Post-COVID-19 Vaccine Hyperproduction of Anti-Spike Antibodies and Rheumatological Manifestations
Abstract
1. Introduction
2. Material and Methods
3. Results
3.1. Cohort 1
3.2. Cohort 2
| Patients | Age | Gender | Ethnic | Vaccines | Vaccine Doses/Delay Days | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F | M | F | M | Caucasian | Black African | Asian | mRNA | DNA | 1st/Delay | 2nd/Delay | ||
| 3rd/Delay | 4th/Delay | |||||||||||
| Cohort 1 | 124 | 54.6 | 59.6 | 87 | 37 | 79 F/32 M | 7 F/3 M | 1 F/1 M | 120 | 4 | 17/12, 5 d | 50/20, 3 d |
| 55/30, 5 d | 4/30, 5 d | |||||||||||
| Cohort 2 | 125 | 41.2 | 50.6 | 94 | 31 | 86 F/29 M | 7 F/0 M | 1 F/2 M | 123 | 2 | 4/12, 5 d | 45/>122 d |
| 58/>113 d | 18/>126 d | |||||||||||
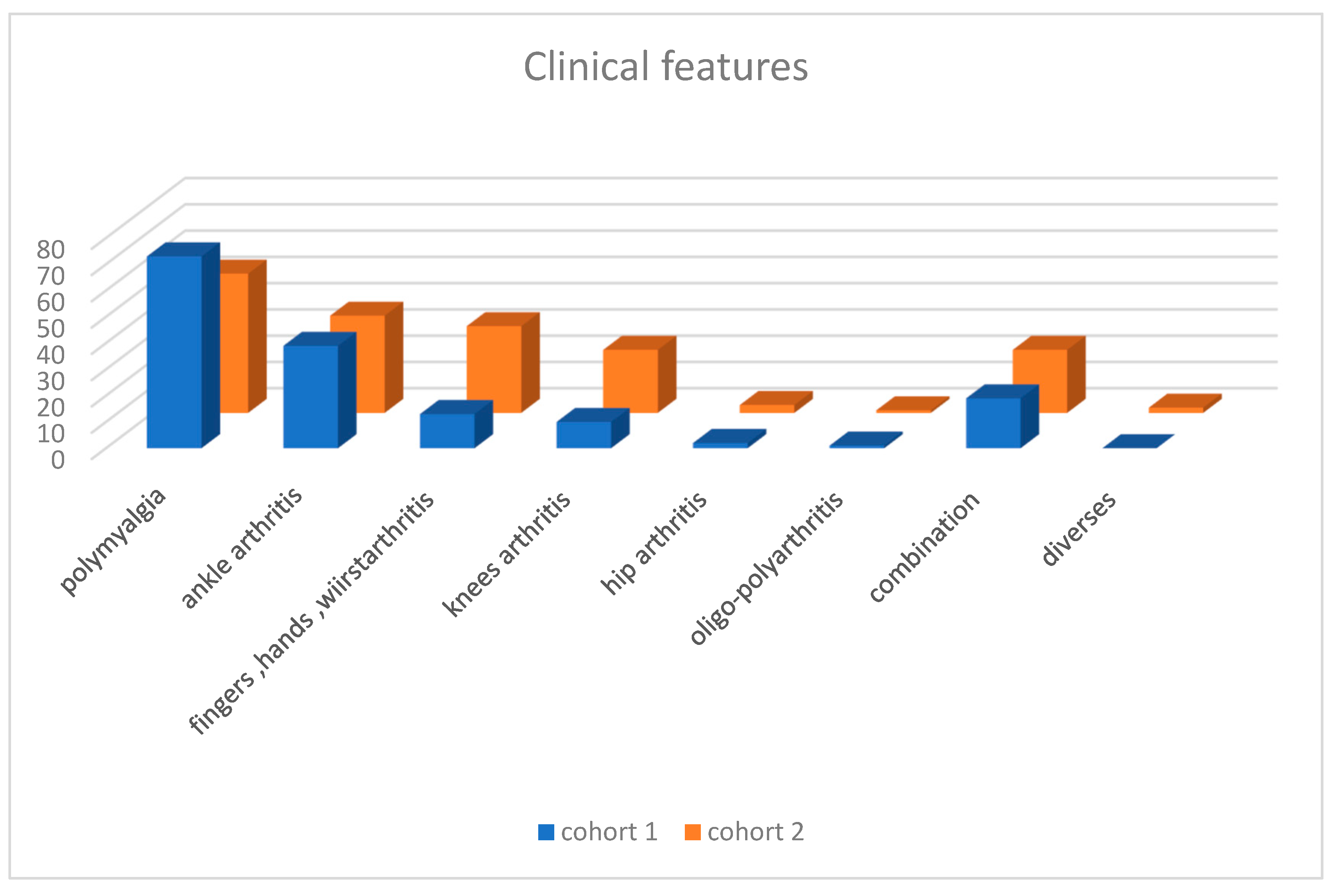
| Polymyalgia | Ankle Arthritis | Fingers Hands Wrist | Knees Arthritis | Hips Arthritis | Ploy—Oligo Arthritis | Combination | Diverse | |
|---|---|---|---|---|---|---|---|---|
| Cohort 1 | 73 | 38 + 1 | 13 | 9 + 1 | 2 | 1 | 19 | 0 |
| Cohort 2 | 53 | 37 | 33 | 15 + 9 | 3 | 1 | 24 | 2 |
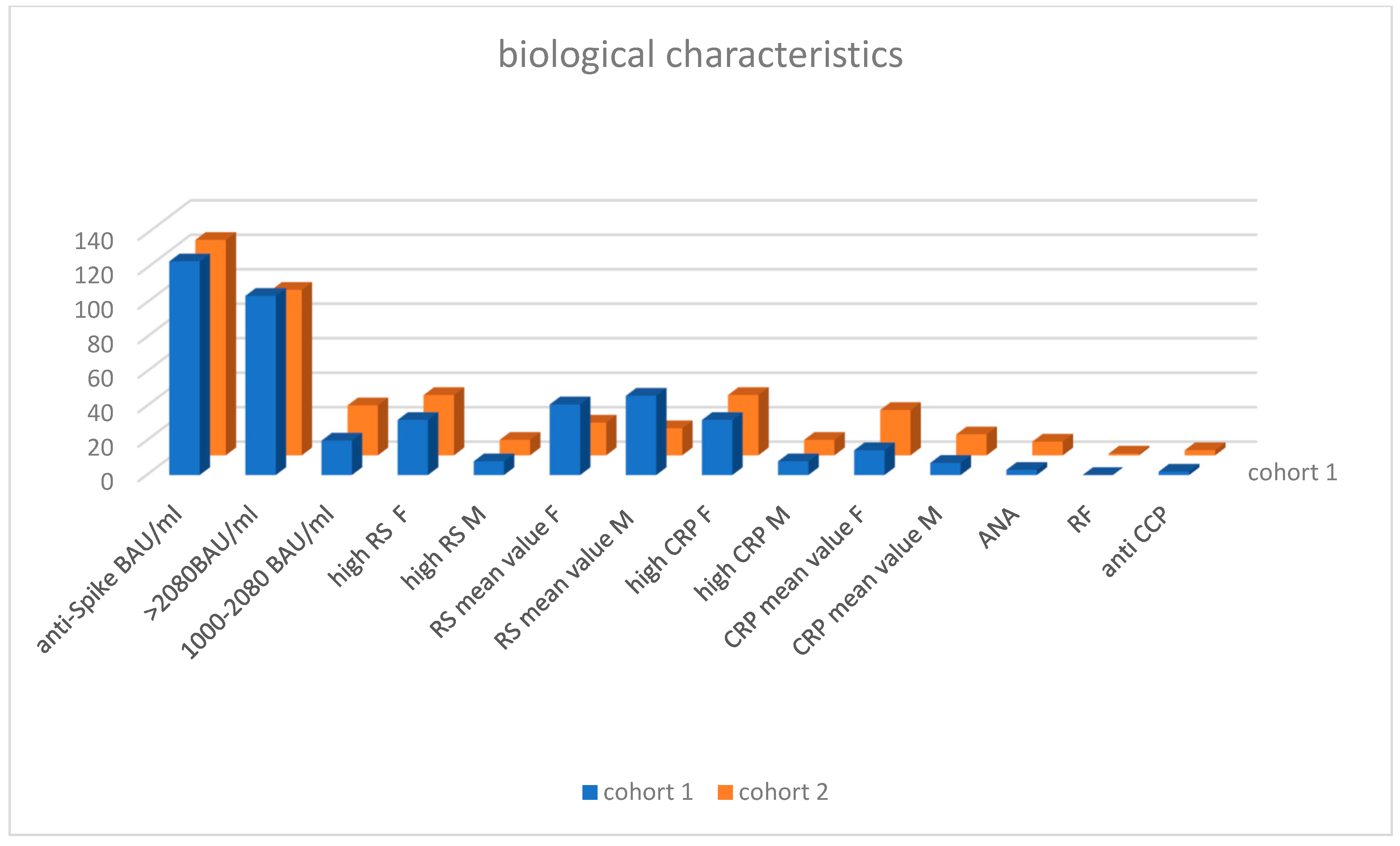
| Anti-Spike BAU/mL | High SR mm/h Patient/Mean Value | High CRP mg/L Patient/Mean Value | ANA | RF | Anti CCP | ||||
|---|---|---|---|---|---|---|---|---|---|
| >2080 | 1000–2080 | ||||||||
| Cohort 1 | 104 | 20/1318 | 32 F/41 mm/h | 8 M/46 mm/h | 32 F/14.6 mg/L | 8 M/26.3 mg/L | 3 | 0 | 2 |
| Cohort 2 | 96 | 29/1434 | 35 F/19 mm/h | 9 M/15.7 mm/h | 35 F/7.04 mg/L | 9 M/12.2 mg/L | 8 | 1 | 3 |
- Flare and new onset of sarcoidosis (Table 6)
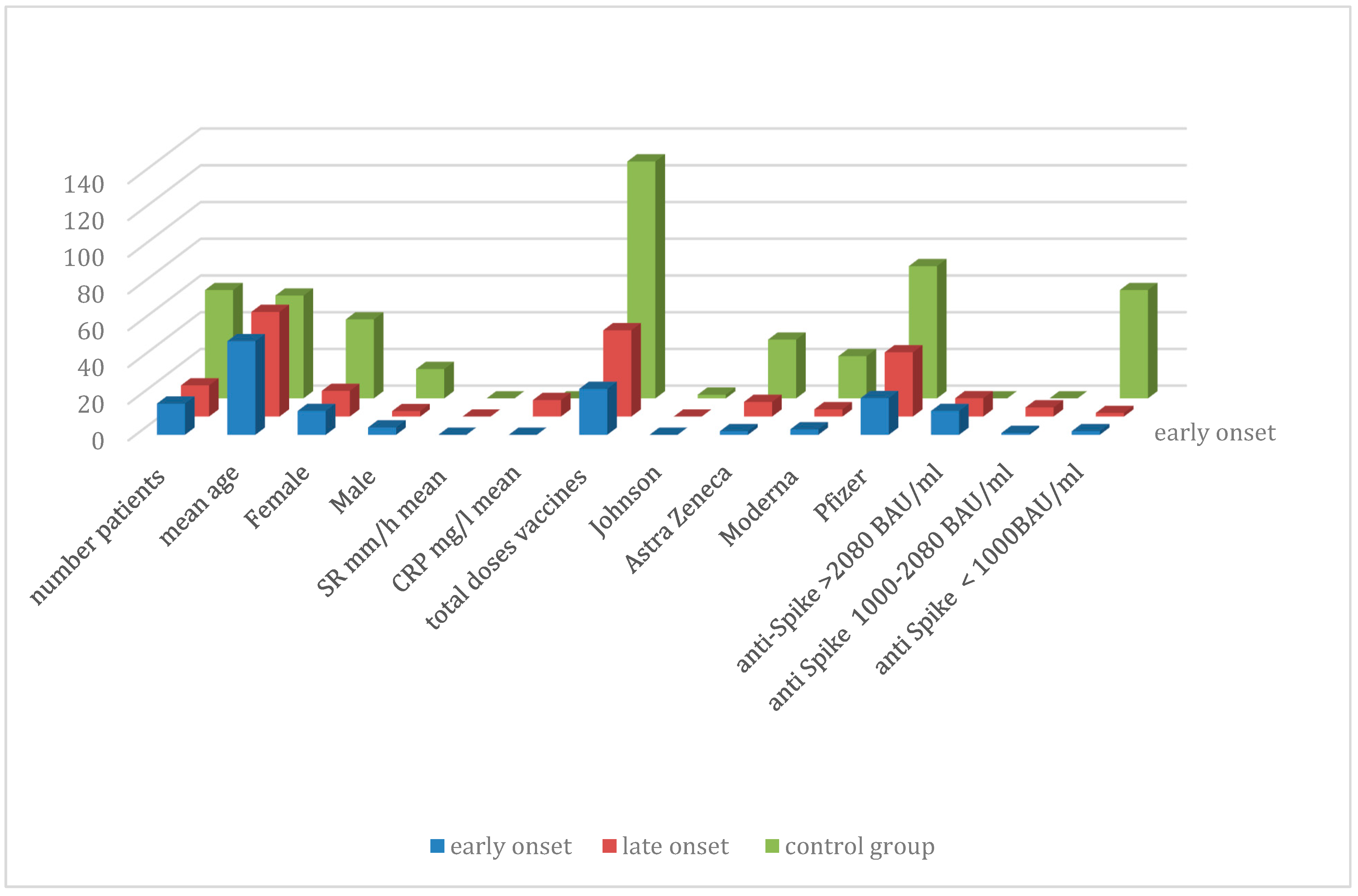
| Patients | VS/CRP | Number Vaccine Doses | Anti-Spike Antibodies BAU/mL | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | Gender | VS mm/h | CRP mg/L | Johnson | Astra Zeneca | Moderna | Pfizer | >2080 | 1000–2080 | <1000 | |
| 59 Control | 56 | 43 F/16 M | 2 | 32 | 23 | 72 | 0 | 0 | 59 | ||
| 17 Early | 51.8 | 13 F/4 M | 27.7 (3–85) | 23.7 (2–69) | 0 | 2 | 3 | 20 | 13 | 1 | 2 |
| 17 Late | 57.1 | 14 F/3 M | 26.6 (2–73) | 9 (2–52) | 0 | 8 | 4 | 35 | 10 | 5 | 2 |
| Case | Sex/Age | Ethnic | Vaccine | Clinical Features | ESR (mm/h)/CRP (mg/L) | SarsCov2 S IGG AB (Delay) |
|---|---|---|---|---|---|---|
| 1 | F/48 | Caucasian | Pfizer × 2 | Ankle R + L | 73/4 | >2080 (17 months) |
| 2 | F/75 | Caucasian | Pfizer × 3 | Ankle R + L | 48/9 | >2080 (19 months) |
| 3 | M/60 | Caucasian | Pfizer × 3 | Ankle R + L | 7/2 | 1300 (22 months) |
| 4 | F/52 | Caucasian | Pfizer × 3 | Ankle R + L | 22/4 | >2080 (13 months) |
| 5 | F/53 | Caucasian | Pfizer × 3 | Ankle R + L | 15/2 | 425 (15 months) |
| 6 | M/50 | Caucasian | Pfizer × 3 | Ankle R + L | 26/21 | >2080 (13 months) |
| 7 | F/80 | Caucasian | Moderna × 3 | Ankle R + L | 30/04 | >2080 (16 months) |
| 8 | F/74 | Caucasian | Pfizer × 3 | Ankle R + L | 11/52 | >2080 (15 months) |
| 9 | F/54 | Caucasian | AZ × 2 | Ankle R + L | 39/15 | 1280 (22 months) |
| 10 | F/68 | Caucasian | AZ × 2 Pfizer × 1 | Ankle R + L Knee R | 21/02 | 1680 (17 months) |
| 11 | F/55 | Caucasian | Pfizer × 2 | Ankle R + L | 39/4 | >2080 (25 months) |
| 12 | M/69 | Caucasian | AZ × 2 Pfizer × 2 | Ankle R + L | 6/2 | 641 (8 months) |
| 13 | F/39 | Asian | Pfizer × 2 Moderna × 1 | Ankle R + L | 30/06 | >2080 (17 months) |
| 14 | F/48 | African | Pfizer × 2 | Ankle R + L | 56/8 | 1530 (20 months) |
| 15 | F/38 | African | Pfizer × 3 | Ankle R + L | 19/10 | 1550 (11 months) |
| 16 | F/49 | African | AZ × 2 Pfizer × 1 | Ankle R + L | 2/6 | >2080 (19 months) |
| 17 | F/57 | Caucasian | Pfizerx2Moderna × 1 | Ankle R + L Knee R + L | 9/3 | >2080 (21 months) |
| Age | Gender | Ethnic | Biology | Anti-Spike BAU/mL | Clinical | Vaccine | Delay | ||
|---|---|---|---|---|---|---|---|---|---|
| SR mm/h | CRP mg/L | ||||||||
| 1 | 27 | F | Black African | 27 | 16 | >2080 | Ankle L + R | Moderna × 2 | 7 days |
| 2 | 66 | F | Black African | 44 | 17 | 1780 | Ankle L + R | AZ × 2 | 5 days |
| 3 | 38 | F | Black African | 6 | 4 | >2080 | Ankle L + R | Pfizer × 2 | 7 days |
| 4 | 33 | F | Maghreban | 50 | 24 | >2080 | Ankle L + R and mediastinal lymphadenopathy | Pfizer × 2 | 3 months |
| 5 | 43 | M | Black African | 32 | 24 | 1250 | Ankle L + R | Moderna × 2 | >6 months |
| 6 | 48 | F | Black African | 20 | 2 | >2080 | Ankle L + R | Pfizer × 2 | Unknown |
4. Example of Longitudinal Case Studies
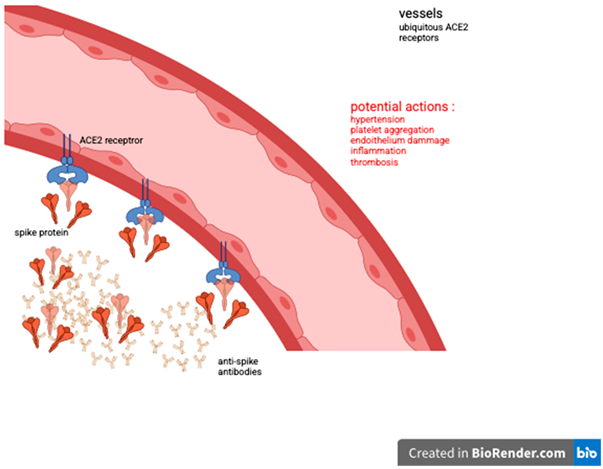
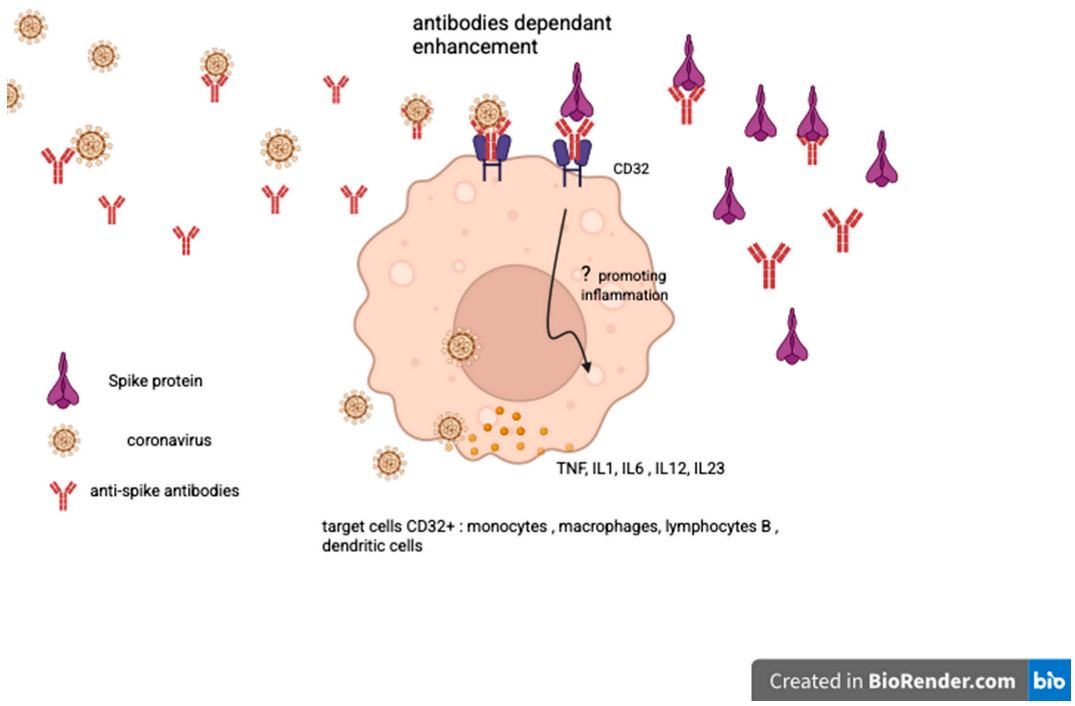
5. Discussion
Bradford Hill Criteria
6. Conclusions
7. Post Scriptum
8. Illustrations

Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Polak, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Pérez Marc, G.; Moreira, E.D.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 mRNA COVID-19 Vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef]
- Baden, L.R.; El Sahly, H.M.; Essink, B.; Kotloff, K.; Frey, S.; Novak, R.; Diemert, D.; Spector, S.A.; Rouphael, N.; Creech, C.B.; et al. Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. N. Engl. J. Med. 2021, 384, 403–416. [Google Scholar] [CrossRef] [PubMed]
- Unal Enginar, A. Arthritis following COVID-19 vaccination: Report of two cases. Int. Immunopharmacol. 2021, 101, 108256. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-C.; Chen, C.-J. New onset inflammatory arthritis after COVID-19 vaccination: A systematic review. Int. J. Rheum. Dis. 2023, 26, 267–277. [Google Scholar] [CrossRef]
- Solis, O.; Beccari, A.R.; Iaconis, D.; Talarico, C.; Ruiz-Bedoya, C.A.; Nwachukwu, J.C.; Cimini, A.; Castelli, V.; Bertini, R.; Montopoli, M.; et al. The SARS-CoV-2 spike protein binds and modulates estrogen receptors. Sci. Adv. 2022, 8, eadd4150. [Google Scholar] [CrossRef]
- Cosentino, M.; Marino, F. Understanding the pharmacology of COVID-19 mRNA vaccines: Playing dice with Spike? Int. J. Mol. Sci. 2022, 23, 10881. [Google Scholar] [CrossRef]
- Sun, Z.; Brodsky, J.L. Protein quality control in the secretory pathway. J. Cell Biol. 2019, 218, 3171–3187. [Google Scholar] [CrossRef]
- Pal, A.; Roongta, R.; Mondal, S.; Sinha, D.; Sinhamahapatra, P.; Ghosh, A.; Chattopadhyay, A. Does post-COVID reactive arthritis exist? Experience of a tertiary care centre with a review of the literature. Rheumatol. Clin. 2023, 19, 67–73. [Google Scholar] [CrossRef]
- Wang, S.-F.; Tseng, S.-P.; Yen, C.-H.; Yang, J.-Y.; Tsao, C.-H.; Shen, C.-W.; Chen, K.-H.; Liu, F.-T.; Liu, W.-T.; Chen, Y.-M.A.; et al. Antibody-dependent SARS coronavirus infection is mediated by antibodies against spike proteins. Biochem. Biophys. Res. Commun. 2014, 451, 208–214. [Google Scholar] [CrossRef]
- Hasan, A.; Al-Mullab, M.R.; Abubakerc, J.; Al-Mulla, F. Early insight into antibody-dependent enhancement after SARS-CoV-2 mRNA vaccination. Hum. Vaccines Immunother. 2021, 17, 4121–4125. [Google Scholar] [CrossRef]
- Scholkmann, F.; May, C.-A. COVID-19, post-acute COVID-19 syndrome (PACS, “long COVID”) and post-COVID-19 vaccination syndrome (PCVS, “post-COVIDvac-syndrome”): Similarities and differences. Pathol.—Res. Pract. 2023, 246, 154497. [Google Scholar] [CrossRef] [PubMed]
- Abramenko, N.; Vellieux, F.; Tesařová, P.; Kejík, Z.; Kaplánek, R.; Lacina, L.; Dvořánková, B.; Rösel, D.; Brábek, J.; Tesař, A.; et al. Estrogen Receptor Modulators in Viral Infections Such as SARS-CoV-2: Therapeutic Consequences. Int. J. Mol. Sci. 2021, 22, 6551. [Google Scholar] [CrossRef]
- Izuka, S.; Komai, T.; Natsumoto, B.; Shoda, H.; Fujio, K. Self-limited Polymyalgia Rheumatica-like Syndrome Following mRNA-1273 SARS-CoV-2 Vaccination. Intern. Med. 2022, 61, 903–906. [Google Scholar] [CrossRef] [PubMed]
- Jarrot, P.-A.; Mirouse, A.; Ottaviani, S.; Cadiou, S.; Salmon, J.H.; Liozon, E.; Parreau, S.; Michaud, M.; Terrier, B.; Gavand, P.E.; et al. Polymyalgia rheumatica and giant cell arteritis following COVID-19 vaccination: Results from a nationwide survey. Hum. Vaccines Immunother. 2024, 20, 2334084. [Google Scholar] [CrossRef]
- Halma, M.T.J.; Plothe, C.; Marik, P.; Lawrie, T.A. Strategies for the Management of Spike Protein-Related Pathology. Microorganisms 2023, 11, 1308. [Google Scholar] [CrossRef]
- Golstein, M.A.; Fagnard, O.; Steinfeld, S.D. Reactive arthritis after COVID 19 vaccination: 17 cases. Rheumatology 2023, 62, 3706–3709. [Google Scholar] [CrossRef]
- Zeidler, H.; Hudson, A.P. Reactive Arthritis Update: Spotlight on New and Rare Infectious Agents Implicated as Pathogens. Curr. Rheumatol. Rep. 2021, 23, 53. [Google Scholar] [CrossRef] [PubMed]
- Abhishek, A.; de Pablo, P.; Cader, M.Z.; Buckley, C.D.; Raza, K.; Filer, A. Diagnostic outcomes associated with ankle synovitis in early inflammatory arthritis: A cohort study. Clin. Exp. Rheumatol. 2014, 32, 533–538. [Google Scholar]
- Li, X.; Tong, X.; Yin Yeung, W.W.; Kuan, P.; Hin Hei Yum, S.; Ling Chui, C.S.; Lai, F.T.T.; Wan, E.Y.F.; Wong, C.K.H.; Chan, E.W.Y.; et al. Two-dose COVID-19 vaccination and possible arthritis flare among patients with rheumatoid arthritis in Hong Kong. Ann. Rheum. Dis. 2022, 81, 564–568. [Google Scholar] [CrossRef]
- Matsuo, T.; Honda, H.; Tanaka, T.; Uraguchi, K.; Kawahara, M.; Hagiya, H. COVID-19 mRNA Vaccine–Associated Uveitis Leading to Diagnosis of Sarcoidosis: Case Report and Review of Literature. J. Investig. Med. High Impact Case Rep. 2022, 10, 23247096221086450. [Google Scholar] [CrossRef]
- Tokumasu, K.; Fujita-Yamashita, M.; Sunada, N.; Sakurada, Y.; Yamamoto, K.; Nakano, Y.; Matsuda, Y.; Otsuka, Y.; Hasegawa, T.; Hagiya, H.; et al. Characteristics of Persistent Symptoms Manifested after SARS-CoV-2 Vaccination: An Observational Retrospective Study in a Specialized Clinic for Vaccination-Related Adverse Events. Vaccines 2023, 11, 1661. [Google Scholar] [CrossRef]
- Chen, Y.; Xu, Z.; Wang, P.; Li, X.M.; Shuai, Z.W.; Ye, D.Q.; Pan, H.F. New-onset autoimmune phenomena post COVID-19 vaccination. Immunology 2022, 165, 386–401. [Google Scholar]
- Yonker, L.M.; Swank, Z.; Bartsch, Y.C.; Burns, M.D.; Kane, A.; Boribong, B.; Davis, J.P.; Loiselle, M.; Novak, T.; Senussi, Y.; et al. Circulating Spike Protein Detected in Post-COVID-19 mRNA Vaccine Myocarditis. Circulation 2023, 147, 867–876. [Google Scholar] [CrossRef]
- Pla-Prats, C.; Thomä, N.H. Quality control of protein complex assembly by the ubiquitin–proteasome system. Trends Cell Biol. 2022, 32, 696–706. [Google Scholar] [CrossRef] [PubMed]
- Khoury, J.; Najjar-Debbiny, R.; Hanna, A.; Jabbour, A.; Abu Ahmad, Y.; Saffuri, A.; Abu-Sinni, M.; Shkeiri, R.; Elemy, A.; Hakim, F. Vaccine long term immune decline and breakthrough infections. Vaccine 2021, 39, 6984–6989. [Google Scholar] [CrossRef]
- Sousa Silva, M.F.; Matias Dinelly Pinto, A.C.; de Cassia Evangelista de Oliveira, F.; Freire Caetano, L.; Montenegro de Carvalho Araujo, F.; Gambim Fonseca, M.H. Antibody response 6 months after booster dose of Pfizer in previous recipients of CoronaVac. J. Med. Virol. 2023, 95, e28169. [Google Scholar] [CrossRef]
- Zhang, L.; Richards, A.; Immaculada Barrasa, M.; Hughes, S.H.; Young, R.A.; Jaenisch, R. Reverse-transcriptase SARS-CoV-2 RNA can integrate into the genome of cultured human cells and can be expressed in patient-derived tissues. Proc. Natl. Acad. Sci. USA 2021, 118, e2105968118. [Google Scholar] [CrossRef]
- Alden, M.; Olofsson Falla, F.; Yang, D.; Barghouth, M.; Luan, C.; Rasmussen, M.; De Marinis, Y. Intracellular Reverse Transcription of Pfizer BioNTech COVID-19 mRNA Vaccine BNT162b2 In Vitro in Human Liver Cell Line. Curr. Issues Mol. Biol. 2022, 44, 1115–1126. [Google Scholar] [CrossRef] [PubMed]
- Crowley, S.D.; Rudemiller, N.P. Immunologic Effects of Renin-Angiotensin System. J. Am. Soc. Nephrol. 2017, 28, 1350–1361. [Google Scholar] [CrossRef] [PubMed]
- Aboudounya, M.M.; Heads, R.J. COVID-19 and Toll-Like Receptor 4 (TLR4): SARS-CoV-2 May Bind and Activate TLR4 to Increase ACE2 Expression, Facilitating Entry and Causing Hyperinflammation. Mediat. Inflamm. 2021, 2021, 8874339. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Golstein, M.A. Post-COVID-19 Vaccine Hyperproduction of Anti-Spike Antibodies and Rheumatological Manifestations. Vaccines 2025, 13, 1028. https://doi.org/10.3390/vaccines13101028
Golstein MA. Post-COVID-19 Vaccine Hyperproduction of Anti-Spike Antibodies and Rheumatological Manifestations. Vaccines. 2025; 13(10):1028. https://doi.org/10.3390/vaccines13101028
Chicago/Turabian StyleGolstein, Marc Alexandre. 2025. "Post-COVID-19 Vaccine Hyperproduction of Anti-Spike Antibodies and Rheumatological Manifestations" Vaccines 13, no. 10: 1028. https://doi.org/10.3390/vaccines13101028
APA StyleGolstein, M. A. (2025). Post-COVID-19 Vaccine Hyperproduction of Anti-Spike Antibodies and Rheumatological Manifestations. Vaccines, 13(10), 1028. https://doi.org/10.3390/vaccines13101028





