Abstract
Vaccination is one of the essential measures in reducing transmission, morbidity, and mortality rates of a disease. However, the COVID-19 vaccination is facing hesitancy across the globe, Malawi included. A population-based cross-sectional study was conducted in Malawi to document knowledge, attitudes, and practices on COVID-19 vaccination. The study targeted the general adult population and employed a multi-stage sampling technique. The Census Enumeration Areas within the 16 selected districts served as a primary sampling unit. Among the total 3068 participants, 1947 (63.6%) were female. About 1039 (34.1%) participants had primary education, while only 169 (5.5%) had college education. A total of 2936 (95.7%) participants knew about the COVID-19 vaccine, and 2063 (68.4%) felt that the COVID-19 vaccine was effective. A total of 1180 (38.7%) got vaccinated. Knowledge of the COVID-19 vaccination was significantly associated with participants’ education levels, location, occupation, marital status, household family income, and whether they were suffering from chronic illness or not. Overall, the level of knowledge and attitudes about the COVID-19 vaccination was good. This study has also established that different population groups have statistically different levels of knowledge and attitudes regarding COVID-19 vaccination. This study has also indicated a significant relationship between the rate of vaccination and several factors. Therefore, this calls for stakeholders to continue awareness and group-targeted tailored campaigns so as to increase COVID-19 vaccination.
1. Introduction
Coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a highly pathogenic virus initially discovered in Wuhan, Hubei Province, China [1]. The World Health Organization has recognized COVID-19 as an ongoing pandemic that affects world security and causes economic instability [2].
In Malawi, the first case of COVID-19 was recorded on April 2, 2020. In the subsequent weeks, sporadic transmission clusters emerged in large cities like Blantyre, Lilongwe, Zomba, and Mzuzu. Additional importations of COVID-19 cases occurred among migrants returning primarily from South Africa, which was the African country with the largest documented outbreak at the time [3]. The recorded incidence of SARS-CoV-2 then increased in the subsequent months. Until July 5, 2023, Malawi had reported 86,600 confirmed cases of COVID-19, and approximately 2646 died from the disease, representing a mortality rate of 3.1%. This rate is higher as compared with the African rate of 1.8% and the global fatality rate of 1.2% [4]. This COVID-19 fatality rate in Malawi is also high if compared with neighboring countries like Zimbabwe (2.2%) and Zambia (1.3%) [4,5,6]. Likely, this is why Malawi appears to be in position 132 out of 230 countries currently reporting on COVID-19 [4,6]. However, when mortality is reported on a per 100,000 population basis, COVID-19 mortality in Malawi (14.04) was lower than that in Zambia (22.07) or Zimbabwe (38.16) [7].
Since the beginning of the pandemic, Malawi has experienced a total of four COVID-19 waves, with the second being the most severe. In response, the Malawi government instituted policies to promote the prevention of new infections. Among the preventative measures, vaccination was one of the key interventions adopted by the Ministry of Health when the vaccine became available. Johnson & Johnson, AstraZeneca, and Pfizer vaccines are some of the COVID-19 vaccines that have been approved and rolled out in Malawi. Studies have revealed that people have varying levels of knowledge, attitudes, and practices regarding vaccination, hence increasing the levels of COVID-19 hesitancy [8,9,10,11,12].
Few Knowledge, Attitudes, and Practices (KAP) studies conducted in Malawi have focused on COVID-19 preventive measures in selected districts. Despite Malawi rolling out a COVID-19 vaccination program for over a year, the vaccine uptake is very low. However, countrywide KAP studies to gauge why the vaccine uptake is low are limited. Such studies are crucial to identifying the factors contributing to low vaccine uptake and hesitancy.
Evidence suggests that public knowledge is vital in tackling pandemics [13]. Knowledge, attitudes, and practices (KAP) of the general population studies can provide useful insights to policymakers in designing proper interventions for controlling COVID-19. For instance, a KAP study conducted by Lee in South Korea established that knowledge directly influenced attitudes (e.g., perceived risk and efficacy beliefs) and practices [9]. However, a study by Islam conducted in Bangladesh established insufficient knowledge but more positive attitudes toward the COVID-19 vaccine among the general population. Therefore, he recommended an instant health education program to be initiated so as to enhance mass COVID-19 vaccination [14]. Thus, the primary objective of this study was to assess knowledge, attitudes, and practices toward COVID-19 vaccination and its associated factors among the general adult population in Malawi so as to guide the policy direction in combating the COVID-19 pandemic in Malawi.
2. Methodology
2.1. Study Design
This study employed a population-based cross-sectional study design as it aimed at capturing current individual knowledge, attitudes, and practices on COVID-19 vaccinations at a single point in time to enlighten related stakeholders like policymakers and practitioners.
2.2. Study Setting and Period
The study was conducted in 16 selected districts from the three regions of Malawi, namely, northern, central, and southern. The districts within the regions of Malawi were selected based on the level of SARS-CoV-2 burden in the area, as this served as a guide in health resource allocation and interventions (Supplementary Materials 1, Table S1). The study data was collected in the months of June and July 2022.
2.3. Target Population
The study targeted adult respondents (aged 18 years and above) of the male and female genders residing in rural and urban communities of selected districts from the northern, central, and southern regions of Malawi [8,9,10,11,12].
2.4. Sampling Technique and Tools
The study employed a multi-stage sampling technique to select participants from each district who satisfied the inclusion criteria. At the regional level, districts were stratified into high and low SARS-CoV-2 burden areas. The COVID-19 disease burden of the district was calculated as the proportion of the total number of confirmed COVID-19 cases to the total district population (Supplementary Materials 1, Table S1) [15,16]. Districts falling into the two strata (low and high) of the SARS-CoV-2 burden were purposefully selected from each region.
Four representative districts were selected from the northern region of Malawi, namely Mzimba and Likoma, which were high COVID-19 burden areas, while Chitipa and Nkhatabay were low COVID-19 burden areas. In the central region of Malawi, Lilongwe, Ntchisi, and Salima were selected as high COVID-19 burden areas, while Ntcheu and Dedza were selected as low COVID-19 burden areas. In the southern region of Malawi, Blantyre, Neno, and Zomba were selected as high COVID-19 burden areas, while Machinga, Thyolo, Chikwawa, and Nsanje were selected as low COVID-19 burden areas. The number of participants to be sampled in each district was calculated using the following formula:
Details of the total number of participants sampled in every district are provided in Supplementary Materials 1, Table S1, while the number of enumeration areas and households per district is provided in Supplementary Materials 2, Table S2.
Census Enumeration Areas within the selected district, as defined for the 2018 Malawi Census, served as primary sampling units (see Supplementary Materials 2, Table S2). The enumeration area (EA) was defined as the smallest functional area with clearly defined boundaries on the map, in tandem with the workload given to a single census enumerator. On average, an enumeration area had 215 households. The enumeration areas falling within the sampling frame of the selected district within the regions of Malawi were geographically stratified by urban/rural code, traditional authority, and EA codes in line with a probability proportionate to size [17].
A sampling frame comprising a list of households in the enumeration area was created. Systematic random sampling was employed to select households. One eligible participant as a unit of analysis was randomly selected within each household. We used a structured questionnaire, which was translated from English to major local languages such as Chichewa and Chitumbuka to capture all required data. We piloted 2% of the targeted sample size among individuals outside the target population. After piloting the questionnaire, we modified it and made it fit for the study. The questionnaire sections consisted of demographic characteristics, questions on knowledge (awareness of the availability, types, side effects, who is eligible, etc.), questions on attitudes (reliability, safety, effectiveness, etc.), and questions on practices (action taken to get vaccinated and challenges faced).
2.5. Sample Size Calculation
The sample size was determined using the single population proportion formula by Kish, considering the following statistical assumptions: 95% confidence level, 0.73 from a pooled global KAPS on COVID-19, and 2% margin of error [14,15,18]. The following single-proportion formula was used:
where n = initial sample size, z = 1.96, the corresponding z-score for the 95% CI, p = proportion (73%), and d =margin of error (0.02). The initial sample size for the study was 1893 and was adjusted for a 10% non-response rate and a design effect of 1.5, giving the final sample size of 3155.
2.6. Data Quality Assurance
Well-trained research assistants who were fluent in the local languages and familiar with the local customs were recruited to collect the data. Investigators and supervisors strictly monitored the data collection process. The data collected were securely kept at the Public Health Institute of Malawi (PHIM).
2.7. Data Analysis
Statistical Package for the Social Sciences (SPSS) was used for data cleaning, editing, sorting, and coding. Descriptive statistics (i.e., frequencies, percentages, means, and standard deviations) and first-order analysis (i.e., chi-square tests and Fisher’s exact tests) were performed using SPSS Version 25 (Chicago, IL, USA). A Pearson chi-square test was performed to determine the association of equally weighted above-median composite binary variables from knowledge, attitudes, and practices scores on COVID-19 vaccination with socio-demographic information. All statistical tests were considered significant at a 95% confidence interval with a p-value of less than 0.05.
To calculate the composite scores on knowledge, seven questions with responses coded as No or Yes, including the following: Do you know about the COVID-19 vaccine; Which COVID-19 vaccines are currently being administered in Malawi; Is it dangerous to use vaccine overdose; Does vaccination increase allergic reactions; Children do not require to get the COVID-19 vaccine; And a vaccine against COVID-19 is available free of charge, were used to assess knowledge. One point was assigned for each correct response, yielding a COVID-19 knowledge composite score of 0 to 7. Individuals who scored at or above the median on the COVID-19 vaccine knowledge items were classified as having good knowledge; those who scored below the median were classified as having poor knowledge [19]. To calculate the composite scores on attitude, five questions were rated using a three-point Likert scale: undecided (0), disagree (1), agree (2), including “do not rely on the COVID-19 vaccine due to emergency development during a pandemic; vaccination is not required because immunity will be acquired naturally by infection; the newly discovered COVID-19 vaccine is safe; it is not possible to reduce the incidence of COVID-19 without vaccination; and in favor of the vaccine against COVID-19 because it is effective and safe”. Respondents who scored above the median on the COVID-19 vaccine attitude items were classified as having a favorable attitude toward the COVID-19 vaccination, and those who scored otherwise were classified as having a not favorable attitude [20].
2.8. Ethical Consideration
Ethical clearance for the study was obtained from the NHSRC (approval number: Protocol #22/03/2888). An approval letter to conduct the study was obtained from the Principal Secretary for Health. Permission to conduct the study in each village was sought from the traditional authorities (TA) or village headmen, and written consent was obtained from each participant before administering the questionnaire. The questionnaire was coded instead of using names as identification markers, and hence, confidentiality was ensured throughout the study.
3. Results
3.1. Socio-Demographic Characteristics of Study Participants
A total of 3068 individuals participated in the study (Table 1). Among these, 1947 (63.6%) were female and 1116 (36.4%) were male. The majority of the study participants were in the age group of 18–60 (92%). About 1039 (34.1%) participants had incomplete primary education; 626 (20.6%) did not complete their secondary education; 527 (17.3%) and 359 (11.8%) completed secondary and primary education, respectively; 326 (10.7%) did not have any educational background; and 169 (5.5%) had at least a college education background. The participants were from 16 different districts in Malawi, with 2046 (66.7%) from urban settings and 1022 (33.3%) from rural locations. Among these, 2755 (90.7%) belonged to the Christian religion. Notably, 1498 (49.9%) were unemployed, while 1322 (43.9%) were businesspersons, and 85 (6.2%) were employed. Additionally, most of the respondents (2086; 69.3%) were married. Worth noting was that 1816 (60.3%) respondents’ monthly household income was less than MK35,000, followed by 534 (17.7%) in the range of MK 35,000 to MK 50,000, 370 (12.3%) within MK 51,000 to MK100,000, 267 (8.9%) within MK100,000 to MK500,000, and lastly 24 (0.8%) earning over MK500,000 per month. Most of the participants did not have chronic illnesses (85.9%); however, 52 (1.7%) reported a history of respiratory and lung disease, and 152 (5%) had HIV/AIDS.

Table 1.
Socio-Demographic Factors.
3.2. Knowledge, Attitudes, and Practices of COVID-19 Vaccination
Remarkably, 2936 (95.7%) knew about the COVID-19 vaccine, and 2063 (68.4%) were aware that the vaccine is effective (Table 2). Knowledge on which COVID-19 vaccine was being administered in Malawi varied among respondents, with 1639 (53.4%), 1840 (60.0%), and 817 (26.6%) indicating it was AstraZeneca, Johnson & Johnson, and Pfizer, respectively (Table 1). About 1006 (33.5%) had perceived knowledge that vaccination increases allergic reactions, while only 765 (26.4%) professed that vaccination increases autoimmune diseases (Table 2). Additionally, 1228 (41.5%) indicated that children do not require COVID-19 vaccination, and 2736 (91.3%) were aware that vaccination against COVID-19 was available for free (Table 2).

Table 2.
Knowledge of Vaccination.
Almost 49.72% were of the view that the COVID-19 vaccine is reliable, although it was developed hastily; however, 31.75% thought it was not proper to rely on such a type of vaccine (Figure 1A). Nearly 64.48% indicated that vaccination was not necessary as one could become immune after infection (Figure 1B). On the contrary, 23.9% thought irrespective of natural immunity, vaccination was still necessary (Figure 1B). Approximately 69.29% of respondents thought the COVID-19 vaccine was safe, whereas 19.42% thought the vaccine was unsafe, and 11.34% were unsure of the safety of the vaccine (Figure 1C). Around 57.1% of study participants thought COVID-19 vaccination was critical in reducing the incidence of COVID-19, but 29.74% indicated that the incidence of the disease could decrease without vaccination (Figure 1D). Largely, 70.2% indicated that COVID-19 vaccines were safe and they would undoubtedly get vaccinated (Figure 1E). Nevertheless, 12.55% questioned the safety of the vaccine and expressed their hesitance to get vaccinated, whereas 17.23% were not sure whether the vaccine was safe or if they would get vaccinated (Figure 1E).

Figure 1.
Attitudes of participants towards COVID-19 vaccine. (A) Do not rely on the COVID-19 vaccine due to emergency developments during the pandemic. (B) Vaccination is not required because immunity will be acquired naturally by infection. (C) The newly discovered COVID-19 vaccine is safe. (D) It is not possible to reduce the incidence of COVID-19 without vaccination. (E) COVID-19 Vaccines are safe, and I will take the COVID-19 vaccine without any hesitation.
Concerning vaccination practices, only 1180 (38.7%) got vaccinated, while 1796 (58.9%) never got vaccinated, and 43 (1.4%) went to vaccination centers but were not offered the service (Figure 2).
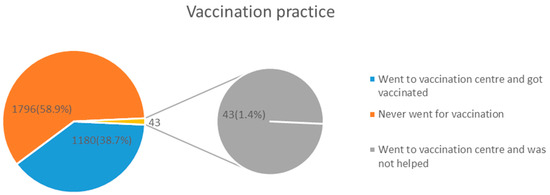
Figure 2.
COVID-19 vaccination practices among study respondents.
3.3. Factors Influencing Knowledge, Attitudes, and Practices towards Coronavirus Disease 19 Vaccination
Knowledge of the COVID-19 vaccination was significantly associated (p < 0.05) with participants’ education levels, location, occupation, marital status, household family income, and whether they were suffering from chronic illness or not (Table 3). It was also observed that there was a significant (p < 0.05) relationship between the respondents’ attitudes towards COVID-19 vaccination and denomination. Furthermore, there was a significant relationship (p < 0.05) between the rate of vaccination and the respondents’ gender, age, level of education, region, location, occupation, marital status, family size, monthly income, and whether they had a chronic illness or not (Table 3).

Table 3.
Association of COVID-19 vaccination knowledge, attitudes, and practices with socio-demographic and health-related factors.
4. Discussion
The present study aimed at assessing the current knowledge, attitudes, and practices (KAP) of Malawians towards the COVID-19 vaccination. The study involved 3068 individuals from 16 districts with varying adult age groups, genders, levels of education, location, denomination, marital status, health condition, levels of monthly income, knowledge, attitudes, and practices about COVID-19 vaccination.
Unlike most studies conducted elsewhere in Africa, participants in this study showed a high (97.2%) level of knowledge regarding the COVID-19 vaccine, with 68.4% having a positive attitude towards the COVID-19 vaccine as being effective [9,21,22,23]. It is more likely that our study participants could have a better level of knowledge compared to previous studies since vaccination campaigns have been on different platforms for over a year now with massive campaigns through different media outlets. For instance, in a study that was conducted in South Korea before the COVID-19 mass vaccination began, the level of knowledge was very low [14]. This is an encouraging finding, as it shows the public is very aware of the vaccine and has a relatively better attitude. However, just like reports from other studies [8,23,24], it is worrisome that some misconceptions about the vaccine exist. Likely, this is why only about 38.7% indicated having been vaccinated. However, this reported vaccination rate was still high as compared to the vaccination rate indicated on the MoH COVID-19 Dashboard (8.3%). This likely could be due to the fact that our study mainly targeted adults, while the MoH online shows a percentage against the total national population [4]. It is also likely to be biased due to self-reporting on vaccine status, where the majority may prefer to report what is expected of them, unlike their actual status.
This study has discovered that knowledge of the COVID-19 vaccination was significantly associated with participants’ level of education, location, occupation, marital status, denomination, household family income, and whether they were suffering from chronic illness or not (p < 0.05).
These findings, particularly for education levels and gender, are very similar to other studies conducted elsewhere [9,14,24,25,26]. This could be due to the fact that being a pandemic, most COVID-19 information is still in international languages like English and mostly spread through social media, posing a big challenge for non-educated people and the female gender in our context.
As reported in other studies [9,14], the decision to receive the COVID-19 vaccine is a controversial aspect with a critical diversity in most epidemiological and demographic characteristics. This is why it has been observed that despite a good number of people having insignificant differences in terms of knowledge and attitudes towards vaccinations, a significant relationship was observed between the rate of vaccination and the respondent’s gender, age, level of education, region, location, occupation, marital status, family size, monthly income, and whether they had a chronic illness or not. This may require detailed unpacking of these differences so as to tailor individualized group-centered messages, which can help increase vaccine uptake. For instance, a message targeting a less or uneducated population needs to be well translated into local languages that can be easily understood by them. For instance, a multinational Delphi consensus to end the COVID-19 public health threat study suggests the need for the messages to clearly explain the efficacy and limitations of all the available vaccines in preventing SARS-CoV-2 transmission and reducing the severity of COVID-19 to the general public [27]. In addition, they recommend the engagement of trusted local leaders and organizations in vaccination efforts, especially in settings where individuals have lower levels of trust in government. It is, therefore, important to unpack the details of these findings and establish the potential individual concerns that may be precursors to vaccine hesitancy. As such, tailored messages that address the underlying bases of an individual’s concerns should be used in targeted public health communications [27].
Furthermore, there is a need to devise a mechanism to reach out to the masses, especially those who do not have access to social media. There is also a need to incorporate the vaccine messages into local village meetings and gatherings. Some of these approaches have been proposed and used in other settings [14]. As noted in other studies, there is a need to make an effort to develop strategies that can positively align with the attitude of the public towards vaccines since negative perceptions about COVID-19 vaccines are associated with poor rates of COVID-19 vaccination [15,28]. Lazarus, J.V (2022) [27] suggested that community leaders, scientific experts, and public health authorities should collaborate to develop public health messages that build and enhance individual and community trust and use the preferred means of access and communication for different populations. Furthermore, in coming up with the messages, public health professionals and authorities should combat false information proactively based on clear, direct, culturally responsive messaging that is free of unnecessary scientific jargon. These recommendations are in line with our study findings, which have shown that vaccination uptake is severely hampered due to several factors that cannot be easily achieved using foreign policies alone but locally tailored approaches.
5. Conclusions
Overall, the level of knowledge and attitudes about the COVID-19 vaccination was good. This study has also established that different population groups have statistically different levels of knowledge and attitudes regarding COVID-19 vaccination. Furthermore, this study has also indicated a significant relationship between the rate of vaccination and the respondent’s gender, age, level of education, region, location, occupation, marital status, family size, monthly income, and whether they had a chronic illness or not.
6. Recommendations
The government of Malawi should keep on promoting the awareness and attitudes campaign on COVID-19 vaccinations. This report may be used when designing public communications interventions since it is the first of its kind and gives a comprehensive available level of COVID-19 KAP on vaccination, hence the need for public dissemination of this report. COVID-19 Vaccine communication strategies are required and need to be emphasized to increase vaccine acceptability. There is a need to tailor the COVID-19 vaccine message which can focus on particular groups; for instance, those with little or no education need to have locally tailored messages in local languages. Future research may focus on longitudinal studies and comparative analyses to build upon these findings.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/vaccines12030221/s1, Table S1: COVID-19 disease burden and sample size. Source: Malawi COVID-19 epidemiological report, Epi Week 8 2022: NSO, 2020; Table S2: Sample sheet of Enumeration areas (EA) and households per district.
Author Contributions
M.R.O.C. was involved in study conception, study design, data collection, data analysis, and manuscript preparation; D.K. was involved in study design, data collection, data analysis, and manuscript preparation; S.E.M. was also involved in study design, data collection, data analysis, and manuscript preparation; B.C.M. took part in study design, data collection, data analysis, and manuscript preparation; R.M. took part in study design, data collection, data analysis, and manuscript preparation; P.K. was involved study design, data collection, data analysis, and manuscript preparation; B.C. was involved in study design, data collection, data analysis, and manuscript preparation; M.C. was involved in data collection, data analysis, and manuscript preparation; B.N. was involved in study design, data collection, data analysis, and manuscript preparation; C.S. was involved in data collection and manuscript preparation; J.G. was involved in data collection and manuscript preparation; C.M. (Collins Mitambo) was involved in data collection and manuscript preparation; A.D. was involved in data collection and manuscript preparation; L.C. was involved in study design, data collection, and manuscript preparation; M.T. was involved in study design, data collection, and manuscript preparation; C.M. (Charity Muwalo) was involved in study design, data collection, and manuscript preparation; M.K. was involved in study design, data collection, and manuscript preparation; and E.C.B. was involved in study design, data collection, analysis, and manuscript preparation. All the authors contributed adequately to the completion of this study. Their career background played roles in this study. All authors were fully involved and took the time to read and verify the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by the World Bank (IDA-D8870). We thank the research funding support from the World Bank.
Institutional Review Board Statement
Ethical approval to conduct the study was obtained from the National Health Science Research Committee (Approval number; Protocol # 22/03/2888), and permission was also obtained from the Public Health Institute of Malawi (PHIM) and Ministry of Health Headquarters on behalf of all the districts involved in the study. Permissions were obtained from the district commissioners of each district and the involved Traditional authorities (TA). Thereafter, each Sub-TA, group village head, and then village headman was alerted and asked to give permission for their respective areas to be involved in the study.
Informed Consent Statement
Informed consent was obtained from each participant before being enrolled in the study. Interviews were only allowed upon getting consent and with strict caution on privacy and confidentiality. Study participant identifications were being used instead of names so as to make sure to protect the participants.
Data Availability Statement
The data for the study are available from the corresponding author upon reasonable request.
Acknowledgments
First, we thank Almighty God for granting us the opportunity to conduct this study and write this paper. Furthermore, we thank the staff of PHIM and all the institutions involved in the technical support throughout the research implementation process. We also thank all the data collectors involved in this study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Stringhini, S.; Zaballa, M.-E.; Pullen, N.; Perez-Saez, J.; de Mestral, C.; Loizeau, A.J.; Lamour, J.; Pennacchio, F.; Wisniak, A.; Dumont, R.; et al. Seroprevalence of anti-SARS-CoV-2 antibodies 6 months into the vaccination campaign in Geneva, Switzerland, 1 June to 7 July 2021. Euro Surveill. 2021, 26, 1–8. [Google Scholar] [CrossRef]
- WHO. COVID-19 Vaccine Efficacy, Effectiveness and Protection. 2021. Available online: https://www.who.int/news-room/feature-stories/detail/vaccine-efficacy-effectiveness-and-protection (accessed on 1 November 2023).
- Chisale, M.R.O.; Nyambalo, B.W.; Mitambo, C.; Kumwenda, P.; Mwale, S.E.; Mbakaya, B.C. Comparative characterisation of COVID-19 patients with hypertension comorbidity in Malawi: A 1:2 matched retrospective case-control study. IJID Reg. 2022, 2, 25–29. [Google Scholar] [CrossRef]
- Ministry of Health Malawi. COVID-19 Malawi Dashboard. 2022. Available online: https://covid19.health.gov.mw/ (accessed on 31 March 2022).
- World Health Organization. COVID-19 Vaccinations. 2023. Available online: https://covid19.who.int/?mapFilter=vaccinations (accessed on 2 January 2023).
- Reuters. COVID-19 Vaccine Tracker. 2023. Available online: https://www.reuters.com/graphics/world-coronavirus-tracker-and-maps/vaccination-rollout-and-access/ (accessed on 2 January 2023).
- Johns Hopkins University. COVID-19 Mortality Analyses. 2023. Available online: https://coronavirus.jhu.edu/data/mortality (accessed on 22 January 2024).
- Reuben, R.C.; Danladi, M.M.A.; Saleh, D.A.; Ejembi, P.E. Knowledge, Attitudes and Practices Towards COVID-19: An Epidemiological Survey in North-Central Nigeria. J. Community Health 2021, 46, 457–470. [Google Scholar] [CrossRef]
- Lee, S.K.; Sun, J.; Jang, S.; Connelly, S. Misinformation of COVID-19 vaccines and vaccine hesitancy. Sci. Rep. 2022, 12, 13681. [Google Scholar] [CrossRef]
- Acharya, S.R.; Moon, D.H.; Shin, Y.C. Assessing Attitude Toward COVID-19 Vaccination in South Korea. Front. Psychol. 2021, 12, 1–6. [Google Scholar] [CrossRef]
- Graham, M.S.; May, A.; Varsavsky, T.; Sudre, C.; Murray, B.; Klaser, K.; Antonelli, M.; Canas, L.; Molteni, E.; Modat, M.; et al. Knowledge barriers in the symptomatic-COVID-19 testing programme in the UK: An observational study. medRxiv 2021. [Google Scholar] [CrossRef]
- Li, Y.; Liu, G.; Egolet, R.O.; Yang, R.; Huang, Y.; Zheng, Z. Knowledge, attitudes, and practices related to COVID-19 among Malawi adults: A community-based survey. Int. J. Environ. Res. Public Health 2021, 18, 4090. [Google Scholar] [CrossRef]
- Chirwa, G.C. ‘Who knows more, and why?’ Explaining socioeconomic-related inequality in knowledge about HIV in Malawi. Sci. Afr. 2020, 7, e00213. [Google Scholar] [CrossRef]
- Islam, S.; Siddique, A.B.; Akter, R.; Tasnim, R.; Sujan, S.H.; Ward, P.R.; Sikder, T. Knowledge, attitudes and perceptions towards COVID-19 vaccinations: A cross-sectional community survey in Bangladesh. BMC Public Health 2021, 21, 1851. [Google Scholar] [CrossRef]
- Sengupta, M.; Dutta, S.; Roy, A.; Chakrabarti, S.; Mukhopadhyay, I. Knowledge, attitude and practice survey towards COVID-19 vaccination: A mediation analysis. Int. J. Health Plan. Manag. 2022, 37, 2063–2080. [Google Scholar] [CrossRef]
- Brynildsrud, O. COVID-19 prevalence estimation by random sampling in population—Optimal sample pooling under varying assumptions about true prevalence. BMC Med. Res. Methodol. 2020, 20, 196. [Google Scholar] [CrossRef]
- Wiegand, R.P. An Analysis of Cooperative Coevolutionary Algorithms; George Mason University: Fairfax, VA, USA, 2003; pp. 1–115. [Google Scholar]
- Wiegand, H. Kish, L.: Survey Sampling; John Wiley & Sons, Inc.: New York, London 1965, IX + 643 S., 31 Abb., 56 Tab., Preis 83 s. Biom. J. 1968, 10, 88–89. [Google Scholar] [CrossRef]
- Azene, Z.N.; Merid, M.W.; Muluneh, A.G.; Geberu, D.M.; Kassa, G.M.; Yenit, M.K.; Tilahun, S.Y.; Gelaye, K.A.; Mekonnen, H.S.; Azagew, A.W.; et al. Adherence towards COVID-19 mitigation measures and its associated factors among Gondar City residents: A community-based cross-sectional study in Northwest Ethiopia. PLoS ONE 2020, 15, e0244265. [Google Scholar] [CrossRef]
- Khamis, F.; Badahdah, A.; Al, N.; Furqan, M.; Lawati, A.; Al, J. Attitudes Towards COVID-19 Vaccine: A Survey of Health Care Workers in Oman. J. Epidemiol. Glob. Health 2022, 12, 1–6. [Google Scholar] [CrossRef]
- Al-Marshoudi, S.; Al-Balushi, H.; Al-Wahaibi, A.; Al-Khalili, S.; Al-Maani, A.; Al-Farsi, N.; Al-Jahwari, A.; Al-Habsi, Z.; Al-Shaibi, M.; Al-Msharfi, M.; et al. Knowledge, attitudes, and practices (Kap) toward the COVID-19 vaccine in Oman: A pre-campaign cross-sectional study. Vaccines 2021, 9, 602. [Google Scholar] [CrossRef]
- Cheng, J.Y.J.; Loong, S.S.E.; Ho, C.E.S.M.; Ng, K.J.; Ng, M.M.Q.; Chee, R.C.H.; Chin, T.X.L.; Fong, F.J.Y.; Goh, S.L.G.; Venkatesh, K.N.S.; et al. Knowledge, Attitudes, and Practices of COVID-19 Vaccination among Adults in Singapore: A Cross-Sectional Study. Am. J. Trop. Med. Hyg. 2022, 107, 540–550. [Google Scholar] [CrossRef]
- Sinuraya, R.K.; Kusuma, A.S.W.; Pardoel, Z.E.; Postma, M.J.; Suwantika, A.A. Parents’ Knowledge, Attitude, and Practice on Childhood Vaccination During the COVID-19 Pandemic in Indonesia. Patient Prefer. Adherence 2022, 16, 105–112. [Google Scholar] [CrossRef]
- Hossain, M.A.; Jahid, I.K.; Hossain, K.M.A.; Walton, L.M.; Uddin, Z.; Haque, O.; Kabir, F.; Arafat, S.M.Y.; Sakel, M.; Faruqui, R.; et al. Knowledge Attitudes and fear of COVID-19 during the Rapid Rise Period in Bangladesh. PLoS ONE 2020, 15, e0239646. [Google Scholar] [CrossRef]
- Banik, R.; Rahman, M.; Sikder, M.T.; Rahman, Q.M.; Pranta, M.U.R. Knowledge, attitudes, and practices related to the COVID-19 pandemic among Bangladeshi youth: A web-based cross-sectional analysis. J. Public Health 2023, 31, 9–19. [Google Scholar] [CrossRef]
- Rahman, S.M.M.; Akter, A.; Mostary, K.F.; Ferdousi, S.; Ummon, I.J.; Mubdi-Un-Naafi, S.; Rahman, M.M.; Uddin, M.G.M.N.; Tasmin, S.; Uddin, M.A.; et al. Assessment of knowledge, attitudes and practices towards prevention of coronavirus disease (COVID-19) among Bangladeshi population. Bangladesh Med. Res. Counc. Bull. 2020, 46, 73–82. [Google Scholar] [CrossRef]
- Adane, M.; Ademas, A.; Kloos, H. Knowledge, attitudes, and perceptions of COVID-19 vaccine and refusal to receive COVID-19 vaccine among healthcare workers in Northeastern Ethiopia. BMC Public Health 2022, 22, 128. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, J.V.; Romero, D.; Kopka, C.J.; Karim, S.A.; Abu-Raddad, L.J.; Almeida, G.; Baptista-Leite, R.; Barocas, J.A.; Barreto, M.L.; Bar-Yam, Y.; et al. A multinational Delphi consensus to end the COVID-19 public health threat. Nature 2022, 611, 332–345. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).