1. Introduction
Vaccination is a transformative and cost-effective public health strategy, preventing an estimated 4.4 million deaths annually and significantly reducing the burden of vaccine-preventable diseases, particularly among children under five [
1]. Achieving herd immunity depends on high vaccine acceptance, defined as the willingness of individuals especially caregivers to adhere to recommended immunization schedules [
2,
3]. Each year, more than 20 million infants globally miss at least one dose of routine vaccines, and over 13 million remain “zero-dose” children, never having received any basic immunizations [
4]. These gaps result from both supply-side challenges, including poverty, remote locations, and insecurity, and demand-side barriers such as vaccine hesitancy, defined by WHO as the delay or refusal of vaccination despite availability [
5]. Hesitancy, driven by trust in vaccines, complacency, accessibility, is further exacerbated by misinformation, cultural beliefs, and systemic distrust [
5,
6,
7,
8,
9]. In Ethiopia, childhood immunization coverage is estimated to rise from 14.3% in 2000 to projections estimating 53.6% by 2025 (Projection) still far below the 90% target set by the Immunization Agenda 2030 (IA2030) [
10,
11]. National strategies such as the Expanded Program on Immunization (EPI) and the Health Extension Program (HEP) have improved access, particularly in rural areas, yet disparities persist among pastoralist, conflict-affected, and hard-to-reach populations [
12,
13]. Ethiopia’s Health Sector Transformation Plan II and EPI Multi-Year Plan prioritize universal access and community engagement, but challenges remain in addressing hesitancy and achieving equity [
14].
Gender plays a critical but underexplored role in immunization outcomes. In sub-Saharan Africa, including Ethiopia, women are typically the primary caregivers, responsible for managing children’s health, including vaccinations [
15]. Their knowledge and access to health services are vital, yet social norms, economic dependence, low decision-making autonomy, and domestic burdens often limit their ability to act [
16]. Conversely, men, who frequently control household finances and key decisions, have less direct involvement in child health services and are more susceptible to misinformation through peer networks and social media [
17]. Gender norms shape caregivers’ ability to act and limit autonomy, while also affecting health worker (both female and male) capacities and institutional frameworks. Both caregivers and female health extension workers face distinct gender-related barriers, from limited mobility and decision-making power to policy-level oversights that hinder uptake [
13,
18,
19].
Evidence highlighted that male involvement and spousal support enhance vaccine uptake, while reliance solely on maternal responsibility leads to missed or delayed immunizations [
20,
21,
22]. These dynamics are particularly relevant in Ethiopia, where vaccine hesitancy often manifests as delayed uptake rather than outright refusal, frequently due to competing caregiving demands [
23]. While maternal education and antenatal care attendance consistently correlate with higher vaccine uptake, male partner engagement and intra-household decision-making remain under-addressed in Ethiopian health policies [
12,
13,
24]. In response, global strategies such as WHO’s Immunization Agenda 2030 and the Behavioural and Social Drivers (BeSD) of Vaccination framework call for inclusive, equitable immunization systems. They emphasize gender-responsive programming that considers how gender norms influence vaccine access, confidence, and uptake [
11,
25]. Similarly, Gavi’s Gender Equality and Immunization Framework highlights the need to empower women while engaging men and dismantling structural barriers to under-vaccination [
26]. Despite growing recognition of gender’s influence, substantial evidence gaps persist in Ethiopia. Most national datasets lack gender-disaggregated insights into vaccine confidence, decision-making authority, and social support systems. Few studies explore how gender intersects with structural barriers such as geography, poverty, and conflict. Existing research often relies on self-reported data and fails to capture the emotional, cognitive, and contextual dimensions of vaccine behavior, limiting the development of gender-responsive interventions. While global frameworks like WHO’s Immunization Agenda 2030 and Gavi’s Gender Equality Framework emphasize gender-responsive programming, implementation in Ethiopia has primarily focused on maternal engagement, overlooking opportunities to involve men and address intra-household dynamics.
Therefore, this study aims to address these gaps by examining gender dynamics in vaccine hesitancy and acceptance among caregivers in four Ethiopian regions: Amhara, Oromia, Afar, and Tigray.
To better conceptualize the complex interplay between gender and vaccine behaviors, this study employs a gender-responsive adaptation of the WHO BeSD framework. This approach explicitly considers how gender norms, roles, and power dynamics influence cognitive, emotional, behavioral, and trust-related drivers of vaccine acceptance and hesitancy. This conceptualization guides both the quantitative and qualitative analyses, enabling a nuanced understanding of gendered vaccine dynamics in Ethiopia.
3. Results
3.1. Socio-Demographic Characteristics
Out of 980 caregivers surveyed (across Amhara, Oromia, Afar, and Tigray), 65.8% were aged 18–34, and 92.2% were married. Women constituted 65% of participants. Education levels varied: 18.9% were illiterate, 34.6% had primary education, and 24.3% had education beyond secondary school. About 71.8% of respondents were unemployed, and 54.6% identified as Muslim. The average household had three children, and about 62.7% of caregivers reported one child under five (see
Table 1).
3.2. Knowledge About Immunization
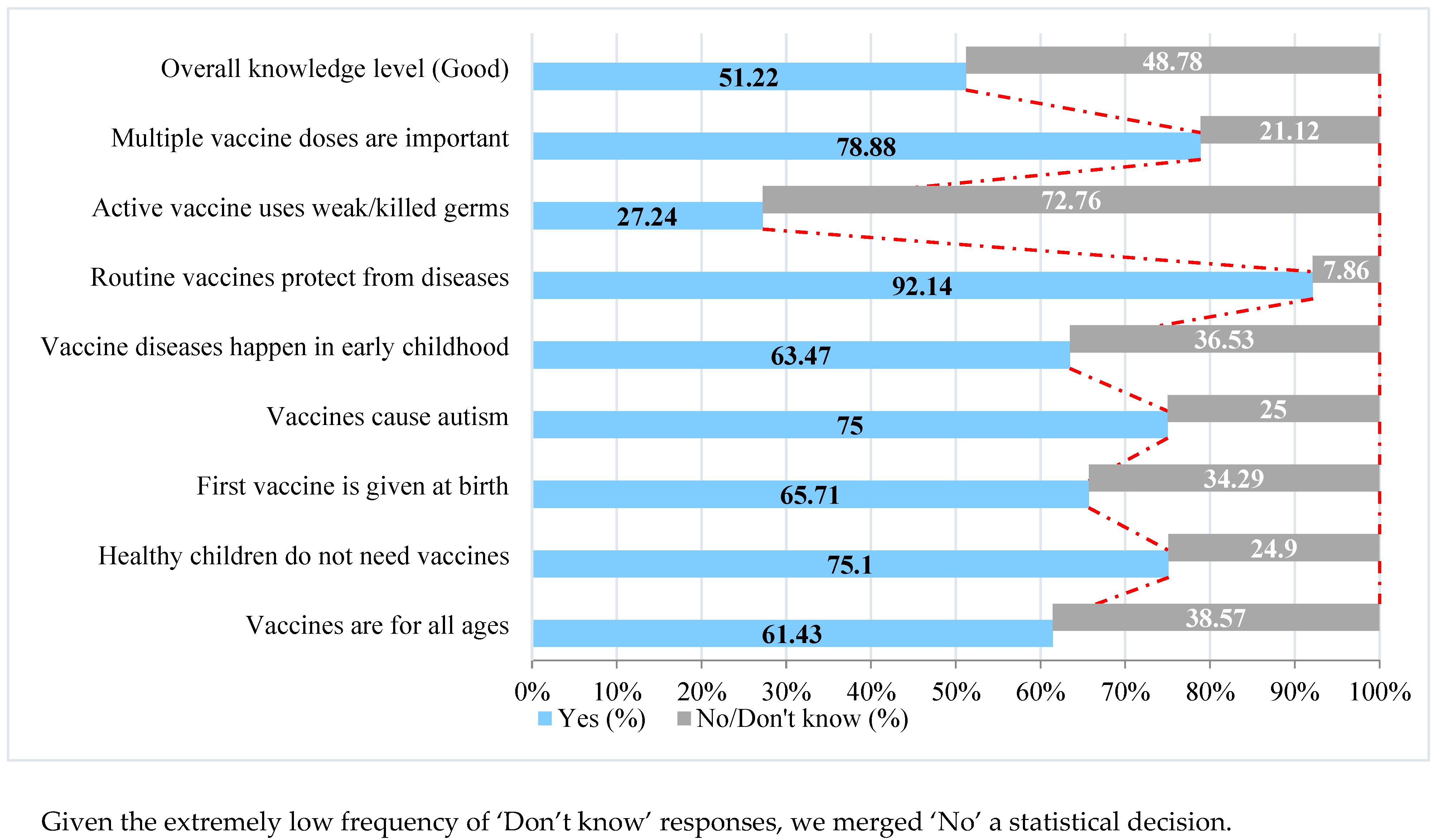
The mean vaccine knowledge score was 5.39 (out of eight) (±1.43), indicating moderate to good knowledge with 502 (51.2%) demonstrating good knowledge, 441 (45.0%) moderate, and 37 (3.8%) poor knowledge. Awareness was particularly high for statements affirming vaccine importance and safety (75.1% knew healthy children need vaccination; 75% rejected autism myths). Gender differences were minimal (
Figure 1).
3.3. Attitudes and Confidence Toward Immunization
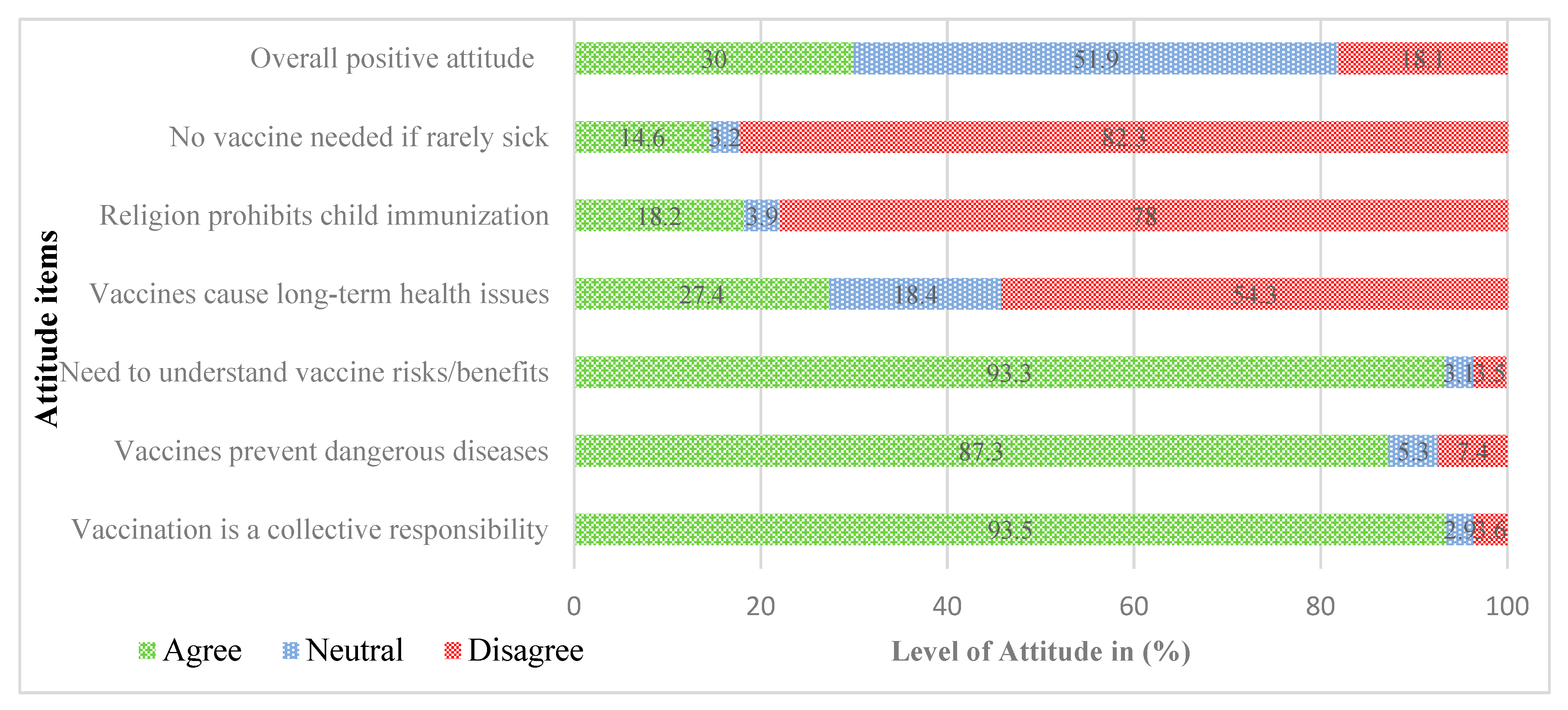
The study assessed attitudes toward vaccination using six key statements, with responses recorded on a five-point Likert scale. A total attitude score was then calculated by summing the coded responses across all statements and categorized into three levels (negative, neutral and positive attitude using a modified Bloom’s taxonomy framework (see operational definition part).
The results showed that about 30% expressed a positive attitude toward vaccines; 52% were neutral and 18% had a negative attitude toward vaccines. Female caregivers showed more favorable attitudes than male caregivers towards immunization. Neutrality was higher among males (58.3%) than females (48.5%). A strong majority agreed that vaccination is a collective responsibility (93.5%), prevents dangerous diseases (87.3%), and that understanding vaccine risks and benefits is essential (93.3%). Fewer respondents agreed that vaccines cause long-term health issues (27.4%), that religion prohibits child immunization18.2%) and that vaccination is unnecessary for rarely sick children (14.6%) (See
Figure 2).
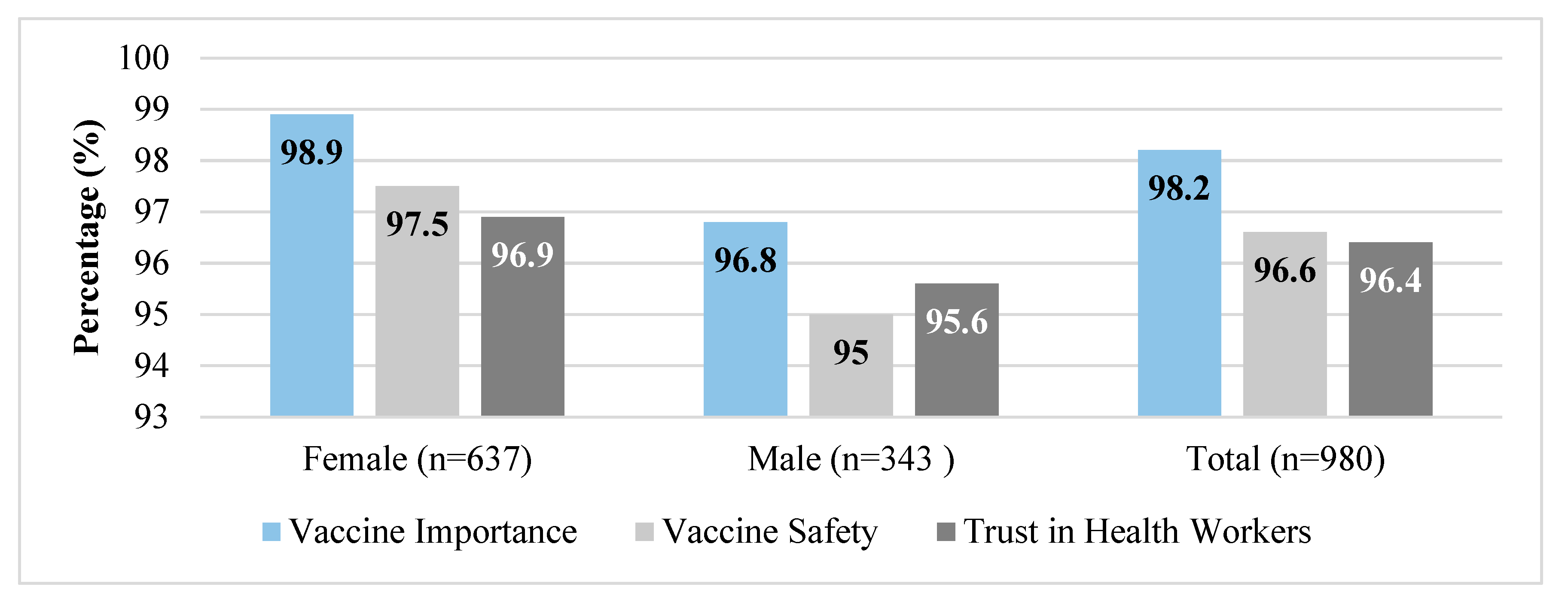
Vaccine confidence was found to be very high among the surveyed caregivers A vast majority (98.2%) believed vaccines are important, 96.6% considered them safe, and 96.4% trusted health workers. Disaggregated by sex, female caregivers consistently reported slightly higher confidence levels than males (see
Figure 3).
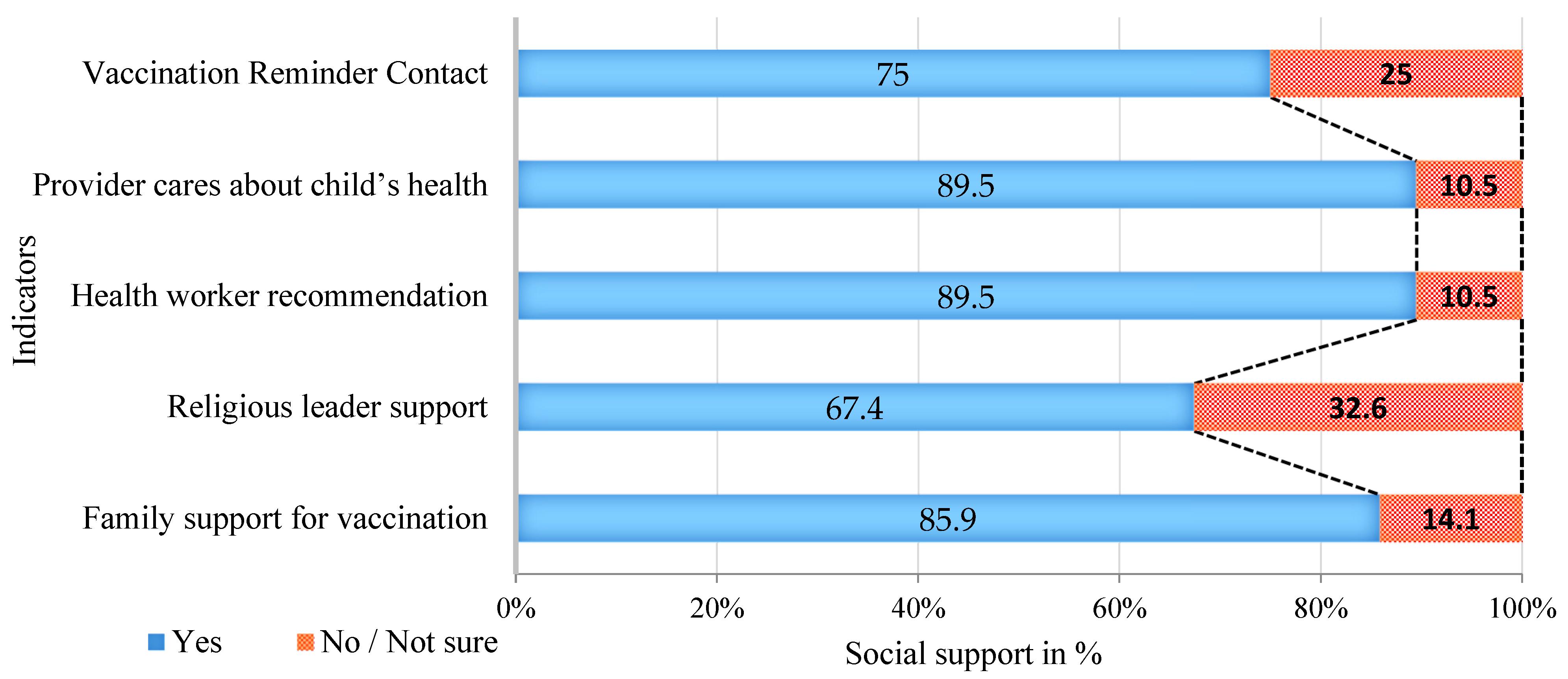
3.4. Social Support and Health System Engagement in Childhood Vaccination
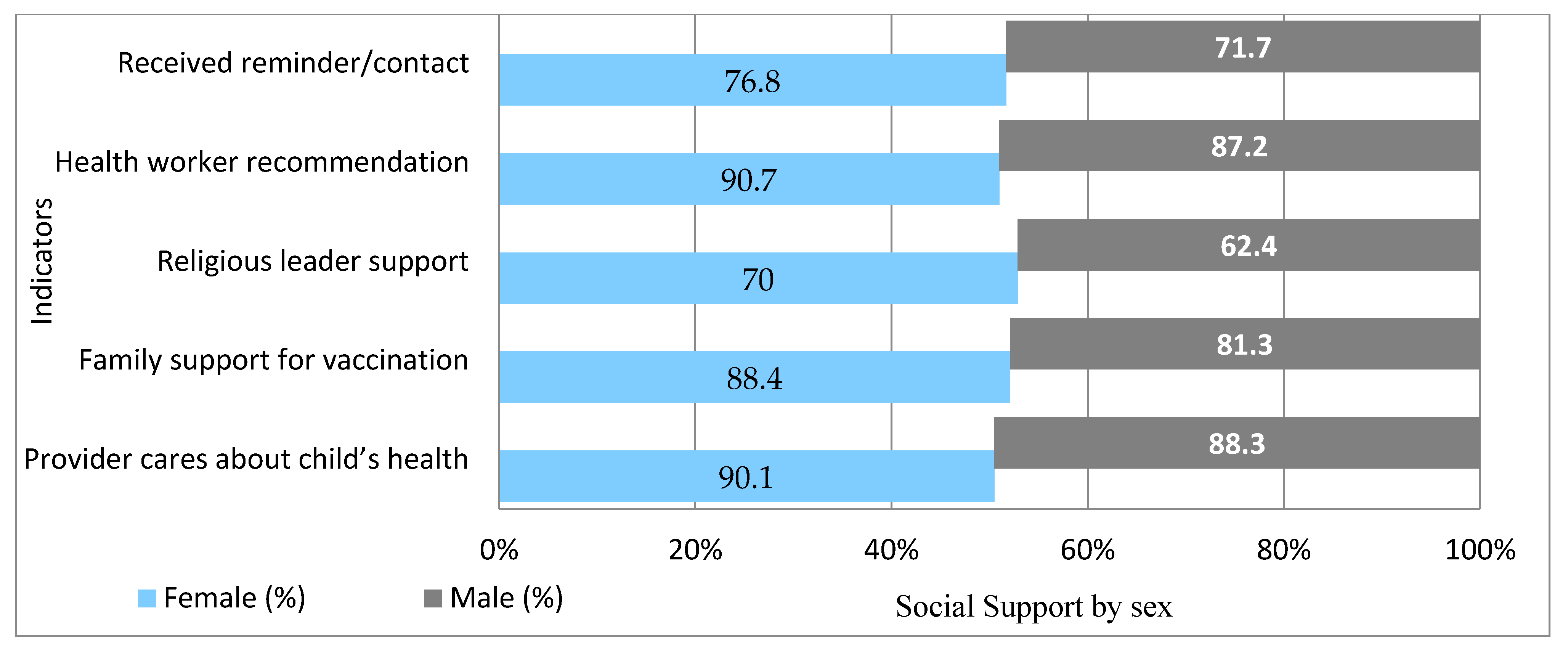
Strong support networks were evident: 86% received family support, 67.4% felt supported by religious leaders, and 89.5% received recommendations from health workers. Women consistently reported higher support across all domains. (See
Figure 4 and
Figure 5).
3.5. Gender Roles and Decision-Making
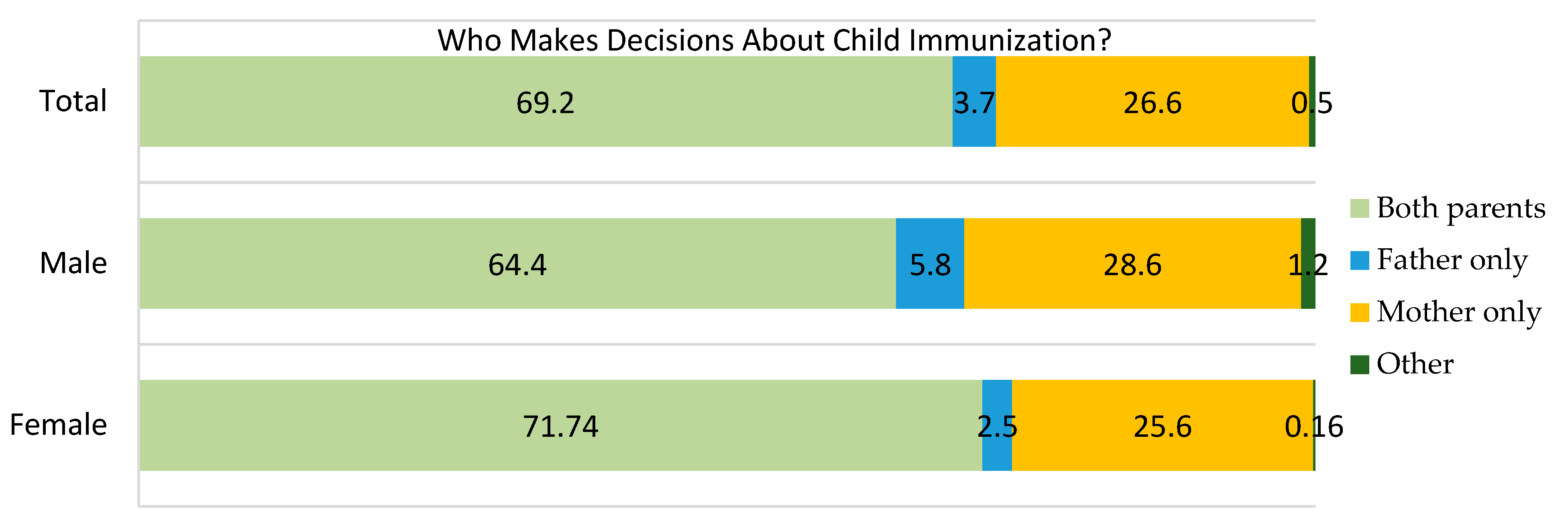
Although 678 (69.2%) reported joint decision-making for vaccination, a significant number (65.6%) still perceived immunization as the mother’s primary responsibility. Only 4.4% of households reported mothers solely deciding on finances, with a higher proportion among females (
n = 457, 71.7%) than males (
n = 221, 64.4%). A considerable percentage of males (
n = 98, (28.6%) and female (
n = 163, 25.6%) caregivers reported that immunization related issues are solely decided by mothers, suggesting skewed gender role in households (
Figure 6).
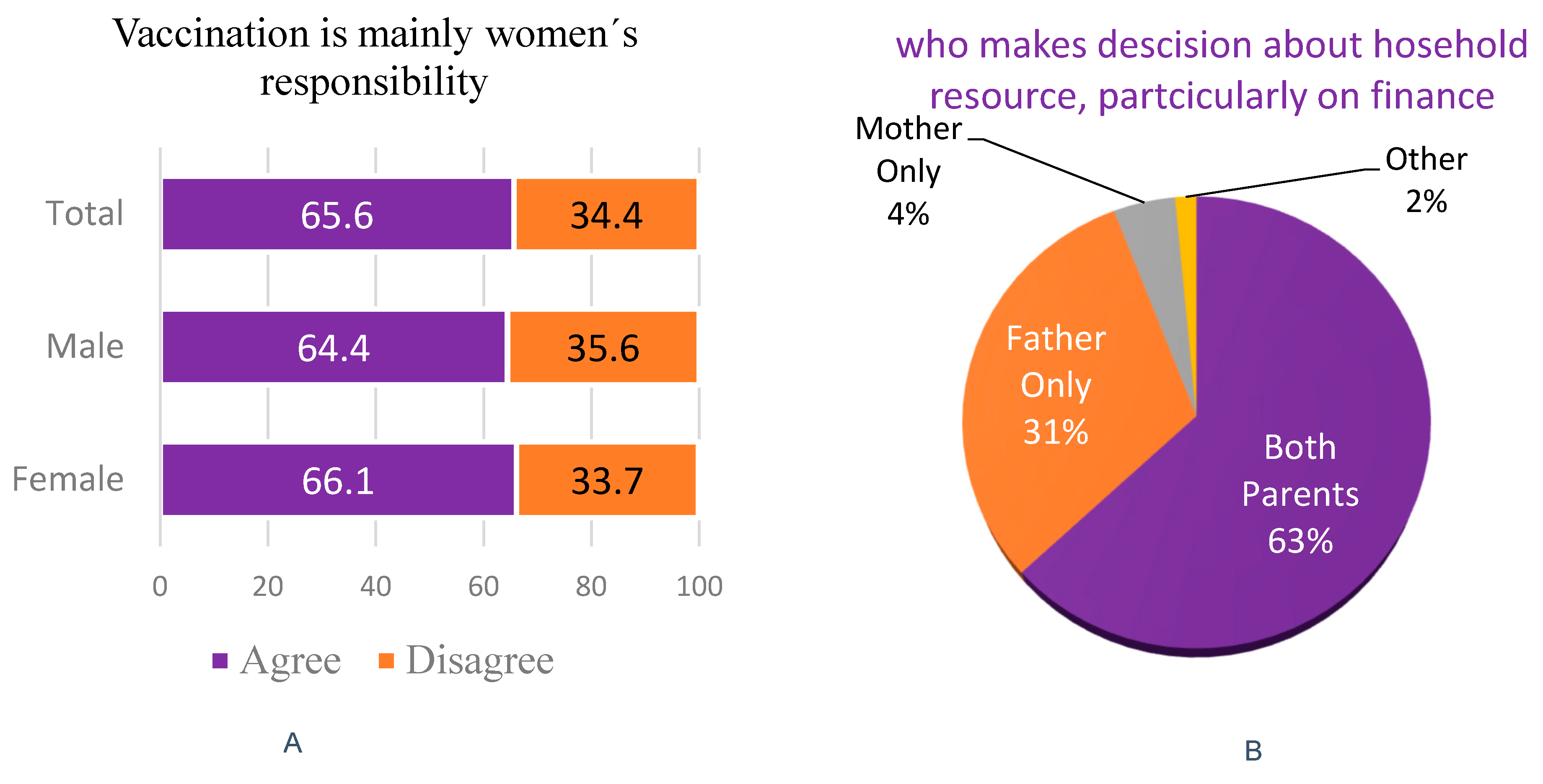
Two-thirds (65.6%) of caregivers stated that ensuring child vaccination is primarily the mother’s responsibility, with more females (
n = 432, 68.1%) than males (
n = 211, 61.5%) agreeing. This suggests limited male participation in the practical aspects of child health, despite their reported role in decision-making (
Figure 7A). Regarding household resource decisions, about 63.9% of caregivers indicated joint decision-making by both parents, similar among females (
n = 402, 63.1%) and males (
n = 224, 65.3%). Fathers alone made decisions in 31.0% of cases, while mothers were sole decision-makers in a minority (
n = 43, 4.4%) (
Figure 7B) of cases.
3.6. Access and Satisfaction with Vaccination Services
Most caregivers found vaccination services accessible and affordable, with over 95% reporting satisfaction. Barriers were minor but include vaccine stock-outs, delayed openings, and long wait (see
Table 2).
3.7. Vaccine Acceptance
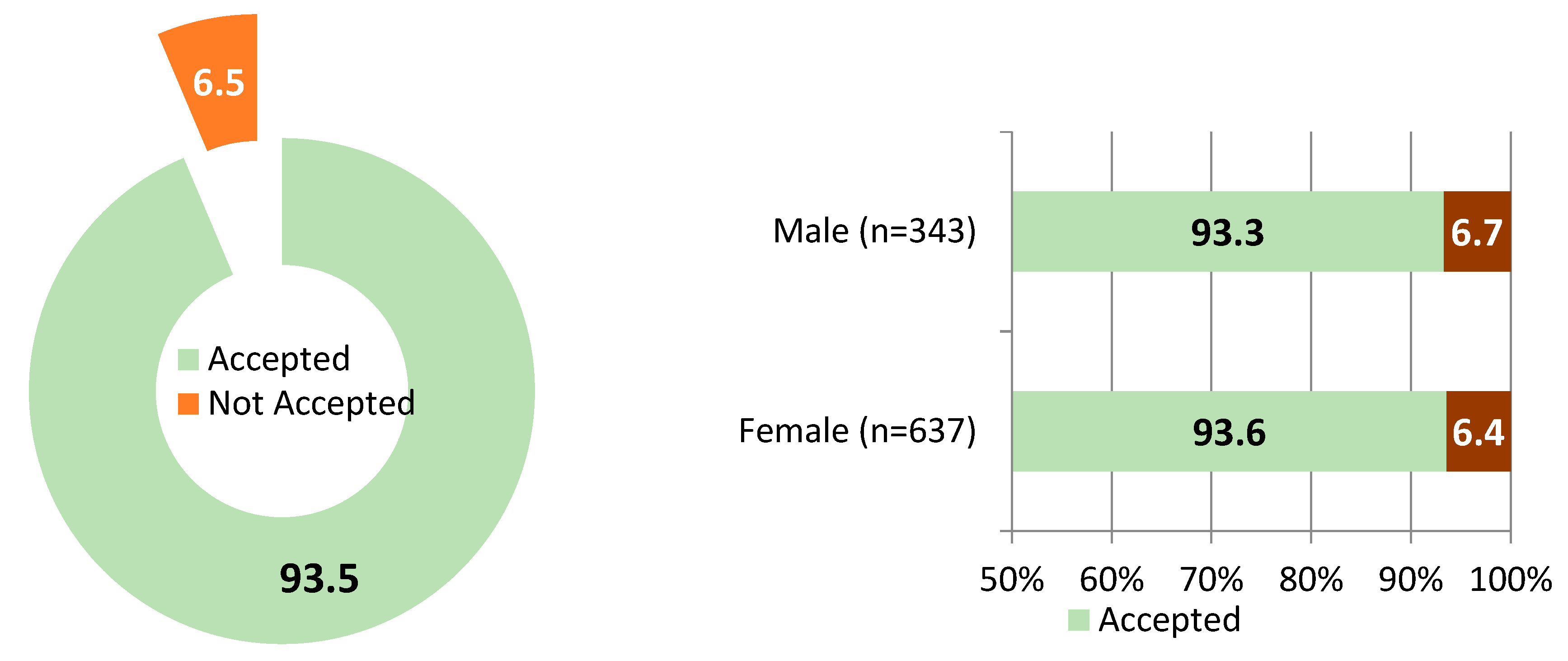
Acceptance was high at 93.5% (95% CI: 91.7–94.9%), with gender difference. Most non-accepting caregivers expressed intent to complete vaccination, indicating low outright refusal (
Figure 8).
Qualitative findings strongly reinforced these quantitative patterns, illustrating that the decision to vaccinate was deeply rooted in caregivers lived experiences and values. Across all four study regions, caregivers described vaccination not simply as a medical task but as a profound parental duty, often shaped by prior experiences with child illness or health improvements linked to immunization. In Oromia, one caregiver explained how her perception of vaccination was informed by the positive health outcomes observed in her children. One of the participants shared (P1):
“Since my first child was fully vaccinated, we rarely visit the health institution for sickness. That is why I never miss the appointments for the younger ones.”
This comment reflects a common view that immunization leads to fewer illnesses and reduced health care costs, reinforcing parental commitment to completing vaccine schedules.
Similarly, in Tigray, a mother described her unwavering determination:
Another participant shared (P2): “No matter how early or how far, I carry my child for every dose; it is on me to protect her.”
Such expressions of responsibility and agency were consistently reported, suggesting that vaccine acceptance is driven more by proactive health-seeking behavior than by compliance alone. This motivation extended even into areas affected by conflict. In Tigray, where health services had been interrupted, providers and caregivers made concerted efforts to resume immunization. One health worker shared (P3):
“After the war, we started zero dose of Penta in the form of campaign, and we have completed three doses now. The trend is backing to the right track.”
This example illustrates the resilience of both the community and health system, with vaccination quickly rebounding as a priority despite the disruption. For many, the ability to resume child immunization was a signal of recovery and hope.
3.8. Predictors of Vaccine Acceptance
Engagement with health workers was another important predictor. Caregivers who had recent contact with health professionals were twice as likely to vaccinate their children (AOR = 2.01; 95% CI: 1.07–3.76). Qualitative interviews highlighted that health providers not only delivered information but acted as mobilizers and facilitators, especially in pastoralist and remote communities. A health worker in Afar noted that pastoralist families often pause vaccinations during seasonal migration, requiring outreach teams to follow and provide services. This illustrates that missed vaccinations are often due to logistical barriers—such as distance, mobility, and system limitations—rather than outright refusal.
Despite high motivation levels, structural and contextual barriers persist in some of the study areas related to insecurity and conflict, particularly in Amhara and Tigray regions. A health official in Amhara explained that conflict disrupted service delivery, participant (P6) stating, “The primary obstacles are instability and conflicts… health services operate amid war and instability.” Infrastructure weaknesses further limited access; a health worker in Mille (Afar) described challenges in meeting demand with only one health center serving the entire town. Additionally, supply-side issues, such as vaccine shortages post-conflict, have eroded trust. A caregiver in Tigray expressed skepticism about vaccine quality following war-induced stockouts, participant (P4) saying, “After the war, the health institution ran out of vaccines; now I doubt the quality of the new supply.” These concerns underscore how historical disruptions continue to affect current perceptions of vaccine reliability and safety.
Quantitative analysis revealed several significant predictors of vaccine acceptance among caregivers. Educational attainment was a strong and consistent factor: individuals with primary (AOR = 0.48; 95% CI: 0.32–0.72), secondary (AOR = 0.33; 95% CI: 0.21–0.52), and above-secondary education (AOR = 0.47; 95% CI: 0.29–0.79) were significantly more likely to accept vaccination compared to those without formal education. This trend was supported by qualitative findings, where more educated parents demonstrated proactive health-seeking behaviors and a better understanding of vaccines’ preventive benefits.
Social and community support also emerged as powerful enablers. Caregivers who received support from family were 56% less likely to refuse vaccination (AOR = 0.44; 95% CI: 0.28–0.70), while those supported by religious leaders were 42% less likely (AOR = 0.58; 95% CI: 0.42–0.80). Interviews confirmed these associations; for instance, a religious leader in Amhara emphasized the harmony between faith and science, Participant (P7) stating, “We keep telling parents that science and faith agree vaccine save life; so, bring your children.” In Afar, community elders played a critical role in countering misinformation, with one elder noting efforts to correct misconceptions among young fathers who feared vaccines might weaken boys. These testimonies highlight how trusted local figures, religious and cultural, have been instrumental in sustaining community-wide vaccine confidence and combating misinformation.
Engagement with health workers was another important predictor. Caregivers who had recent contact with health professionals were twice as likely to vaccinate their children (AOR = 2.01; 95% CI: 1.07–3.76). Qualitative interviews highlighted that health providers not only delivered information but acted as mobilizers and facilitators, especially in pastoralist and remote communities. A health worker in Afar noted that pastoralist families often paused vaccinations during seasonal migration, requiring outreach teams to follow and provide services. This illustrates that missed vaccinations are often due to logistical barriers—such as distance, mobility, and system limitations—rather than outright refusal.
A caregiver in Tigray expressed skepticism about vaccine quality following war-induced stockouts, participant (P4) saying, “After the war, the health institution ran out of vaccines; now I doubt the quality of the new supply.” The accompanying multivariable logistic regression analysis (
Table 3) quantifies these associations and supports the qualitative insights. Statistically significant factors include higher education levels, family and religious support, and health worker contact, all of which positively correlate with vaccine acceptance. Conversely, factors like marital status, knowing where to immunize, and gender-related attitudes showed less definitive associations. These results emphasize the multifaceted nature of vaccine acceptance, shaped by educational, social, and systemic influences.
3.9. Vaccine Hesitancy: Composite Index
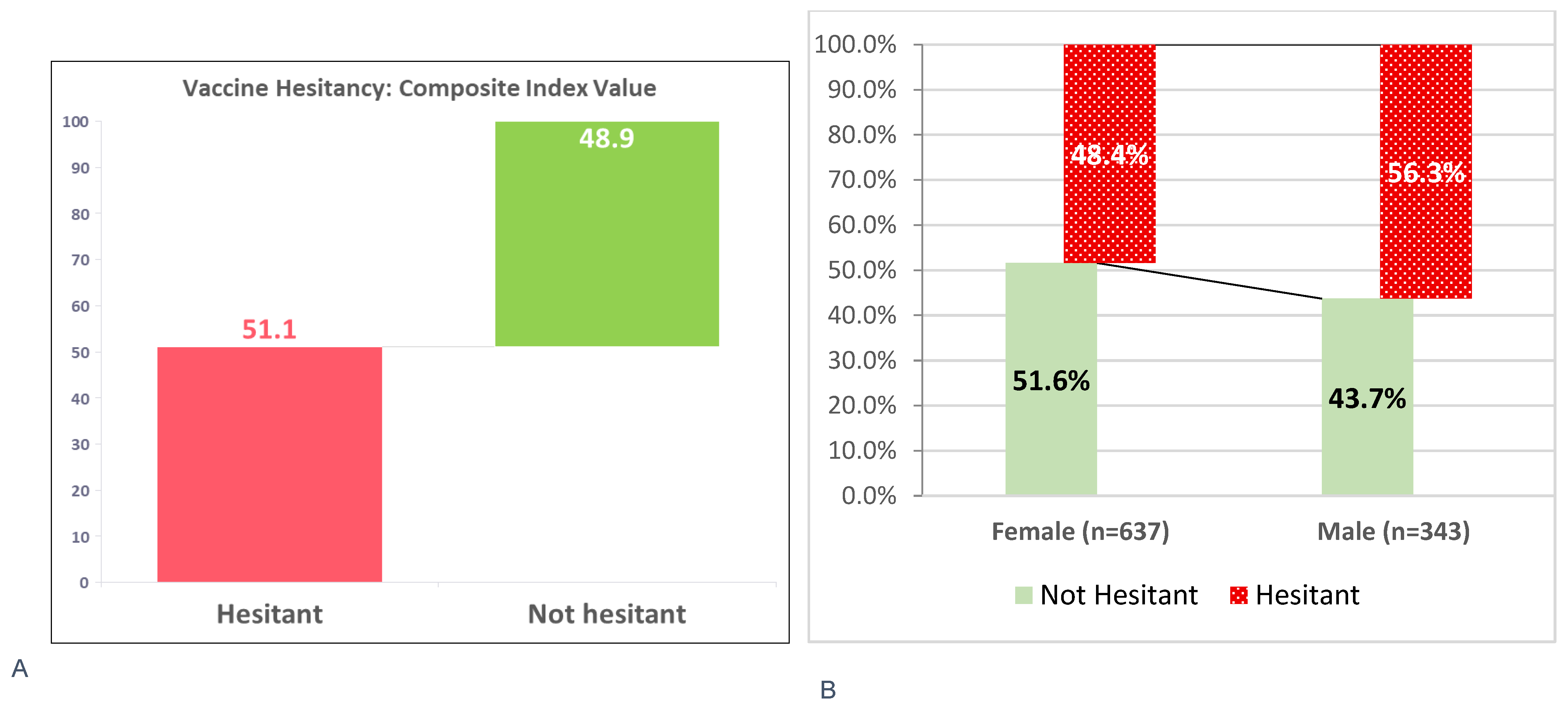
The composite index of vaccine hesitancy revealed that 501 caregivers (51.1%; 95% CI: 47.99–54.25%) were hesitant, with higher rates among males (56.3%) than females (48.4%). Conversely, 479 caregivers (48.9%) were not hesitant, including more females (51.6%) than males (43.7%) (see
Figure 9). However, when asked directly, 765 caregivers (78.1%) denied any hesitancy, suggesting a disconnect between perceived and actual hesitancy—possibly due to limited awareness or social desirability bias. Many caregivers equate hesitancy only with outright refusal, overlooking doubts or delays.
Health workers reported low hesitancy toward familiar vaccines like measles and polio, seen as routine and trusted. As one EPI officer in Oromia noted, “People trust them.” In Amhara, a health provider remarked that rapid deployment led many to believe the vaccine lacked sufficient testing. Conflict-affected areas like Tigray saw added layers of distrust, where caregivers questioned the origin and safety of vaccines distributed amid political instability. As one provider explained (P8), “Some parents doubt the safety… They ask where the vaccine came from and hesitate even though we explain it is safe.”
These findings underscore the nuanced nature of vaccine hesitancy: often less about refusal and more about uncertainty, shaped by familiarity, context, and trust in systems.
These narratives illustrate the complexity behind the composite hesitancy index, where caregivers may be categorized as hesitant due to doubts or delayed uptake even when direct questioning finds no outright refusal.
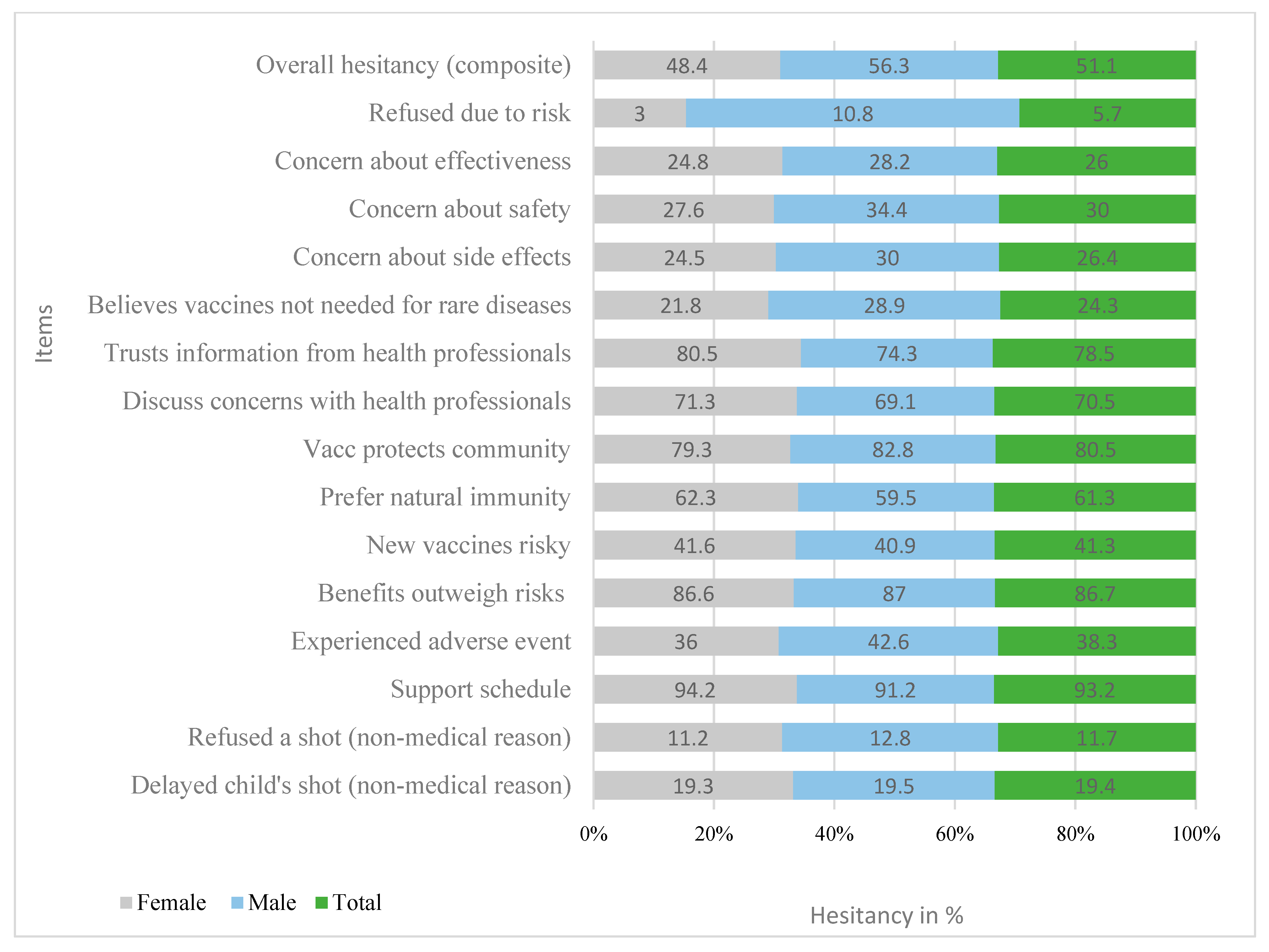
Of the 980 caregivers surveyed, 501 (51.1%) showed some level of vaccine hesitancy. Specifically, 190 (19.4%) delayed vaccination—similar across genders—and 115 (11.7%) reported outright refusal. Despite this, the majority (93.2%) supported the recommended immunization schedule, and 86.7% believed the benefits of vaccines outweigh the risks. However, 38.3% reported adverse events, and safety concerns persisted: 18% were somewhat concerned and 8.5% very concerned about side effects. Notably, 41.3% felt new vaccines were riskier, and 29.7% preferred natural immunity. Trust remained relatively high—78.5% trusted health professionals and 70.5% felt comfortable discussing concerns—while 87.8% agreed vaccination helps protect others. Still, 24.3% believed vaccines were unnecessary for rare diseases, and 5.7% reported refusing vaccines specifically due to safety fears, with male caregivers reporting higher rates of concern-driven refusal (See
Figure 10).
3.10. Predictors of Vaccine Hesitancy
Multivariable analysis identified five key factors significantly associated with vaccine hesitancy. Agreement with traditional gender norms—specifically, the belief that vaccination is solely a woman’s responsibility—increased hesitancy by 69% (AOR = 1.69; 95% CI: 1.25–2.28; p = 0.001). Qualitative data showed that while many mothers internalized this duty and felt a strong sense of personal responsibility, the lack of shared support from partners or family often led to delays or missed appointments, particularly in rural and pastoralist communities. One caregiver in Amhara expressed, “Vaccination is part of what I must do as a mother… I want the same [health] for my baby.”
Education had a protective effect: caregivers with secondary education were 47% less likely to be hesitant (AOR = 0.53; 95% CI: 0.31–0.90; p = 0.019). However, qualitative insights revealed that a minority of formally educated individuals, particularly in Amhara and Oromia, were more vocal in spreading vaccine misinformation—such as conspiracy theories involving microchips or infertility—underscoring that partial or misapplied knowledge can also contribute to hesitancy. As one provider in Oromia noted, “Some educated people were the ones spreading rumours.”
Urban residence was linked to a 62% increase in hesitancy (AOR = 1.62; 95% CI: 1.21–2.16; p = 0.001). Caregivers in urban areas were more exposed to misinformation through social media and informal networks, leading to doubts about vaccine safety and campaign motives. In contrast, rural communities showed higher trust in health workers and lower exposure to misinformation. A provider in Amhara shared, “In town, there were people saying the COVID vaccine has a chip or causes infertility.”
Employment status also influenced hesitancy. Unemployed caregivers had 41% lower odds of hesitancy (AOR = 0.59; 95% CI: 0.40–0.88;
p = 0.009). (see
Table 4) Employed individuals often faced scheduling conflicts, especially when male household members were unavailable to assist with transport or decision-making. In regions like Afar and Oromia, such logistical barriers were compounded in pastoralist or migratory households. Qualitative data linked this to time constraints and rigid work schedules, limiting their participation in immunization activities. In addition, employed caregivers are more exposed to rumors and misinformation via social media and peer networks, fostering fears about vaccine safety and mistrust.
Conversely, social support emerged as a strong protective factor. Family encouragement reduced hesitancy by 75% (AOR = 0.25; 95% CI: 0.09–0.71;
p = 0.009), and support from religious leaders lowered it by 50% (AOR = 0.50; 95% CI: 0.36–0.71;
p < 0.001) (see
Table 4). Health providers in Afar and Tigray emphasized the role of religious and community leaders in dispelling myths and fostering trust, particularly during immunization campaigns. Family members, especially spouses and mothers-in-law, were also crucial in building caregiver confidence. In areas affected by recent outbreaks or vaccine-preventable deaths, shared grief catalyzed stronger vaccine demand, as one official in Afar noted: “When families lose a child to measles, it changes everything.”
No statistically significant differences were found across regions in relation to vaccine acceptance; therefore, results are presented without regional stratification.
Overall, the findings highlight that while education and social support can reduce hesitancy, structural barriers, traditional gender roles, and misinformation—particularly in urban and employed populations—remain key challenges. These insights suggest targeted strategies for increasing vaccine confidence, including gender-inclusive outreach, support mobilization, and countering misinformation in urban settings.
4. Discussion
This mixed-methods study investigated gender differences in vaccine acceptance and hesitancy among 980 caregivers across four Ethiopian regions. The findings reveal how gender intersects with social, cultural, and health system factors to shape immunization behaviors. Although overall vaccine acceptance was high, underlying hesitancy patterns showed distinct gendered attitudes and decision-making roles, highlighting the urgent need for gender-sensitive approaches to improve vaccine equity.
The study confirmed a remarkably high overall vaccine acceptance rate of 93.5%, with similar levels among female (93.6%) and male (93.3%) caregivers. This aligns with regional and global findings: a study in Addis Ababa, Ethiopia reported 96% caregiver acceptance [
23], while research from Rwanda and Uganda also highlights strong maternal trust and motivation toward immunization [
21,
33,
34]. A systematic review of 42 studies across Africa further supports this, showing widespread caregiver willingness despite structural barriers [
16]. These findings corroborate the strong caregiver acceptance rates reported in our study. These findings reflect Ethiopia’s robust primary health care system, strong community trust in health workers, and effective communication through the Health Extension Program. Confidence in vaccine importance (98.2%), safety (96.6%), and trust in health workers (96.4%) was also notably high, reinforcing a strong immunization culture. However, qualitative insights revealed key gender dynamics: women took proactive responsibility for childhood immunization, while men were more passive, consistent with patterns observed in Nigeria and Uganda [
21,
35]. These gendered roles suggest that maternal engagement is central to vaccine uptake, but greater male involvement may require targeted strategies.
Building on these high levels of acceptance, the study further explored key predictors that shape caregivers’ decisions to vaccinate. One of the strongest factors identified was educational attainment. Caregivers with primary, secondary, or higher education were more likely to vaccinate their children. This aligns with evidence from various African contexts, where education enhances health literacy and informed decision-making [
33,
36,
37,
38]. However, studies also show that strong community engagement, such as outreach by health workers, can significantly improve vaccination uptake even among caregivers with little or no formal education, demonstrating the capacity of community health systems to overcome literacy-related barriers [
39].
A gendered pattern also emerged in relation to education: educated mothers actively sought vaccination services, while educated fathers often played passive roles or, in some cases, contributed to misinformation. This highlights that education alone is not enough and must be paired with gender-sensitive health communication. Caregivers who received encouragement from family members or religious leaders were more likely to vaccinate their children. Women reported higher levels of such support than men, reflecting gender norms around caregiving roles. This finding aligns with studies from Nigeria and Uganda, where community and faith-based networks have been shown to shape health-seeking behaviors and support maternal roles in child immunization. For example, in Uganda, Babirye et al. (2011) found that mothers, as primary decision-makers for immunization, were strongly influenced by community encouragement [
21]. In Nigeria, Oku et al. (2017) demonstrated that engaging religious leaders in communication strategies enhanced vaccine uptake [
40]. Melillo et al. (2022) further confirmed that in many low- and middle-income countries, trusted religious actors help expand immunization coverage by building trust and addressing community concerns [
41].
Qualitative findings from this study also pointed to the influence of male-led community groups in dispelling harmful beliefs, such as the notion that vaccines weaken boys. However, men’s limited engagement in these networks remains a missed opportunity for outreach. At the same time, the literature cautions that religious and community platforms can also spread misinformation when not guided by accurate information. Building on these insights, another strong predictor of vaccine acceptance was caregivers’ recent contact with health providers. Those who had been contacted or visited by health workers were twice as likely to vaccinate their children. Female caregivers reported more frequent contact, reflecting their routine engagement in maternal and child health services. Similar gendered patterns have been observed in qualitative findings in Afar regions, where health posts are often perceived as female spaces, limiting men’s involvement. Additionally, the qualitative data reinforced the critical role of health workers, especially in pastoralist areas where outreach compensates for seasonal migration. However, inconsistent communication and impersonality during the COVID-19 pandemic undermined trust and reduced immunization uptake. House-to-house visits were effective only when health workers were trusted and culturally aligned; otherwise, skepticism persisted [
42].
Turning to vaccine hesitancy, the study’s composite index found that over half of caregivers (51.1%) exhibited some degree of hesitancy, higher among males (56.3%) than females (48.4%). This contrasts with only 21.9% who self-reported hesitancy, highlighting likely underreporting due to social desirability bias. In addition, the considerably higher composite index value compared to the indicators based self-reported value suggested that many caregivers might not recognize or admit their own hesitancy, especially if they think hesitancy only means outright refusal. In reality, even doubts, fears, or delays can indicate hesitancy. This gap could also reflect a desire to give socially acceptable answers, or a lack of awareness about what counts as hesitancy. A similar pattern was observed in earlier studies in Ethiopia, where national surveys reported just 3–4% caregiver hesitancy, yet 56% of children experienced delayed vaccinations, indicating a gap between stated attitudes and actual behaviors [
23]. The gendered discrepancy also aligns with regional evidence. In Nigeria, Galadima et al. (2021) found that male caregivers were over twice as likely to exhibit behavioral hesitancy compared to females, despite verbal agreement with vaccination [
37]. The composite index in this study captured nuanced forms of hesitancy, such as doubt, delay, and ambivalence that are often missed by direct questioning. Male hesitancy was linked to lower involvement in immunization decisions and greater exposure to misinformation, especially in urban and conflict-affected areas. Qualitative findings described persistent myths circulating in male-dominated social spaces, while women’s frequent contact with health workers fostered vaccine confidence. Supporting this, multivariable analysis revealed that caregivers with strong family and religious leader support were significantly less likely to be hesitant. Women reported higher levels of such support (70.0% vs. 62.4% from religious leaders; 88.4% vs. 81.3% family support). Systematic reviews confirm these patterns, showing that family and religious support improve childhood vaccination uptake by 22–38% across low- and middle-income countries [
9,
37].
Qualitative data from this study also highlighted the importance of interpersonal trust, especially from spouses, mothers-in-law, and local leaders, in countering misinformation and encouraging vaccine uptake. In contrast, men’s lower reported support reflects structural barriers: Ethiopia’s Health Extension Program is predominantly staffed by women and primarily targets mothers, limiting male engagement. Another important predictor identified was fathers’ perceptions of vaccination responsibility. Fathers who view immunization as solely a woman’s duty were significantly more likely to have under-vaccinated children, highlighting how traditional gender norms contribute to vaccine hesitancy and delay timely immunization. In this study, most caregivers reported joint decision-making, yet many men still perceived vaccination as primarily the mother’s duty. Similarly, mothers were generally seen as the main caregivers responsible for immunization. This imbalance aligns with qualitative evidence from Uganda, where low male involvement and limited support during immunization visits hinder timely vaccine uptake [
21].
The higher hesitancy observed in urban areas contrasts with earlier Ethiopian studies reporting greater rural hesitancy due to access barriers [
43]. This shift likely reflects evolving information ecosystems where urban populations face greater exposure to conflicting messages and rumors, particularly regarding newer vaccines like COVID-19. Tailored urban interventions, including digital rumor surveillance and engagement of trusted male influencers, are critical to counteract misinformation and rebuild trust in these settings. The shift likely reflects changing urban information dynamics, where caregivers, particularly men, are more exposed to rumors and misinformation via social media and peer networks, fostering fears about vaccine safety and mistrust despite better service availability. Conversely, rural caregivers rely more on trusted local health workers and community networks for immunization information and encouragement [
19]. These findings suggest access alone does not overcome distrust in urban settings. Additionally, employment status emerged as a significant factor influencing vaccine hesitancy, with employed caregivers demonstrating higher likelihood of hesitancy compared to their unemployed counterparts. Findings of the qualitative study linked this to time related constraints, exposed to rumors and misinformation via social media and peer networks and rigid work schedules, especially among men, limiting their participation in immunization activities. Women, notably in pastoralist communities, also faced access barriers when lacking partner support. Similar challenges have been documented in India and Mozambique, where work demands and inflexible clinic hours hinder timely vaccination [
44,
45].
Finally, education plays a crucial role in reducing vaccine hesitancy by improving knowledge, building confidence, and fostering critical thinking. However, qualitative findings revealed a paradox: some educated individuals, particularly urban men, were more likely to spread or believe misinformation, undermining vaccine confidence. Similar trends have been documented in South Africa and Nigeria, where higher education does not always guarantee vaccine acceptance due to conflicting information and distrust in authorities [
46,
47,
48]. In contrast, in rural Ethiopian settings, caregivers with limited formal education but high trust in health workers and community programs often demonstrate strong vaccine acceptance [
19]. These findings emphasize the need for context-specific education approaches that blend formal instruction with culturally grounded health communication.
Recent studies from low- and middle-income countries underscore the critical role of gender-transformative approaches in improving vaccine uptake [
46,
47,
48]. For example, research in Nigeria and South Africa highlights how male engagement and addressing misinformation within male social networks can reduce hesitancy [
46,
48]. Similarly, implementation research in Mozambique and India demonstrates that flexible immunization services tailored to working caregivers improve timely vaccination [
44,
45]. These insights reinforce the need for context-specific, gender-responsive strategies in Ethiopia to sustain immunization gains.
Policy Implications
To address these identified gender disparities in vaccine acceptance and hesitancy, Ethiopia’s Ministry of Health should integrate gender-transformative approaches into both the Expanded Program on Immunization (EPI) and the Health Extension Program (HEP). Efforts must explicitly promote shared parental responsibility, challenging entrenched perceptions that immunization is solely a mother’s role. Strengthening male engagement is critical and can be achieved through recruitment of male health workers and leveraging trusted platforms such as religious institutions, workplaces, and male-led community groups. These channels are essential for improving outreach and countering misinformation that disproportionately affects male caregivers. Collaboration with religious and community leaders should be enhanced by providing them with culturally sensitive, evidence-based communication tools.
Health literacy interventions must be context-specific, targeting men and urban populations via hybrid education models that combine formal instruction with community-based approaches. Immunization services in Ethiopia should better accommodate working caregivers by offering mobile vaccination units and organizing workplace vaccination campaigns, particularly in urban and peri-urban areas where caregivers often face scheduling challenges. Urban immunization strategies require particular attention, incorporating digital rumor surveillance and targeted social media campaigns that enlist trusted male influencers to combat misinformation prevalent in urban settings. In pastoralist and mobile communities, culturally competent outreach and flexible, family-centered services are vital to ensuring equitable access. Routine monitoring frameworks should include composite indices capable of capturing nuanced forms of hesitancy and disaggregated data by gender, location, and employment status to inform responsive interventions.
Mainstreaming gender in Health Extension Program training will better equip health workers to promote equitable decision-making and increase male involvement. To operationalize male engagement, the Ministry of Health should pilot recruitment and training of male health extension workers and community mobilizers who can effectively reach men in their social spaces. Integrating gender-sensitivity modules into Health Extension Program curricula will equip all health workers to address gender norms and promote shared parental responsibility. Leveraging workplaces, religious institutions, and male-led community groups as platforms for vaccine education can increase male caregiver involvement. Workplace vaccination campaigns and flexible service hours will accommodate employed caregivers’ schedules, particularly in urban areas. Monitoring frameworks should include gender-disaggregated indicators such as male caregiver participation rates and vaccine uptake to track progress toward gender equity in immunization. Finally, existing community structures such as the Health and Women’s Development Armies should be mobilized to actively engage both mothers and fathers, thereby closing gender gaps and advancing equitable vaccine coverage in Ethiopia. Such comprehensive, gender-transformative strategies are essential to sustaining immunization gains, improving resilience against health crises, and achieving universal vaccine equity.
This study generated valuable evidence on immunization but is limited by the potential for reporting bias due to self-reported vaccination status, acceptance, and hesitancy. Social desirability bias may have led caregivers to underreport vaccine hesitancy, as evidenced by the discrepancy between the composite hesitancy index (51.1%) and direct self-reported hesitancy (21.9%). Recall bias and interviewer effects may also have influenced responses, particularly for sensitive questions related to gender roles and decision-making. Future research should consider triangulating self-reports with vaccination card verification or health facility records to enhance data accuracy. Additionally, qualitative data collection in private settings aimed to minimize social desirability, but residual bias cannot be excluded.