Abstract
Given the increase in COVID-19 emergency department visits and hospitalizations during the winter of 2023–2024, identifying groups that have a high prevalence of COVID-19 cases, severity, and long-term symptoms can help increase efforts toward reducing disparities and prevent severe COVID-19 outcomes. Using data from the 2022 National Health Interview Survey (n = 27,651), we assessed the prevalence of COVID-19 outcomes (prior diagnosis, moderate/severe COVID-19, and long COVID) by sociodemographic characteristics and factors associated with each COVID-19 outcome. Approximately one third of adults reported a prior COVID-19 diagnosis (30.7%), while one half (51.6%) who had COVID-19 reported moderate or severe symptoms, and one fifth (19.7%) who had COVID-19 symptoms reported long COVID. The following were associated with higher odds of moderate/severe COVID-19 and long COVID: havinga high-risk condition (aOR = 1.20, OR = 1.52); having anxiety or depression (OR = 1.46, OR = 1.49); having a disability (OR = 1.41, OR = 1.60); and having a food insecurity (OR = 1.37, OR = 1.50) compared to a lack of these conditions. Having two or more COVID-19 vaccinations was associated with lower odds of a COVID-19 diagnosis (OR = 0.75), moderate/severe COVID-19 (OR = 0.86), and long COVID (OR = 0.82). Improving vaccination coverage and reducing disparities in COVID-19 outcomes could advance health equities and protect against future resurgence of disease.
1. Introduction
While the Public Health Emergency for Coronavirus disease 2019 (COVID-19) ended in May 2023, effects of COVID-19 remain due to variant strains causing infection, severe symptoms, or long-term effects (“long COVID”) [1,2]. With an increase in COVID-19 disease activity from 19–25 November 2023, there was a 10% increase in emergency department visits and hospitalizations compared to the prior week [3]. Previous studies found that older adults, males, and those with underlying medical conditions were associated with more severe COVID-19 outcomes [4,5]. However, other factors associated with COVID-19 outcomes are still unknown, such as mental health, disability, and food insecurity. Many studies found that the pandemic exacerbated mental health conditions and food insecurity in the U.S. [6,7,8,9,10]. Furthermore, previous studies have found that these groups were more vulnerable to infection and severe health outcomes, and were less likely to get vaccinated against COVID-19 [11,12,13,14,15,16,17]. However, the association between sociodemographic and health-related factors and long COVID is not well understood. Understanding how COVID-19 outcomes differ by population subgroups may inform future vaccination communication strategies, including tailoring provider recommendations and increasing vaccine access for vulnerable groups.
The goal of this study is to examine factors associated with COVID-19 diagnosis, severity of symptoms, and long COVID among a nationally representative sample of U.S. adults in 2022. It is hypothesized that groups who are at high risk for severe COVID-19 may also be at high risk for long COVID, and that vulnerable groups such as those with mental health symptoms, disability, and food insecurity are at higher risk for severe COVID outcomes. Identifying groups that have high prevalence of COVID-19 cases, severity, and long-term symptoms can help increase efforts toward reducing disparities. Furthermore, assessing the association between COVID-19 vaccination and infection, severe symptoms, or long-term effects is needed to develop targeted strategies to increase vaccination confidence/uptake and early detection to prevent the severe consequences of COVID-19 for all adults.
2. Methods
2.1. Study Sample
The National Health Interview Survey (NHIS) is a cross-sectional, nationally representative household survey that is conducted by the Center for Disease Control and Prevention’s (CDC) of U.S. non-institutionalized adults ≥ 18 years. The dataset and questionnaires are publicly available at: https://www.cdc.gov/nchs/nhis/2022nhis.htm (accessed on 14 January 2024). The NHIS uses a complex sampling design to select a probability sample of households, and uses statistical measures such as stratification, clustering, and multistage sampling, as well as weighting, to ensure that estimates are representative of the U.S. population. In-person interviews were conducted with one adult aged ≥18 years, who was randomly selected to complete the survey, from each household. The adult sample size and response rate for the 2022 survey was 27,651 and 47.7%, respectively [18]. This study was reviewed by Emory University Sciences Institutional Review Board and determined to be not human subject research.
2.2. COVID-19 Outcomes
COVID-19 diagnosis was determined from the question, “Has a doctor or other health professional ever told you that you had or likely had coronavirus or COVID-19?” Among adults who were ever told they had COVID-19 or had ever tested positive for COVID-19, symptom severity was assessed by the following question: “How would you describe your coronavirus symptoms when they were at their worst?” Those who responded with “moderate” or “severe” symptoms were categorized as having moderate/severe symptoms while those who responded with “none” or “mild” were categorized as not having moderate/severe symptoms. This classification is based on the literature, which demonstrates that moderate/severe COVID typically refers to cases of COVID-19 that present significant symptoms and complications, potentially requiring intensive care unit (ICU) treatment and extracorporeal membrane oxygenation (ECMO) therapy [19]. Among adults who had experienced at least mild COVID-19 symptoms, long COVID was determined as an affirmative response to the following question: “Would you describe yourself as having ‘long COVID’, that is, you are still experiencing symptoms more than 3 months after you first had COVID-19, that are not explained by something else?”.
2.3. Health-Related Variables
People who are at high risk for severe COVID-19 were categorized as anyone who reported ever being told by a physician or other health professional they had cancer, asthma, chronic obstructive pulmonary disease, emphysema, chronic bronchitis, dementia, diabetes, coronary heart disease, hypertension, or stroke, or those who had any health condition or medical treatment or used any prescription medication that would weaken immune system [20]. While this is a comprehensive list, there may be other high-risk conditions not included here due to the limitations of the survey.
Smoking status was categorized into three groups: (1) Current smoker, which is defined as someone who has smoked at least 100 cigarettes in his/her lifetime and now smokes some days or every day; (2) Former smoker, which is defined as someone who has smoked at least 100 cigarettes in his/her lifetime and does not currently smoke; and (3) Never smoker, which is defined as someone who has not smoked 100 cigarettes in his/her lifetime.
Anxiety and depression were determined from questions that asked if the respondent had ever been told by a doctor or other health professional that they had any type of depression or if they had ever been told by a doctor or other health professional that they had any type of anxiety disorder. Disability was assessed by asking respondents if they have difficulty seeing (even with glasses), hearing (even with hearing aids), remembering or concentrating, understanding or being understood by others, walking or climbing stairs, or washing or dressing. Those who answered “a lot of difficulty” or “cannot do at all” to any of the previous choices were categorized as having a disability [21].
The food security status of the household was determined by responses to 10 food security questions that measured the households’ food situation based on the past 30 days. The NHIS survey recoded responses from these questions to form a food insecurity variable with three categories: food security, low food security, and very low food security. For this study, low and very low food security were coded as being food insecure.
Nativity was determined by asking respondents whether they were born in the United States or a U.S. territory. U.S. citizenship was defined as anyone who was born in in the U.S. or a U.S. territory. People were also asked whether they were citizens of the U.S.
Sociodemographic variables assessed were age, sex, race/ethnicity, educational status, poverty level (based on family income in relation to the federal poverty threshold), insurance status, and geographic region. Health care utilization was determined as having one or more places “that you usually go to if you are sick and need health care”. COVID-19 vaccination status was assessed by asking respondents whether they had received the COVID-19 vaccine and how many vaccinations they had received.
2.4. Statistical Analysis
To account for complex sample survey design and produce nationally representative estimates, weighted point estimates and 95% confidence intervals (CIs) were calculated using Stata v18. Sociodemographic characteristics were assessed for all adults in the sample. In addition, COVID-19 outcomes (prior diagnosis, moderate/severe COVID-19, and long COVID) were assessed overall and by each sociodemographic characteristic. Bivariate analyses compared the proportion of the COVID-19 outcomes by sociodemographic characteristics (e.g., age, sex, race/ethnicity, education, poverty level, health insurance, region, high risk, anxiety or depression, disability, food insecurity, U.S. nativity, citizenship status). Multivariable logistic regression was conducted to examine factors associated with each COVID-19 outcome [22]. Forest plots were presented for the results from multivariable logistic regression models. All sociodemographic variables were included in the model except health insurance status and citizenship status due to collinearity with other explanatory variables. All tests were two-tailed with the significance level set at α < 0.05. In multivariable regression models, an additional footnote was provided for all results with p < 0.001 to set a more stringent criteria for significant associations. Missing responses were low and accounted for 0–4.9% of all variables. Only significant results are presented in the text of this manuscript.
3. Results
In the sample, 50.9% of adults had a high-risk condition, 11.6% were current smokers, 23.9% had anxiety or depression, 9.3% had a disability, and 7.9% had food insecurity (Table 1). The majority of adults were born in the U.S. (81.6%) or were U.S. citizens (91.9%). Three quarters (75.1%) of adults had received two or more COVID-19 vaccinations.

Table 1.
Distribution of sociodemographic and other characteristics among adults, National Health Interview Survey, United States, 2022.
Approximately one third of adults reported a prior COVID-19 diagnosis (30.7%), while one half (51.6%) who had COVID-19 reported moderate or severe COVID-19, and one fifth (19.7%) who had COVID-19 symptoms reported having long COVID (Table 2). Moderate/severe COVID-19 was higher among younger adults (aged 18–59 years: 51.6–55.1%) compared to adults ≥ 65 years (44.1%) and females (55.1%) compared to males (47.7%). In addition, moderate/severe COVID-19 was higher among adults with a high-risk condition (53.9%) compared to those without (49.4%), those with anxiety or depression (61.5%) compared to those without (48.3%), those with a disability (61.6%) compared to those without (50.8%), and those with food insecurity (61.9%) compared to those without (50.8%). Similarly, long COVID was higher among adults with a high-risk condition (24.3%) compared to those without (15.4%), former smokers (22.5%) compared to never smokers (18.4%), those with anxiety or depression (28.0%) compared to those without (16.8%), those with a disability (33.7%) compared to those without (18.5%), and those with food insecurity (31.7%) compared to those without (18.5%). Lastly, long COVID was also higher among females (23.3%) compared to males (15.5%), those with lower educational attainment (e.g., high school diploma or some college: 20.4–22.6%) compared to those with a college degree or higher (15.4%), and those who were below poverty level (24.0%) compared to those who were at or above poverty level (19.3%).

Table 2.
Distribution of adults’ COVID-19 outcomes by sociodemographic characteristics, National Health Interview Survey, United States, 2022.
The odds of ever having COVID-19 were highest among younger age groups (e.g., 18–29 years: odds ratio [OR] = 2.67, 95%CI: 2.36, 3.01) compared to adults ≥ 65 years, females (OR = 1.11, 95%CI: 1.04, 1.19) compared to males, Hispanic adults (OR = 1.35, 95%CI: 1.22, 1.50) compared to non-Hispanic (NH) White adults, and those with a usual place for healthcare (OR = 1.60, 95% CI: 1.41, 1.81) compared to those without a usual place for healthcare (Table 3, Figure 1). NH Black adults were less likely to be diagnosed with COVID-19 (OR = 0.78, 95%CI: 0.70, 0.87) compared to NH White adults. The odds of ever having COVID-19 were higher among adults with a high-risk condition (OR = 1.24, 95%CI: 1.15, 1.33) compared to those without, and those who were former smokers (OR = 1.13, 95%CI: 1.05, 1.23) compared to never smokers.

Table 3.
Factors associated with adults’ COVID-19 outcomes, National Health Interview Survey, United States, 2022.
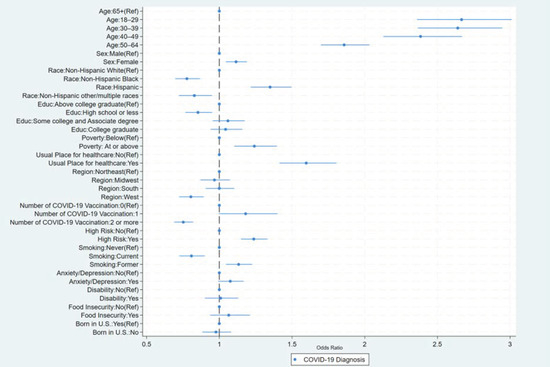
Figure 1.
Factors associated with adults’ COVID-19 diagnosis, National Health Interview Survey, United States, 2022.
The odds of having moderate/severe COVID-19 were higher among younger age groups (e.g., adults 40–49 years: OR = 1.67, 95%CI: 1.43, 1.95) compared to those ≥65 years, and females (OR = 1.25, 95%CI: 1.14, 1.38) compared to males; however, the odds of moderate/severe COVID-19 were lower for NH Black adults (OR = 0.75, 95%CI: 0.62, 0.90) compared to NH White adults (Table 3, Figure 2). In addition, the odds of having moderate/severe COVID-19 were higher for those who had a high-risk condition (OR = 1.20, 95% CI: 1.08, 1.33) compared to those who did not. Furthermore, the odds of having moderate/severe COVID-19 were highest among those who had anxiety or depression (OR = 1.46, 95%CI: 1.29, 1.65) compared to those who did not, those who have a disability (OR = 1.41, 95%CI: 1.14, 1.74) compared to those who did not, and those who had a food insecurity (OR = 1.37, 95%CI: 1.13, 1.67) compared to those who did not.

Figure 2.
Factors associated with adults’ moderate/severe COVID-19 symptoms, National Health Interview Survey, United States, 2022.
The odds of having long COVID were higher for adults 30–39 years (OR = 1.41, 95%CI: 1.13, 1.77), 40–49 years (OR = 1.42, 95%CI: 1.14, 1.77), and 50–59 years (OR = 1.38, 95%CI: 1.13, 1.68) compared to those ≥65 years, and were higher for females (OR = 1.51, 95%CI: 1.31, 1.73) compared to males (Table 3, Figure 3). Furthermore, the odds of having long COVID were higher for those with high-risk conditions (OR = 1.52, 95%CI: 1.31, 1.77) compared to those without, those with anxiety or depression (OR = 1.49, 95%CI: 1.28, 1.72) compared to those without, those with a disability (OR = 1.60, 95%CI: 1.28, 1.99) compared to those without, and those with food insecurity (OR = 1.50, 95%CI: 1.18, 1.91) compared to those without.
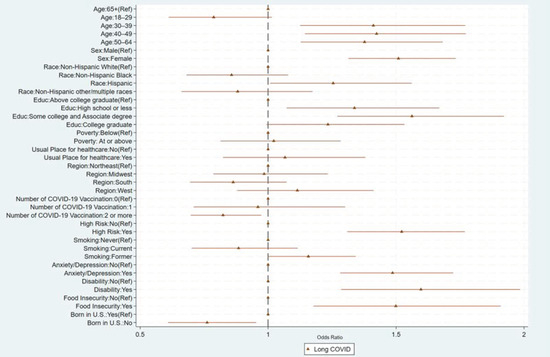
Figure 3.
Factors associated with adults’ long COVID, National Health Interview Survey, United States, 2022.
For all outcomes, having two or more COVID-19 vaccinations was associated with lower odds of a COVID-19 diagnosis (OR = 0.75, 95%CI: 0.69, 0.82), lower odds of moderate/severe COVID-19 (OR = 0.86, 95%CI: 0.75, 0.97), and lower odds of long COVID (OR = 0.82, 95%CI: 0.70, 0.97).
4. Discussion/Conclusions
This study found disparities in COVID-19 outcomes by sociodemographic characteristics and health-related variables. For example, females and adults with high-risk conditions were more likely to have negative health outcomes from COVID-19, such as having a prior diagnosis, more severe outcomes, or long COVID. Former smokers were also more likely to have a prior diagnosis or more severe outcomes than never smokers. Adults with anxiety or depression, a disability, or food insecurity were more likely to have severe outcomes and long COVID. This suggests further efforts, such as increased messaging and strategies to increase vaccination uptake and confidence, should be made to protect vulnerable populations from severe and long-term COVID-19 outcomes. Additionally, we suggest several populations for whom it may be beneficial to target early identification and treatment to prevent severe COVID-19 and long COVID-19.
While not a direct goal of this study, this study found that having two or more COVD-19 vaccines was negatively associated with COVID-19 diagnosis, severe disease, and long COVID, suggesting that receiving the completed primary series or booster vaccination provided greater protection than receiving incomplete or no vaccines. As a result, ensuring that people have access to vaccines and confidence in receiving all recommended vaccinations is important for them to protect themselves and their loved ones from severe health consequences. These results add to previous studies demonstrating the effectiveness of COVID-19 vaccines in reducing the severity of disease [23,24,25].
This study adds to the literature on disparities in COVID-19 outcomes by sociodemographic characteristics and high-risk groups. For example, this study found that females were more likely to have COVID-19 diagnoses, moderate/severe COVID-19, and long COVID than males. In addition, Hispanic adults were more likely to have COVID-19 diagnoses, whereas NH Black adults were less likely to be diagnosed or to have moderate/severe COVID-19 than NH White adults, suggesting potential barriers to healthcare resources. Finally, those with a high-risk condition, anxiety or depression, disability, or food insecurity were more likely to have moderate/severe COVID-19 and long COVID than those without, highlighting the disparities in COVID-19 outcomes among these vulnerable populations. These results could reflect differences in COVID-19 outcomes due to access to healthcare, hesitancy toward vaccines, or other barriers, which underscores the need for healthcare resources to diagnose, treat, and prevent severe outcomes. Furthermore, reducing the disparities in COVID-19 outcomes, particularly among vulnerable populations, is needed to prevent morbidity and mortality in groups who are most at risk for severe consequences from COVID-19.
This study found disparities in COVID-19 outcomes by age group, which is consistent with other nationally representative studies conducted in the U.S. While some studies found that older adults had the highest COVID-19 hospitalizations and severity [26,27], other studies found differences in adverse COVID-19 outcomes by age group. For example, a study in 2020 found that older U.S adults (≥85 years) had lower ICU admissions than those aged <65 years [28]. Another study conducted in 2021 found that U.S. adults aged ≥65 years were less likely to have ever had COVID-19 or emergency department visits due to COVID-19 than adults aged 18–49 years [29]. Christie et al. suggests that the decline in COVID-19 cases, emergency department visits, hospital admissions, and deaths among older adults from 2020 to 2021 was due to higher COVID-19 vaccination coverage among older adults, highlighting the potential benefits of rapidly increasing vaccination coverage. Since the NHIS data were collected in 2022, when vaccination coverage was high among older adults, and that the results were adjusted for vaccination status, the findings in this study were consistent with other nationally representative U.S. studies and reinforce the potential benefits of vaccination in protecting adults from severe COVID-19 outcomes.
While the COVID-19 Public Health Emergency has ended, much work is still needed to reduce the lingering effects of circulating variants and severe outcomes of COVID-19. Increased COVID-19 testing can help identify symptoms early so that treatment can be provided to prevent severe COVID-19. To reduce disparities in access to COVID-19 testing, the CDC’s Increasing Community Access to Testing (ICATT) program provides no-cost COVID-19 testing for people without health insurance with symptoms related to COVID-19 or who were exposed to someone with COVID-19 [30]. This program has been found to successfully increase access to COVID-19 testing in communities that are at greater risk, such as those with high transmission rates.
While studies have shown the effectiveness of COVID-19 vaccines in preventing the severe disease [24,31,32,33], the waning effectiveness of COVID-19 vaccines over time underscores the importance of being up to date with all COVID-19 vaccination doses for additional protection against infection, particularly for vulnerable populations who have a higher risk of severe COVID-19 outcomes [34,35,36,37]. Despite the Centers for Disease Control and Prevention (CDC)’s recommendations that all eligible individuals receive up-to-date COVID-19 vaccinations to protect against new COVID-19 variants [36], coverage for the booster vaccination is low in the U.S. (20.5% among adults as of May 2023) [38]. Several strategies can help to improve COVID-19 booster vaccination, such integrating vaccination in patient visits and medical practice procedures, recommending and increasing confidence in vaccines, and reducing barriers to access [39]. Targeted messaging and interventions can improve vaccination uptake and confidence, particularly among vulnerable populations, and protect all adults from the severe and long-term consequences of COVID-19.
The study is subject to a few limitations. First, because the NHIS is a cross-sectional study, causal inferences cannot be drawn. Second, COVID-19 vaccination statuses were based on self-reported data and were not verified by medical records; as a result, estimates may be affected by recall or social-desirability bias. Third, the high-risk medical conditions reported in this study were self-reported and were not inclusive of all high-risk conditions for COVID-19; as a result, they may be subject to misclassification. Fourth, COVID-19 outcomes, such as severity of disease and long COVID, may be subjective and may not reflect clinical definitions. However, the prevalence of long COVID found in this study is similar to that found in other national U.S. household surveys [40,41,42,43]. Fifth, there may be a potential for unobserved confounding (such as factors related to COVID-19 outcomes and the available covariates that were not captured) that may result in bias in the reported coefficients. Sixth, although more stringent criteria were used to assess significant associations in multivariable models, there is a possibility of false positives due to multiple comparisons. Finally, survey weighting adjustments may not adequately control for the differences in the vaccination statuses of survey respondents and nonrespondents since the survey completion rate was 47.7%.
Improving vaccination coverage and confidence can decrease the negative health consequences of COVID-19. Furthermore, reducing the disparities in COVID-19 outcomes, especially among people with underlying health conditions or food insecurity, could advance health equity and protect all from the serious and long-term consequences of COVID-19.
Author Contributions
K.H.N. conceptualized the study, interpreted the data, drafted the original manuscript, and revised and reviewed for critical content. Y.B. and S.C. analyzed and interpreted the data and reviewed for critical content. R.A.B. and L.V. conceptualized the study, interpreted the data, and revised and reviewed for critical content. L.C. conceptualized the study, supervised the analyses, interpreted the data, and revised and reviewed for critical content. All authors have read and agreed to the published version of the manuscript.
Funding
No funding was secured for this study. Laura Corlin was supported by Tufts University. Robert Bednarczyk was supported by National Cancer Institute (NCI) grant number R37 CA234119.
Institutional Review Board Statement
This study was reviewed by Emory University Sciences Institutional Review Board and determined to be not human subjects research.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data that support the findings of this study are openly available at https://www.cdc.gov/nchs/nhis/2022nhis.htm (accessed on 14 January 2024).
Conflicts of Interest
The authors declare no conflict of interest.
References
- WHO. Statement on the Fifteenth Meeting of the IHR (2005) Emergency Committee on the COVID-19 Pandemic. 2023. Available online: https://www.who.int/news/item/05-05-2023-statement-on-the-fifteenth-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-coronavirus-disease-(covid-19)-pandemic?adgroupsurvey={adgroupsurvey}&gclid=Cj0KCQjw8NilBhDOARIsAHzpbLBFHQNmP7_R2UD4_KXEmDslaE7EzLlsb6SMnkJIfIRYRRlQ-T83lBgaAiVNEALw_wcB (accessed on 14 January 2024).
- United Nations. WHO Chief Declares End to COVID-19 as a Global Health Emergency. 2023. Available online: https://news.un.org/en/story/2023/05/1136367 (accessed on 16 January 2024).
- CDC. COVID Data Tracker. 2023. Available online: https://covid.cdc.gov/covid-data-tracker/#datatracker-home (accessed on 21 February 2024).
- Gao, Y.D.; Ding, M.; Dong, X.; Zhang, J.J.; Kursat Azkur, A.; Azkur, D.; Gan, H.; Sun, Y.L.; Fu, W.; Li, W.; et al. Risk factors for severe and critically ill COVID-19 patients: A review. Allergy 2021, 76, 428–455. [Google Scholar] [CrossRef]
- Booth, A.; Reed, A.B.; Ponzo, S.; Yassaee, A.; Aral, M.; Plans, D.; Labrique, A.; Mohan, D. Population risk factors for severe disease and mortality in COVID-19: A global systematic review and meta-analysis. PLoS ONE 2021, 16, e0247461. [Google Scholar] [CrossRef] [PubMed]
- Cullen, W.; Gulati, G.; Kelly, B.D. Mental health in the COVID-19 pandemic. QJM 2020, 113, 311–312. [Google Scholar] [CrossRef]
- Rajkumar, R.P. COVID-19 and mental health: A review of the existing literature. Asian J. Psychiatr. 2020, 52, 102066. [Google Scholar] [CrossRef]
- Usher, K.; Durkin, J.; Bhullar, N. The COVID-19 pandemic and mental health impacts. Int. J. Ment. Health Nurs. 2020, 29, 315–318. [Google Scholar] [CrossRef]
- Wolfson, J.A.; Leung, C.W. Food Insecurity during COVID-19: An Acute Crisis with Long-Term Health Implications. Am. J. Public. Health 2020, 110, 1763–1765. [Google Scholar] [CrossRef] [PubMed]
- Niles, M.T.; Bertmann, F.; Belarmino, E.H.; Wentworth, T.; Biehl, E.; Neff, R. The Early Food Insecurity Impacts of COVID-19. Nutrients 2020, 12, 2096. [Google Scholar] [CrossRef] [PubMed]
- CDC. People with Certain Medical Conditions. 2022. Available online: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html (accessed on 14 January 2024).
- Nguyen, K.H.; Chen, S.; Morris, K.; Chui, K.; Allen, J.D. Mental health symptoms and association with COVID-19 vaccination receipt and intention to vaccinate among adults, United States. Prev. Med. 2022, 154, 106905. [Google Scholar] [CrossRef]
- Ryerson, A.B.; Rice, C.E.; Hung, M.C.; Patel, S.A.; Weeks, J.D.; Kriss, J.L.; Peacock, G.; Lu, P.J.; Asif, A.F.; Jackson, H.L.; et al. Disparities in COVID-19 Vaccination Status, Intent, and Perceived Access for Noninstitutionalized Adults, by Disability Status-National Immunization Survey Adult COVID Module, United States, May 30–June 26, 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1365–1371. [Google Scholar] [CrossRef]
- Testa, A.; Sharma, B.B. Food Insecurity and COVID-19 Vaccination Status and Vaccination Hesitancy in the United States. Fam. Community Health 2023, 46, 136–142. [Google Scholar] [CrossRef]
- Nguyen, K.H.; Irvine, S.; Epstein, R.; Allen, J.D.; Corlin, L. Prior COVID-19 Infection, Mental Health, Food and Financial Insecurity, and Association with COVID-19 Vaccination Coverage and Intent among College-Aged Young Adults, US, 2021. Prev. Chronic. Dis. 2021, 18, E101. [Google Scholar] [CrossRef]
- Kimani, M.E.; Sarr, M.; Cuffee, Y.; Liu, C.; Webster, N.S. Associations of Race/Ethnicity and Food Insecurity with COVID-19 Infection Rates across US Counties. JAMA Netw. Open 2021, 4, e2112852. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Xu, R.; Volkow, N.D. Increased risk of COVID-19 infection and mortality in people with mental disorders: Analysis from electronic health records in the United States. World Psychiatry 2021, 20, 124–130. [Google Scholar] [CrossRef] [PubMed]
- NCHS. National Health Interview Survey 2022 Survey Description. 2022. Available online: https://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2022/srvydesc-508.pdf (accessed on 13 December 2023).
- NIH. Clinical Spectrum of SARS-CoV-2 Infection. 2023. Available online: https://www.covid19treatmentguidelines.nih.gov/overview/clinical-spectrum/ (accessed on 8 November 2023).
- Fiore, A.E.; Uyeki, T.M.; Broder, K.; Finelli, L.; Euler, G.L.; Singleton, J.A.; Iskander, J.K.; Wortley, P.M.; Shay, D.K.; Bresee, J.S.; et al. Prevention and control of influenza with vaccines: Recommendations of the Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Recomm. Rep. 2010, 59, 1–62. [Google Scholar] [PubMed]
- CDC. Functioning and Disability. 2022. Available online: https://www.cdc.gov/nchs/covid19/pulse/functioning-and-disability.htm (accessed on 25 January 2024).
- Kleinbaum, D.G.; Kupper, L.L.; Muller, K.E.; Nizam, A. Applied Regression Analysis and Other Multivariable Methods; Duxbury Press: Belmont, CA, USA, 1988. [Google Scholar]
- Feikin, D.R.; Higdon, M.M.; Abu-Raddad, L.J.; Andrews, N.; Araos, R.; Goldberg, Y.; Groome, M.J.; Huppert, A.; O’Brien, K.L.; Smith, P.G.; et al. Duration of effectiveness of vaccines against SARS-CoV-2 infection and COVID-19 disease: Results of a systematic review and meta-regression. Lancet 2022, 399, 924–944. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, I.; Nauman, A.; Paul, P.; Ganesan, S.; Chen, K.H.; Jalil, S.M.S.; Jaouni, S.H.; Kawas, H.; Khan, W.A.; Vattoth, A.L.; et al. The efficacy and effectiveness of the COVID-19 vaccines in reducing infection, severity, hospitalization, and mortality: A systematic review. Hum. Vaccin. Immunother. 2022, 18, 2027160. [Google Scholar] [CrossRef] [PubMed]
- Ssentongo, P.; Ssentongo, A.E.; Voleti, N.; Groff, D.; Sun, A.; Ba, D.M.; Nunez, J.; Parent, L.J.; Chinchilli, V.M.; Paules, C.I. SARS-CoV-2 vaccine effectiveness against infection, symptomatic and severe COVID-19: A systematic review and meta-analysis. BMC Infect. Dis. 2022, 22, 439. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Duan, Y.; Qian, J.; Qu, Y.; Wang, Y.; Fan, G.; Huang, Q.; Li, Z.; Yang, W.; Feng, L. A Large-Scale Online Survey on Clinical Severity and Associated Risk Factors for SARS-CoV-2 Omicron Infection-China, April–May 2023. China CDC Wkly. 2024, 6, 305–311. [Google Scholar] [CrossRef] [PubMed]
- Klein, E.Y.; Fall, A.; Norton, J.M.; Eldesouki, R.E.; Abdullah, O.; Han, L.; Yunker, M.; Mostafa, H.H. Severity outcomes associated with SARS-CoV-2 XBB variants, an observational analysis. J. Clin. Virol. 2023, 165, 105500. [Google Scholar] [CrossRef] [PubMed]
- CDC COVID-19 Response Team. Severe outcomes among patients with coronavirus disease 2019 (COVID-19)—United States, February 12–March 16, 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 343–346. [Google Scholar] [CrossRef]
- Christie, A.; Henley, S.J.; Mattocks, L.; Fernando, R.; Lansky, A.; Ahmad, F.B.; Adjemian, J.; Anderson, R.N.; Binder, A.M.; Carey, K.; et al. Decreases in COVID-19 Cases, Emergency Department Visits, Hospital Admissions, and Deaths among Older Adults Following the Introduction of COVID-19 Vaccine-United States, September 6, 2020–May 1, 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 858–864. [Google Scholar] [CrossRef]
- CDC. End of the Federal COVID-19 Public Health Emergency (PHE) Declaration. 2023. Available online: https://www.cdc.gov/coronavirus/2019-ncov/your-health/end-of-phe.html (accessed on 1 February 2024).
- Feikin, D.R.; Abu-Raddad, L.J.; Andrews, N.; Davies, M.A.; Higdon, M.M.; Orenstein, W.A.; Patel, M.K. Assessing vaccine effectiveness against severe COVID-19 disease caused by omicron variant. Report from a meeting of the World Health Organization. Vaccine 2022, 40, 3516–3527. [Google Scholar] [CrossRef] [PubMed]
- Tenforde, M.W.; Self, W.H.; Gaglani, M.; Ginde, A.A.; Douin, D.J.; Talbot, H.K.; Casey, J.D.; Mohr, N.M.; Zepeski, A.; McNeal, T.; et al. Effectiveness of mRNA Vaccination in Preventing COVID-19-Associated Invasive Mechanical Ventilation and Death-United States, March 2021–January 2022. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 459–465. [Google Scholar] [CrossRef]
- Bajema, K.L.; Dahl, R.M.; Prill, M.M.; Meites, E.; Rodriguez-Barradas, M.C.; Marconi, V.C.; Beenhouwer, D.O.; Brown, S.T.; Holodniy, M.; Lucero-Obusan, C.; et al. Effectiveness of COVID-19 mRNA Vaccines against COVID-19-Associated Hospitalization-Five Veterans Affairs Medical Centers, United States, February 1–August 6, 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1294–1299. [Google Scholar] [CrossRef]
- Ferdinands, J.M.; Rao, S.; Dixon, B.E.; Mitchell, P.K.; DeSilva, M.B.; Irving, S.A.; Lewis, N.; Natarajan, K.; Stenehjem, E.; Grannis, S.J.; et al. Waning of vaccine effectiveness against moderate and severe COVID-19 among adults in the US from the VISION network: Test negative, case-control study. BMJ 2022, 379, e072141. [Google Scholar] [CrossRef]
- Chemaitelly, H.; Abu-Raddad, L.J. Waning effectiveness of COVID-19 vaccines. Lancet 2022, 399, 771–773. [Google Scholar] [CrossRef] [PubMed]
- CDC. COVID-19 ACIP Vaccine Recommendations. 2022. Available online: https://www.cdc.gov/vaccines/hcp/acip-recs/vacc-specific/covid-19.html (accessed on 3 January 2024).
- CDC. COVID-19 Vaccine Recommendations for Children and Teens. 2022. Available online: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/vaccines-children-teens.html#:~:text=CDC%20recommends%20everyone%20ages%206,%2D19%20booster%2C%20if%20eligible (accessed on 28 February 2024).
- CDC. COVID-19 Vaccinations in the United States. 2022. Available online: https://covid.cdc.gov/covid-data-tracker/#vaccinations_vacc-total-admin-rate-total (accessed on 13 November 2023).
- CDC. 12 COVID-19 Vaccination Strategies for Your Community. 2022. Available online: https://www.cdc.gov/vaccines/covid-19/vaccinate-with-confidence/community.html (accessed on 25 January 2024).
- Nguyen, C.T.T.; Sandhi, A.; Lee, G.T.; Nguyen, L.T.K.; Kuo, S.Y. Prevalence of and factors associated with postnatal depression and anxiety among parents of preterm infants: A systematic review and meta-analysis. J. Affect. Disord. 2023, 322, 235–248. [Google Scholar] [CrossRef]
- Blanchflower, D.G.; Bryson, A. Long COVID in the United States. PLoS ONE 2023, 18, e0292672. [Google Scholar] [CrossRef]
- Ford, N.D.; Slaughter, D.; Edwards, D.; Dalton, A.; Perrine, C.; Vahratian, A.; Saydah, S. Long COVID and Significant Activity Limitation among Adults, by Age-United States, June 1–13, 2022, to June 7–19, 2023. MMWR Morb. Mortal. Wkly. Rep. 2023, 72, 866–870. [Google Scholar] [CrossRef] [PubMed]
- Ford, N.D.; Agedew, A.; Dalton, A.F.; Singleton, J.; Perrine, C.G.; Saydah, S. Notes from the Field: Long COVID Prevalence Among Adults-United States, 2022. MMWR Morb. Mortal. Wkly. Rep. 2024, 73, 135–136. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).