Strengthening Primary Health Care Through Implementation Research: Strategies for Reaching Zero-Dose Children in Low- and Middle-Income Countries’ Immunization Programs
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Analytical Framework
2.3. Identification of the IR Projects
2.4. Data Collection
2.5. Data Extraction and Coding
2.6. Data Analysis
2.7. Consultative Validation
2.8. Ethical Consideration
3. Results
3.1. Characteristics of the Studies and the Intervention
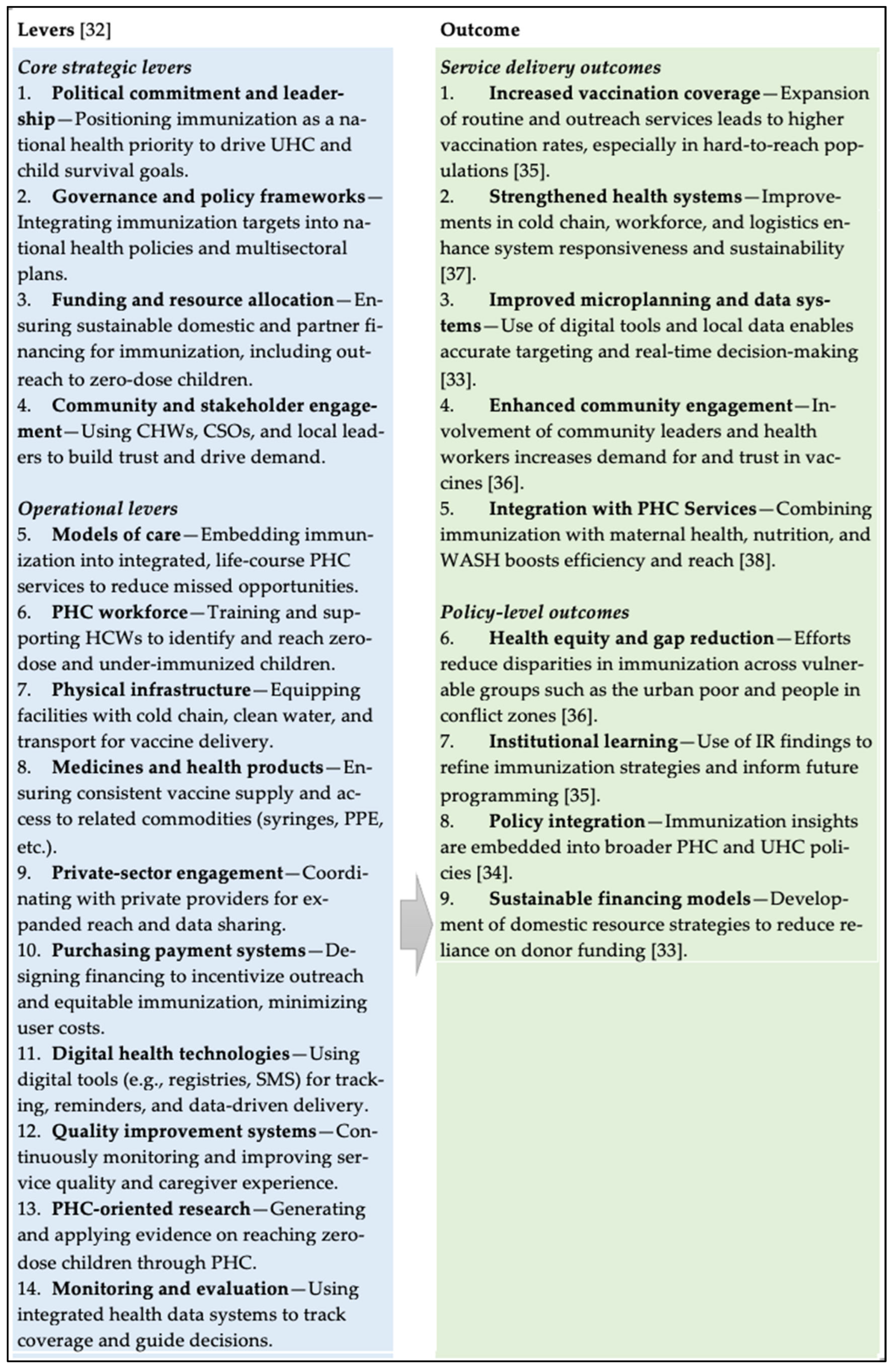
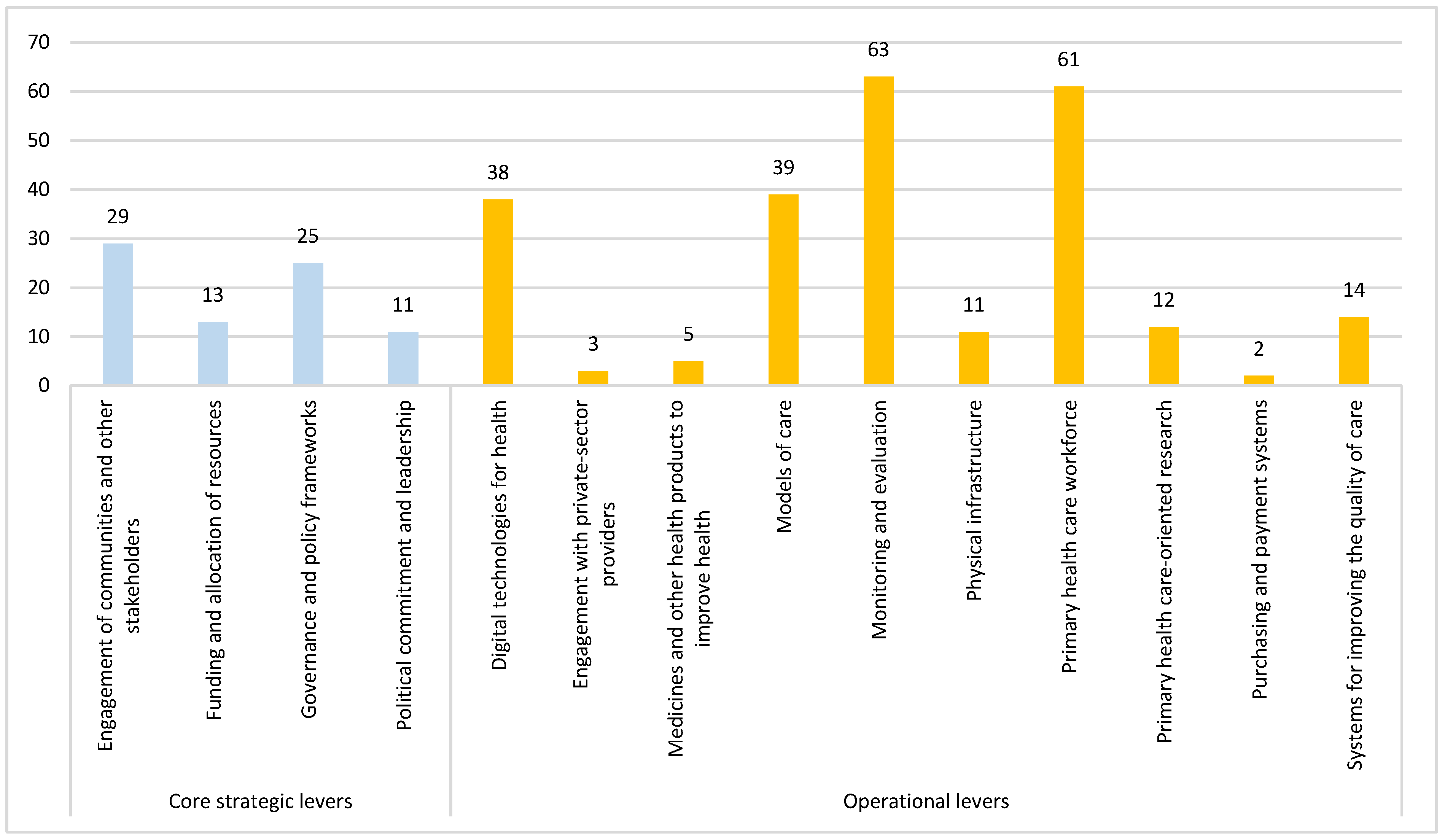
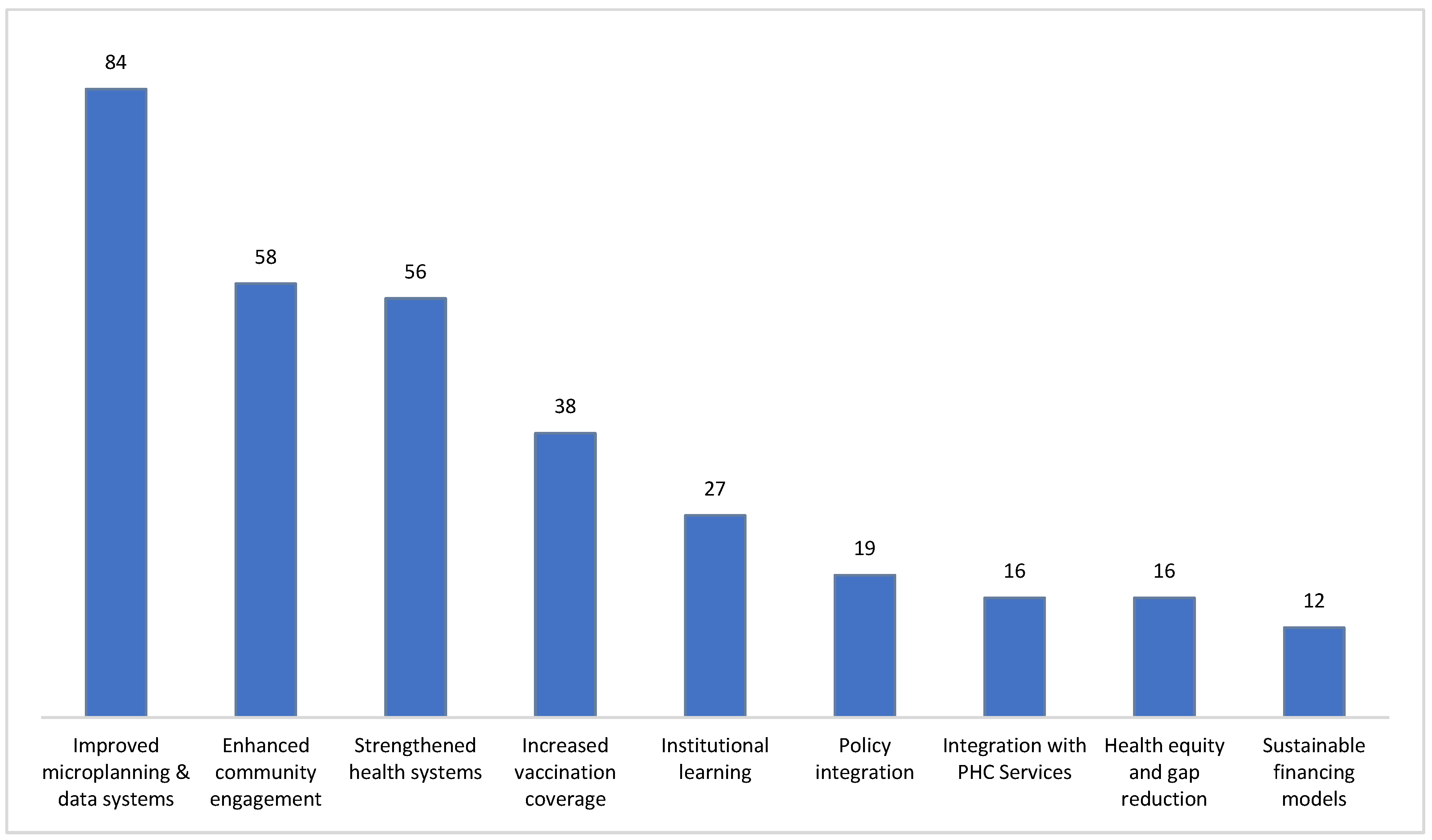
3.2. Immunization Strategies Addressed in the IR Projects and the Outcomes
3.2.1. Immunization Strategies Under Core Strategic Levers
Political Commitment and Leadership
Governance and Policy Frameworks
Funding and Allocation of Resources
Engagement of Communities and Other Stakeholders
3.2.2. Immunization Strategies Under Operational Levers
Model of Care
PHC Workforce
Physical Infrastructure
Medicines and Other Health Products to Improve Health
Engagement with Private-Sector Providers
Purchasing and Payment Systems
Digital Technologies for Health
Systems for Improving the Quality of Care
Primary Health Care-Oriented Research
Monitoring and Evaluation
4. Discussion
4.1. Limitations
4.2. Policy Implication for Eliminating ZD Children
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AC | Auto-disable |
| ASHAs | Accredited social health activists |
| BCC | Behavior change communication |
| BCG | Bacillus Calmette–Guérin |
| CBDV | Community-Based Data Verification |
| CCM | Cold chain management |
| CHWs | Community health workers |
| CSOs | Civil society organizations |
| DHIS2 | District Health Information Software |
| e-Vaccs | Electronic Vaccine Registration System |
| GAVI | The Global Alliance for Vaccines and Immunization |
| GPS | Global Positioning System |
| eCHIS | Electronic Community Health Information System |
| EOC | Emergency Operations Centers |
| EPI | Expanded Programme on Immunization |
| HEWs | Health Extension Workers |
| HCWs | Health care workers |
| HCs | Health Centers |
| HDA | Health Development Army |
| IEC | Information, education, and communication |
| IDPs | Internally displaced persons |
| IPV | Inactivated polio vaccine |
| IR | Implementation research |
| IVR | Interactive Voice Response |
| JAC | Joint Action Committees |
| JHAVP | The Joint Human and Animal Vaccination Project |
| LHWs | Lady health workers |
| LHSs | Lady health supervisors |
| LMICs | Low- and Middle-Income Countries |
| LQAS | Lot Quality Assurance Sampling |
| MIS | Management Information System |
| MoNHSRC | Ministry of National Health Services, Regulation, and Coordination |
| MoU | Memorandum of Understanding |
| NEAP | National Emergency Action Plan |
| NGO | Non-governmental organization |
| NHMIS | National Health Management Information System |
| PEI | Polio Eradication Initiative |
| PHC | Primary Health Care |
| PMTs | Performance Monitoring Teams |
| RI | Routine immunization |
| SOP | Standard Operating Procedure |
| SBCC | Social and Behavior Change Communication |
| SMC | Social Mobilization Committees |
| SMS | Short message service |
| TBAs | Traditional birth attendants |
| VAN | Vaccine Analytics Network |
| vLMIS | Vaccine Logistics Management Information System |
| VVM | Vaccine vial monitoring |
| UHEWs | Urban Health Extension Workers |
| UN | United Nations |
| UNICEF | United Nations Children’s Fund |
| WASH | Water, Sanitation, and Hygiene |
| WDC | Ward Development Committees |
| WDT | Women Health Development Team |
| WHO | World Health Organization |
References
- Shattock, A.J.; Johnson, H.C.; Sim, S.Y.; Carter, A.; Lambach, P.; Hutubessy, R.C.W.; Thompson, K.M.; Badizadegan, K.; Lambert, B.; Ferrari, M.J.; et al. Contribution of vaccination to improved survival and health: Modelling 50 years of the Expanded Programme on Immunization. Lancet 2024, 403, 2307–2316. [Google Scholar] [CrossRef]
- Murhekar, M.V.; Kumar, M.S. Reaching zero-dose children in India: Progress and challenges ahead. Lancet Glob. Health 2021, 9, e1630–e1631. [Google Scholar] [CrossRef] [PubMed]
- Galles, N.C.; Liu, P.Y.; Updike, R.L.; Fullman, N.; Nguyen, J.; Rolfe, S.; Sbarra, A.N.; Schipp, M.F.; Marks, A.; Abady, G.G.; et al. Measuring routine childhood vaccination coverage in 204 countries and territories, 1980–2019: A systematic analysis for the Global Burden of Disease Study 2020, Release 1. Lancet 2021, 398, 503–521. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation and UNICEF. COVID-19 Pandemic Leads to Major Backsliding on Childhood Vaccinations. 2021. Available online: https://www.unicef.org/press-releases/covid-19-pandemic-leads-major-backsliding-childhood-vaccinations-new-who-unicef-data (accessed on 10 August 2021).
- World Health Organization. Global Immunization Efforts Have Saved at Least 154 Million Lives over the Past 50 Years. World Health Organization News. April 2024. Available online: https://www.who.int/news/item/24-04-2024-global-immunization-efforts-have-saved-at-least-154-million-lives-over-the-past-50-years (accessed on 1 May 2025).
- World Health Organization and United Nations Children’s Fund. Global Childhood Vaccination Coverage Holds Steady, Yet Over 14 Million Infants Remain Unvaccinated. 2025. Available online: https://www.who.int/news/item/15-07-2025-global-childhood-vaccination-coverage-holds-steady-yet-over-14-million-infants-remain-unvaccinated-who-unicef (accessed on 12 September 2025).
- Cata-Preta, B.O.; Santos, T.M.; Mengistu, T.; Hogan, D.R.; Barros, A.J.; Victora, C.G. Zero-dose children and the immunisation cascade: Understanding immunisation pathways in low and middle-income countries. Vaccine 2021, 39, 4564–4570. [Google Scholar] [CrossRef] [PubMed]
- Portnoy, A.; Jit, M.; Helleringer, S.; Verguet, S. Impact of measles supplementary immunization activities on reaching children missed by routine programs. Vaccine 2018, 36, 170–178. [Google Scholar] [CrossRef]
- World Health Organization. Immunization Agenda 2030: A Global Strategy to Leave No One Behind. 2020. Available online: https://www.who.int/immunization/immunization_agenda_2030/en/ (accessed on 10 August 2022).
- World Health Organization. Primary Health Care on the Road to Universal Health Coverage: 2019 Global Monitoring Report; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Giersing, B.; Mo, A.X.; Hwang, A.; Baqar, S.; Earle, K.; Ford, A.; Deal, C.; Dull, P.; Friede, M.; Hall, B.F. Meeting summary: Global vaccine and immunization research forum, 2023. Vaccine 2025, 46, 126686. [Google Scholar] [CrossRef]
- UNICEF. UNICEF Immunization Roadmap to 2030. 2023. Available online: https://www.unicef.org/media/138976/file/UNICEF%20Immunization%20Roadmap%20To%202030.pdf (accessed on 1 May 2025).
- Nzilibili, S.M.; Maziku, H.; Araya, A.; Kateule, R.; Malamla, M.A.; Salum, S.; Kyesi, F.; Gadau, L.; Haonga, T.M.; Tinuga, F.; et al. Using Human-Centered Design to Bridge Zero-Dose Vaccine Gap: A Case Study of Ilala District in Tanzania. Vaccines 2025, 13, 38. [Google Scholar] [CrossRef]
- Victora, C.G. Assessing the overlap between immunisation and other essential health interventions in 92 low-and middle-income countries using household surveys: Opportunities for expanding immunisation and primary health care. EClinicalMedicine 2021, 42, 101196. [Google Scholar]
- World Health Organization. Immunization Agenda 2030 Partners, Immunization agenda 2030: A global strategy to leave no one behind. Vaccine 2024, 42, S5–S14. [Google Scholar]
- World Health Organization and UNICEF. Implementation research toolkit. In Implementation Research Toolkit; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Jackson, D.; Shahabuddin, A.S.M.; Sharkey, A.B.; Källander, K.; Muñiz, M.; Mwamba, R.; Nyankesha, E.; Scherpbier, R.W.; Hasman, A.; Balarajan, Y.; et al. Closing the know-do gap for child health: UNICEF’s experiences from embedding implementation research in child health and nutrition programming. Implement. Sci. Commun. 2021, 2, 112. [Google Scholar] [CrossRef]
- Theobald, S.; Brandes, N.; Gyapong, M.; El-Saharty, S.; Proctor, E.; Diaz, T.; Wanji, S.; Elloker, S.; Raven, J.; Elsey, H.; et al. Implementation research: New imperatives and opportunities in global health. Lancet 2018, 392, 2214–2228. [Google Scholar] [CrossRef] [PubMed]
- Shahabuddin, A.; Scherpbier, R.; Sharkey, A.; Källander, K. UNICEF’s Approach to Embedded Implementation Research: Applications in Health Programmes. 2025. Available online: https://www.research4implementation.org/category/news/ (accessed on 4 July 2025).
- UNICEF. Summary Operational Guidance Multisectoral Zero-Dose Strategies to Improve Routine Immunization and Other Child Outcome. 2025. Available online: www.unicef.org/media/168701/file/250310%20UNICEF%20NY%20Zero-dose%20Summary%20Web.pdf.pdf (accessed on 1 May 2025).
- UNICEF. Implementation Research: Country Projects. 2025. Available online: https://irds.quo-staging.com/country-projects/#reporting (accessed on 24 January 2025).
- Mancuso, A.; Malm, S.A.; Sharkey, A.; Shahabuddin, A.S.M.; Shroff, Z.C. Cross-cutting lessons from the Decision-Maker Led Implementation Research initiative. Health Res. Policy Syst. 2021, 19, 83. [Google Scholar] [CrossRef]
- Shroff, Z.C.; Mancuso, A.B.; Sharkey, A.; Shahabuddin, A.S.M.; Kumar, B.; Johnson, H.; Ghaffar, A. Decision-maker led implementation research on immunization: Learning from low- and middle-income countries. Health Res. Policy Syst. 2021, 19, 68. [Google Scholar] [CrossRef]
- Rasanathan, K.; Tran, N.; Johnson, H.L.; Hafeez, A.; Peterson, S.; Ghaffar, A. Realizing the potential of embedded implementation research: Lessons from Pakistan. J. Glob. Health 2020, 10, 020104. [Google Scholar] [CrossRef]
- UNICEF. Multisectoral Zero-Dose Strategies to Improve Routine Immunization and Other Child Outcomes. Operational Guidance: Multisectoral Zero-Dose Strategies to Improve Routine Immunization and Other Child Outcomes 2025. Available online: https://www.unicef.org/media/168696/file/250310%20unicef%20NY%20mutisectoral%20zero-dose%20op%20guidance-Hires.pdf.pdf (accessed on 30 May 2025).
- Yin, K.R. Case Study Research and Applications: Design and Methods, 6th ed.; SAGE Publications: Thousand Oaks, CA, USA, 2018. [Google Scholar]
- Mays, N.; Pope, C.; Popay, J. Systematically reviewing qualitative and quantitative evidence to inform management and policy-making in the health field. J. Health Serv. Res. Policy 2005, 10 (Suppl. S1), 6–20. [Google Scholar] [CrossRef]
- Grant, M.J.; Booth, A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Inf. Libr. J. 2009, 26, 91–108. [Google Scholar] [CrossRef]
- Walt, G.; Shiffman, J.; Schneider, H.; Murray, S.F.; Brugha, R.; Gilson, L. ‘Doing’health policy analysis: Methodological and conceptual reflections and challenges. Health Policy Plan. 2008, 23, 308–317. [Google Scholar] [CrossRef] [PubMed]
- Gilson, L. Health Policy and Systems Research: A Methodology Reader; WHO: Geneva, Switzerland, 2012. [Google Scholar]
- Greene, J.C. Mixed Methods in Social Inquiry; John Wiley & Sons: Hoboken, NJ, USA, 2007; Volume 9. [Google Scholar]
- World Health Organization and United Nations Children’s Fund (UNICEF). A Vision for Primary Health Care in the 21st Century: Towards Universal Health Coverage and the Sustainable Development Goals. 2018. Available online: https://apps.who.int/iris/handle/10665/328065 (accessed on 22 April 2025).
- Fairbrother, G.; Kuttner, H.; Miller, W.; Hogan, R.; McPhillips, H.; Johnson, K.A.; Alexander, E. Findings from case studies of state and local immunization programs. Am. J. Prev. Med. 2000, 19, 54–77. [Google Scholar] [CrossRef] [PubMed]
- Giles, M.; Mason, E.; Muñoz, F.; Moran, A.; Lambach, P.; Merten, S.; Diaz, T.; Baye, M.; Mathai, M.; Pathirana, J.; et al. Antenatal care service delivery and factors affecting effective tetanus vaccine coverage in low-and middle-income countries: Results of the Maternal Immunisation and Antenatal Care Situational analysis (MIACSA) project. Vaccine 2020, 38, 5278–5285. [Google Scholar] [CrossRef]
- Blanc, D.C.; Grundy, J.; Sodha, S.V.; O’COnnell, T.S.; von Mühlenbrock, H.J.M.; Grevendonk, J.; Ryman, T.; Patel, M.; Olayinka, F.; Brooks, A.; et al. Immunization programs to support primary health care and achieve universal health coverage. Vaccine 2024, 42, S38–S42. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, N.; DeRoeck, D.; Sadr-Azodi, N. Private sector engagement and contributions to immunisation service delivery and coverage in Sudan. BMJ Glob. Health 2019, 4, e001414. [Google Scholar]
- Sakas, Z.; Hester, K.A.; Ellis, A.; Ogutu, E.A.; Rodriguez, K.; Bednarczyk, R.; Dixit, S.; Kilembe, W.; Sarr, M.; Freeman, M.C. Critical success factors for high routine immunisation performance: A qualitative analysis of interviews and focus groups from Nepal, Senegal, and Zambia. BMJ Open 2023, 13, e070541. [Google Scholar] [CrossRef] [PubMed]
- Morgan, C.; Giattas, M.R.; Holroyd, T.; Pfitzer, A.; Engel, D.; Sidibe, A.; Holloway, M.; Bloem, P.; Fields, R.; Shimp, L.; et al. Integration of other services with human papillomavirus vaccination; lessons from earlier in the life course highlight the need for new policy and implementation evidence. Vaccine 2022, 40, A94–A99. [Google Scholar] [CrossRef]
- UNICEF. Pakistan Implementation Research for Immunization—A compilation of project objectives, results and recommendations. In Alliance for Health Policy and Systems Research, and Gavi the Vaccine Alliance; UNICEF: Geneva, Switzerland, 2018. [Google Scholar]
- UNICEF. Immunization Coverage: Are We Losing Ground? 2020. Available online: https://data.unicef.org/resources/immunization-coverage-are-we-losing-ground/ (accessed on 19 March 2025).
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar]
- Craig, P.; Dieppe, P.; Macintyre, S.; Michie, S.; Nazareth, I.; Petticrew, M. Developing and evaluating complex interventions: The new Medical Research Council guidance. BMJ 2008, 337, a1655. [Google Scholar] [CrossRef]
- Council for International Organizations of Medical Sciences. International Ethical Guidelines for Health-Related Research Involving Humans: Prepared by the Council for International Organizations of Medical Sciences (CIOMS) in Collaboration with the World Health Organization (WHO); Council for International Organizations of Medical Sciences: Geneva, Switzerland, 2016. [Google Scholar]
- Mafigiri, D.K.; Iradukunda, C.; Atumanya, C.; Odie, M.; Mancuso, A.; Tran, N.; McGrath, J.; Luzze, H. A qualitative study of the development and utilization of health facility-based immunization microplans in Uganda. Health Res. Policy Syst. 2021, 19, 52. [Google Scholar]
- Abakar, M.F.; Seli, D.; Lechthaler, F.; Crump, L.; Mancus, A.; Tran, N.; Zinsstag, J.; Muñoz, D.C. Evaluation of the feasibility and sustainability of the joint human and animal vaccination and its integration to the public health system in the Danamadji health district, Chad. Health Res. Policy Syst. 2021, 19, 44. [Google Scholar]
- Etokidem, A.; Nkpoyen, F.; Ekanem, C.; Mpama, E.; Isika, A. Potential barriers to and facilitators of civil society organization engagement in increasing immunization coverage in Odukpani Local Government Area of Cross River State, Nigeria: An implementation research. Health Res. Policy Syst. 2021, 19, 46. [Google Scholar] [CrossRef]
- Nair, A.T.; Nayar, K.R.; Koya, S.F.; Abraham, M.; Lordson, J.; Grace, C.; Sreekumar, S.; Chembon, P.; Swarnam, K.; Pillai, A.M.; et al. Social media, vaccine hesitancy and trust deficit in immunization programs: A qualitative enquiry in Malappuram District of Kerala, India. Health Res. Policy Syst. 2021, 19, 56. [Google Scholar] [CrossRef] [PubMed]
- Zewde, T.; Teklu, A.; Bedada, D.; Tsehaye, Y. The influence of linkages, feedback mechanisms, and caregiver mobility on immunization follow-up visits in Lideta sub-city of Addis Ababa, Ethiopia: A qualitative study. Health Res. Policy Syst. 2021, 19, 69. [Google Scholar] [CrossRef] [PubMed]
- Yazdani, A.T.; Muhammad, A.; Nisar, M.I.; Khan, U.; Shafiq, Y. Unveiling and addressing implementation barriers to routine immunization in the peri-urban slums of Karachi, Pakistan: A mixed-methods study. Health Res. Policy Syst. 2021, 19, 55. [Google Scholar] [CrossRef]
- Tilahun, B.; Teklu, A.; Mancuso, A.; Endehabtu, B.F.; Gashu, K.D.; Mekonnen, Z.A. Using health data for decision-making at each level of the health system to achieve universal health coverage in Ethiopia: The case of an immunization programme in a low-resource setting. Health Res. Policy Syst. 2021, 19, 48. [Google Scholar] [CrossRef]
- Akwataghibe, N.N.; Ogunsola, E.A.; Popoola, O.A.; Agbo, A.I.; Dieleman, M.A. Using participatory action research to improve immunization utilization in areas with pockets of unimmunized children in Nigeria. Health Res. Policy Syst. 2021, 19, 88. [Google Scholar] [CrossRef]
- Shahabuddin, A.; Sharkey, A.; Khalid, F.; Rasanathan, K.; Hasman, A.; Tran, N.; Durrani, A.; Ongwae, K.; Duncan, R.; Ahmed, K.A.; et al. An embedded implementation research initiative to tackle service delivery bottlenecks in the expanded programme on immunisation in Pakistan: Overview and reflections. J. Glob. Health 2021, 11, 06003. [Google Scholar] [CrossRef]
- Sahito, A.; Ahmed, S.; Fatmi, Z. Covering the last mile for vaccination: Feasibility and acceptability of traditional birth attendant-based referral system in hard-to-reach areas in rural Pakistan. J. Glob. Health 2020, 10, 021303. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.A.; Ashfaq, M.; Ayub, A.; Jamil, A.; Badshah, J.; Ullah, I.; Shahabuddin, A.; Khalid, F. Developing a three-dimensional narrative to counter polio vaccine refusal in Charsadda. J. Glob. Health 2020, 10, 021301. [Google Scholar] [CrossRef] [PubMed]
- Malik, M.N.; Awan, M.S.; Saleem, T. Social mobilization campaign to tackle immunization hesitancy in Sargodha and Khushab districts of Pakistan. J. Glob. Health 2020, 10, 021302. [Google Scholar] [CrossRef] [PubMed]
- Haq, Z.; Shaikh, B.T.; Tran, N.; Hafeez, A.; Ghaffar, A. System within systems: Challenges and opportunities for the Expanded Programme on Immunisation in Pakistan. Health Res. Policy Syst. 2019, 17, 51. [Google Scholar] [CrossRef]
- Altaf, A.; Siddiqui, A.; Ashfaq, A.M.; Shahabuddin, A. Visibility and Analytics Network (VAN) approach to improve immunization supply chain and management performance system in Pakistan. J. Glob. Health 2021, 11, 06002. [Google Scholar] [CrossRef]
- Qayyum, K.; Rehan, N.; Khalid, F.; Younas, M. Addressing community barriers to immunization in Rajanpur district, Pakistan: An implementation research. J. Glob. Health Rep. 2021, 5, e2021088. [Google Scholar] [CrossRef]
- Asrade, G.; Alemu, K.; Gebeye, E.; Walle, M.; Teklu, A.; Mekonnen, Z.A.; Shiferaw, A.; Assan, A.; Tilahun, B. The burden of internal conflict on expanded programs on immunization in northwest Ethiopia: Implementation science study. Ethiop. J. Health Dev. 2021, 35, 39–48. [Google Scholar]
- Bayih, G.; Teklu, A.; Mekonnen, Z.A.; Tsedaw, T.; Tefera, S.; Feletto, M.; Shahabuddin, A.; Tilahun, B. The implementation of social and behavior change communication intervention to improve immunization demand: A qualitative study in Awabel district, Northwest Ethiopia. Ethiop. J. Health Dev. 2021, 35, 49–55. [Google Scholar]
- Amare, G.; Seyoum, T.; Zayede, T.; Tazebew, A.; Teklu, A.; Mekonnen, Z.A.; Endehabtu, B.F.; Sharkey, A.; Tilahun, B. Vaccine safety practices and its implementation barriers in Northwest Ethiopia: A qualitative study. Ethiop. J. Health Dev. 2021, 35, 111–117. [Google Scholar]
- Gelagay, A.A.; Geremew, A.B.; Teklu, A.; Mekonnen, Z.A.; Gera, R.; Ba-Nguz, A.; Tilahun, B. Full immunization coverage and its determinants among children aged 12–23 months in Wogera district, Northwest Ethiopia. Ethiop. J. Health Dev. 2021, 35, 6–27. [Google Scholar]
- Gelagay, A.A.; Geremew, A.B.; Teklu, A.; Mekonnen, Z.A.; Sharkey, A.; Assan, A.; Tilahun, B. Women’s Independent Household Decision Making Power and its influence on their Autonomy in relation to Child Vaccinations: A mixed-method study among Women of Reproductive Age in Northwest Ethiopia. Ethiop. J. Health Dev. 2021, 35, 86–97. [Google Scholar]
- Kerebih, M.; Minyihun, A.; Gudale, A.; Shiferaw, A.; Hagos, A.; Mekonnen, Z.A.; Teklu, A.; Feletto, M.; Shahabuddin, A.; Tilahun, B. How to optimize health facilities and community linkage in order to enhance immunization service? The case of West Amhara Region, Ethiopia. Ethiop. J. Health Dev. 2021, 35, 75–85. [Google Scholar]
- Endehabtu, B.F.; Lakew, Y.; Tegegn, B.; Morka, T.; Mekonnen, Z.A.; Teklu, A.; Shahabuddin, A.; Gera, R.; Tilahun, B. How to optimize Immunization Supply Management at different levels of the health system in Oromia Region? An implementation science research. Ethiop. J. Health Dev. 2021, 35, 65–74. [Google Scholar]
- Madebo, T.H.; Gezie, L.D.; Teklu, A.; Mekonnen, Z.A.; Shahabuddin, A.; Tilahun, B. Immunization data quality and factors influencing data generation, handling and use in Wogera District, Northern Ethiopia, 2020. Ethiop. J. Health Dev. 2021, 35, 56–64. [Google Scholar]
- Gedlu, T.; Gashu, K.D.; Birhanu, N.; Tessema, S.; Deti, T.; Mekonnen, Z.A.; Teklu, A.; Shiferaw, A.; Tilahun, B. Implementation fidelity and challenges of optimal cold chain management in Assossa district health system, Benshangul-Gumuz region, Western Ethiopia. Ethiop. J. Health Dev. 2021, 35, 3–8. [Google Scholar]
- Mekonnen, Z.A.; Nigus, M.; Assefa, S.; Biru, A.; Teklu, A.; Feletto, M.; Gera, R.; Ba-Nguz, A.; Tilahun, B. Strategies to revitalize immunization service provision in urban settings of Ethiopia. Ethiop. J. Health Dev. 2021, 35, 98–110. [Google Scholar]
- Kefiyalew, B.; Mamo, W.; Chanyalew, M.A.; Abay, S.; Abate, B.; Necho, A.; Ayalew, Y.; Mekonnen, Z.A.; Teklu, A.; Shiferaw, A.; et al. Assessment of barriers to the implementation of community-based data verification and immunization data discrepancies between health facilities and the community in Tach Gayint district, Northwest Ethiopia. Ethiop. J. Health Dev. 2021, 35, 9–15. [Google Scholar]
- Kefiyalew, B.; Abay, S.; Mamo, W.; Abate, B.; Chanyalew, M.A.; Ayalew, Y.; Necho, A.; Mekonnen, Z.A.; Teklu, A.; Shahabuddin, A.; et al. Assessment of immunization data management practices, facilitators, and barriers to immunization data quality in the health facilities of Tach Gayint district, Northwest Ethiopia. Ethiop. J. Health Dev. 2021, 35, 31–38. [Google Scholar]
- Dadari, I.; Higgins-Steele, A.; Sharkey, A.; Charlet, D.; Shahabuddin, A.; Nandy, R.; Jackson, D. Pro-equity immunization and health systems strengthening strategies in select Gavi-supported countries. Vaccine 2021, 39, 2434–2444. [Google Scholar] [CrossRef]
- Haq, Z.; Chandio, A.K.; Zafar, S.; Iqbal, F.; Naeem, A.; Karim, S. The synergy between Expanded Program on Immunization and Polio Eradication Initiative in Pakistan: A policy and program exploration. J. Glob. Health Rep. 2021, 5, e2021081. [Google Scholar] [CrossRef]
- Haq, Z.U.; Rana, M.S. Synergized immunization programming: Pakistan’s road to polio eradication. J. Glob. Health 2021, 11, 03103. [Google Scholar] [CrossRef]
- Naveed, Z.; Saeed, A.; Kakar, A.; Khalid, F.; Alnaji, N.; Kumar, G. Understanding the accountability issues of the immunization workforce for the Expanded Program on Immunization (EPI) in Balochistan: An exploratory study. J. Glob. Health 2021, 11, 06001. [Google Scholar] [PubMed]
- Shahabuddin, A.S.M.; Sharkey, A.B.; Jackson, D.; Rutter, P.; Hasman, A.; Sarker, M. Carrying out embedded implementation research in humanitarian settings: A qualitative study in Cox’s Bazar, Bangladesh. PLoS Med. 2020, 17, e1003148. [Google Scholar] [CrossRef]
- Bugase, E.; Tindana, P. Influence of trust on the acceptance of the RTS, S malaria vaccine in the Kassena-Nankana districts of Ghana. Malar. J. 2024, 23, 365. [Google Scholar] [CrossRef]
- Lees, S.; Alcanya-Stevens, L.; Bowmer, A.; Marchant, M.; Enria, L.; Vanderslott, S. Political and Community Logics of Emergent Disease Vaccine Deployment: Anthropological Insights from DRC, Uganda and Tanzania. Anthropologica 2024, 66, 1–28. [Google Scholar] [CrossRef]
- Chauhadry, I.A.; Soofi, S.B.; Sajid, M.; Ali, R.; Khan, A.; Naqvi, S.K.; Hussain, I.; Umer, M.; Bhutta, Z.A. Bridging the Vaccination Equity Gap: A Community-Driven Approach to Reduce Vaccine Inequities in Polio High-Risk Areas of Pakistan. Vaccines 2024, 12, 1340. [Google Scholar] [CrossRef]
- Siddiqi, D.A.; Iftikhar, S.; Siddique, M.; Mehmood, M.; Dharma, V.K.; Shah, M.T.; Setayesh, H.; Chandir, S. Immunization gender inequity in Pakistan: An analysis of 6.2 million children born from 2019 to 2022 and enrolled in the Sindh Electronic Immunization Registry. Vaccines 2023, 11, 685. [Google Scholar] [CrossRef]
- Doocy, S.; Lyles, E.; Akhu-Zaheya, L.; Burton, A.; Burnham, G. Health service access and utilization among Syrian refugees in Jordan. Int. J. Equity Health 2016, 15, 108. [Google Scholar] [CrossRef]
- Cleaveland, S.; Sharp, J.; Abela-Ridder, B.; Allan, K.J.; Buza, J.; Crump, J.A.; Davis, A.; Vilas, V.J.D.R.; de Glanville, W.A.; Kazwala, R.R.; et al. One Health contributions towards more effective and equitable approaches to health in low-and middle-income countries. Philos. Trans. R. Soc. B Biol. Sci. 2017, 372, 20160168. [Google Scholar] [CrossRef]
- Cheuyem, F.Z.L.; Amani, A.; Ajong, B.N.; Otsali, R.K.N.; Nouko, A.; Guissama, E.O.; Ngos, C.S.; Mohamadou, A.; Nloga, G.S.; Edzamba, M.F.; et al. Assessment of Vaccine Managers’ Knowledge and Observance of Vaccination Norms and Standards in an Urban Health District of Yaounde (Cameroon) during the COVID-19 Pandemic. medRxiv 2024. [Google Scholar] [CrossRef]
- World Health Organization and UNICEF. Joint policy statement. In Promoting the Exclusive Use of Injection Safety Devices for All Immunization Activities; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- United States Centre for Disease Control and Prevention. Vaccine Storage and Handling Toolkit Updated with Mpox Vaccines Storage and Handling Information Addendum. 2024. Available online: https://www.cdc.gov/vaccines/hcp/downloads/storage-handling-toolkit.pdf (accessed on 30 April 2025).
- World Health Organization. Quality Immunization Services: A Planning Guide; World Health Organization: Geneva, Switzerland, 2022; Volume 2025. [Google Scholar]
- World Health Organization. Engagement of private/nongovernmental health providers in immunization service delivery: Considerations for National Immunization Programmes. In Engagement of Private/Nongovernmental Health Providers in Immunization Service Delivery: Considerations For National Immunization Programmes; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Sharma, G.; Morgan, C.; Wanyoike, S.; Kenyon, S.; Sheel, M.; Jain, M.; Boggs, M.; Olayinka, F. Private sector engagement for immunisation programmes: A pragmatic scoping review of 25 years of evidence on good practice in low-income and middle-income countries. BMJ Glob. Health 2024, 8 (Suppl. S5), e014728. [Google Scholar] [CrossRef] [PubMed]
- Ormel, H.; Kok, M.; Kane, S.; Ahmed, R.; Chikaphupha, K.; Rashid, S.F.; Gemechu, D.; Otiso, L.; Sidat, M.; Theobald, S.; et al. Salaried and voluntary community health workers: Exploring how incentives and expectation gaps influence motivation. Hum. Resour. Health 2019, 17, 59. [Google Scholar] [CrossRef] [PubMed]
- Carmichael, S.L.; Mehta, K.; Raheel, H.; Srikantiah, S.; Chaudhuri, I.; Trehan, S.; Mohanty, S.; Borkum, E.; Mahapatra, T.; Weng, Y.; et al. Effects of team-based goals and non-monetary incentives on front-line health worker performance and maternal health behaviours: A cluster randomised controlled trial in Bihar, India. BMJ Glob. Health 2019, 4, e001146. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharyya, K.; Winch, P.; LeBan, K.; Tien, M. Community Health Worker Incentives and Disincentives: How They Affect Motivation, Retention, and Sustainability; BASICS II: Arlington, VA, USA, 2001. [Google Scholar]
- Restrepo-Méndez, M.C.; Barros, A.J.; Wong, K.L.; Johnson, H.L.; Pariyo, G.; França, G.V.; Wehrmeister, F.C.; Victora, C.G. Inequalities in full immunization coverage: Trends in low-and middle-income countries. Bull. World Health Organ. 2016, 94, 794. [Google Scholar] [CrossRef]
- Newbrander, W.; Ickx, P.; Feroz, F.; Stanekzai, H. Afghanistan’s basic package of health services: Its development and effects on rebuilding the health system. Glob. Public Health 2014, 9 (Suppl. S1), S6–S28. [Google Scholar] [CrossRef] [PubMed]
- Rao, K.D.; Bhatnagar, A.; Berman, P. So many, yet few: Human resources for health in India. Hum. Resour. Health 2012, 10, 19. [Google Scholar] [CrossRef]
- Wolff, B.; Aborigo, R.A.; Dalaba, M.; Opare, J.K.L.; Conklin, L.; Bonsu, G.; Amponsa-Achiano, K. Community Barriers, Enablers, and Normative Embedding of Second Year of Life Vaccination in Ghana: A Qualitative Study. Glob. Health Sci. Pract. 2023, 11, e2200496. [Google Scholar] [CrossRef] [PubMed]
- Glenton, C.; Scheel, I.B.; Pradhan, S.; Lewin, S.; Hodgins, S.; Shrestha, V. The female community health volunteer programme in Nepal: Decision makers’ perceptions of volunteerism, payment and other incentives. Soc. Sci. Med. 2010, 70, 1920–1927. [Google Scholar] [CrossRef]
- Del Riccio, M.; Bechini, A.; Buscemi, P.; Bonanni, P.; on behalf of the Working Group DHS; Boccalini, S. Reasons for the intention to refuse COVID-19 vaccination and their association with preferred sources of information in a nationwide, Population-Based sample in Italy, before COVID-19 vaccines roll out. Vaccines 2022, 10, 913. [Google Scholar] [CrossRef]
- Smith, L.E.; Amlôt, R.; Weinman, J.; Yiend, J.; Rubin, G.J. A systematic review of factors affecting vaccine uptake in young children. Vaccine 2017, 35, 6059–6069. [Google Scholar] [CrossRef]
- Werner, L.; Seymour, D.; Puta, C.; Gilbert, S. Three waves of data use among health workers: The experience of the Better Immunization Data Initiative in Tanzania and Zambia. Glob. Health Sci. Pract. 2019, 7, 447–456. [Google Scholar] [CrossRef]
- Feikin, D.R.; Nguyen, L.M.; Adazu, K.; Ombok, M.; Audi, A.; Slutsker, L.; Lindblade, K.A. The impact of distance of residence from a peripheral health facility on pediatric health utilisation in rural western Kenya. Trop. Med. Int. Health 2009, 14, 54–61. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Vaccine Action Plan 2011–2020: Midterm Review Report. 2018. Available online: https://www.who.int/publications/i/item/global-vaccine-action-plan-2011-2020 (accessed on 29 April 2025).
- Mutua, M.K.; Kimani-Murage, E.; Ettarh, R.R. Childhood vaccination in informal urban settlements in Nairobi, Kenya: Who gets vaccinated? BMC Public Health 2011, 11, 6. [Google Scholar] [CrossRef] [PubMed]

| Changes Made | Focus Areas | Country |
|---|---|---|
| * Improved community mobilization and communication strategies in two wards to increase immunization coverage | EPI | Nigeria |
| m-Health technology and recruitment of new vaccinators introduced | EPI | Pakistan |
| Pain management strategy scaled-up in several hospitals | EPI | Kenya |
| * Birth registration enhanced through inclusion in MNCH and EPI programming and in community health platforms | BR4MNCH | Ethiopia |
| Federal government involved in social media content management to reduce anti-vaccine propaganda | EPI | Pakistan |
| * Improved vaccine literacy by creating a manual for health workers to build their knowledge and to better respond to the vaccine misinformation circulating in the communities | EPI | India |
| Enhanced communication strategies for reaching nomadic communities for vaccination through integrated human and animal vaccination campaign | EPI | Chad |
| Improved supply-side service delivery by provincial authorities | EPI | Pakistan |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oyugi, B.; Kallander, K.; Shahabuddin, A.S.M. Strengthening Primary Health Care Through Implementation Research: Strategies for Reaching Zero-Dose Children in Low- and Middle-Income Countries’ Immunization Programs. Vaccines 2025, 13, 1040. https://doi.org/10.3390/vaccines13101040
Oyugi B, Kallander K, Shahabuddin ASM. Strengthening Primary Health Care Through Implementation Research: Strategies for Reaching Zero-Dose Children in Low- and Middle-Income Countries’ Immunization Programs. Vaccines. 2025; 13(10):1040. https://doi.org/10.3390/vaccines13101040
Chicago/Turabian StyleOyugi, Boniface, Karin Kallander, and A. S. M. Shahabuddin. 2025. "Strengthening Primary Health Care Through Implementation Research: Strategies for Reaching Zero-Dose Children in Low- and Middle-Income Countries’ Immunization Programs" Vaccines 13, no. 10: 1040. https://doi.org/10.3390/vaccines13101040
APA StyleOyugi, B., Kallander, K., & Shahabuddin, A. S. M. (2025). Strengthening Primary Health Care Through Implementation Research: Strategies for Reaching Zero-Dose Children in Low- and Middle-Income Countries’ Immunization Programs. Vaccines, 13(10), 1040. https://doi.org/10.3390/vaccines13101040











