The Impact of the Coronavirus Pandemic on Vaccination Coverage in Latin America and the Caribbean
Abstract
1. Introduction
2. Methodology
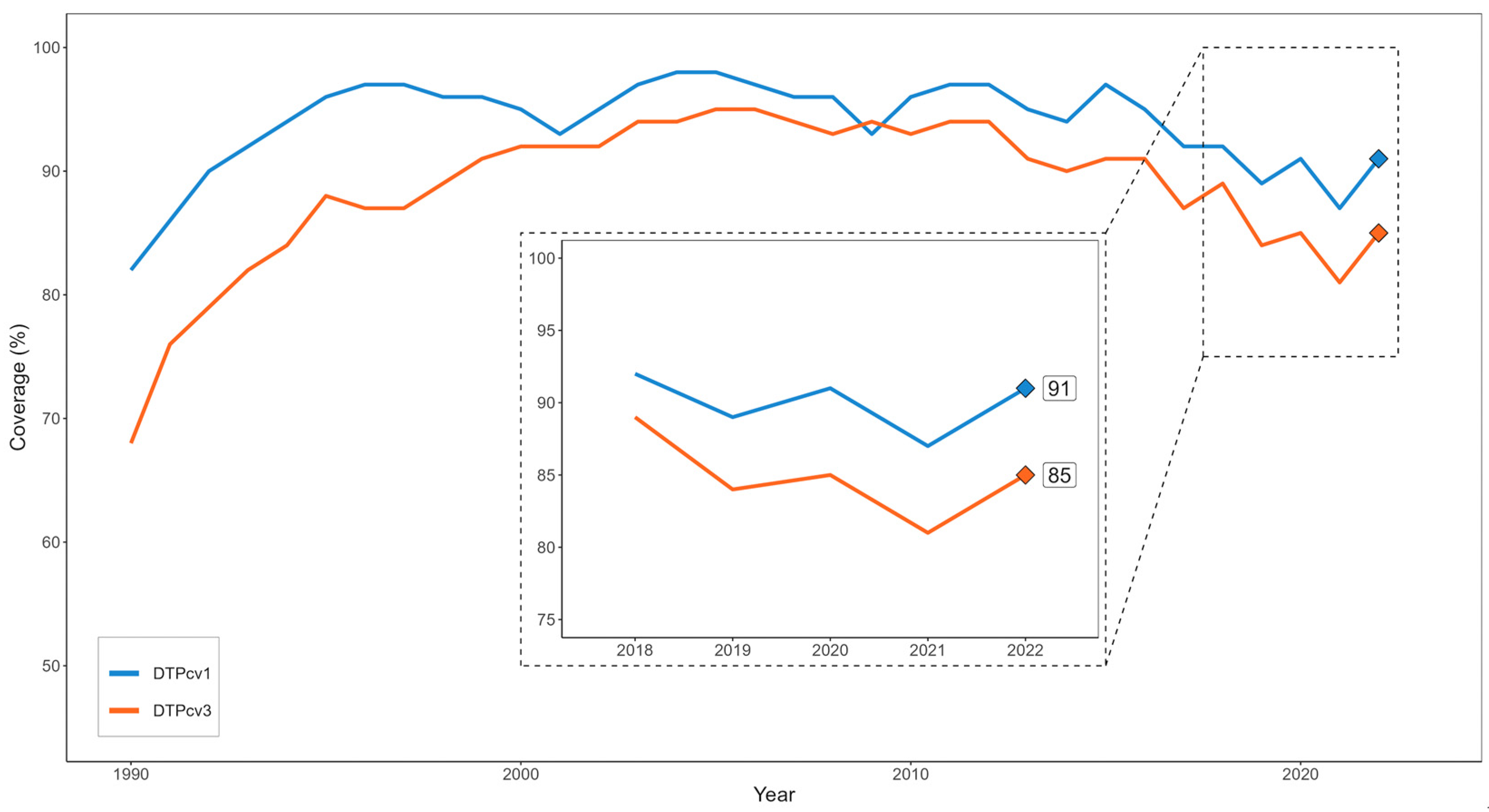
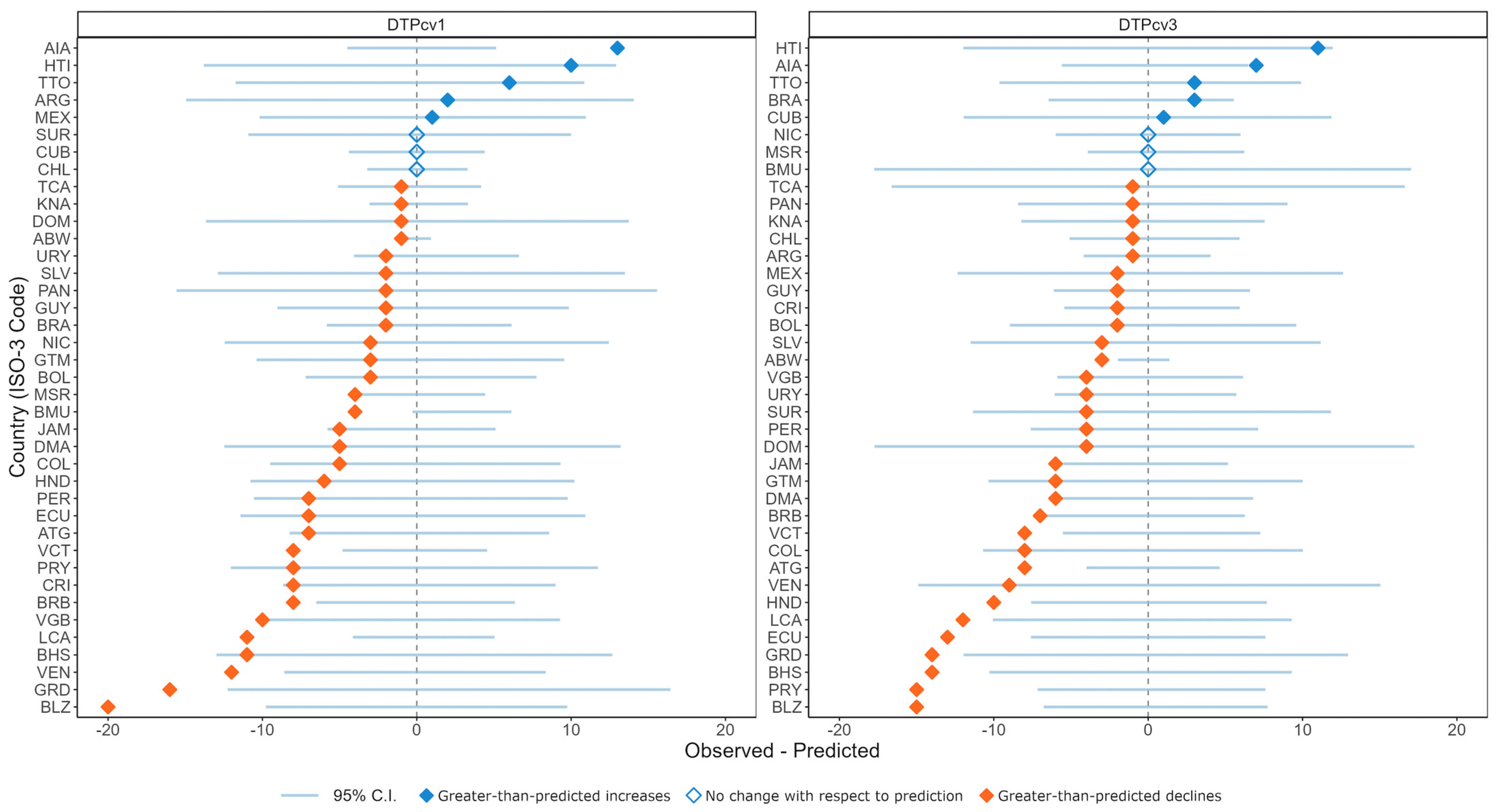
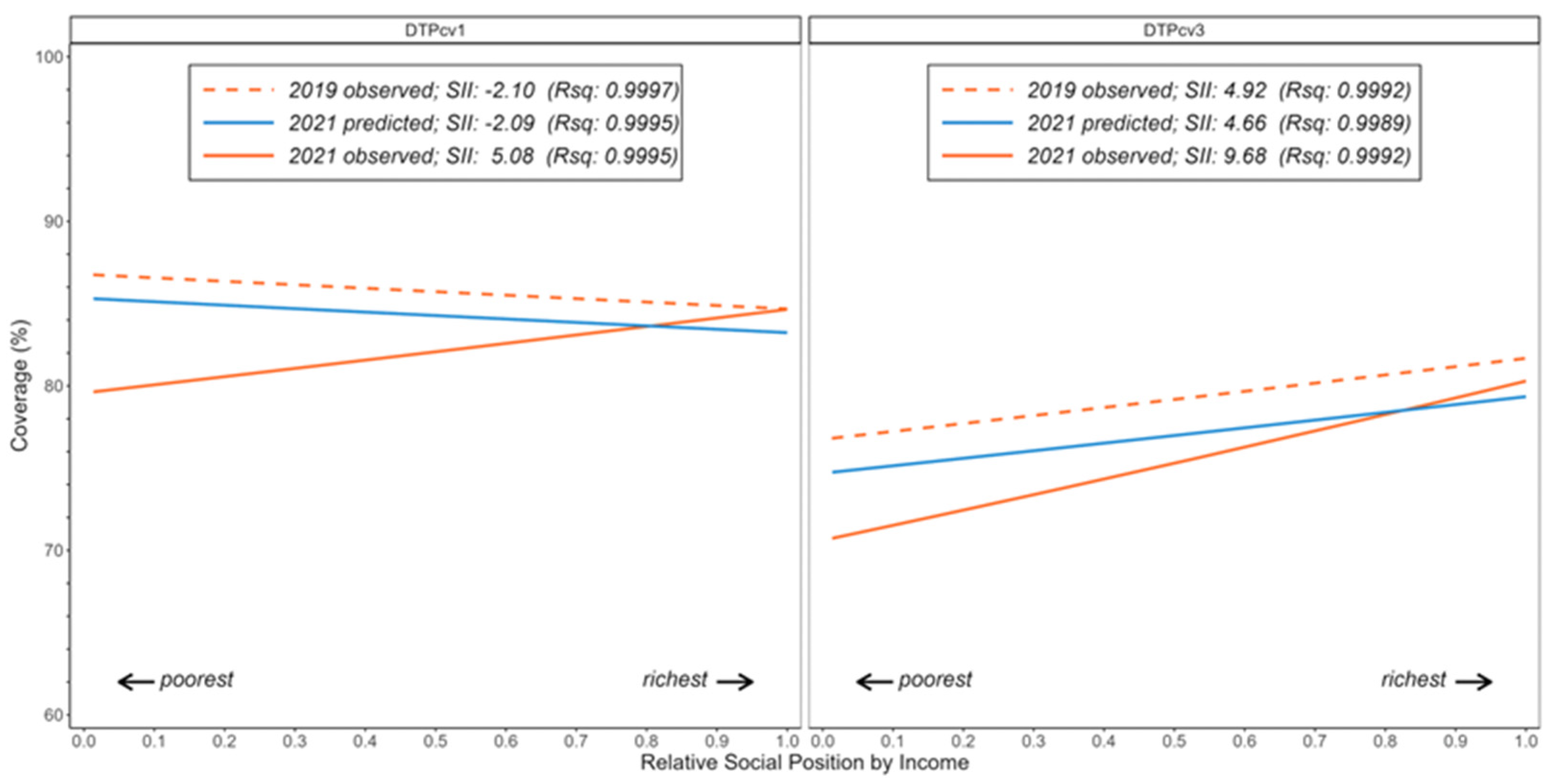
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pan American Health Organization. Reinvigorating Immunization as a Public Good for Universal Health. 2021. Available online: https://www.paho.org/en/documents/ce16814-reinvigorating-immunization-public-good-universal-health (accessed on 7 January 2024).
- Chan, I.L.; Mowson, R.; Alonso, J.P.; Roberti, J.; Contreras, M.; Velandia-González, M. Promoting immunization equity in Latin America and the Caribbean: Case studies, lessons learned, and their implication for COVID-19 vaccine equity. Vaccine 2022, 40, 1977–1986. [Google Scholar] [CrossRef] [PubMed]
- Pan American Health Organization. Immunization Dashboard. 2024. Available online: https://immunizationdata.who.int (accessed on 7 January 2024).
- Plans-Rubió, P. Vaccination coverage for routine vaccines and herd immunity levels against measles and pertussis in the world in 2019. Vaccines 2021, 9, 256. [Google Scholar] [CrossRef] [PubMed]
- Matta-Chuquisapon, J.; Gianella, C.; Carrasco-Escobar, G. Missed opportunities for vaccination in Peru 2010–2020, A study of socioeconomic inequalities. Lancet Reg. Health—Am. 2022, 14, 100321. [Google Scholar] [CrossRef] [PubMed]
- Guzman-Holst, A.; DeAntonio, R.; Prado-Cohrs, D.; Juliao, P. Barriers to vaccination in Latin America: A systematic literature review. Vaccine 2020, 38, 470–481. [Google Scholar] [CrossRef] [PubMed]
- Cardoso Pinto, A.M.; Ranasinghe, L.; Dodd, P.J.; Budhathoki, S.S.; Seddon, J.A.; Whittaker, E. Disruptions to routine childhood vaccinations in low- and middle-income countries during the COVID-19 pandemic: A systematic review. Front. Pediatr. 2022, 10, 979769. [Google Scholar] [CrossRef] [PubMed]
- Matos, C.C.S.A.; Barbieri, C.L.A.; Couto, M.T. COVID-19 and its impact on immunization programs: Reflections from Brazil. Rev. Saude Publica 2020, 54, 114. [Google Scholar] [CrossRef] [PubMed]
- Sato, A.P.S. Pandemic and vaccine coverage: Challenges of returning to schools. Rev. Saude Publica 2020, 54, 115. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Routine Immunization Services during the Coronavirus (COVID-19) Pandemic. 2020. Available online: https://apps.who.int/iris/bitstream/handle/10665/331925/Routine-immunization-services-COVID-19-eng.pdf?sequence=1&isAllowed=y (accessed on 26 December 2023).
- La Organización Panamericana de la Salud. Cuarta Ronda de la Encuesta Nacional Sobre la Continuidad de los Servicios Esenciales de Salud Durante la Pandemia de COVID-19. Resumen de Resultados y Conclusiones para la Regiόn de las Américas. Noviembre 2022–Enero 2023. 2023. Available online: https://iris.paho.org/bitstream/handle/10665.2/57793/OPSHSSPH230003_spa.pdf?sequence=7&isAllowed=y (accessed on 26 December 2023).
- Edelman. Edelman Trust Barometer 2022. Special Report: Trust and Health. 2022. Available online: https://www.edelman.com/sites/g/files/aatuss191/files/2022-08/2022%20Trust%20Barometer%20Special%20Report%20Trust%20and%20Health%20with%20Talk%20Track.pdf (accessed on 14 March 2024).
- Halpern, B.; Ranzani, O.T. Lessons From the COVID-19 Pandemic in Latin America: Vulnerability Leading to More Vulnerability. Am. J. Public Health 2022, 112, S579–S580. [Google Scholar] [CrossRef] [PubMed]
- Puertas, E.B.; Velandia-Gonzalez, M.; Vulanovic, L.; Bayley, L.; Broome, K.; Ortiz, C.; Rise, N.; Antelo, M.V.; Rhoda, D.A. Concerns, attitudes, and intended practices of Caribbean healthcare workers concerning COVID-19 vaccination: A cross-sectional study. Lancet Reg. Health—Am. 2022, 9, 100193. [Google Scholar] [CrossRef]
- Siani, A.; Tranter, A. Is vaccine confidence an unexpected victim of the COVID-19 pandemic? Vaccine 2022, 40, 7262–7269. [Google Scholar] [CrossRef]
- World Health Organization. Immunization Agenda 2030. A Global Strategy to Leave No One Behind. 2021, pp. 1–24. Available online: https://cdn.who.int/media/docs/default-source/immunization/strategy/ia2030/ia2030-draft-4-wha_b8850379-1fce-4847-bfd1-5d2c9d9e32f8.pdf?sfvrsn=5389656e_69&download=true (accessed on 26 December 2023).
- Hyndman, R.J.; Athanasopoulos, G. Forecasting: Principles and Practice. 2018. Available online: https://otexts.com/fpp2/ (accessed on 10 February 2023).
- Hale, T.; Angrist, N.; Goldszmidt, R.; Kira, B.; Petherick, A.; Phillips, T.; Webster, S.; Cameron-Blake, E.; Hallas, L.; Majumdar, S.; et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nat. Hum. Behav. 2021, 5, 529–538. [Google Scholar] [CrossRef] [PubMed]
- The World Bank. The World by Income and Region. 2022. Available online: https://datatopics.worldbank.org/world-development-indicators/the-world-by-income-and-region.html (accessed on 15 January 2024).
- Global Health Data Exchange. Gross Domestic Product per Capita 1960–2050. 2021. Available online: https://ghdx.healthdata.org/record/ihme-data/global-gdp-per-capita-1960-2050-fgh-2021 (accessed on 28 July 2023).
- The World Bank. Gini Index. 2023. Available online: https://data.worldbank.org/indicator/SI.POV.GINI (accessed on 26 December 2023).
- Mújica, Ó.J.; Moreno, C.M. De la retórica a la acción: Medir desigualdades en salud para “no dejar a nadie atrás” [From words to action: Measuring health inequalities to “leave no one behind”Da retórica à ação: Mensurar as desigualdades em saúde para não deixar ninguém atrás]. Rev. Panam. Salud Publica 2019, 43, e12. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Inequality Monitoring in Immunization: A Step-by-Step Manual; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- The R Foundation. The R Project for Statistical Computing. 2023. Available online: https://www.r-project.org (accessed on 10 February 2023).
- Yunusa, A.; Cabral, C.; Anderson, E. The impact of the COVID-19 pandemic on the uptake of routine maternal and infant vaccines globally: A systematic review. PLoS Glob. Public Health 2022, 2, e0000628. [Google Scholar] [CrossRef] [PubMed]
- Causey, K.; Fullman, N.; Sorensen, R.J.D.; Galles, N.C.; Zheng, P.; Aravkin, A.; Danovaro-Holliday, M.C.; Martinez-Piedra, R.; Sodha, S.V.; Velandia-González, M.P.; et al. Estimating global and regional disruptions to routine childhood vaccine coverage during the COVID-19 pandemic in 2020, a modelling study. Lancet 2021, 398, 522–534. [Google Scholar] [CrossRef] [PubMed]
- Lassi, Z.S.; Naseem, R.; Salam, R.A.; Siddiqui, F.; Das, J.K. The impact of the COVID-19 pandemic on immunization campaigns and programs: A systematic review. Int. J. Environ. Res. Public Health 2021, 18, 988. [Google Scholar] [CrossRef] [PubMed]
- Dalton, M.; Sanderson, B.; Robinson, L.J.; Homer, C.S.; Pomat, W.; Danchin, M.; Vaccher, S. Impact of COVID-19 on routine childhood immunisations in low- and middle-income countries: A scoping review. PLoS Glob. Public Health 2023, 3, e0002268. [Google Scholar] [CrossRef] [PubMed]
- Essoh, T.A.; Adeyanju, G.C.; Adamu, A.A.; Ahawo, A.K.; Aka, D.; Tall, H.; Aplogan, A.; Wiysonge, C.S. Early Impact of SARS-CoV-2 Pandemic on Immunization Services in Nigeria. Vaccines 2022, 10, 1107. [Google Scholar] [CrossRef] [PubMed]
- Firman, N.; Marszalek, M.; Gutierrez, A.; Homer, K.; Williams, C.; Harper, G.; Dostal, I.; Ahmed, Z.; Robson, J.; Dezateux, C. Impact of the COVID-19 pandemic on timeliness and equity of measles, mumps and rubella vaccinations in North East London: A longitudinal study using electronic health records. BMJ Open 2022, 12, e066288. [Google Scholar] [CrossRef]
- Bambra, C.; Riordan, R.; Ford, J.; Matthews, F. The COVID-19 pandemic and health inequalities. J. Epidemiol. Community Health 2020, 74, 964–968. [Google Scholar] [CrossRef]
- Spencer, N.; Markham, W.; Johnson, S.; Arpin, E.; Nathawad, R.; Gunnlaugsson, G.; Homaira, N.; Rubio, M.L.M.; Trujillo, C.J. The Impact of COVID-19 Pandemic on Inequity in Routine Childhood Vaccination Coverage: A Systematic Review. Vaccines 2022, 10, 1013. [Google Scholar] [CrossRef]
- Ahmed Ali, H.; Hartner, A.M.; Echeverria-Londono, S.; Roth, J.; Li, X.; Abbas, K.; Portnoy, A.; Vynnycky, E.; Woodruff, K.; Ferguson, N.M.; et al. Correction: Vaccine equity in low and middle income countries: A systematic review and meta-analysis. Int. J. Equity Health 2022, 21, 92. [Google Scholar] [CrossRef] [PubMed]
- Wigley, A.; Lorin, J.; Hogan, D.; Utazi, C.E.; Hagedorn, B.; Dansereau, E.; Tatem, A.J.; Tejedor-Garavito, N. Estimates of the number and distribution of zero-dose and under-immunised children across remote-rural, urban, and conflict-affected settings in low and middle-income countries. PLoS Glob. Public Health 2022, 2, e0001126. [Google Scholar] [CrossRef] [PubMed]
- Harrison, E.A.; Wu, J.W. Vaccine confidence in the time of COVID-19. Eur. J. Epidemiol. 2020, 35, 325–330. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, N.E.; SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Pan American Health Organization/World Health Organization. Epidemiological Alert Epidemiological situation in the Region of the Americas—29 January 2024. 2024. Available online: https://www.paho.org/en/documents/epidemiological-alert-measles-region-americas-29-january-2024 (accessed on 14 March 2024).
- Countries of the Caribbean Agree to Strengthen National Immunization Programs through Declaration of Nassau. 2023. Available online: https://www.paho.org/en/news/27-4-2023-countries-caribbean-agree-strengthen-national-immunization-programs-through (accessed on 15 August 2023).
- Organização Pan-Americana da Saúde. Brasil Lança Movimento Nacional para Ampliar Vacinação. 2023. Available online: https://www.paho.org/pt/noticias/28-2-2023-brasil-lanca-movimento-nacional-para-ampliar-vacinacao (accessed on 4 September 2023).
- Organização Pan-Americana da Saúde. No Senado do Brasil, Diretor da OPAS Destaca Importância de Intersetorialidade, Compromisso Político e Participação Social para Manter Alta a Cobertura de Vacinação. 2023. Available online: https://www.paho.org/pt/noticias/4-7-2023-no-senado-do-brasil-diretor-da-opas-destaca-importancia-intersetorialidade (accessed on 4 September 2023).
- La Organización Panamericana de la Salud. Al Ritmo de Muchachos, Argentina Tuvo su Festival de Vacunas, Música y Color. 2023. Available online: https://www.paho.org/es/noticias/27-4-2023-al-ritmo-muchachos-argentina-tuvo-su-festival-vacunas-musica-color (accessed on 4 September 2023).
- World Health Organization. Report of the SAGE Working Group on Quality and Use of Immunization and Surveillance Data 2019. Available online: https://terrance.who.int/mediacentre/data/sage/SAGE_Docs_Ppt_Oct2019/8_session_immunization_data/Oct2019_session8_SAGE-Data_WGreport.pdf (accessed on 10 August 2023).
- Velandia-González, M.; Vilajeliu, A.; Contreras, M.; Trumbo, S.P.; Pacis, C.; Ropero, A.M.; Ruiz-Matus, C. Monitoring progress of maternal and neonatal immunization in Latin America and the Caribbean. Vaccine 2021, 39, B55–B63. [Google Scholar] [CrossRef] [PubMed]
- COVID-19 National Preparedness Collaborators. Pandemic preparedness and COVID-19, an exploratory analysis of infection and fatality rates, and contextual factors associated with preparedness in 177 countries, from 1 Jan 2020, to 30 Sept 2021. Lancet 2022, 399, 1489–1512. [Google Scholar] [CrossRef]
- Llau, A.F.; Williams, M.L.; Tejada, C.E. National vaccine coverage trends and funding in Latin America and the Caribbean. Vaccine 2021, 39, 317–323. [Google Scholar] [CrossRef]
| DTPcv 1 | DTPcv3 | |||
|---|---|---|---|---|
| Variable | Median (IQR) | p-Value | Median (IQR) | p-Value |
| Vaccine administration in school | ||||
| Yes | −4.00 (−8.00; −1.00) | 0.98 | −3.00 (−8.00; −1.00) | 0.55 |
| No | −3.00 (−6.00; −1.50) | −4.00 (−7.50; −1.50) | ||
| School-closing policies | ||||
| None/recommended | −2.50 (−3.75; −1.25) | 0.37 | −1.50 (−3.75; 0.00) | 0.06 |
| Required | −3.00 (−7.25; −0.75) | −4.00 (−8.25; −1.75) | ||
| Stay-at-home policies | ||||
| None/recommended | −3.00 (−5.00; −2.00) | 0.60 | −3.00 (−6.00; −2.00) | 0.82 |
| Required | −3.00 (−7.00; 0.00) | −4.00 (−8.00; −1.00) | ||
| Closing of public transportation | ||||
| None | −3.00 (−5.00; −1.00) | 0.95 | −2.00 (−4.00; −1.00) | 0.40 |
| Recommended/required | −3.00 (−7.00; −1.00) | −4.00 (−8.00; −1.00) | ||
| WB income group | ||||
| High | −2.00 (−7.25; −1.00) | 0.57 | −2.00 (−4.75; −1.00) | 0.41 |
| Middle | −4.00 (−7.25; −1.75) | −4.00 (−8.50; −2.00) | ||
| GDP per capita | ||||
| High | −1.85 (−4.00; −1.00) | 0.18 | −2.08 (−4.00; 0.00) | 0.14 |
| Middle | −4.85 (−8.00; −1.00) | −5.15 (−8.00; −2.00) | ||
| Low | −5.08 (−7.00; −3.00) | −5.46 (−10.00; −2.00) | ||
| GINI index | ||||
| Less unequal | −1.50 (−2.75; 0.75) | 0.04 * | −2.50 (−4.00; −1.25) | 0.54 |
| More unequal | −5.00 (−7.00; −3.00) | −6.00 (−10.00; −1.00) | ||
| SDIx 2021 | ||||
| High | −2.00 (−7.00; 0.00) | 0.42 | −1.00 (−7.00; −1.00) | 0.65 |
| Middle | −6.00 (−8.00; −1.00) | −4.00 (−8.25; −2.00) | ||
| Low | −4.00 (−6.25; −2.75) | −6.00 (−10.50; −1.50) | ||
| Vaccine | Timepoint, Scenario | Vaccine Coverage (%) | Q1 v Q5 Inequality Gap | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q5 | Setting Average | Absolute Gap | Relative Gap | ||
| DTPcv1 | 2019 observed | 86.9 | 91.9 | 82.5 | 87.3 | 91.5 | 86.0 | −4.6 | 0.95 |
| 2021 predicted | 86.2 | 85.8 | 82.6 | 92.4 | 89.8 | 84.7 | −3.6 | 0.96 | |
| 2021 observed | 82.4 | 80.9 | 80.6 | 93.1 | 91.9 | 82.5 | −9.5 | 0.90 | |
| DTPcv3 | 2019 observed | 76.7 | 87.1 | 75.3 | 84.0 | 92.4 | 79.8 | −15.7 | 0.83 |
| 2021 predicted | 75.5 | 82.9 | 75.7 | 86.8 | 90.9 | 77.8 | −15.4 | 0.83 | |
| 2021 observed | 72.8 | 73.6 | 75.1 | 85.1 | 90.3 | 75.9 | −17.5 | 0.81 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castro-Aguirre, I.E.; Alvarez, D.; Contreras, M.; Trumbo, S.P.; Mujica, O.J.; Salas Peraza, D.; Velandia-González, M. The Impact of the Coronavirus Pandemic on Vaccination Coverage in Latin America and the Caribbean. Vaccines 2024, 12, 458. https://doi.org/10.3390/vaccines12050458
Castro-Aguirre IE, Alvarez D, Contreras M, Trumbo SP, Mujica OJ, Salas Peraza D, Velandia-González M. The Impact of the Coronavirus Pandemic on Vaccination Coverage in Latin America and the Caribbean. Vaccines. 2024; 12(5):458. https://doi.org/10.3390/vaccines12050458
Chicago/Turabian StyleCastro-Aguirre, Ignacio E., Dan Alvarez, Marcela Contreras, Silas P. Trumbo, Oscar J. Mujica, Daniel Salas Peraza, and Martha Velandia-González. 2024. "The Impact of the Coronavirus Pandemic on Vaccination Coverage in Latin America and the Caribbean" Vaccines 12, no. 5: 458. https://doi.org/10.3390/vaccines12050458
APA StyleCastro-Aguirre, I. E., Alvarez, D., Contreras, M., Trumbo, S. P., Mujica, O. J., Salas Peraza, D., & Velandia-González, M. (2024). The Impact of the Coronavirus Pandemic on Vaccination Coverage in Latin America and the Caribbean. Vaccines, 12(5), 458. https://doi.org/10.3390/vaccines12050458






