Construction of a Full-Length Infectious Clone Derived from Type O Foot-and-Mouth Disease Virus Isolated in South Korea for Vaccine Development with High Antigen Productivity
Abstract
1. Introduction
2. Materials and Methods
2.1. Cells and Viruses
2.2. Cloning of Full-Length cDNA
2.3. Rescue of FMDV Through Transfection in Serial Cell Lines
2.4. Transmission Electron Microscopy
2.5. Virus Titration
2.6. Quantification of FMDV Particles
2.7. Animal Experiment
2.8. Virus Neutralization Test
2.9. Enzyme-Linked Immunosorbent Assay
2.10. Statistical Analysis
3. Results
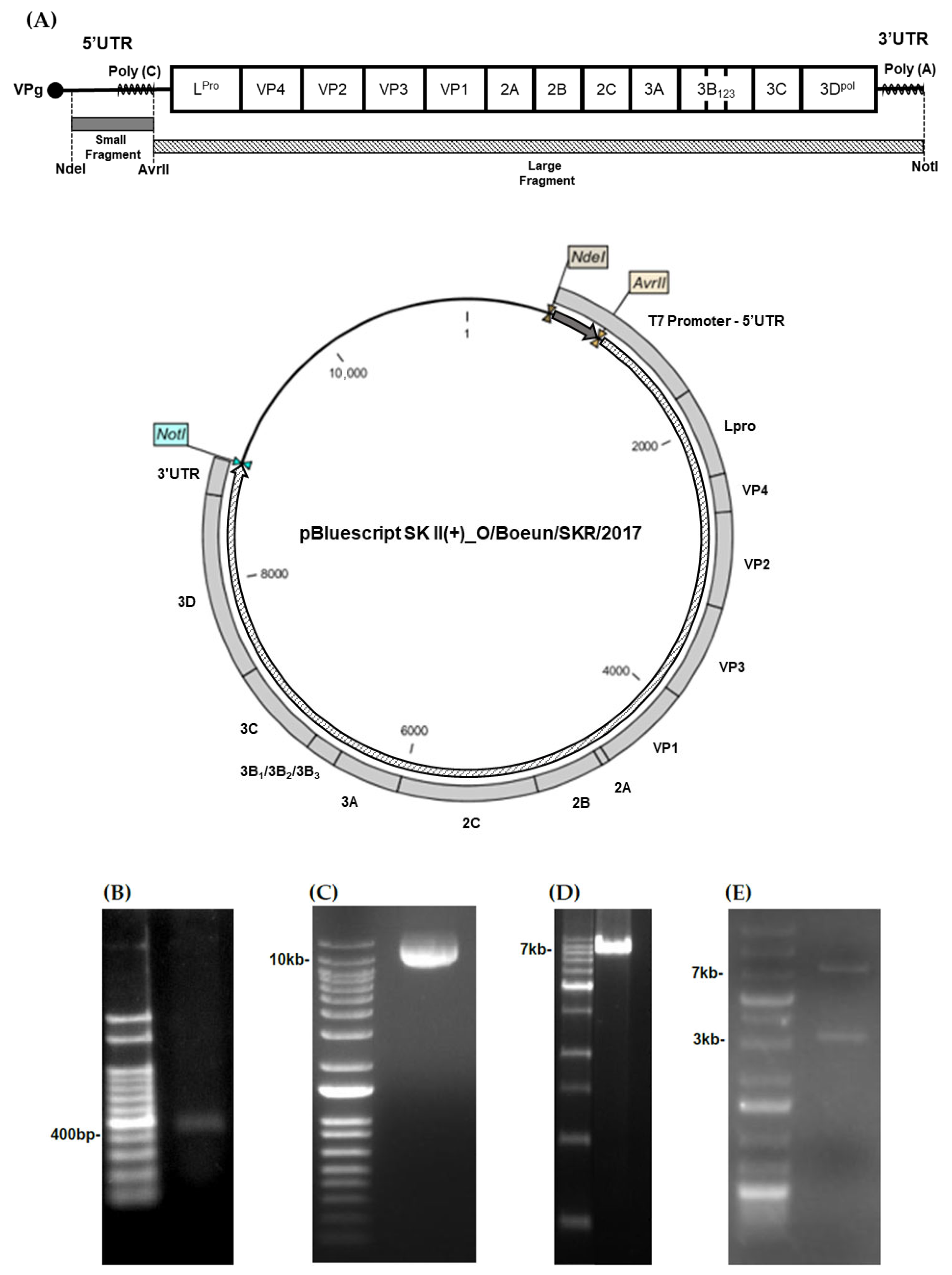
3.1. Construction of an Infectious Clone Derived from the Domestic FMDV
3.2. Rescue of Infectious FMDV from the cDNA Clone
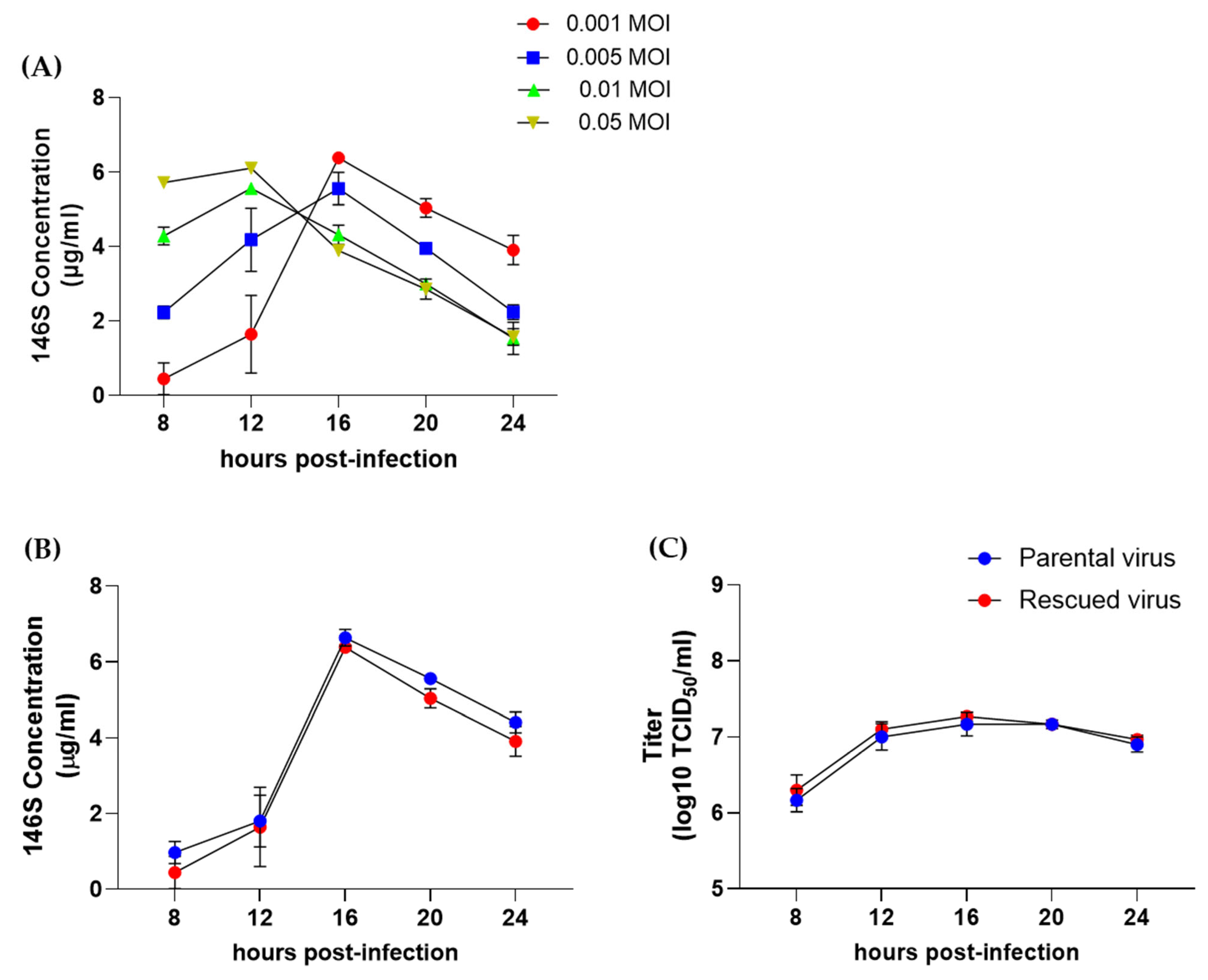
3.3. Antigen Production of the Rescued O/Boeun/SKR/2017 Virus
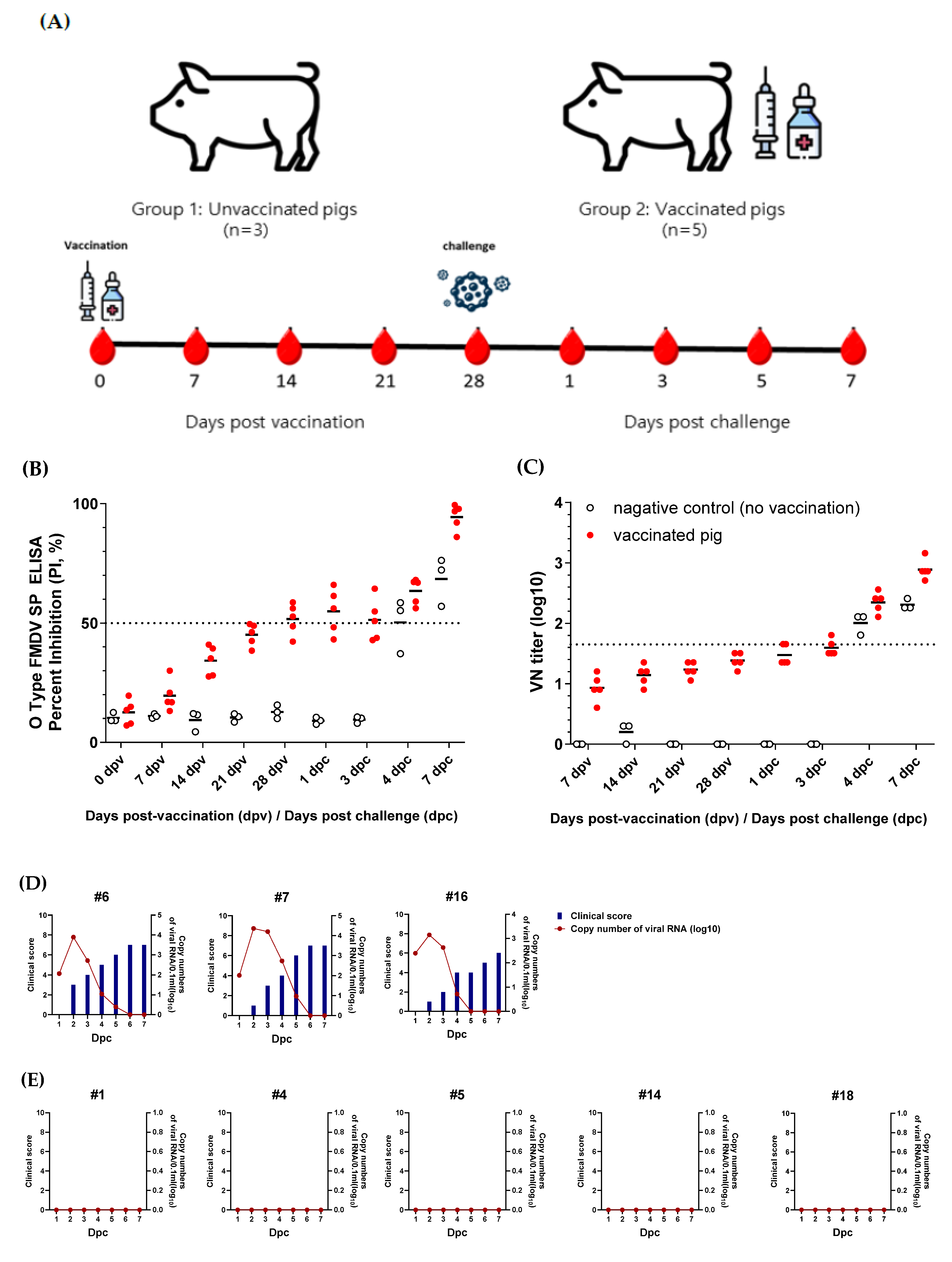
3.4. Evaluation of the Protective Efficacy of the Rescued O/Boeun/SKR/2017 Virus
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Arzt, J.; Baxt, B.; Grubman, M.; Jackson, T.; Juleff, N.; Rhyan, J.; Rieder, E.; Waters, R.; Rodriguez, L. The pathogenesis of foot-and-mouth disease II: Viral pathways in swine, small ruminants, and wildlife; myotropism, chronic syndromes, and molecular virus–host interactions. Transbound. Emerg. Dis. 2011, 58, 305–326. [Google Scholar] [CrossRef]
- Paton, D.J.; Gubbins, S.; King, D.P. Understanding the transmission of foot-and-mouth disease virus at different scales. Curr. Opin. Virol. 2018, 28, 85–91. [Google Scholar] [CrossRef]
- Yuan, H.; Li, P.; Bao, H.; Sun, P.; Bai, X.; Bai, Q.; Li, N.; Ma, X.; Cao, Y.; Fu, Y.; et al. Engineering viable foot-and-mouth disease viruses with increased acid stability facilitate the development of improved vaccines. Appl. Microbiol. Biotechnol. 2020, 104, 1683–1694. [Google Scholar] [CrossRef]
- Herod, M.R.; Loundras, E.-A.; Ward, J.C.; Tulloch, F.; Rowlands, D.J.; Stonehouse, N.J. Employing transposon mutagenesis to investigate foot-and-mouth disease virus replication. J. Gen. Virol. 2015, 96, 3507–3518. [Google Scholar] [CrossRef] [PubMed]
- Doel, T. FMD vaccines. Virus Res. 2003, 91, 81–99. [Google Scholar] [CrossRef] [PubMed]
- An, Q.; Lv, Y.; Li, Y.; Sun, Z.; Gao, X.; Wang, H. Global foot-and-mouth disease risk assessment based on multiple spatial analysis and ecological niche model. Vet. Q. 2025, 45, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Mohapatra, J.K.; Dahiya, S.S.; Subramaniam, S.; Rout, M.; Biswal, J.K.; Giri, P.; Nayak, V.; Singh, R.P. Emergence of a novel genetic lineage ‘A/ASIA/G-18/2019′ of foot and mouth disease virus serotype A in India: A challenge to reckon with. Virus Res. 2023, 333, 199140. [Google Scholar] [CrossRef]
- Bari, F.D.; Parida, S.; Tekleghiorghis, T.; Dekker, A.; Sangula, A.; Reeve, R.; Haydon, D.T.; Paton, D.J.; Mahapatra, M. Genetic and antigenic characterisation of serotype A FMD viruses from East Africa to select new vaccine strains. Vaccine 2014, 32, 5794–5800. [Google Scholar] [CrossRef]
- Rout, M.; Dahiya, S.S.; Subramaniam, S.; Acharya, R.; Samanta, R.; Biswal, J.K.; Mohapatra, J.K.; Singh, R.P. Complete coding region sequence analyses and antigenic characterization of emerging lineage G-IX of foot-and-mouth disease virus serotype Asia1. Vet. Q. 2024, 44, 1–10. [Google Scholar] [CrossRef]
- Di Nardo, A.; Shaw, A.E.; Gondard, M.; Wadsworth, J.; Girault, G.; Parekh, K.; Ludi, A.; Mioulet, V.; Bernelin-Cottet, C.; Hicks, H.M.; et al. Eastern Africa Origin of SAT2 Topotype XIV Foot-and-Mouth Disease Virus Outbreaks, Western Asia, 2023. Emerg. Infect. Dis. 2025, 31, 368. [Google Scholar] [CrossRef]
- Park, M.-Y.; Han, Y.J.; Choi, E.-J.; Kim, H.; Pervin, R.; Shin, W.; Kwon, D.; Kim, J.M.; Pyo, H.M. Post-vaccination monitoring to assess foot-and-mouth disease immunity at population level in Korea. Front. Vet. Sci. 2021, 8, 673820. [Google Scholar] [CrossRef]
- Habtewold, W.T.; Welde, N.; Kenubih, A.; Getahun, Y.A.; Abayneh, T.; Getachew, B.; Woldemedhin, W.; Tesfaye, Y.; Tesfaw, L.; Getachew, Y.; et al. Effects of binary ethyleneimine and formaldehyde inactivation methods on foot-and-mouth disease virus vaccine immune responses and kinetics. Sci. Rep. 2025, 15, 33788. [Google Scholar] [CrossRef] [PubMed]
- Hema, M.; Chandran, D.; Nagendrakumar, S.; Madhanmohan, M.; Srinivasan, V. Construction of an infectious cDNA clone of foot-and-mouth disease virus type O1BFS 1860 and its use in the preparation of candidate vaccine. J. Biosci. 2009, 34, 45–58. [Google Scholar] [CrossRef] [PubMed]
- Kärber, G. Beitrag zur kollektiven Behandlung pharmakologischer Reihenversuche. Naunyn-Schmiedebergs Arch. Exp. Pathol. Pharmakol. 1931, 162, 480–483. [Google Scholar] [CrossRef]
- Kim, A.-Y.; Park, S.Y.; Park, S.H.; Kim, J.Y.; Jin, J.S.; Kim, E.-S.; Park, J.-H.; Ko, Y.-J. Comparison of high-performance liquid chromatography with sucrose density gradient ultracentrifugation for the quantification of foot-and-mouth disease vaccine antigens. Vaccines 2022, 10, 667. [Google Scholar] [CrossRef]
- Kim, A.-Y.; Park, S.Y.; Park, S.H.; Jin, J.S.; Kim, E.-S.; Kim, J.Y.; Park, J.-H.; Ko, Y.-J. Validation of pretreatment methods for the in-process quantification of foot-and-mouth disease vaccine antigens. Vaccines 2021, 9, 1361. [Google Scholar] [CrossRef]
- Spitteler, M.A.; Romo, A.; Magi, N.; Seo, M.-G.; Yun, S.-J.; Barroumeres, F.; Régulier, E.G.; Bellinzoni, R. Validation of a high performance liquid chromatography method for quantitation of foot-and-mouth disease virus antigen in vaccines and vaccine manufacturing. Vaccine 2019, 37, 5288–5296. [Google Scholar] [CrossRef]
- Alves, M.; Guzylack-Piriou, L.; Juillard, V.; Audonnet, J.-C.; Doel, T.; Dawson, H.; Golde, W.; Gerber, H.; Peduto, N.; McCullough, K.; et al. Innate immune defenses induced by CpG do not promote vaccine-induced protection against foot-and-mouth disease virus in pigs. Clin. Vaccine Immunol. 2009, 16, 1151–1157. [Google Scholar] [CrossRef]
- WOAH. WOAH Terrestrial Manual 2022. In Foot and Mouth Disease (Infection with Foot and Motu Disease Virus); WOAH: Paris, France, 2022. [Google Scholar]
- Zheng, H.; Guo, J.; Jin, Y.; Yang, F.; He, J.; Lv, L.; Zhang, K.; Wu, Q.; Liu, X.; Cai, X. Engineering foot-and-mouth disease viruses with improved growth properties for vaccine development. PLoS ONE 2013, 8, e55228. [Google Scholar] [CrossRef]
- Nishi, T.; Onozato, H.; Ohashi, S.; Fukai, K.; Yamada, M.; Morioka, K.; Kanno, T. Construction and characterization of a full-length infectious cDNA clone of foot-and-mouth disease virus strain O/JPN/2010 isolated in Japan in 2010. Res. Vet. Sci. 2016, 106, 165–169. [Google Scholar] [CrossRef]
- Lian, K.; Yang, F.; Zhu, Z.; Cao, W.; Jin, Y.; Li, D.; Zhang, K.; Guo, J.; Zheng, H.; Liu, X. Recovery of infectious type Asia1 foot-and-mouth disease virus from suckling mice directly inoculated with an RNA polymerase I/II-driven unidirectional transcription plasmid. Virus Res. 2015, 208, 73–81. [Google Scholar] [CrossRef]
- Semkum, P.; Thangthamniyom, N.; Chankeeree, P.; Keawborisuth, C.; Theerawatanasirikul, S.; Lekcharoensuk, P. The application of the Gibson assembly method in the production of two pKLS3 vector-derived infectious clones of foot-and-mouth disease virus. Vaccines 2023, 11, 1111. [Google Scholar] [CrossRef]
- Chang, Y.; Zheng, H.; Shang, Y.; Jin, Y.; Wang, G.; Shen, X.; Liu, X. Recovery of infectious foot-and-mouth disease virus from full-length genomic cDNA clones using an RNA polymerase I system. Acta Biochim. Biophys. Sin. 2009, 41, 998–1007. [Google Scholar] [CrossRef] [PubMed]
- Zibert, A.; Maass, G.; Strebel, K.; Falk, M.; Beck, E. Infectious foot-and-mouth disease virus derived from a cloned full-length cDNA. J. Virol. 1990, 64, 2467–2473. [Google Scholar] [CrossRef] [PubMed]
- Van Rensburg, H.; Henry, T.; Mason, P. Studies of genetically defined chimeras of a European type A virus and a South African Territories type 2 virus reveal growth determinants for foot-and-mouth disease virus. J. Gen. Virol. 2004, 85, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Kim, R.-H.; Chu, J.-Q.; Park, J.-N.; Lee, S.-Y.; Lee, Y.-J.; Ko, M.-K.; Hwang, J.-H.; Lee, K.-N.; Kim, S.-M.; Tark, D.; et al. Antigenic properties and virulence of foot-and-mouth disease virus rescued from full-length cDNA clone of serotype O, typical vaccine strain. Clin. Exp. Vaccine Res. 2015, 4, 114–118. [Google Scholar] [CrossRef]
- Kotecha, A.; Seago, J.; Scott, K.; Burman, A.; Loureiro, S.; Ren, J.; Porta, C.; Ginn, H.M.; Jackson, T.; Perez-Martin, E.; et al. Structure-based energetics of protein interfaces guides foot-and-mouth disease virus vaccine design. Nat. Struct. Mol. Biol. 2015, 22, 788–794. [Google Scholar] [CrossRef]
- Barteling, S.; Meloen, R. A simple method for the quantification of 140 S particles of foot-and-mouth disease virus (FMDV). Arch. Gesamte Virusforsch. 1974, 45, 362–364. [Google Scholar] [CrossRef]
- Doel, T.; Chong, W. Comparative immunogenicity of 146S, 75S and 12S particles of foot-and-mouth disease virus. Arch. Virol. 1982, 73, 185–191. [Google Scholar] [CrossRef]
- Aarthi, D.; Rao, K.A.; Robinson, R.; Srinivasan, V. Validation of binary ethyleneimine (BEI) used as an inactivant for foot and mouth disease tissue culture vaccine. Biologicals 2004, 32, 153–156. [Google Scholar] [CrossRef]
- Van Rensburg, H.G.; Mason, P.W. Construction and Evaluation of a Recombinant Foot-and-Mouth Disease Virus: Implications for Inactivated Vaccine Production. Ann. N. Y. Acad. Sci. 2002, 969, 83–87. [Google Scholar] [CrossRef]
- Rweyemamu, M.; Umehara, O.; Giorgi, W.; Medeiros, R.; Lucca Neto, D.; Baltazar, M. Effect of formaldehyde and binary ethyleneimine (BEI) on the integrity of foot and mouth disease virus capsid. Rev. Sci. Tech. 1989, 8, 747–764. [Google Scholar] [CrossRef]
- Li, X.-R.; Yang, Y.-K.; Wang, R.-B.; An, F.-L.; Zhang, Y.-D.; Nie, J.-Q.; Ahamada, H.; Liu, X.-X.; Liu, C.-L.; Deng, Y.; et al. A scale-down model of 4000-L cell culture process for inactivated foot-and-mouth disease vaccine production. Vaccine 2019, 37, 6380–6389. [Google Scholar] [CrossRef]
- Dill, V.; Zimmer, A.; Beer, M.; Eschbaumer, M. Targeted modification of the foot-and-mouth disease virus genome for quick cell culture adaptation. Vaccines 2020, 8, 583. [Google Scholar] [CrossRef]
- Park, S.-H.; Lee, S.-Y.; Kim, J.-S.; Kim, A.-Y.; Park, S.-Y.; Lee, J.-H.; Lee, M.; Kim, H.; Lee, S.-I.; Kang, N.-Y.; et al. Scale-up production of type O and a foot-and-mouth disease bivalent vaccine and its protective efficacy in pigs. Vaccines 2021, 9, 586. [Google Scholar] [CrossRef] [PubMed]
- Dill, V.; Eschbaumer, M. Cell culture propagation of foot-and-mouth disease virus: Adaptive amino acid substitutions in structural proteins and their functional implications. Virus Genes 2020, 56, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Lee, S.-H.; Kim, H.-H.; Shin, S.-H.; Park, S.-H.; Park, J.-H.; Park, C.-K. An alternative serological measure for assessing foot-and-mouth disease vaccine efficacy against homologous and heterologous viral challenges in pigs. Vaccines 2024, 12, 10. [Google Scholar] [CrossRef] [PubMed]
- Hwang, J.-h.; Lee, K.-N.; Kim, S.-M.; Kim, H.; Park, S.-H.; Kim, D.-W.; Cho, G.; Lee, Y.-H.; Lee, J.-S.; Park, J.-H. Enhanced Effects of ISA 207 Adjuvant via Intradermal Route in Foot-and-Mouth Disease Vaccine for Pigs. Vaccines 2024, 12, 963. [Google Scholar] [CrossRef]
- Lee, G.; Hwang, J.-H.; Park, J.-H.; Lee, M.J.; Kim, B.; Kim, S.-M. Vaccine strain of O/ME-SA/Ind-2001e of foot-and-mouth disease virus provides high immunogenicity and broad antigenic coverage. Antivir. Res. 2020, 182, 104920. [Google Scholar] [CrossRef]
- Seago, J.; Jackson, T.; Doel, C.; Fry, E.; Stuart, D.; Harmsen, M.M.; Charleston, B.; Juleff, N. Characterization of epitope-tagged foot-and-mouth disease virus. J. Gen. Virol. 2012, 93, 2371–2381. [Google Scholar] [CrossRef]
- Biswal, J.K.; Bisht, P.; Subramaniam, S.; Ranjan, R.; Sharma, G.K.; Pattnaik, B. Engineering foot-and-mouth disease virus serotype O IND R2/1975 for one-step purification by immobilized metal affinity chromatography. Biologicals 2015, 43, 390–398. [Google Scholar] [CrossRef]
- Childs, K.; Juleff, N.; Moffat, K.; Seago, J. Demonstration of Co-Infection and Trans-Encapsidation of Viral RNA In Vitro Using Epitope-Tagged Foot-and-Mouth Disease Viruses. Viruses 2021, 13, 2433. [Google Scholar] [CrossRef]
- Park, J.-N.; Ko, M.-K.; Kim, R.-H.; Park, M.-E.; Lee, S.-Y.; Yoon, J.-E.; Choi, J.-H.; You, S.-H.; Park, J.-W.; Lee, K.-N.; et al. Construction of stabilized and tagged foot-and-mouth disease virus. J. Virol. Methods 2016, 237, 187–191. [Google Scholar] [CrossRef] [PubMed]
- Rai, D.K.; Diaz-San Segundo, F.; Schafer, E.; Burrage, T.G.; Rodriguez, L.L.; de Los Santos, T.; Hoeprich, P.D.; Rieder, E. Novel 6xHis tagged foot-and-mouth disease virus vaccine bound to nanolipoprotein adjuvant via metal ions provides antigenic distinction and effective protective immunity. Virology 2016, 495, 136–147. [Google Scholar] [CrossRef] [PubMed]
- Oem, J.K.; Chang, B.S.; Joo, H.D.; Yang, M.Y.; Kim, G.J.; Park, J.Y.; Ko, Y.J.; Kim, Y.J.; Park, J.H.; Joo, Y.S. Development of an epitope-blocking-enzyme-linked immunosorbent assay to differentiate between animals infected with and vaccinated against foot-and-mouth disease virus. J. Virol. Methods 2007, 142, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Fu, Y.; Lu, Z.; Li, P.; Cao, Y.; Sun, P.; Tian, M.; Wang, N.; Bao, H.; Bai, X.; Li, D.; et al. Development of a blocking ELISA based on a monoclonal antibody against a predominant epitope in non-structural protein 3B2 of foot-and-mouth disease virus for differentiating infected from vaccinated animals. PLoS ONE 2014, 9, e111737. [Google Scholar] [CrossRef]
- Choi, J.-H.; Ko, M.-K.; Shin, S.H.; You, S.-H.; Jo, H.-E.; Jo, H.; Lee, M.J.; Kim, S.-M.; Lee, J.-S.; Kim, B.; et al. Improved foot-and-mouth disease vaccine, O TWN-R, protects pigs against SEA topotype virus occurred in South Korea. Vet. Microbiol. 2019, 236, 108374. [Google Scholar] [CrossRef]
- You, S.-H.; Jo, H.-E.; Choi, J.-H.; Ko, M.-K.; Shin, S.H.; Lee, M.J.; Kim, S.-M.; Kim, B.; Park, J.-H. Evaluation of novel inactivated vaccine for type C foot-and-mouth disease in cattle and pigs. Vet. Microbiol. 2019, 234, 44–50. [Google Scholar] [CrossRef]
- Doel, T.; Baccarini, P. Thermal stability of foot-and-mouth disease virus. Arch. Virol. 1981, 70, 21–32. [Google Scholar] [CrossRef]
- Scott, K.A.; Kotecha, A.; Seago, J.; Ren, J.; Fry, E.E.; Stuart, D.I.; Charleston, B.; Maree, F.F. SAT2 foot-and-mouth disease virus structurally modified for increased thermostability. J. Virol. 2017, 91, e02312-16. [Google Scholar] [CrossRef]

| Region | Primer | Sequence (5′→3′) |
|---|---|---|
| Small fragment | Forward | GACCATATGTAATACGACTCACTATAGGGTTGAAAGGGGGCGTTAGGGT |
| Reverse | TTGCCTAGGGGGGGGGGGGGGGGGGGGTGAAAGGTGGGCTTC | |
| Large fragment | Forward | TTGCCTAGGTTTTCCGTCGTCCCCGACGT |
| Reverse | GACGCGGCCGCTCTAGAACTAGTTTTTTTTTTTTTTTTTTTGGAAGAGGAAGCGGGAA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.Y.; Park, S.Y.; Lee, G.; Park, S.H.; Jin, J.S.; Park, J.-H.; Ko, Y.-J. Construction of a Full-Length Infectious Clone Derived from Type O Foot-and-Mouth Disease Virus Isolated in South Korea for Vaccine Development with High Antigen Productivity. Vaccines 2025, 13, 1195. https://doi.org/10.3390/vaccines13121195
Kim JY, Park SY, Lee G, Park SH, Jin JS, Park J-H, Ko Y-J. Construction of a Full-Length Infectious Clone Derived from Type O Foot-and-Mouth Disease Virus Isolated in South Korea for Vaccine Development with High Antigen Productivity. Vaccines. 2025; 13(12):1195. https://doi.org/10.3390/vaccines13121195
Chicago/Turabian StyleKim, Jae Young, Sun Young Park, Gyeongmin Lee, Sang Hyun Park, Jong Sook Jin, Jong-Hyeon Park, and Young-Joon Ko. 2025. "Construction of a Full-Length Infectious Clone Derived from Type O Foot-and-Mouth Disease Virus Isolated in South Korea for Vaccine Development with High Antigen Productivity" Vaccines 13, no. 12: 1195. https://doi.org/10.3390/vaccines13121195
APA StyleKim, J. Y., Park, S. Y., Lee, G., Park, S. H., Jin, J. S., Park, J.-H., & Ko, Y.-J. (2025). Construction of a Full-Length Infectious Clone Derived from Type O Foot-and-Mouth Disease Virus Isolated in South Korea for Vaccine Development with High Antigen Productivity. Vaccines, 13(12), 1195. https://doi.org/10.3390/vaccines13121195





