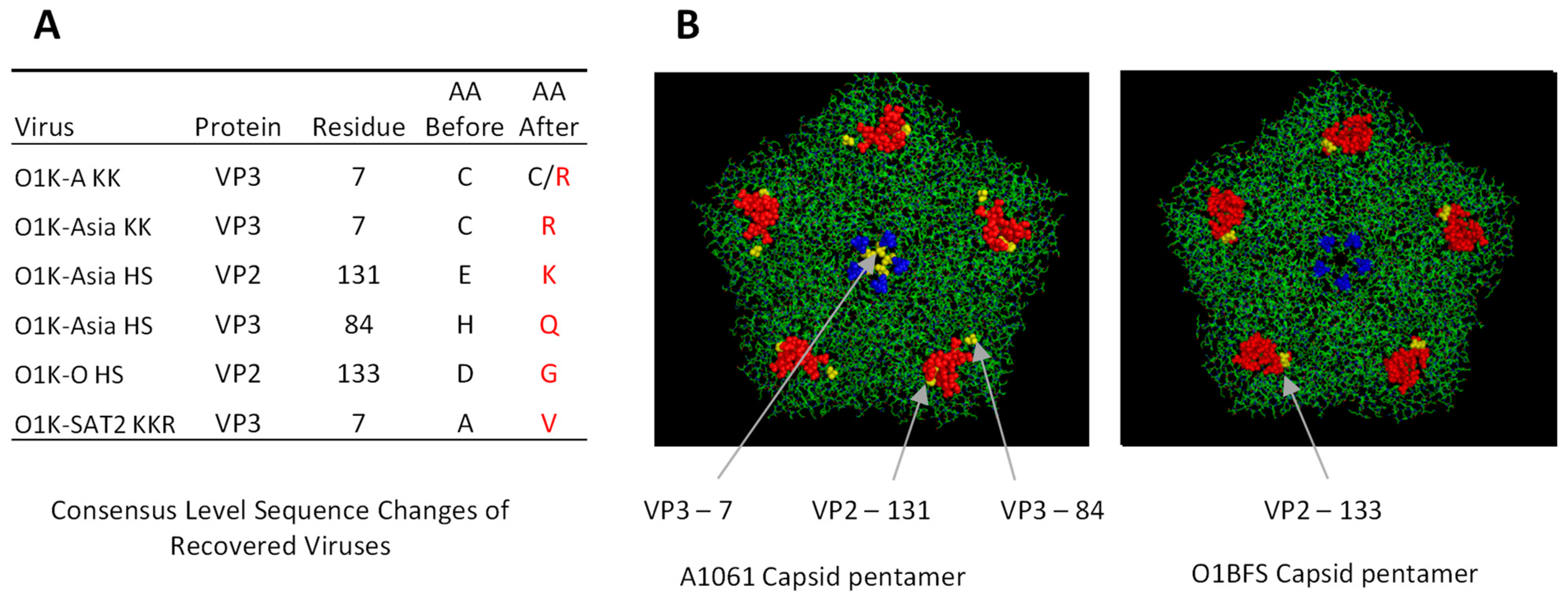
39]. One nanogram of each cDNA sample (0.2 ng/μL) was used to prepare sequencing libraries using the Nextera XT DNA Sample Preparation Kit (Illumina, San Diego, CA, USA). Libraries were sequenced on a MiSeq using 300 cycle version 2 reagent cartridges (Illumina) to produce paired-end reads of approximately 150 bp each. Reads were assembled against an expected reference sequence using Seqman Ngen 14, and Seqman Pro 14 software (DNAstar, Madison, WI, USA) was used to view the line-ups and to generate a consensus sequence for each virus. Where additional non-synonymous mutations were found during virus recovery, the locations of aa changes were mapped onto the structure of an O
1BFS FMDV pentamer (type O viruses; Protein Database ID:1FOD) or an A1061 FMDV pentamer (other serotypes; Protein Database ID:1ZBE).
2.5. Virus Titration (Plaque Assay)
Subconfluent BHK-21 or BTY cell monolayers in 6-well plates were incubated with serial dilutions of FMDV for 15 min at 37 °C. The cells were then overlaid with 4 mL of Eagle’s overlay (0.6% indubiose A37 (MP biomedicals, Santa Ana, CA, USA), 5% tryptone phosphate broth, 1% FCS in Eagle’s medium). After 48 h of incubation at 37 °C, the cells were fixed and stained with 4% formaldehyde/0.1% methylene blue.
2.6. Virus Purification
BHK-21 cells (O1K-O KK, O1K-O RK, O1K-O HS) or BTY cells (O1K-O WT) were infected with FMDV and freeze-thawed at the point of a complete CPE (cytopathic effect). The resulting lysate was clarified and the virus was precipitated by means of the addition of ammonium sulphate to give a 50% saturated solution. The precipitate was pelleted at 4800× g at 4 °C for 1 h and resuspended in phosphate-buffered saline (PBS) (pH 7.4) containing 1% IGEPAL CA-630. The virus was pelleted through a 30% sucrose cushion at 134,000× g (280,000 rpm) for 2.5 h, resuspended as described before, and purified by sedimentation through a 15–30% continuous sucrose gradient by centrifugation at 304,000× g (50,000 rpm) for 35 min. The purified virus was located by measuring the absorbance of gradient fractions at 260 nm using a spectrophotometer and quantified using the following formula: (OD260)/7.6 = mg/mL of virus.
2.7. Thermal Stability Assay
Thermal stability assays (PaSTRy assays) were performed using an MX3005 PCR machine (Agilent Technologies, Discot, UK) as described previously [
40]. The assays were performed using 1 μg of purified virus and SYBR green-II dye (Invitrogen; final dilution 1:10,000) diluted to 100 μL in PBS buffer lacking divalent cations, and the sucrose content was kept constant between samples. The temperature was ramped from 25 °C to 94 °C in 0.5 °C increments with intervals of 20 seconds and fluorescence was read at each temperature (Excitation: 490 nm Emission: 516 nm). Data were visualised using MxPro version 4.10 software (Stratagene). Capsid dissociation, and hence the release of vRNA, was detected by the increases in fluorescence signal, and the temperature of RNA exposure (T
R) was taken as the minimum of the negative first derivative of the fluorescence curve.
2.8. Adherent BHK-21 Cells: CPE and Infectious Yield Assays
Adherent BHK-21 cells were grown to 95% confluency in 96-well tissue culture plates. Wells were washed once with virus growth medium (VGM: normal cell culture medium with reduced (1%) serum) and infected with FMDV in a volume of 50 μL at a multiplicity of infection (MOI) of 0.01. After 1 h at 37 °C, the virus inoculum was replaced with 150 μL of VGM. The infection was continued at 37 °C and cell confluency in each well was quantified at 0.5 h intervals (10× objective, 4 images per well) for 50 h using the Incucyte S3 live cell analysis system (Sartorius, Gottingen, Germany) and Incucyte S3 2018B software using default software settings. To assess the rate of CPE, the average confluency of five replicate wells was plotted against time.
For virus yield experiments, BHK-21 cells in 96-well plates were infected (MOI = 0.01) and incubated at 37 °C until the cell confluency dropped below 80%. Cells were then freeze-thawed, cell supernatants and cell debris were separated by centrifugation, and the supernatant was transferred to separate Eppendorf tubes and stored at −80 °C. The infectious viral titre (using triplicate samples for each virus) was determined by a standard plaque assay on BHK-21 cells.
2.9. FMDV Growth in Suspension BHK-21 Cell Bioreactors
A BHK-21 suspension culture in log growth phase was transferred to 400 mL mini-bioreactors (AppliKon Biotechnology, Delft, The Netherlands) at a density of ~2 × 10
6 cells/mL. Cells were settled to the bottom of the reactor at 5 °C and the medium (GMEM + 5%ABS) was replaced with GMEM without ABS. After resuspension of the cells, the culture was infected with the relevant virus at an MOI of 0.001 under pH and dO2 control (pH 7.3, 40% dO2) at 37 °C and with continuous stirring at 400 rpm. Virus stocks used for infection were made on the same batch of primary pig kidney cells and were sequenced to check for aa changes in the capsid. At 16 h, 19 h, 22 h and 40 h post-infection, samples were taken, of which 15 mL was directly frozen at −80 °C (harvest sample) and 15 mL was clarified by centrifugation for 20 min at 2585×
g (3400 rpm) and then stored (clarified samples) to mimic centrifugation downstream processing steps in industrial operations. Yield data from suspension BHK cells presented in this study were obtained using the “clarified” samples. To identify dead cells, live cell counts were carried out using a counting chamber (Fuchs Rosenthal) and cells were diluted in PBS plus Trypan Blue (0.4%) (Life technologies, Paisley, UK). Cell counts were used to calculate CPE using the following formula:
VCD = viable cell density
Suspension culture experiments were performed in triplicate.
For chimeric viruses with type A and Asia-1 capsids, antigen from a single batch was used for antiserum generation.
2.10. Quantitation of 146S Particles from Bioreactor Cultures by ELISA
The yield of 146S particles for FMDV with type A and type O capsids was determined by the enzyme-linked immunosorbent assay (ELISA) [
41]. Briefly, 96-well plates (Corning) were coated overnight at 4 °C with 100 µL (0.05 µg/mL) per well of 12S-specific M3 single-domain antibody fragments (VHH). The wells were washed and sequentially incubated for 1 h at room temperature (RT) with twofold serial dilutions of unheated or heated (2 h at 56 °C to dissociate 146S in to 12S) FMDV samples, biotinylated M3 (0.1 µg/mL), and 1:10,000 streptavidin-HRP (Jackson ImmunoResearch), with washing between incubations. After a final washing step, 100 μL/well TMB (3,3′,5,5′-Tetramethylbenzidine) was added and the reaction was stopped after ten minutes using 0.5 M H
2SO
4. The absorbance was measured at 450 nm and the 12S content was calculated using a standard curve generated using 12S particles of the FMDV O
1Manisa reference strain. The difference between the 12S content of unheated and heated samples (to dissociate 146S into 12S) is a measure for the amount of 146S particles present. ELISAs were only valid when the internal control differed by less than two SDs from the trend. For each 400 mL culture experiment, ELISAs were performed twice.
2.11. UV-Peak for 146S Quantification
The yield of 146S particles for FMDV with Asia-1 and SAT2 capsids was determined by sucrose density gradients as described previously [
42]. Briefly, a 2 mL antigen sample was slowly added into 10 mL premade discontinuous 15–45% sucrose gradient solutions. Gradients were centrifuged at 48,700×
g (16,500 rpm) at 5 °C for 16 h in an ultracentrifuge (Optima XE-90; Beckman Coulter, Brea, CA, USA). The centrifuged solution was pumped through a UV detector (LKB-Bromma 2238 UVICORD S-II; Cytiva, Marlborough, MA, USA) at an adsorption of 254 nm. Based on the area under the curve of the UV peak, the 146S antigenic mass could be calculated. All assays were performed in duplicate, and assays were only valid when a known reference differed by less than two SDs from the trend.
2.12. Antiserum Production
Antisera for the virus neutralisation tests (VNTs) were raised against the chimeric viruses with type A and Asia-1 capsid using 13-week-old healthy SPF White New Zealand rabbits. Immunisation in rabbits was approved by the ethical committee of Wageningen University and Research under project number 2016.D-0062.13 and was carried out in the Veterinary BSL-4 facilities at Wageningen Bioveterinary Research, Lelystad, The Netherlands.
In order to raise the antisera, vaccines were prepared by infecting 400 mL suspension cultures of BHK-21 cells with O1K-A WT, O1K-A KK, O1K-A RK, O1K-Asia WT, O1K-AsiaI KK, or O1K-Asia HS virus. Virus cultures were inactivated by the addition of 0.01 M Binary ethylenimine (BEI) for 24 h at RT. BEI was neutralised by the addition of 0.5% sodium thiosulphate for 1 h at RT. Antigens were concentrated by means of precipitation with 7.5% polyethylene glycol for 16 h at 4 °C. After centrifugation at 2500× g for 45 min at 4 °C, the pellet was resuspended in Tris/KCl (20 mM Tris, 300 mM KCl, pH 7.5) buffer and the antigen concentration was determined using the UV peak.
Groups of four rabbits were subcutaneously vaccinated with 0.5 mL of 20 μg/mL (O1K-A WT, O1K-A KK, O1K-A RK) or 15 μg/mL (O1K-Asia WT, O1K-AsiaI KK or O1K-Asia HS) antigens diluted 1:1 in Tris/KCl and Montanide ISA50V2 (Seppic). After 21 days, the rabbits were booster vaccinated using the same method. At 42 days post-vaccination, the rabbits were sacrificed and serum was retrieved from the blood by means of centrifugation and stored at −20 °C until use in VNTs.
2.13. Virus Neutralisation Tests Using IBRS-2 Cells
Virus stocks used in the VNT were grown on IBRS-2 monolayers and were titrated in triplicate using the same cells. Experimental serum samples obtained by vaccination of rabbits using viruses generated in this study (see “Antiserum production”) were inactivated at 56 °C for 0.5 h before testing. Virus neutralisation tests were performed according to the protocol recommended by the World Organisation for Animal Health [
43,
44]. Neat serum stocks were initially diluted 1:8 and then in two-fold dilutions for the tests. For each test, a 100 TCID50 of virus was used in a total volume of 50 μL. Neutralising antibody titres, calculated by the Spearman–Karber method, were expressed as the last dilution of serum that neutralises 50% of the virus.
2.14. Virus Neutralisation Tests Using BTY Cells
Virus stocks used in the VNT were grown on BTY monolayers and were titrated in triplicate using the same cells. Anti-Asia-1, -type O, -type A, and -SAT-2 antisera were obtained from the World Reference Laboratory at Pirbright. Virus samples and sera were diluted in reduced serum (1%) BTY cell culture medium. Sera were diluted to an initial dilution of 1/8 or 1/16, diluted two-fold six subsequent times in duplicate, and 70 μL of the serum dilutions were added per well of a 96-well flat bottom plate. Diluted viruses (70 μL) were added to the wells with the serum dilutions, such that each well contained 200 TCID50 per 100 μL. The mixtures were incubated for 1 h at RT. BTY cells grown to confluency in a separate 96-well plate were washed once with reduced serum BTY medium, and 50 μL of BTY medium was added to each well. The antibody/virus mixtures (100 μL) were transferred to the equivalent well of the 96-well plate containing BTY cells. Plates were then incubated for 3 days at 37 °C and 5% CO2, in a humidified atmosphere, and then fixed and read as above for IBRS-2 cells.
2.15. Statistical Analysis
Statistical significance between groups was assessed via an unpaired two-tailed t-test. A p-value of <0.05 was considered statistically significant. Data distribution was analysed via the Ryan Joiner normality test using Minitab 10 software prior to the t-test.
4. Discussion
The production of a new vaccine to combat an emerging novel variant of FMDV may require the adaptation of the outbreak virus to BHK cells. This can be time consuming, as field viruses often grow poorly in the suspension BHK cell lines used for vaccine manufacture. The adaptation process is driven, in part, by the availability of integrin receptors that are used by FMDV field viruses to enter cells, and it selects variants with capsid aa changes that allow use of novel cell attachment receptors. Interestingly, even for viruses of the same FMDV serotype, this process does not always involve aa changes at the same site on the capsid or result in the ability to use a common alternative receptor [
20,
24,
25,
26,
27,
28,
29,
32,
33,
34,
35,
47]. Furthermore, changes in the capsid may be different when the same FMDV strain is adapted to adherent or suspension BHK cell culture systems [
48,
49].
Previously, we [
32,
47] and others [
21,
26,
27,
50] have generated chimeric viruses that combine the capsid proteins of FMDV field strains with the non-structural proteins (nsps) of cell-culture-adapted viruses. Such chimeric viruses have proven useful to study the aa changes in the capsid proteins that allow for integrin-independent infection of cultured cells, such as BHK-21 and CHO cells. Furthermore, it has been proposed that such viruses could be engineered to include aa changes in the capsid proteins that allow for infection of BHK-21 cells, as a means to bypass the need for cell culture adaptation, especially for field viruses when adaptation proves intractable. In the current study, we used four chimeric viruses (O1K-A WT, O1K-Asia WT, O1K-O WT and O1K-SAT2 WT) with wt capsids derived from the FMDV field strains A-Turkey/2/2006, Asia-1/Bar/9/2009, OUKG/35/2001, and SAT2/EGY/9/2012. All four could be readily recovered using BTY cells, and two (O1K-A WT and O1K-Asia WT) could readily infect BHK-21 cells without the need to make additional aa substitutions. In contrast, the other two viruses (O1K-O WT and O1K-SAT2 WT) were poorly infectious for BHK-21 cells. A possible explanation for this is that whilst viruses with wt capsids are able to use the αvβ6 integrin, the preferred receptor used by field strains and expressed on BTY cells [
51], they may have different abilities to utilise the αvβ3 integrin receptor expressed on BHK-21 cells [
7]. This is consistent with previous work reporting that type O viruses use αvβ3 much less efficiently than type A viruses [
52]. In an attempt to bypass the need for cell culture adaptation, we also generated variants of the above chimeric viruses with aa changes in the capsids and characterised their growth in adherent and suspension BHK-21 cells. We targeted two sites on the capsid: the canonical HS binding site (as identified on FMDV O1BFS and A1061) and the icosahedral, 5-fold symmetry axes of the capsid. In addition, the different abilities of the viruses with wt capsids to infect BHK-21 cells allowed us to investigate the effects of introducing aa substitutions into viruses that could or could not already infect BHK-21 cells.
For the chimeric viruses with capsids derived from A-Turkey/2/2006 (O1K-A KK and O1K-A RK), Asia-1/Bar/9/2009 (O1K-Asia KK), or OUKG/35/2001 (O1K-O KK and O1K-O RK), five of the six viruses with positively charged aa at both VP1 109 and 110 could be recovered using BHK-21 cells (see
Table 1) and could also infect CHO cells ([
32] and this study), which indicates the ability to use non-integrin receptors. However, we were surprised to find that we could not recover the O1K-Asia RK virus. This included repeated attempts to rescue the virus from transfected BHK-21 cells by passage on BTY cells. It is not clear why the O1K-Asia RK virus could not be recovered. However, the observations that the O1K-O RK and O1K-A RK viruses are viable suggest that it is unlikely that such small changes (four nucleotides and two aa) would alter vRNA translation, viral polyprotein processing, or vRNA replication, and further work will be required to identify the reasons why the O1K-Asia RK virus is non-viable. During cell culture passage, SAT viruses also accumulate aa substitutions in their capsid proteins that often involve the gain of positively charged aa at VP1 110–112. Here, we constructed chimeric viruses based on the capsids of SAT2/EGY/9/2012 with targeted aa changes at these residues (O1K-SAT2 KGR and O1K-SAT2 KKR). Both of these viruses were viable as they could be recovered using BTY cells; however, although the O1K-SAT2-KGR virus could be recovered using BTY cells, it was not recovered when using BHK-21 cells for the post-transfection passage steps. This suggests that a single R substitution at VP1 112 is tolerated in the SAT2 capsid, but it is insufficient by itself to allow the use of non-integrin receptors to initiate infection. During cell culture passage, SAT viruses also accumulate aa substitutions at VP1 83–85. A study by Maree et al. suggested that a negatively charged aa at VP1 83 could interfere with receptor interactions that involve the R at VP1 85 [
26]. Therefore, based on this possibility, in the chimeric SAT2 virus generated in our study (O1K-SAT2 KHR), we introduced positively charged aa at both VP1 83 and 85. However, for reasons that we do not yet understand, this virus could not be recovered.
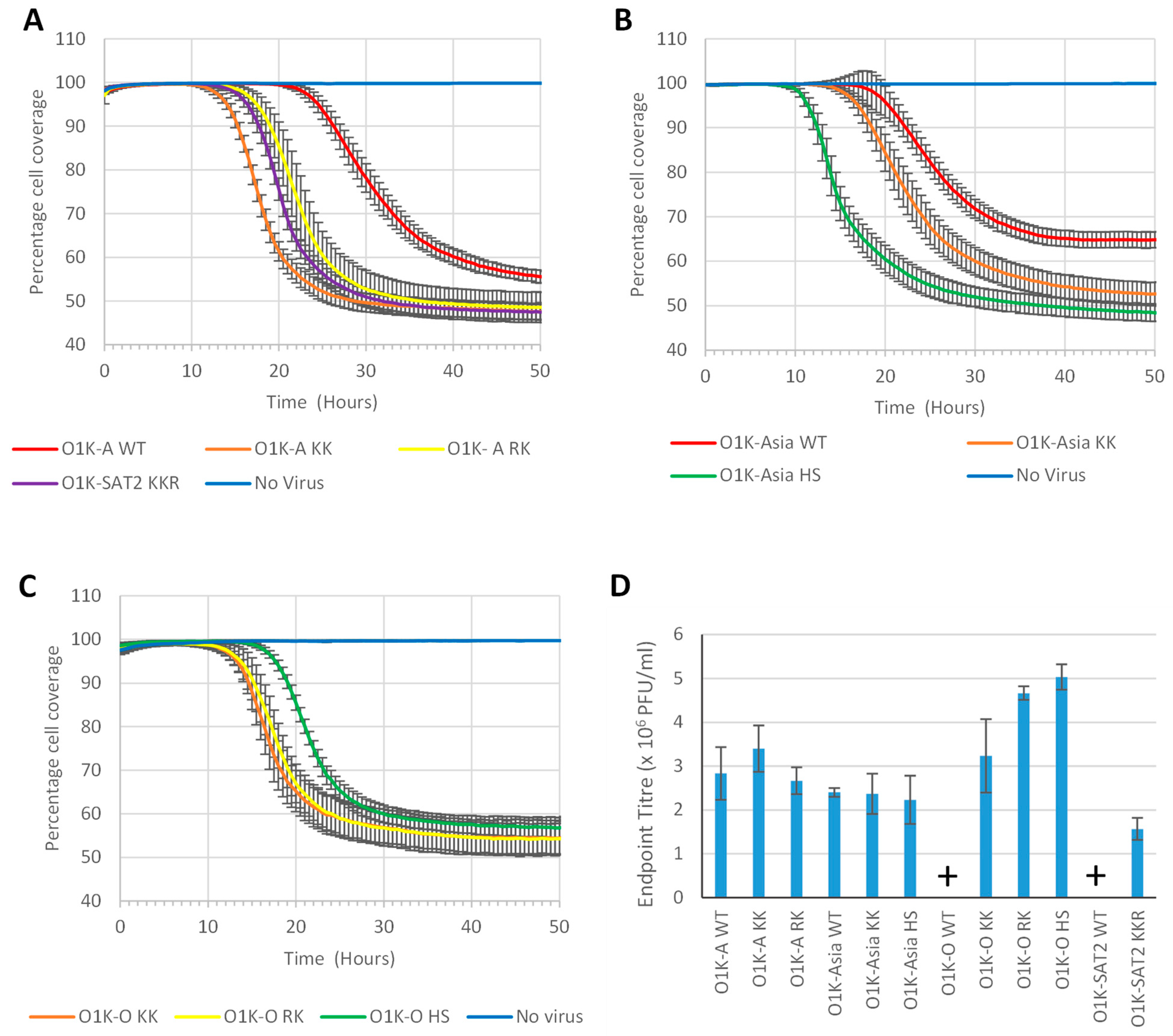
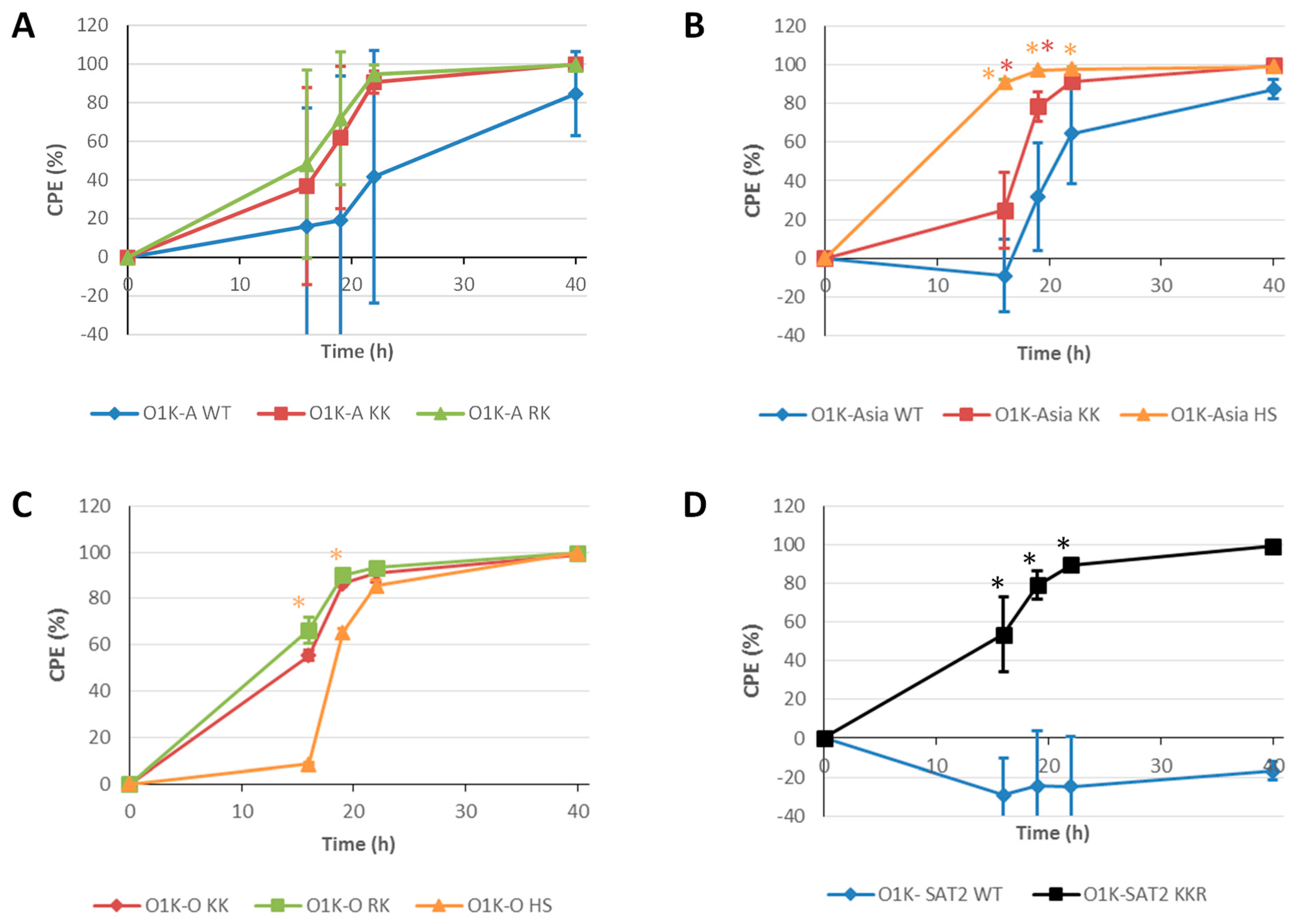
Importantly, the changes introduced at VP1 109–110 or 110–112 were stably maintained during cell passage for all of the recovered viruses. Furthermore, all of the recovered viruses with changes at these residues caused more rapid CPE in adherent BHK-21 cells than their corresponding parental virus, suggesting that they could spread more rapidly through the cell monolayer. However, despite causing more rapid CPE, the O1K-A KK, O1K-A RK, and O1K-Asia KK viruses only reached similar virus titres to their parental viruses (note: O1K-A WT and O1K-Asia WT could readily infect BHK-21 cells without capsid modifications). In contrast, the virus yields generated by O1K-O KK, O1K-O RK, and O1K-SAT2 KKR were dramatically increased over their parental viruses (O1K-O WT and O1K-SAT2 WT). Similar observations were made for suspension BHK-21 cells, as all of the recovered viruses with changes in VP1 (VP1 109–110 or 110–112) caused more rapid CPE than their corresponding parental virus (although this was less clear for O1K-A KK and O1K-A RK), and again, this was most dramatic for O1K-O KK, O1K-O RK, and O1K-SAT2 KKR. In line with similar virus growth in adherent BHK-21 cells, the yield of 146S intact virus particles was also similar between O1K-A KK, O1K-A RK, and O1K-Asia KK and their corresponding parental viruses (O1K-A WT and O1K-Asia WT). In contrast, and importantly for this study, in suspension BHK-21 cells, the O1K-O KK, O1K-O RK, and O1K-SAT2 KKR viruses generated significantly higher yields of intact 146S virus particles than their corresponding parental viruses. Thus, it appears that although the introduction of aa changes that allow for infection of BHK-21 cells can increase the rate of virus spread, for chimeric viruses with wt capsids (A-Turkey/2/2006 and Asia-1/Bar/9/2009) that can infect BHK-21 cells, this is not necessarily associated with concomitant increased virus yields or 146S particles. In contrast, for chimeric viruses with wt capsids (OUKG/35/2001 and SAT2/EGY/9/2012) that infect BHK-21 cells poorly, the introduction of such aa changes can greatly increase virus and 146S particle yield.
We also attempted to create a canonical HS binding site on each of the capsids selected for our study. As described above, for type O FMDV, the switch from non-HS binding to HS binding involves only a small number of aa changes in a shallow depression on the outer capsid surface. Thus, it was not surprising that the O1K-O HS virus could be recovered, as only two aa changes were required to generate the same aa sequence at the canonical HS binding site as O1BFS. The resulting virus (O1K-O HS) could infect CHO cells and caused more rapid CPE in both adherent and suspension BHK-21 cells than the parental O1K-O WT virus. However, for both cell systems, the rate of CPE was slightly slower than O1K-O KK and O1K-O RK. In addition, O1K-O HS generated greatly increased virus yields in adherent BHK-21 cells compared to O1K-O WT. Interestingly, despite causing CPE only slightly more slowly than O1K-O KK and O1K-O RK, the O1K-O HS virus gave a noticeably lower 146S yield in suspension BHK-21 cells. The identity of the receptor that is used by the O KK RK viruses to infect BHK-21 cells is yet to be identified, but it is highly likely that the HS virus uses HS receptors. Thus, it is possible that, as HS is abundantly expressed on the surfaces of most cells, the changes in the capsid may alter the propensity for the virion to remain cell associated upon cell lysis (i.e., CPE). Since the 146S yield in the suspension culture system was determined following vigorous clarification of the infected-cell lysates (to remove maximum cell debris), this could in part explain the reduced yield. It is also possible that the aa changes required to form a canonical HS binding site reduce virion stability. A study by Borca et al. [
53] showed that a matched pair of viruses (based on FMDV O
1 Campos) that differed only at VP3-56 (H or R) had similar growth kinetics in cell culture but concluded that the virus with R at VP3-56 was less temperature-stable than the virus with H at this position. However, our analysis suggests that the O1K-O HS virus (which has R at VP3-56) had a similar thermal stability to O1K-O WT (which has H at VP3-56), which suggests that different temperature sensitivities may not contribute to the lower 146S yields. A HS binding site has also been identified on the capsid of FMDV A1061. Therefore, we attempted to make a HS binding site on the chimeric virus with the capsid of A-Turkey/2/2006 by making four aa substitutions that created the same aa sequence at the HS binding site as A1061. However, for reasons that we do not yet understand, this was unsuccessful, as we could not recover a virus with these changes.
In contrast to type O and type A viruses, cell-culture-adapted Asia-1 and SAT2 viruses have not been observed with aa changes at the depression that forms the canonical HS binding site on O1BFS and A1061. This suggests that these serotypes do not have a natural propensity to generate a HS binding site at this location during cell culture adaptation. Nevertheless, we attempted to create a HS binding site on the O1K-Asia WT and O1K-SAT2 WT viruses. This involved making 7 and 10 aa changes in the capsid proteins, respectively. Given the large number of aa changes, we were not surprised to find that the O1K-SAT2 HS virus could not be rescued (including on BTY cells). In contrast, we were somewhat surprised to rescue the O1K-Asia HS virus. This virus induced rapid CPE in both adherent and suspension BHK-21 cells, which was considerably faster than for the O1K-Asia WT parental virus. Nevertheless, despite inducing faster CPE, the virus yield in adherent BHK-21 cells was not improved, and the yield of 146S particles from suspension BHK-21 cells was greatly reduced compared to O1K-Asia WT and the O1K-Asia KK variant. Thus, similarly to O1K-O HS, the yield of 146S particles was disappointing. We do not yet know the reasons for the poor yield of 146S particles but, as described above, it could be linked to an increased propensity to remain bound to abundant receptors on dead-cell membranes and/or reduced capsid stability. However, given that for O1K-Asia HS, the yield of 146S particles was extremely low, it is possible that capsid instability resulting from the introduced aa changes may provide a larger contribution to the reduced yield. Thus, our results show that increasing the rate of CPE in BHK-21 cells does not necessarily lead to an increased yield of the virus or 146S particles.
As mentioned above, full-genome sequencing indicated that all of the introduced aa changes were faithfully retained in the rescued viruses. However, for some of the rescued viruses, additional changes were observed. These mapped to the outer capsid surfaces and were located very close to the site of the introduced changes (see
Figure 1). Given that the additional changes are close to the site of the introduced changes, they could directly contribute to forming a receptor-binding site that allows the infection of BHK-21 cells. With this in mind, for the O1K-Asia HS virus, the additional changes were within or close to the canonical HS binding site (VP3 H84Q and VP2 E131K), and the changes (VP3 C7R) in O1K-A KK and O1K-Asia KK viruses would further increase the number of positively charged aa at the icosahedral 5-fold symmetry axes, which could strengthen interactions with negatively charged receptors, such as heparan sulphate (or other glycosaminoglycans). Alternatively, the additional changes could indirectly influence receptor interactions or serve as capsid-stability-restoring compensatory aa substitutions [
54] to offset possible reduced capsid stability that results from the introduced changes.
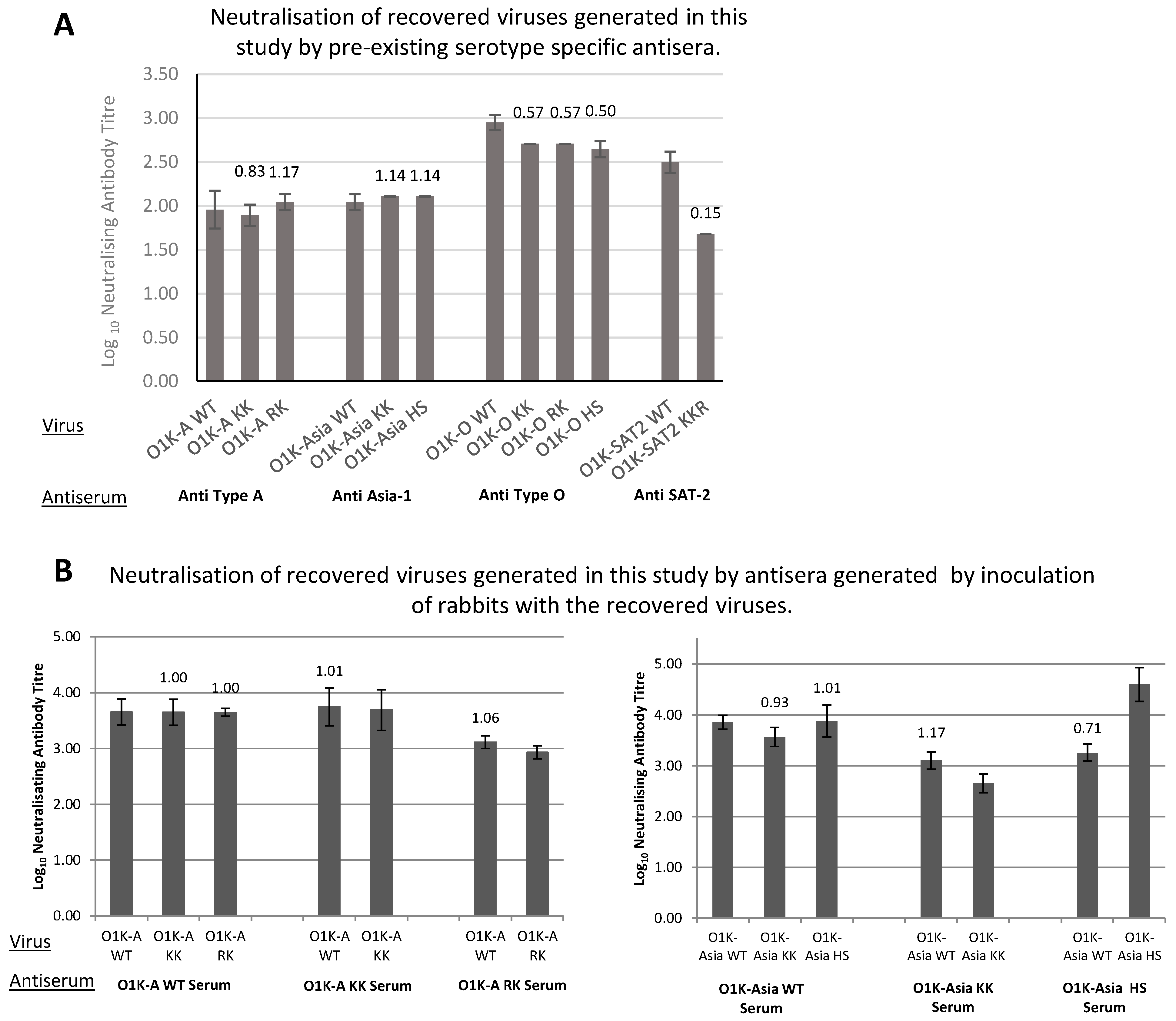
Importantly for vaccine efficacy, the antigenicity of most of the viruses with aa changes in the capsid was not adversely affected (
Figure 3). The only exception was the O1K-SAT-KKR virus, which had a significantly lower antibody neutralisation titre when compared to the parental virus with an unmodified capsid. However, these observations were made using an antiserum that was generated using a related tissue-culture-adapted SAT2 virus, so they do not necessarily mean that a vaccine generated using the O1K-SAT2 KKR virus would not be protective against the SAT2/EGY/9/2012 field virus. Furthermore, as the aa changes introduced in our study have been seen in SAT viruses that have been adapted for growth in BHK cells [
26], it is highly probable that they are present in existing vaccine viruses, which suggests that they may not adversely affect vaccine efficacy.
In summary, here we have reported a number of key findings that were obtained using chimeric viruses with capsids representative of the four most prevalent FMDV serotypes: (i) in general, chimeric viruses with capsids derived from FMDV field strains have the potential to be used in vaccine manufacture; (ii) making aa substitutions in the capsid proteins that are associated with cell culture adaptation can enhance the infection of suspension BHK cells, which are used for virus propagation for vaccine manufacture; (iii) for viruses with wt capsids (derived from field strains) that can infect BHK cells without the need for modification, the introduction of aa substitutions associated with cell culture adaptation can increase the rate of CPE in BHK suspension cells, but this is not always accompanied by an increased yield of 146S particles; and (iv) for viruses with wt capsids (derived from field strains) that poorly infect BHK cells, the introduction of aa substitutions associated with cell culture adaptation can dramatically increase the rate of CPE and yield of 146S particles in BHK suspension cells. In addition, our results show that viruses with aa substitutions that map to the icosahedral, 5-fold symmetry axes of the capsid give greater yields of 146S particles than viruses with aa substitutions at the depression that forms the canonical HS binding site. Surprisingly, this appears to also include type O FMDV, which preferentially acquires aa substitutions at the canonical HS binding site during cell culture adaptation.