Turkish Adaptation, Reliability, and Validity Study of the Vaccine Acceptance Instrument
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Sample
2.2. Study Design
2.3. Participation Rate
2.4. Questionnaire
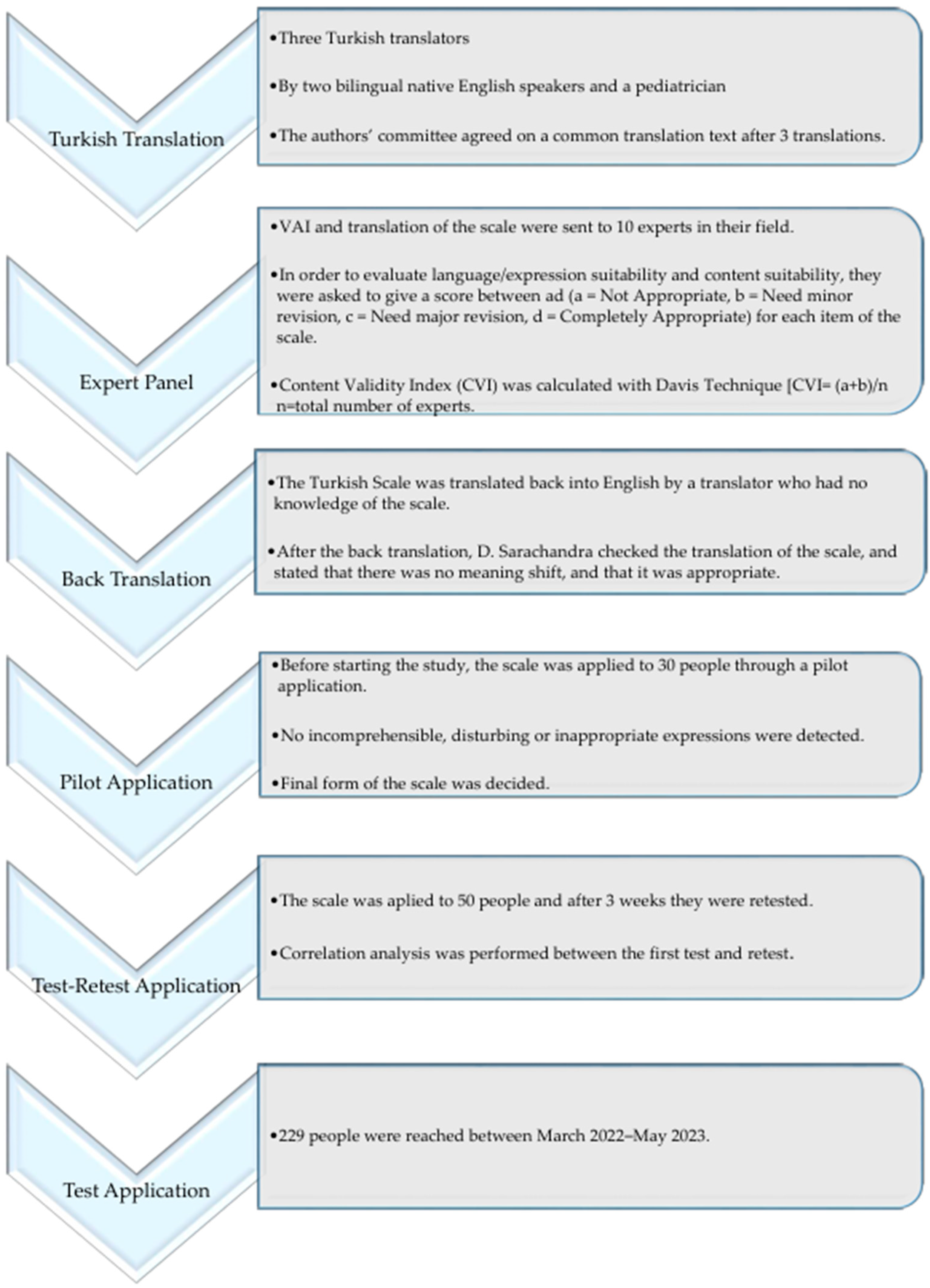
2.5. Process
2.6. Ethical Aspect of the Research
2.7. Data Analyses
3. Results
3.1. Descriptive Characteristics of the Participants
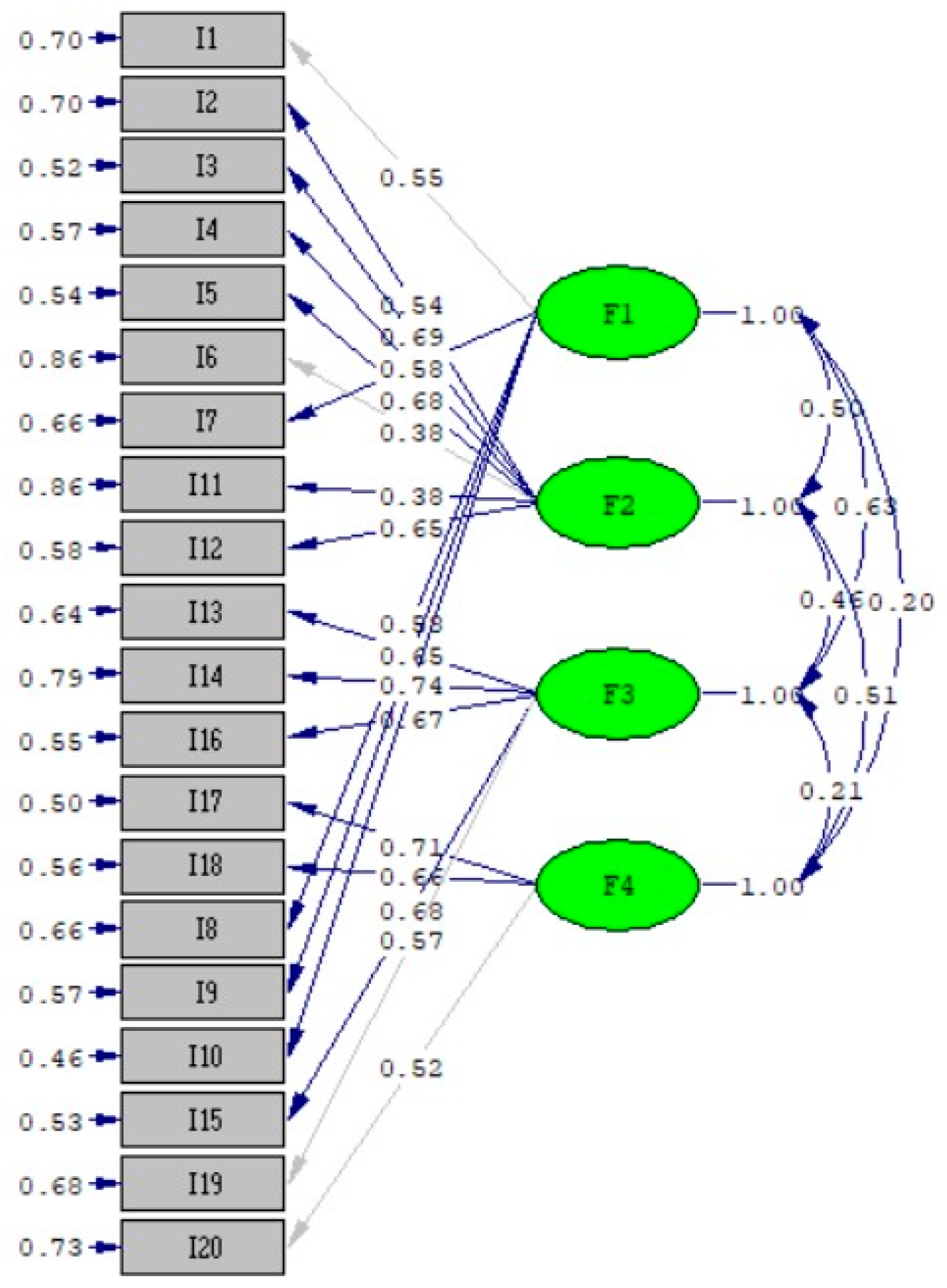
3.2. Validation and Consistency Analyses of the VAI
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dubé, E.; Laberge, C.; Guay, M.; Bramadat, P.; Roy, R.; Bettinger, J.A. Vaccine hesitancy: An overview. Hum. Vaccines Immunother. 2013, 9, 1763–1773. [Google Scholar] [CrossRef]
- Dubé, E.; Vivion, M.; MacDonald, N.E. Vaccine hesitancy, vaccine refusal and the anti-vaccine movement: Influence, impact and implications. Expert Rev. Vaccines 2015, 14, 99–117. [Google Scholar] [CrossRef]
- Yalçin, S.S.; Kömürlüoğlu, A.; Topaç, O. Rates of childhood vaccine refusal in Turkey during 2016–2017: Regional causes and solutions. Arch. Pédiatrie 2022, 29, 594–598. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The Global Vaccine Action Plan 2011–2020: Review and Lessons Learned: Strategic Advisory Group of Experts on Immunization; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- The Strategic Advisory Group of Experts (SAGE). Report of the SAGE Working Group on Vaccine Hesitancy; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Yalçin, S.S.; Bakacak, A.G.; Topaç, O. Unvaccinated children as community parasites in National Qualitative Study from Turkey. BMC Public Health 2020, 20, 1087. [Google Scholar] [CrossRef]
- Larson, H.J.; Jarrett, C.; Eckersberger, E.; Smith, D.M.; Paterson, P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: A systematic review of published literature, 2007–2012. Vaccine 2014, 32, 2150–2159. [Google Scholar] [CrossRef] [PubMed]
- Murphy, J.; Vallières, F.; Bentall, R.P.; Shevlin, M.; McBride, O.; Hartman, T.K.; McKay, R.; Bennett, K.; Mason, L.; Gibson-Miller, J. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat. Commun. 2021, 12, 29. [Google Scholar] [CrossRef]
- Opel, D.J.; Mangione-Smith, R.; Taylor, J.A.; Korfiatis, C.; Wiese, C.; Catz, S.; Martin, D.P. Development of a survey to identify vaccine-hesitant parents: The parent attitudes about childhood vaccines survey. Hum. Vaccines 2011, 7, 419–425. [Google Scholar] [CrossRef]
- Oduwole, E.O.; Pienaar, E.D.; Mahomed, H.; Wiysonge, C.S. Overview of tools and measures investigating vaccine hesitancy in a ten year period: A scoping review. Vaccines 2022, 10, 1198. [Google Scholar] [CrossRef]
- Opel, D.J.; Taylor, J.A.; Mangione-Smith, R.; Solomon, C.; Zhao, C.; Catz, S.; Martin, D. Validity and reliability of a survey to identify vaccine-hesitant parents. Vaccine 2011, 29, 6598–6605. [Google Scholar] [CrossRef]
- Gilkey, M.B.; Magnus, B.E.; Reiter, P.L.; McRee, A.-L.; Dempsey, A.F.; Brewer, N.T. The Vaccination Confidence Scale: A brief measure of parents’ vaccination beliefs. Vaccine 2014, 32, 6259–6265. [Google Scholar] [CrossRef] [PubMed]
- Larson, H.J.; Jarrett, C.; Schulz, W.S.; Chaudhuri, M.; Zhou, Y.; Dube, E.; Schuster, M.; MacDonald, N.E.; Wilson, R. Measuring vaccine hesitancy: The development of a survey tool. Vaccine 2015, 33, 4165–4175. [Google Scholar] [CrossRef] [PubMed]
- Wallace, A.S.; Wannemuehler, K.; Bonsu, G.; Wardle, M.; Nyaku, M.; Amponsah-Achiano, K.; Dadzie, J.F.; Sarpong, F.O.; Orenstein, W.A.; Rosenberg, E.S. Development of a valid and reliable scale to assess parents’ beliefs and attitudes about childhood vaccines and their association with vaccination uptake and delay in Ghana. Vaccine 2019, 37, 848–856. [Google Scholar] [CrossRef] [PubMed]
- Sarathchandra, D.; Navin, M.C.; Largent, M.A.; McCright, A.M. A survey instrument for measuring vaccine acceptance. Prev. Med. 2018, 109, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Social Foundations of Thought and Action: A Social Cognitive Theory; Prentice-Hall, Inc.: Hoboken, NJ, USA, 1986. [Google Scholar]
- AlSaeed, A.A.; Rabbani, U. Explaining COVID-19 vaccine rejection using social cognitive theory in Qassim, Saudi Arabia. Vaccines 2021, 9, 1304. [Google Scholar] [CrossRef] [PubMed]
- Kowalsky, J.M.; Buelow, M.T.; Brunell, A.B. One-size fits all? Evaluating group differences in an integrated social cognition model to understand COVID-19 vaccine intention and uptake. Soc. Sci. Med. 2024, 348, 116780. [Google Scholar] [CrossRef] [PubMed]
- Rosenstock, I.M.; Strecher, V.J.; Becker, M.H. Social learning theory and the health belief model. Health Educ. Q. 1988, 15, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Cheney, M.K.; John, R. Underutilization of influenza vaccine: A test of the health belief model. Sage Open 2013, 3, 2158244013484732. [Google Scholar] [CrossRef]
- Berger, C.; Ben-Shalom, U.; Tarant, Z.; Longo, J.; DeDonno, M. The Influence of the Health Belief Model on the Decision to Get the COVID-19 Vaccine: An International Survey Study of College Students. INQUIRY J. Health Care Organ. Provis. Financ. 2023, 60, 00469580231164229. [Google Scholar] [CrossRef]
- Akgül, A.; Çevik, O. İstatistiksel Analiz Teknikleri; Emek Ofset Ltd. Şti.: Ankara, Turkey, 2003. [Google Scholar]
- World Health Organization. Process of Translation and Adaptation of Instruments; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Davis, L.L. Instrument review: Getting the most from a panel of experts. Appl. Nurs. Res. 1992, 5, 194–197. [Google Scholar] [CrossRef]
- Tavşancıl, E. Tutumların Ölçülmesi ve SPSS ile Veri Analizi, 2nd ed.; Nobel Yayınevi: Ankara, Turkey, 2014; p. 54. [Google Scholar]
- Tavakol, M.; Dennick, R. Making sense of Cronbach’s alpha. Int. J. Med. Educ. 2011, 2, 53. [Google Scholar] [CrossRef] [PubMed]
- Eisinga, R.; te Grotenhuis, M.; Pelzer, B. The reliability of a two-item scale: Pearson, Cronbach, or Spearman-Brown? Int. J. Public Health 2013, 58, 637–642. [Google Scholar] [CrossRef] [PubMed]
- Karagöz, Y.; Kösterelioğlu, İ. İletişim becerileri değerlendirme ölçeğinin faktör analizi metodu ile geliştirilmesi. Dumlupınar Üniversitesi Sos. Bilim. Derg. 2008, 21, 81–97. [Google Scholar]
- de Vaus, D. Surveys in Social Research; Allen and Unwin Pty Ltd.: Crows Nest, Australia, 1991. [Google Scholar]
- Brown, T.A. Confirmatory Factor Analysis for Applied Research; Guilford Publications: New York, NY, USA, 2015. [Google Scholar]
- Çokluk, Ö.; Şekercioğlu, G.; Büyüköztürk, Ş. Sosyal Bilimler Için çok Değişkenli Istatistik: SPSS ve LISREL Uygulamaları; Pegem Akademi: Ankara, Turkey, 2012. [Google Scholar]
- Ozdamar, K. Paket Programlar ile Istatistiksel veri Analizi; Nisan Publication: Eskişehir, Türkiye, 2017. [Google Scholar]
- Liu, Y. Developing a scale to measure the interactivity of websites. J. Advert. Res. 2003, 43, 207–216. [Google Scholar] [CrossRef]
- Bertoncello, C.; Ferro, A.; Fonzo, M.; Zanovello, S.; Napoletano, G.; Russo, F.; Baldo, V.; Cocchio, S. Socioeconomic determinants in vaccine hesitancy and vaccine refusal in Italy. Vaccines 2020, 8, 276. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, N.L.; Gilmour, H.; Wilson, S.E.; Cantin, L. Determinants of non-vaccination and incomplete vaccination in Canadian toddlers. Hum. Vaccines Immunother. 2017, 13, 1447–1453. [Google Scholar] [CrossRef]
- Konstantinou, N.; Nicolaou, S.A.; Petrou, C.; Pieri, M. Trust in authorities and demographic factors affect vaccine acceptance during the COVID-19 pandemic in Cyprus. Eur. J. Psychol. Open 2021, 80, 88–97. [Google Scholar] [CrossRef]
- Anello, P.; Cestari, L.; Baldovin, T.; Simonato, L.; Frasca, G.; Caranci, N.; Pascucci, M.G.; Valent, F.; Canova, C. Socioeconomic factors influencing childhood vaccination in two northern Italian regions. Vaccine 2017, 35, 4673–4680. [Google Scholar] [CrossRef]
- Hak, E.; Schönbeck, Y.; De Melker, H.; Van Essen, G.A.; Sanders, E.A. Negative attitude of highly educated parents and health care workers towards future vaccinations in the Dutch childhood vaccination program. Vaccine 2005, 23, 3103–3107. [Google Scholar] [CrossRef]
- Capasso, M.; Bianchi, M.; Caso, D. Psychosocial Factors Influencing Parents’ Acceptance of COVID-19 Vaccination for Their Children: An Italian Cross-Sectional Study. Vaccines 2024, 12, 317. [Google Scholar] [CrossRef]
- Morgan, J.; Wagoner, J.A.; Pyszczynski, T. Psychosocial Determinants of COVID-19 Vaccine Hesitancy and the Mediating Role of Various Attitudes Towards Science. Vaccines 2023, 11, 1310. [Google Scholar] [CrossRef] [PubMed]
- Soysal, G.; Durukan, E.; Akdur, R. The Evaluation of Vaccine Hesitancy and Refusal for Childhood Vaccines and the COVID-19 Vaccine in Individuals Aged Between 18 and 25 Years. Turk. J. Immunol. 2021, 9, 120–127. [Google Scholar] [CrossRef]
- Führer, A.; Pacolli, L.; Yilmaz-Aslan, Y.; Brzoska, P. COVID-19 vaccine acceptance and its determinants among migrants in Germany—Results of a cross-sectional study. Vaccines 2022, 10, 1350. [Google Scholar] [CrossRef]
- Maqsood, M.B.; Islam, M.A.; Al Qarni, A.; Nisa, Z.-U.; Ishaqui, A.A.; Alharbi, N.K.; Almukhamel, M.; Hossain, M.A.; Fatani, N.; Mahrous, A.J. Assessment of COVID-19 vaccine acceptance and reluctance among staff working in public healthcare settings of Saudi Arabia: A multicenter study. Front. Public Health 2022, 10, 847282. [Google Scholar] [CrossRef]
- Caban-Martinez, A.J.; Silvera, C.A.; Santiago, K.M.; Louzado-Feliciano, P.; Burgess, J.L.; Smith, D.L.; Jahnke, S.; Horn, G.P.; Graber, J.M. COVID-19 vaccine acceptability among US firefighters and emergency medical services workers: A cross-sectional study. J. Occup. Environ. Med. 2021, 63, 369–373. [Google Scholar] [CrossRef] [PubMed]
- Omar, A.; Gul, I.; Ali, I. Exploring vaccine hesitancy and acceptance in the general population of Pakistan: Insights into COVID-19-related distress, risk perception, and stigma. Hum. Vaccines Immunother. 2024, 20, 2309699. [Google Scholar] [CrossRef] [PubMed]
- Pivetti, M.; Melotti, G.; Bonomo, M.; Hakoköngäs, E. Conspiracy beliefs and acceptance of COVID-vaccine: An exploratory study in Italy. Soc. Sci. 2021, 10, 108. [Google Scholar] [CrossRef]
- Drummond, C.; Fischhoff, B. Development and validation of the scientific reasoning scale. J. Behav. Decis. Mak. 2017, 30, 26–38. [Google Scholar] [CrossRef]
- Lewandowsky, S.; Gignac, G.E.; Oberauer, K. The role of conspiracist ideation and worldviews in predicting rejection of science. PLoS ONE 2013, 8, e75637. [Google Scholar] [CrossRef]
| n (%) | VAI Score (Mean ± SD) | p Value | F1 Subscale Score (Mean ± SD) | F2 Subscale Score (Mean ± SD) | F3 Subscale Score (Mean ± SD) | F4 Subscale Score (Mean ± SD) | |
|---|---|---|---|---|---|---|---|
| Parent | 0.73 | ||||||
| Mother | 199 (86.9%) | 112.89 ± 16.19 | 30.32 ± 5.21 | 35.6 ± 8.54 | 32.13 ± 4.38 | 14.83 ± 5.25 | |
| Father | 30 (13.1%) | 111.46 ± 22.05 | 29.86 ± 6.06 | 35.66 ± 10.36 | 31.66 ± 5.79 | 14.26 ± 5.21 | |
| Child age (year) | (6.96 ± 4.38) | 0.72 | |||||
| ≤5 years | 104 (45.4%) | 113.14 ± 17.63 | 30.33 ± 4.67 | 35.83 ± 9.34 | 32.03 ± 4.36 | 14.93 ± 5.40 | |
| 6 years and older | 125 (54.6%) | 112.35 ± 16.55 | 30.2 ± 5.82 | 35.42 ± 8.31 | 32.1 ± 4.76 | 14.61 ± 5.11 | |
| Child gender | 0.63 | ||||||
| Male | 103 (45%) | 112.12 ± 17.77 | 30.07 ± 5.13 | 35.31 ± 9 | 31.55 ± 5.05 | 15.18 ± 5.02 | |
| Female | 126 (55%) | 113.19 ± 16.44 | 30.42 ± 5.49 | 35.85 ± 8.61 | 32.5 ± 4.11 | 14.41 ± 5.40 | |
| Mother’s age (years) | (36.12 ± 6.65) | 0.24 | |||||
| <35 | 100 (43.7%) | 111.21 ± 16.8 | 30.13 ± 4.89 | 35.06 ± 8.75 | 31.75 ± 4.12 | 14.27 ± 5.69 | |
| ≥35 | 129 (56.3%) | 113.87 ± 17.18 | 30.37 ± 5.65 | 36.03 ± 8.80 | 32.32 ± 4.9 | 15.13 ± 4.85 | |
| Father’s age (years) | (39.62 ± 6.78) | 0.66 | |||||
| <35 | 57 (24.9%) | 111.8 ± 17.84 | 30.14 ± 5.43 | 35.31 ± 9.18 | 31.75 ± 4.18 | 14.49 ± 5.59 | |
| ≥35 | 172 (75.1%) | 113.01 ± 16.78 | 30.3 ± 5.30 | 35.7 ± 8.66 | 32.18 ± 4.70 | 14.81 ± 5.13 | |
| Family type | 0.78 | ||||||
| Nuclear | 220 (96.1%) | 112.7 ± 17.27 | 30.21 ± 5.38 | 35.63 ± 8.89 | 32.01 ± 4.64 | 14.83 ± 5.21 | |
| Extended/broken family | 9 (3.9%) | 112.88 ± 9.94 | 31.44 ± 3.74 | 35.11 ± 5.55 | 33.44 ± 2.18 | 12.88 ± 5.79 | |
| Parent education (Mother) | |||||||
| <High school | 59 (25.8%) | 108.86 ± 15.16 | 0.043 | 28.93 ± 6.61 | 35.11 ± 8.25 | 30.86 ± 5.32 * | 13.94 ± 5.32 |
| ≥High school and higher | 170 (74.2%) | 114.04 ± 17.46 | 30.72 ± 4.72 | 35.78 ± 8.97 | 32.49 ± 4.22 * | 15.04 ± 5.20 | |
| Parent education (Father) | 0.14 | ||||||
| <High school | 45 (19.7%) | 109.35 ± 16.40 | 29.73 ± 6.26 | 35.11 ± 8.22 | 31.08 ± 5.36 | 13.42 ± 5.70 | |
| ≥High school and higher | 184 (80.3%) | 113.53 ± 17.11 | 30.39 ± 5.08 | 35.73 ± 8.92 | 32.31 ± 4.35 | 15.08 ± 5.08 | |
| Household income | 0.003 | ||||||
| Low income | 60 (26.2%) | 111.63 ± 15.55 | 30.11 ± 6.09 | 36.05 ± 8.24 | 31.06 ± 5.58 | 14.4 ± 5.38 | |
| Moderate income | 73 (31.9%) | 108.08 ± 16.35 | 29.83 ± 5.56 | 33.05 ± 8.74 | 31.82 ± 4.04 | 13.36 ± 5.26 | |
| High income | 96 (41.9%) | 116.90 ± 17.54 | 30.68 ± 4.6 | 37.28 ± 8.76 | 32.89 ± 4.15 | 16.04 ± 4.87 | |
| Living in | |||||||
| Center | 190 (83%) | 112.85 ± 17.22 | 0.77 | 30.53 ± 5.08 | 35.42 ± 8.82 | 31.97 ± 4.73 | 14.92 ± 5.1 |
| Others | 39 (17%) | 112.02 ± 16.2 | 28.97 ± 6.25 | 36.53 ± 8.61 | 32.56 ± 3.74 | 13.94 ± 5.87 | |
| Mother’s employment | 0.005 | ||||||
| Housewife | 124 (54.1%) | 109.83 ± 15.54 | 29.98 ± 5.86 | 34.63 ± 8.02 | 31.48 ± 4.68 * | 13.73 ± 5.25 * | |
| Employed | 105 (45.9%) | 116.1 ± 18.1 | 30.6 ± 4.6 | 36.76 ± 9.5 | 32.77 ± 4.37 * | 15.97 ± 4.98 * | |
| Father’s employment | 0.001 | ||||||
| Unemployed | 2 (0.9%) | 132.5 ± 10.6 | 30.5 ± 6.36 | 47 ± 2.82 | 34.5 ± 0.7 | 20.5 ± 0.7 | |
| Education sector | 22 (9.6%) | 115.13 ± 16.14 | 31.72 ± 3.41 | 35.68 ± 9.38 | 33.27 ± 3.10 | 14.45 ± 4.65 | |
| Health sector | 29 (12.7%) | 123.13 ± 14.89 | 31.24 ± 3.44 | 40.89 ± 7.83 | 33.31 ± 3.43 | 17.68 ± 4.24 | |
| Others | 176 (76.9%) | 110.46 ± 16.79 | 29.92 ± 5.73 | 34.60 ± 8.53 | 31.69 ± 4.86 | 14.25 ± 5.31 | |
| Number of children in the household | 0.47 | ||||||
| 1 | 51 (22.3%) | 111.13 ± 18.39 | 30.8 ± 3.81 | 34.17 ± 10.11 | 32.19 ± 4.53 | 13.96 ± 5.47 | |
| 2–3 | 149 (65.1%) | 113.71 ± 16.48 | 30.07 ± 5.69 | 36.07 ± 8.14 | 32.22 ± 4.31 | 15.33 ± 5.06 | |
| ≥4 | 29 (12.7%) | 110.34 ± 17.41 | 30.31 ± 5.7 | 35.75 ± 9.44 | 31.06 ± 5.85 | 13.20 ± 5.42 | |
| İmmunization status of the child | 0.11 | ||||||
| Fully vaccinated | 222 (96.9%) | 113.02 ± 16.73 | 30.26 ± 5.35 | 35.74 ± 8.68 | 32.14 ± 4.49 | 14.86 ± 5.26 * | |
| incompletely vaccinated/unvaccinated | 7 (3.1%) | 102.71 ± 24.12 | 30.28 ± 4.82 | 31.42 ± 11.45 | 29.71 ± 6.84 | 11.28 ± 2.69 * | |
| Mother’s COVID-19 vaccination status | 0.03 | ||||||
| At least 2 doses given | 216 (94.3%) | 113.65 ± 16.04 | 30.5 ± 5.05 | 35.93 ± 8.56 * | 32.36 ± 4.03 | 14.85 ± 5.26 | |
| Unvaccinated | 13 (5.7%) | 97 ± 24.73 | 26.38 ± 7.93 | 30.15 ± 10.8 * | 27.3 ± 9.03 | 13.15 ± 4.82 | |
| Father’s COVID-19 vaccination status | 0.09 | ||||||
| At least 2 doses given | 215 (93.9%) | 113.49 ± 15.97 | 30.45 ± 5.06 | 35.87 ± 8.53 | 32.34 ± 4.03 | 14.82 ± 5.25 | |
| Unvaccinated | 14 (6.1%) | 100.64 ± 26.75 | 27.42 ± 8.12 | 31.57 ± 11.56 | 27.85 ± 8.91 | 13.78 ± 5.1 | |
| Mother’s vaccination in the last 5 years, | 0.66 | ||||||
| Yes | 110 (48%) | 113.20 ± 16.26 | 30.09 ± 5.10 | 35.99 ± 8.85 | 32.3 ± 3.91 | 14.8 ± 5.43 | |
| No | 119 (52%) | 112.26 ± 17.75 | 30.42 ± 5.53 | 35.26 ± 8.72 | 31.85 ± 5.12 | 14.71 ± 5.07 | |
| Father’s vaccination in the last 5 years, | 0.40 | ||||||
| Yes | 72 (31.4%) | 114.09 ± 15.79 | 30.47 ± 4.85 | 36.29 ± 8.33 | 32.47 ± 4.08 | 14.86 ± 5.38 | |
| No | 157 (68.6%) | 112.07 ± 17.56 | 30.17 ± 5.53 | 35.29 ± 8.98 | 31.89 ± 4.79 | 14.71 ± 5.19 | |
| Total | 229 (100%) | 112.71 ± 17.02 | 30.26 ± 5.32 | 35.61 ± 8.77 | 32.07 ± 4.58 | 14.75 ± 5.24 |
| Expert Opinion (n = 15) | |||||
|---|---|---|---|---|---|
| Appropriate | Need Minor Revision | Need Major Revision | Not Appropriate | CVI | |
| Item1 | 15 | 0 | 0 | 0 | 1.00 |
| Item2 | 14 | 1 | 0 | 0 | 1.00 |
| Item3 | 15 | 0 | 0 | 0 | 1.00 |
| Item4 | 15 | 0 | 0 | 0 | 1.00 |
| Item5 | 11 | 3 | 1 | 0 | 0.93 |
| Item6 | 13 | 2 | 0 | 0 | 1.00 |
| Item7 | 15 | 0 | 0 | 0 | 1.00 |
| Item8 | 12 | 3 | 0 | 0 | 1.00 |
| Item9 | 13 | 2 | 0 | 0 | 1.00 |
| Item10 | 9 | 5 | 1 | 0 | 0.93 |
| Item11 | 10 | 5 | 0 | 0 | 1.00 |
| Item12 | 14 | 1 | 0 | 0 | 1.00 |
| Item13 | 10 | 3 | 2 | 0 | 0.86 |
| Item14 | 9 | 4 | 2 | 0 | 0.86 |
| Item15 | 15 | 0 | 0 | 0 | 1.00 |
| Item16 | 8 | 5 | 2 | 0 | 0.86 |
| Item17 | 12 | 2 | 1 | 0 | 0.93 |
| Item18 | 12 | 2 | 1 | 0 | 0.93 |
| Item19 | 12 | 2 | 1 | 0 | 0.93 |
| Item20 | 11 | 3 | 1 | 0 | 0.93 |
| Items | Factor 1 | Factor 2 | Factor 3 | Factor 4 |
|---|---|---|---|---|
| I10 | 0.766 | |||
| I8 | 0.685 | |||
| I7 | 0.661 | |||
| I9 | 0.657 | |||
| I1 | 0.506 | |||
| I3 (R) | 0.765 | |||
| I2 (R) | 0.662 | |||
| I6 (R) | 0.639 | |||
| I5 (R) | 0.613 | |||
| I4 (R) | 0.587 | |||
| I12 (R) | 0.499 | |||
| I11 (R) | 0.325 | |||
| I16 (R) | 0.735 | |||
| I13 (R) | 0.720 | |||
| I14 (R) | 0.598 | |||
| I15 | 0.587 | |||
| I19 | 0.464 | |||
| I17 (R) | 0.816 | |||
| I18 (R) | 0.712 | |||
| I20 | 0.711 | |||
| Eigenvalues | 5.144 | 2.344 | 1.509 | 1.413 |
| % of variance | 25.57 | 11.72 | 7.54 | 7.06 |
| Total variance explained, % | 51.9 | |||
| Kaiser-Meyer-Olkin Measure of Sampling Adequacy | 0.787 | |||
| Bartlett’s Test of Sphericity | 1358.6 | |||
| df | 190 | |||
| p value | <0.01 | |||
| Fit Indices | The Scale Value | Reference Values for Acceptable Fit | Reference Values for Good Fit |
|---|---|---|---|
| X2/df | 380.04/164 = 2.317 | 2 < X2/df ≤ 3 | 0 ≤ X2/df ≤ 2 |
| RMSEA | 0.076 | 0.05 < RMSEA ≤ 0.08 | 0 < RMSEA ≤ 0.05 |
| GFI | 0.90 | 0.90 ≤ GFI < 0.95 | 0.95 ≤ GFI < 1.0 |
| AGFI | 0.906 | 0.90 ≤ AGFI < 0.95 | 0.95 ≤ AGFI < 1.0 |
| CFI | 0.910 | 0.90 ≤ CFI < 0.95 | 0.95 ≤ CFI < 1.0 |
| NFI | 0.90 | 0.90 ≤ NFI < 0.95 | 0.95 ≤ NFI < 1.0 |
| Item Number | Mean | Standard Deviation | Item-Total Correlation | Cronbach’s Alpha If Item Deleted | Cronbach’s Alpha of the Subscale | ICC * of Test–Retest Analyses (95%CI **) | |
|---|---|---|---|---|---|---|---|
| Factor 1 | 1 | 6.2 | 1.43 | 0.398 | 0.817 | 0.754 | |
| 7 | 6.25 | 1.38 | 0.384 | 0.817 | |||
| 8 | 5.86 | 1.62 | 0.38 | 0.817 | 0.977 (0.96–0.987) | ||
| 9 | 5.76 | 1.60 | 0.432 | 0.815 | |||
| 10 | 6.17 | 1.43 | 0.408 | 0.816 | |||
| Factor 2 | 2 | 4.69 | 1.79 | 0.389 | 0.817 | 0.753 | |
| 3 | 5.14 | 1.88 | 0.505 | 0.811 | |||
| 4 | 6.06 | 1.45 | 0.566 | 0.810 | |||
| 5 | 5.58 | 1.87 | 0.567 | 0.807 | 0.986 (0.976–0.992) | ||
| 6 | 4.48 | 2.24 | 0.241 | 0.827 | |||
| 11 | 4.29 | 2.45 | 0.321 | 0.823 | |||
| 12 | 5.34 | 1.95 | 0.614 | 0.804 | |||
| Factor 3 | 13 | 6.49 | 1.35 | 0.419 | 0.816 | 0.714 | |
| 14 | 6.04 | 1.63 | 0.447 | 0.814 | |||
| 15 | 6.42 | 1.28 | 0.371 | 0.818 | 0.972 (0.951–0.984) | ||
| 16 | 6.69 | 1.08 | 0.386 | 0.818 | |||
| 19 | 6.41 | 1.28 | 0.308 | 0.820 | |||
| Factor 4 | 17 | 5.06 | 2.28 | 0.385 | 0.818 | 0.662 | |
| 18 | 4.36 | 2.45 | 0.331 | 0.822 | 0.945 (0.903–0.969) | ||
| 20 | 5.32 | 2.02 | 0.331 | 0.820 | |||
| Total | 0.992 (0.987–0.996) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kömürlüoğlu, A.; Akaydın Gültürk, E.; Yalçın, S.S. Turkish Adaptation, Reliability, and Validity Study of the Vaccine Acceptance Instrument. Vaccines 2024, 12, 480. https://doi.org/10.3390/vaccines12050480
Kömürlüoğlu A, Akaydın Gültürk E, Yalçın SS. Turkish Adaptation, Reliability, and Validity Study of the Vaccine Acceptance Instrument. Vaccines. 2024; 12(5):480. https://doi.org/10.3390/vaccines12050480
Chicago/Turabian StyleKömürlüoğlu, Ayça, Esra Akaydın Gültürk, and Sıddika Songül Yalçın. 2024. "Turkish Adaptation, Reliability, and Validity Study of the Vaccine Acceptance Instrument" Vaccines 12, no. 5: 480. https://doi.org/10.3390/vaccines12050480
APA StyleKömürlüoğlu, A., Akaydın Gültürk, E., & Yalçın, S. S. (2024). Turkish Adaptation, Reliability, and Validity Study of the Vaccine Acceptance Instrument. Vaccines, 12(5), 480. https://doi.org/10.3390/vaccines12050480





