The Influence of SARS-CoV-2 Vaccination on the Mortality and Outcomes of Patients with Both Myocardial Infarction and COVID-19
Abstract
1. Introduction
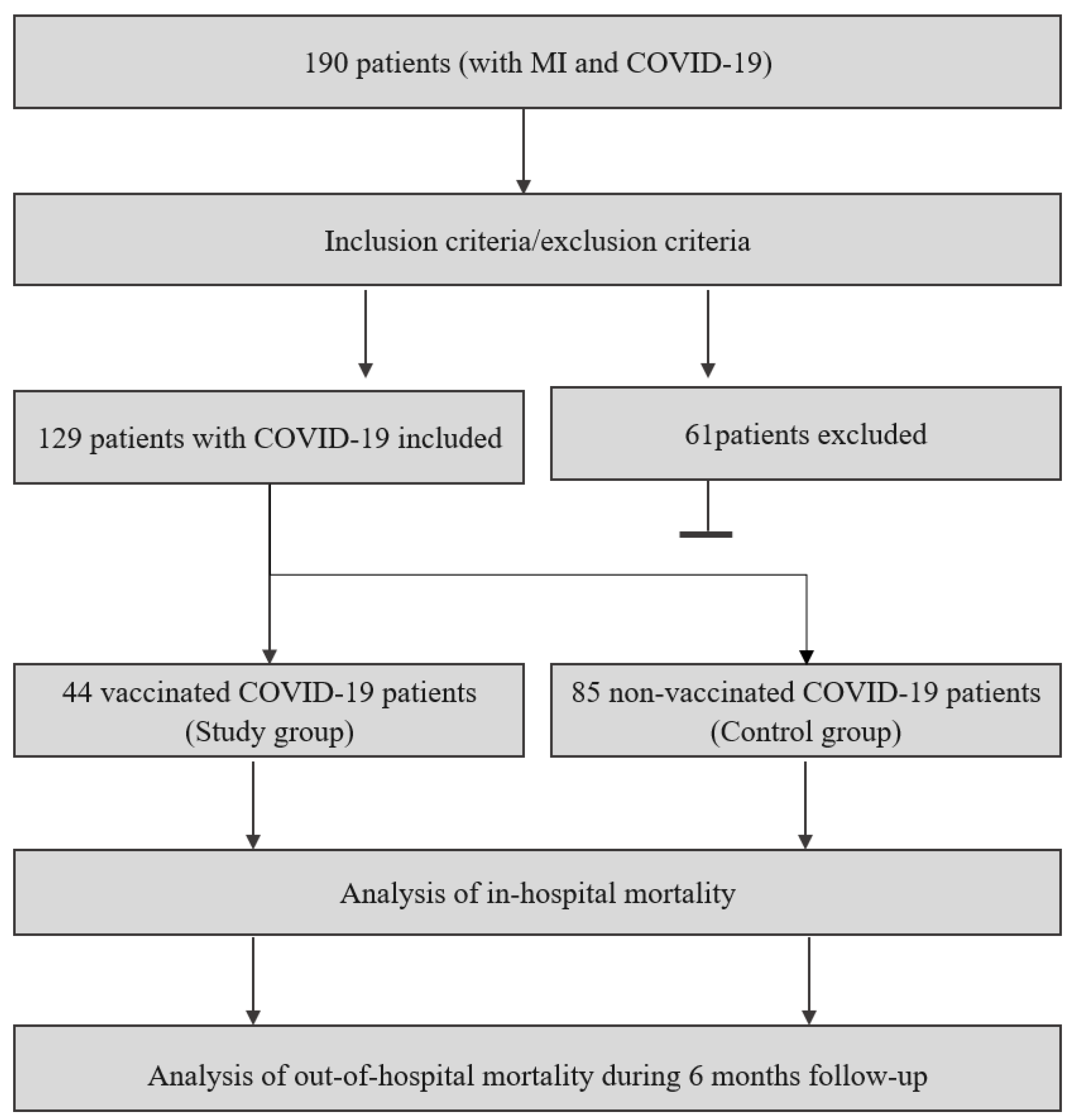
2. Materials and Methods
2.1. Study Group
- Confirmed MI, according to the ESC Fourth Universal Definition of Myocardial Infarction [33];
- Confirmed COVID-19 based on a PCR-positive test;
- Verified vaccination status with government-approved vaccines;
- Available after discharge a minimum observation period of 1 month (for patients who were discharged to allow us to create reasonable follow-up);
- Age > 18 years.
- Any coexisting disease potentially limiting lifetime during observation (e.g., end-stage organ failure or end-stage cancer);
- Lack of primary clinical data necessary for groups comparison, e.g., glomerular filtration rate (GFR) or ejection fraction (EF).
2.2. Study Outcomes
2.3. Methods
2.4. Statical Analysis and Utilized Software
2.5. Rationale for Study Design
3. Results
3.1. Study Group
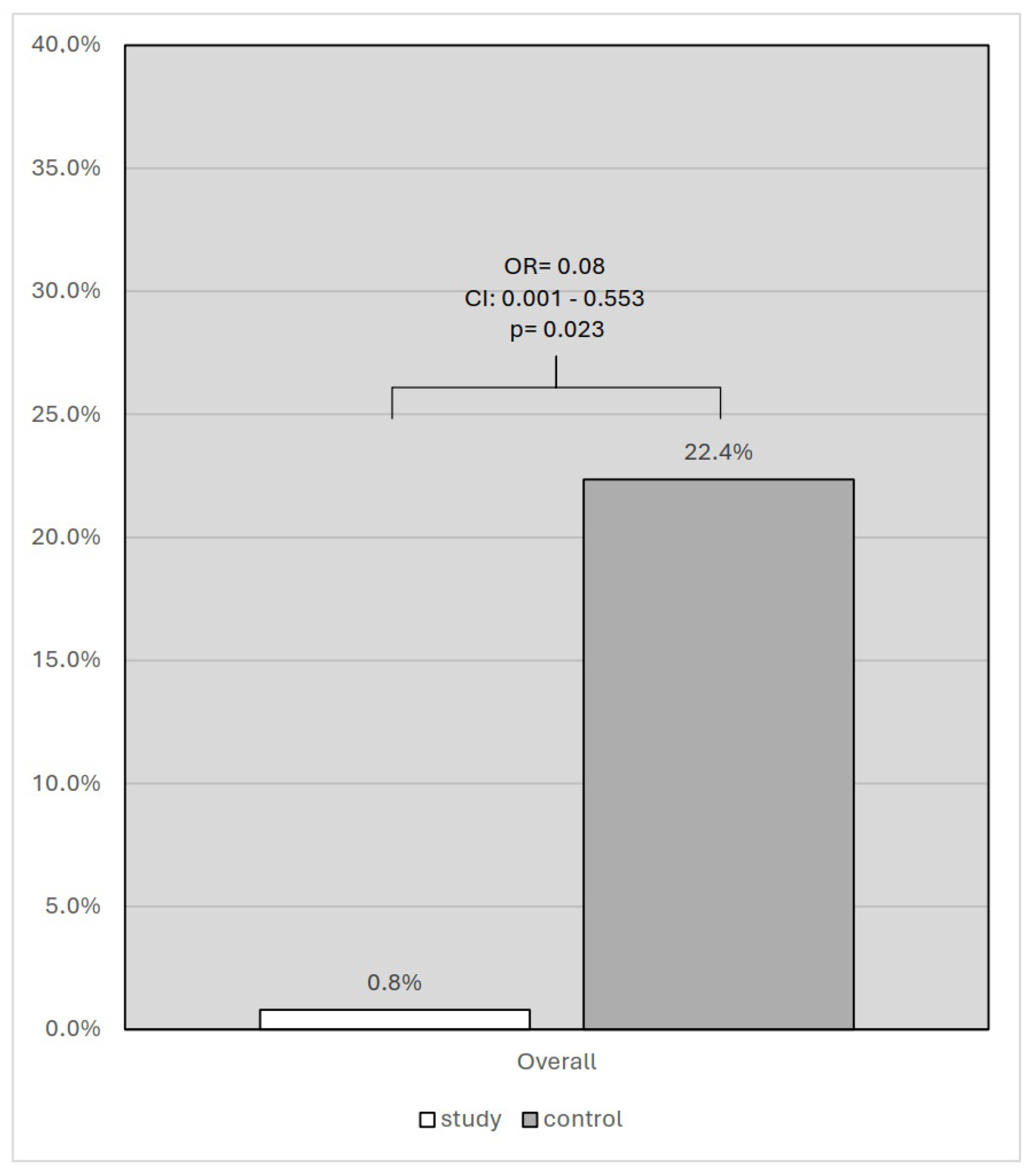
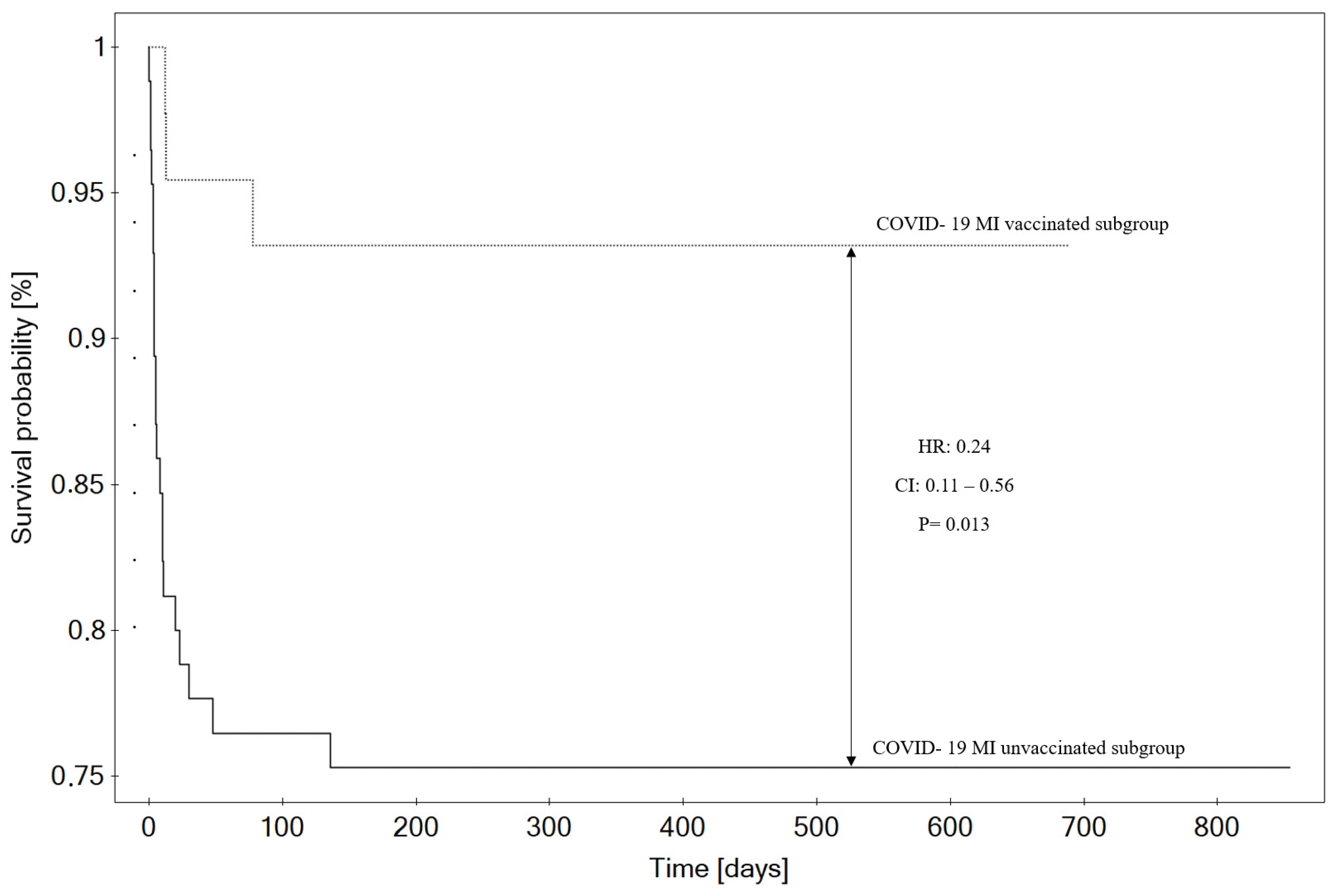
3.2. Mortality
4. Discussion
5. Study Limitations
6. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wang, S.Y.; Seghieri, C.; Vainieri, M.; Groene, O. Changes in Acute Myocardial Infarction, Stroke, and Heart Failure Hospitalizations during COVID-19 Pandemic in Tuscany-An Interrupted Time Series Study. Int. J. Public Health 2022, 67, 1604319. [Google Scholar] [CrossRef] [PubMed]
- Griewing, S.; Gremke, N.; Kreutz, J.; Schieffer, B.; Timmermann, L.; Markus, B. Chronological Development of Cardiovascular Disease in Times of COVID-19: A Retrospective Analysis of Hospitalized Diseases of the Circulatory System and COVID-19 Patients of a German University Hospital. J. Cardiovasc. Dev. Dis. 2022, 9, 325. [Google Scholar] [CrossRef] [PubMed]
- Gylfason, A.D.; Bjarnason, A.; Helgason, K.O.; Rognvaldsson, K.G.; Armannsdottir, B.; Gudmundsdottir, I.J.; Gottfredsson, M. Effects of the COVID-19 pandemic and associated non-pharmaceutical interventions on diagnosis of myocardial infarction and selected infections in Iceland 2020. Laeknabladid 2022, 108, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Zeymer, U.; Ahmadli, V.; Schneider, S.; Werdan, K.; Weber, M.; Hohenstein, S.; Hindricks, G.; Desch, S.; Bollmann, A.; Thiele, H. Effects of the COVID-19 Pandemic on Acute Coronary Syndromes in Germany during the First Wave: The COVID-19 Collateral Damage Study. Clin. Res. Cardiol. 2023, 112, 539–549. [Google Scholar] [CrossRef] [PubMed]
- Pourasghari, H.; Tavolinejad, H.; Soleimanpour, S.; Abdi, Z.; Arabloo, J.; Bragazzi, N.L.; Behzadifar, M.; Rashedi, S.; Omidi, N.; Ayoubian, A.; et al. Hospitalization, Major Complications and Mortality in Acute Myocardial Infarction Patients during the COVID-19 Era: A Systematic Review and Meta-Analysis. Int. J. Cardiol. Heart Vasc. 2022, 41, 101058. [Google Scholar] [CrossRef]
- Schmitz, T.; Meisinger, C.; Kirchberger, I.; Thilo, C.; Amann, U.; Baumeister, S.E.; Linseisen, J. Impact of COVID-19 Pandemic Lockdown on Myocardial Infarction Care. Eur. J. Epidemiol. 2021, 36, 619–627. [Google Scholar] [CrossRef]
- Choi, H.; Lee, J.H.; Park, H.K.; Lee, E.; Kim, M.S.; Kim, H.J.; Park, B.E.; Kim, H.N.; Kim, N.; Jang, S.Y.; et al. Impact of the COVID-19 Pandemic on Patient Delay and Clinical Outcomes for Patients With Acute Myocardial Infarction. J. Korean Med. Sci. 2022, 37, e167. [Google Scholar] [CrossRef] [PubMed]
- Janke, A.T.; Gettel, C.J.; Haimovich, A.; Kocher, K.E.; Krumholz, H.M.; Venkatesh, A.K. Changes in Emergency Department Arrival Times for Acute Myocardial Infarction During the COVID-19 Pandemic Suggest Delays in Care Seeking. Circ. Cardiovasc. Qual. Outcomes 2022, 15, e008402. [Google Scholar] [CrossRef]
- Sturkenboom, H.N.; van Hattem, V.A.E.; Nieuwland, W.; Paris, F.M.A.; Magro, M.; Anthonio, R.L.; Algin, A.; Lipsic, E.; Bruwiere, E.; Van den Branden, B.J.L.; et al. COVID-19-Mediated Patient Delay Caused Increased Total Ischaemic Time in ST-Segment Elevation Myocardial Infarction. Neth. Heart J. 2022, 30, 96–105. [Google Scholar] [CrossRef]
- McNamara, D.A.; VanOosterhout, S.; Klungle, D.; Busman, D.; Parker, J.L.; Kampfschulte, A.; Jovinge, S.; Wohns, D.; Madder, R.D. Pandemic-Associated Delays in Myocardial Infarction Presentation in Predominantly Rural Counties With Low COVID-19 Prevalence. Am. J. Cardiol. 2022, 169, 18–23. [Google Scholar] [CrossRef]
- Granström, J.; Lantz, P.; Lidin, M.; Wahlström, M.; Nymark, C. Perceptions of Delay When Afflicted by an Acute Myocardial Infarction during the First Wave of the COVID-19 Pandemic. Eur. J. Cardiovasc. Nurs. 2023, 22, 89–97. [Google Scholar] [CrossRef]
- Kobayashi, S.; Sakakura, K.; Jinnouchi, H.; Taniguchi, Y.; Tsukui, T.; Watanabe, Y.; Yamamoto, K.; Seguchi, M.; Wada, H.; Fujita, H. Comparison of Door-to-Balloon Time and in-Hospital Outcomes in Patients with ST-Elevation Myocardial Infarction between before versus after COVID-19 Pandemic. Cardiovasc. Interv. Ther. 2022, 37, 641–650. [Google Scholar] [CrossRef] [PubMed]
- Mao, Q.; Zhao, J.; Li, Y.; Xie, L.; Xiao, H.; Wang, K.; Qiu, Y.; Chen, J.; Xu, Q.; Xu, Z.; et al. Impact of COVID-19 Pandemic on Mechanical Reperfusion in ST-Segment-Elevation Myocardial Infarction Undergoing Primary Percutaneous Coronary Intervention: A Multicenter Retrospective Study From a Non-Epicenter Region. Front. Cardiovasc. Med. 2021, 8, 698923. [Google Scholar] [CrossRef] [PubMed]
- Budrys, P.; Lizaitis, M.; Cerlinskaite-Bajore, K.; Bajoras, V.; Rodevic, G.; Martinonyte, A.; Dieckus, L.; Badaras, I.; Serpytis, P.; Gurevicius, R.; et al. Increase of Myocardial Ischemia Time and Short-Term Prognosis of Patients with Acute Myocardial Infarction during the First COVID-19 Pandemic Wave. Medicina 2021, 57, 1296. [Google Scholar] [CrossRef]
- Tokarek, T.; Dziewierz, A.; Zeliaś, A.; Malinowski, K.P.; Rakowski, T.; Dudek, D.; Siudak, Z. Impact of COVID-19 Pandemic on Patients with ST-Segment-Elevation Myocardial Infarction Complicated by Out-of-Hospital Cardiac Arrest. Int. J. Environ. Res. Public Health 2022, 20, 337. [Google Scholar] [CrossRef]
- Lechner, I.; Reindl, M.; Tiller, C.; Holzknecht, M.; Troger, F.; Fink, P.; Mayr, A.; Klug, G.; Bauer, A.; Metzler, B.; et al. Impact of COVID-19 Pandemic Restrictions on ST-Elevation Myocardial Infarction: A Cardiac Magnetic Resonance Imaging Study. Eur. Heart J. 2022, 43, 1141–1153. [Google Scholar] [CrossRef] [PubMed]
- Katsoularis, I.; Fonseca-Rodríguez, O.; Farrington, P.; Lindmark, K.; Fors Connolly, A.-M. Risk of Acute Myocardial Infarction and Ischaemic Stroke Following COVID-19 in Sweden: A Self-Controlled Case Series and Matched Cohort Study. Lancet 2021, 398, 599–607. [Google Scholar] [CrossRef]
- Saad, M.; Kennedy, K.F.; Imran, H.; Louis, D.W.; Shippey, E.; Poppas, A.; Wood, K.E.; Abbott, J.D.; Aronow, H.D. Association Between COVID-19 Diagnosis and In-Hospital Mortality in Patients Hospitalized with ST-Segment Elevation Myocardial Infarction. JAMA 2021, 326, 1940–1952. [Google Scholar] [CrossRef]
- Little, C.D.; Kotecha, T.; Candilio, L.; Jabbour, R.J.; Collins, G.B.; Ahmed, A.; Connolly, M.; Kanyal, R.; Demir, O.M.; Lawson, L.O.; et al. COVID-19 Pandemic and STEMI: Pathway Activation and Outcomes from the Pan-London Heart Attack Group. Open Heart 2020, 7, e001432. [Google Scholar] [CrossRef]
- Choudry, F.A.; Hamshere, S.M.; Rathod, K.S.; Akhtar, M.M.; Archbold, R.A.; Guttmann, O.P.; Woldman, S.; Jain, A.K.; Knight, C.J.; Baumbach, A.; et al. High Thrombus Burden in Patients With COVID-19 Presenting With ST-Segment Elevation Myocardial Infarction. J. Am. Coll. Cardiol. 2020, 76, 1168–1176. [Google Scholar] [CrossRef]
- Garcia, S.; Dehghani, P.; Grines, C.; Davidson, L.; Nayak, K.R.; Saw, J.; Waksman, R.; Blair, J.; Akshay, B.; Garberich, R.; et al. Initial Findings From the North American COVID-19 Myocardial Infarction Registry. J. Am. Coll. Cardiol. 2021, 77, 1994–2003. [Google Scholar] [CrossRef] [PubMed]
- Kite, T.A.; Ludman, P.F.; Gale, C.P.; Wu, J.; Caixeta, A.; Mansourati, J.; Sabate, M.; Jimenez-Quevedo, P.; Candilio, L.; Sadeghipour, P.; et al. International Prospective Registry of Acute Coronary Syndromes in Patients With COVID-19. J. Am. Coll. Cardiol. 2021, 77, 2466–2476. [Google Scholar] [CrossRef] [PubMed]
- Choudry, F.A.; Rathod, K.S.; Baumbach, A.; Mathur, A.; Jones, D.A. Long-Term Outcomes of COVID-19-Associated ST-Elevation Myocardial Infarction Treated With Primary PCI. Cardiovasc. Revascularization Med. 2022, 43, 133–135. [Google Scholar] [CrossRef] [PubMed]
- Dehghani, P.; Schmidt, C.W.; Garcia, S.; Okeson, B.; Grines, C.L.; Singh, A.; Patel, R.A.G.; Wiley, J.; Htun, W.W.; Nayak, K.R.; et al. North American COVID-19 Myocardial Infarction (NACMI) Risk Score for Prediction of In-Hospital Mortality. J. Soc. Cardiovasc. Angiogr. Interv. 2022, 1, 100404. [Google Scholar] [CrossRef]
- Hrycek, E.; Walawska-Hrycek, A.; Hamankiewicz, M.; Milewski, K.; Nowakowski, P.; Buszman, P.; Żurakowski, A. The Influence of SARS-CoV-2 Infection on Acute Myocardial Infarction Outcomes. J. Clin. Med. 2023, 12, 5899. [Google Scholar] [CrossRef] [PubMed]
- Fedeli, U.; Casotto, V.; Barbiellini Amidei, C.; Vianello, A.; Guarnieri, G. COPD-Related Mortality before and after Mass COVID-19 Vaccination in Northern Italy. Vaccines 2023, 11, 1392. [Google Scholar] [CrossRef]
- Tylicki, L.; Biedunkiewicz, B.; Puchalska-Reglińska, E.; Gellert, R.; Burnier, M.; Wolf, J.; Dȩbska-Ślizień, A. COVID-19 Vaccination Reduces Mortality in Patients on Maintenance Hemodialysis. Front. Med. 2022, 9, 937167. [Google Scholar] [CrossRef]
- Shields, A.M.; Tadros, S.; Al-Hakim, A.; Nell, J.M.; Lin, M.M.N.; Chan, M.; Goddard, S.; Dempster, J.; Dziadzio, M.; Patel, S.Y.; et al. Impact of Vaccination on Hospitalization and Mortality from COVID-19 in Patients with Primary and Secondary Immunodeficiency: The United Kingdom Experience. Front. Immunol. 2022, 13, 984376. [Google Scholar] [CrossRef]
- Rivera, J.C.H.H.; Mendoza, M.S.; Covarrubias, L.G.; Ramírez, A.L.Q.; Reyes, L.C.; Hernández, M.B.; Martínez, J.R.; Contla, Y.P.; Durán, J.M.V.; Rivas, A.T.; et al. Mortality Due to COVID-19 in Renal Transplant Recipients, Related to Variants of SARS-CoV-2 and Vaccination in Mexico. Transplant. Proc. 2022, 54, 1434–1438. [Google Scholar] [CrossRef]
- Liu, S.; Jiang, C.; Liu, Y.; Zhang, Y.; Qiu, X.; Luo, J.; Xu, Y.; Wang, J. The Effectiveness of COVID–19 Vaccination against All–Cause Mortality in Patients with Type 2 Diabetes Mellitus: The Observation during the Initial Period of the Cancellation of the “Dynamic Zero Policy” in Mainland China. Diabetes Res. Clin. Pract. 2023, 200, 110694. [Google Scholar] [CrossRef]
- Pellegrino, R.; Pellino, G.; Selvaggi, L.; Selvaggi, F.; Federico, A.; Romano, M.; Gravina, A.G. BNT162b2 mRNA COVID-19 Vaccine Is Safe in a Setting of Patients on Biologic Therapy with Inflammatory Bowel Diseases: A Monocentric Real-Life Study. Expert Rev. Clin. Pharmacol. 2022, 15, 1243–1252. [Google Scholar] [CrossRef]
- Li, H.; Ping, F.; Li, X.; Wang, Z.; Xiao, J.; Jiang, H.; Xue, Y.; Quan, J.; Yao, H.; Zheng, X.; et al. COVID-19 Vaccine Coverage, Safety, and Perceptions among Patients with Diabetes Mellitus in China: A Cross-Sectional Study. Front. Endocrinol. 2023, 14, 1172089. [Google Scholar] [CrossRef] [PubMed]
- ESC Guidelines—Fourth Universal Definition of Myocardial Infarction. Available online: https://www.escardio.org/Guidelines/Clinical-Practice-Guidelines/Fourth-Universal-Definition-of-Myocardial-Infarction (accessed on 12 August 2024).
- Peduzzi, P.; Concato, J.; Feinstein, A.R.; Holford, T.R. Importance of Events per Independent Variable in Proportional Hazards Regression Analysis. II. Accuracy and Precision of Regression Estimates. J. Clin. Epidemiol. 1995, 48, 1503–1510. [Google Scholar] [CrossRef]
- Alharbi, A.; Franz, A.; Alfatlawi, H.; Wazzan, M.; Alsughayer, A.; Eltahawy, E.; Assaly, R. Impact of COVID-19 Pandemic on the Outcomes of Acute Coronary Syndrome. Curr. Probl. Cardiol. 2023, 48, 101575. [Google Scholar] [CrossRef] [PubMed]
- Kontos, M.C.; Rennyson, S.L.; Chen, A.Y.; Alexander, K.P.; Peterson, E.D.; Roe, M.T. The Association of Myocardial Infarction Process of Care Measures and In-Hospital Mortality: A Report from the NCDR®. Am. Heart J. 2014, 168, 766–775. [Google Scholar] [CrossRef]
- Liu, B.; Stepien, S.; Dobbins, T.; Gidding, H.; Henry, D.; Korda, R.; Mills, L.; Pearson, S.-A.; Pratt, N.; Vajdic, C.M.; et al. Effectiveness of COVID-19 Vaccination against COVID-19 Specific and All-Cause Mortality in Older Australians: A Population Based Study. Lancet Reg. Health West. Pac. 2023, 40, 100928. [Google Scholar] [CrossRef]
- Abhilash, K.P.P.; Mathiyalagan, P.; Krishnaraj, V.R.K.; Selvan, S.; Kanagarajan, R.; Reddy, N.P.; Rajendiran, N.; Hazra, D.; Gunasekaran, K.; Moorthy, M.; et al. Impact of Prior Vaccination with CovishieldTM and Covaxin® on Mortality among Symptomatic COVID-19 Patients during the Second Wave of the Pandemic in South India during April and May 2021: A Cohort Study. Vaccine 2022, 40, 2107–2113. [Google Scholar] [CrossRef]
- Baker, T.B.; Bolt, D.M.; Smith, S.S.; Piasecki, T.M.; Conner, K.L.; Bernstein, S.L.; Hayes-Birchler, T.; Theobald, W.E.; Fiore, M.C. The Relationship of COVID-19 Vaccination with Mortality Among 86,732 Hospitalized Patients: Subpopulations, Patient Factors, and Changes over Time. J. Gen. Intern. Med. 2023, 38, 1248–1255. [Google Scholar] [CrossRef]
- Ikeokwu, A.E.; Lawrence, R.; Osieme, E.D.; Gidado, K.M.; Guy, C.; Dolapo, O. Unveiling the Impact of COVID-19 Vaccines: A Meta-Analysis of Survival Rates Among Patients in the United States Based on Vaccination Status. Cureus 2023, 15, e43282. [Google Scholar] [CrossRef]
- Grapsa, E.; Adamos, G.; Andrianopoulos, I.; Tsolaki, V.; Giannakoulis, V.G.; Karavidas, N.; Giannopoulou, V.; Sarri, K.; Mizi, E.; Gavrielatou, E.; et al. Association Between Vaccination Status and Mortality Among Intubated Patients With COVID-19-Related Acute Respiratory Distress Syndrome. JAMA Netw. Open 2022, 5, e2235219. [Google Scholar] [CrossRef] [PubMed]
- Jagadeesh, N.; Gnany, J.; Kapadi, S.; Koshy, N.; Shaw, D. COVID-19 Vaccination: Does It Alter Postoperative Mortality and Morbidity in Hip Fractures? Cureus 2022, 14, e32688. [Google Scholar] [CrossRef] [PubMed]
- Lerner, A.H.; Arvanitis, P.; Vieira, K.; Klein, E.J.; Farmakiotis, D. mRNA Vaccination Decreases COVID-19-Associated Morbidity and Mortality Among Organ Transplant Recipients: A Contemporary Cohort Study. Open Forum Infect. Dis. 2022, 9, ofac503. [Google Scholar] [CrossRef]
- Sezen, Y.I.; Senoglu, S.; Karabela, S.N.; Yesilbag, Z.; Borcak, D.; Canbolat Unlu, E.; Korkusuz, R.; Ozdemir, Y.; Kart Yasar, K. Risk Factors and the Impact of Vaccination on Mortality in COVID-19 Patients. BLL 2022, 123, 440–443. [Google Scholar] [CrossRef] [PubMed]
- Gül, F.; Kasapoğlu, U.S.; Sabaz, M.S.; Ay, P.; Oktay, B.D.; Çalışkan, G.; Demir, N.; Sayan, İ.; Kabadayı, F.; Altuntaş, G.; et al. The Impact of CoronaVac Vaccination on 28-Day Mortality Rate of Critically Ill Patients with COVID-19 in Türkiye. Balk. Med. J. 2023, 40, 435–444. [Google Scholar] [CrossRef]
- Stepanova, M.; Lam, B.; Younossi, E.; Felix, S.; Ziayee, M.; Price, J.; Pham, H.; de Avila, L.; Terra, K.; Austin, P.; et al. The Impact of Variants and Vaccination on the Mortality and Resource Utilization of Hospitalized Patients with COVID-19. BMC Infect. Dis. 2022, 22, 702. [Google Scholar] [CrossRef] [PubMed]
- Muthukrishnan, J.; Vardhan, V.; Mangalesh, S.; Koley, M.; Shankar, S.; Yadav, A.K.; Khera, A. Vaccination Status and COVID-19 Related Mortality: A Hospital Based Cross Sectional Study. Med. J. Armed Forces India 2021, 77, S278–S282. [Google Scholar] [CrossRef] [PubMed]
- Hoxha, I.; Agahi, R.; Bimbashi, A.; Aliu, M.; Raka, L.; Bajraktari, I.; Beqiri, P.; Adams, L.V. Higher COVID-19 Vaccination Rates Are Associated with Lower COVID-19 Mortality: A Global Analysis. Vaccines 2022, 11, 74. [Google Scholar] [CrossRef]
- Matveeva, O.; Shabalina, S.A. Comparison of Vaccination and Booster Rates and Their Impact on Excess Mortality during the COVID-19 Pandemic in European Countries. Front. Immunol. 2023, 14, 1151311. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-T. Effect of Vaccination Patterns and Vaccination Rates on the Spread and Mortality of the COVID-19 Pandemic. Health Policy Technol. 2023, 12, 100699. [Google Scholar] [CrossRef]
- Mendoza-Cano, O.; Trujillo, X.; Huerta, M.; Ríos-Silva, M.; Guzmán-Esquivel, J.; Lugo-Radillo, A.; Benites-Godínez, V.; Bricio-Barrios, J.A.; Cárdenas-Rojas, M.I.; Ríos-Bracamontes, E.F.; et al. Assessing the Influence of COVID-19 Vaccination Coverage on Excess Mortality across 178 Countries: A Cross-Sectional Study. Vaccines 2023, 11, 1294. [Google Scholar] [CrossRef]
- Shah, S.; Paudel, K.; Bhattarai, A.; Thapa, S.; Bhusal, S.; Adhikari, Y.R.; Adhikari, T.B.; Bhatta, N.; Mandal, P.; Sharma, P.; et al. Association of Vaccination Status with the Clinicobiochemical Profile, Hospital Stay, and Mortality in COVID-19: A Case–Control Study. Health Sci. Rep. 2023, 6, e1579. [Google Scholar] [CrossRef] [PubMed]
- Marchand, G.; Masoud, A.T.; Medi, S. Risk of All-Cause and Cardiac-Related Mortality after Vaccination against COVID-19: A Meta-Analysis of Self-Controlled Case Series Studies. Hum. Vaccines Immunother. 2023, 19, 2230828. [Google Scholar] [CrossRef] [PubMed]
| Study Group (n = 44) | Control Group (n = 85) | p | |
|---|---|---|---|
| Male, n (%) | 32 (72.73%) | 59 (69.41%) | 0.70 |
| STEMI, n (%) | 15 (34.09%) | 43 (50.59%) | 0.08 |
| Age, years | 67 (60–75) | 71 (61–76.5) | 0.36 |
| EF, % | 45 (35–50) | 50 (40–55) | 0.053 |
| GFR, mL/min | 78.8 (56–95.77) | 74.39 (47.77–97.92) | 0.67 |
| Diabetes, n (%) | 13 (29.55%) | 23 (27.06%) | 0.77 |
| Hypertension, n (%) | 31 (70.45%) | 60 (70.59%) | 0.99 |
| Hyperlipidemia, n (%) | 27 (61.36%) | 36 (42.35%) | 0.05 |
| Smoking, n (%) | 8 (18.18%) | 14 (16.47%) | 0.81 |
| Peripheral arterial disease, n (%) | 2 (4.55%) | 1 (1.18%) | 0.23 |
| Obesity, n (%) | 3 (6.82%) | 12 (14.12%) | 0.22 |
| Previous stroke, n (%) | 3 (6.82%) | 6 (7.06%) | 0.96 |
| Atrial fibrillation, n (%) | 6 (13.64%) | 14 (16.47%) | 0.68 |
| Myocardial infarction, n (%) | 11 (25%) | 13 (15.29%) | 0.18 |
| Previous PTCA, n (%) | 8 (18.18%) | 11 (12.94%) | 0.43 |
| Previous CABG, n (%) | 5 (11.36%) | 1 (1.18%) | 0.01 |
| Time from vaccination to COVID-19, days | 257 (201.5–294.5) |
| Study Group (n = 44) | Control Group (n = 85) | p | |
|---|---|---|---|
| Coronarography, n (%) | 43 (97.73%) | 82 (96.47%) | 0.70 |
| Optimal medical therapy, n (%) | 1 (2.27%) | 3 (3.53%) | 0.70 |
| Coronary artery bypass grafting qualified, n (%) | 6 (13.64%) | 3 (3.53%) | 0.03 |
| Percutaneous transluminal coronary angioplasty, n (%) | 32 (72.73%) | 73 (85.88%) | 0.07 |
| Reached TIMI 3, n (%) | 30 (93.75%) | 62 (84.93%) | 0.15 |
| Multivessel coronary artery disease, n (%) | 16 (36.36%) | 15 (17.65%) | 0.02 |
| Left main coronary artery, n (%) | 1 (2.27%) | 2 (2.35%) | 0.73 |
| Left anterior descending artery, n (%) | 13 (29.55%) | 25 (29.41%) | 0.99 |
| Diagonal branches, n (%) | 3 (6.82%) | 2 (2.35%) | 0.21 |
| Circumflex artery, n (%) | 4 (9.09%) | 7 (8.24%) | 0.87 |
| Obtuse marginal artery, n (%) | 2 (4.55%) | 3 (3.53%) | 0.78 |
| Right coronary artery, n (%) | 7 (15.91%) | 21 (24.71%) | 0.25 |
| Posterior descending artery, n (%) | 0 (0%) | 0 (0%) | |
| Intermediate artery, n (%) | 0 (0%) | 1 (1.18%) | 0.47 |
| Bridge, n (%) | 1 (2.27%) | 1 (1.18%) | 0.64 |
| Stent length, mm | 32.5 (23.25–57.5) | 32 (21.5–48) | 0.45 |
| Staged revascularization *, n (%) | 4 (9.09%) | 1 (1.18%) | 0.03 |
| Study Group (n = 44) | Control Group (n = 85) | p | |
|---|---|---|---|
| Cardiogenic shock, n (%) | 3 (6.82%) | 11 (12.94%) | 0.32 |
| Pulmonary edema, n (%) | 5 (11.36%) | 5 (5.88%) | 0.30 * |
| Respiratory failure, n (%) | 0 (0%) | 14 (16.47%) | 0.02 * |
| Contrast-induced nephropathy, n (%) | 3 (6.82%) | 11 (12.94%) | 0.29 |
| Stroke, n (%) | 0 (0%) | 0 (0%) | |
| Bleeding requiring transfusion, n (%) | 0 (0%) | 4 (4.71%) | 0.30 * |
| Hospitalization time (days) | 10.67 ± 8.78 | 9.13 ± 5.62 | 0.29 |
| Univariable Cox Regression | Multivariable Cox Regression | |||||||
|---|---|---|---|---|---|---|---|---|
| Parameter | HR | −95% CI | +95% CI | p | HR | −95% CI | +95% CI | p |
| Vaccination | 0.11 | 0.01 | 0.86 | 0.036 | 0.10 | 0.01 | 0.77 | 0.026 |
| Sex | 1.33 | 0.48 | 3.71 | 0.584 | ||||
| Diabetes | 2.39 | 0.99 | 5.78 | 0.052 | 2.76 | 1.14 | 6.66 | 0.024 |
| GFR, mL/min | 0.98 | 0.97 | 1.00 | 0.101 | ||||
| EF, % | 0.96 | 0.91 | 1.00 | 0.063 | ||||
| Age, years | 1.02 | 0.99 | 1.06 | 0.206 | ||||
| MI type (STEMI vs. NSTEMI) | 0.76 | 0.30 | 1.09 | 0.56 | ||||
| Year of pandemic (1–3) | 0.58 | 0.28 | 1.18 | 0.12 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hrycek, E.; Walawska-Hrycek, A.; Milewski, K.; Nowakowski, P.; Buszman, P.; Żurakowski, A. The Influence of SARS-CoV-2 Vaccination on the Mortality and Outcomes of Patients with Both Myocardial Infarction and COVID-19. Vaccines 2024, 12, 983. https://doi.org/10.3390/vaccines12090983
Hrycek E, Walawska-Hrycek A, Milewski K, Nowakowski P, Buszman P, Żurakowski A. The Influence of SARS-CoV-2 Vaccination on the Mortality and Outcomes of Patients with Both Myocardial Infarction and COVID-19. Vaccines. 2024; 12(9):983. https://doi.org/10.3390/vaccines12090983
Chicago/Turabian StyleHrycek, Eugeniusz, Anna Walawska-Hrycek, Krzysztof Milewski, Przemysław Nowakowski, Piotr Buszman, and Aleksander Żurakowski. 2024. "The Influence of SARS-CoV-2 Vaccination on the Mortality and Outcomes of Patients with Both Myocardial Infarction and COVID-19" Vaccines 12, no. 9: 983. https://doi.org/10.3390/vaccines12090983
APA StyleHrycek, E., Walawska-Hrycek, A., Milewski, K., Nowakowski, P., Buszman, P., & Żurakowski, A. (2024). The Influence of SARS-CoV-2 Vaccination on the Mortality and Outcomes of Patients with Both Myocardial Infarction and COVID-19. Vaccines, 12(9), 983. https://doi.org/10.3390/vaccines12090983






