T Cell Responses against Orthopoxviruses in HIV-Positive Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Volunteers
2.2. ELISpot Assay
2.3. Statistical Analysis
3. Results
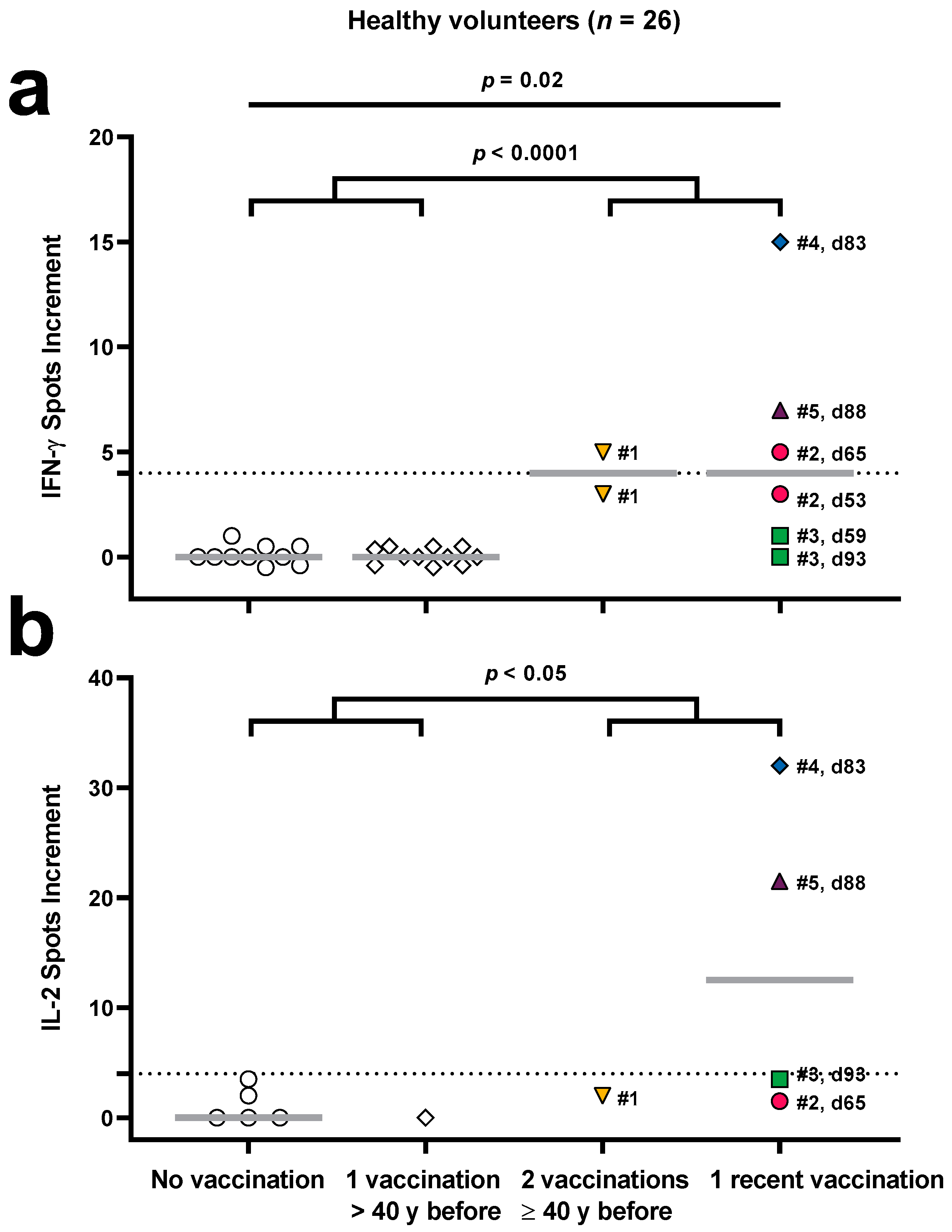
3.1. Validation of an Orthopoxvirus-Specific ELISpot Assay in Healthy Volunteers
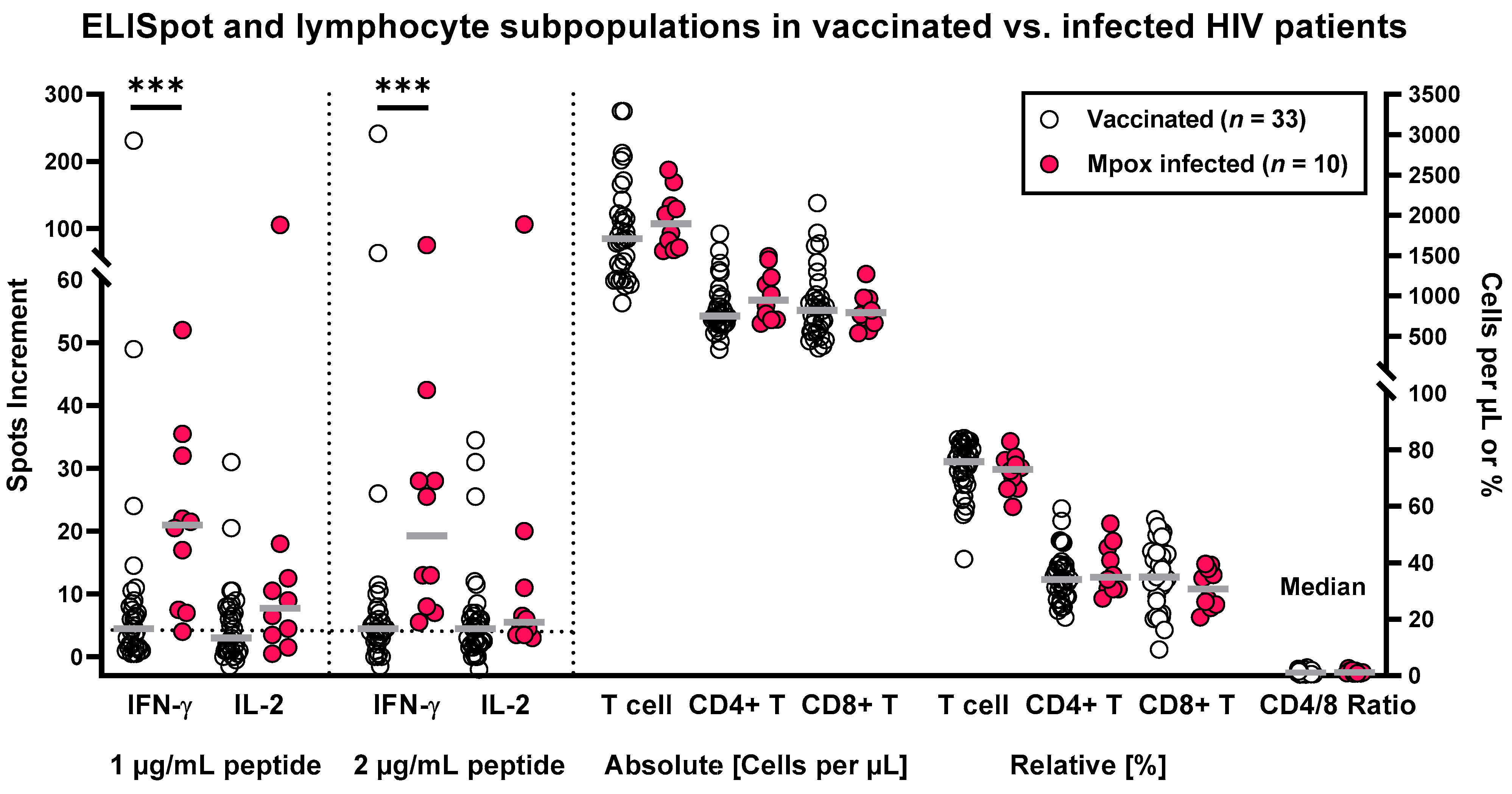
3.2. Orthopoxvirus-Specific ELISpot Results in HIV-Positive Patients after Vaccination and Infection
3.3. Correlation of ELISpot Results and Patient Characteristics
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- CDC. 2023 U.S. Map & Case Count, Data as of 26 October 2023. Available online: https://www.cdc.gov/poxvirus/monkeypox/response/2022/us-map.html (accessed on 17 November 2023).
- WHO. Mpox (Monkeypox), Key Facts. 18 April 2023. Available online: https://www.who.int/news-room/fact-sheets/detail/monkeypox (accessed on 17 November 2023).
- ECDC. Joint ECDC-WHO Regional Office for Europe Mpox Surveillance Bulletin. 9 October 2023. Available online: https://monkeypoxreport.ecdc.europa.eu/ (accessed on 17 November 2023).
- EMA. Imvanex (Modifiziertes Vacciniavirus Ankara, Lebend). Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwjl4vWyvN36AhVNDuwKHYRHBhYQFnoECA0QAQ&url=https%3A%2F%2Fwww.ema.europa.eu%2Fen%2Fdocuments%2Foverview%2Fimvanex-epar-medicine-overview_de.pdf&usg=AOvVaw2ruvZ3i59hjLsvlh4pvszi (accessed on 17 November 2023).
- Earl, P.L.; Americo, J.L.; Wyatt, L.S.; Eller, L.A.; Whitbeck, J.C.; Cohen, G.H.; Eisenberg, R.J.; Hartmann, C.J.; Jackson, D.L.; Kulesh, D.A.; et al. Immunogenicity of a highly attenuated MVA smallpox vaccine and protection against monkeypox. Nature 2004, 428, 182–185. [Google Scholar] [CrossRef]
- Aden, D.; Zaheer, S.; Kumar, R.; Ranga, S. Monkeypox (Mpox) outbreak during COVID-19 pandemic-Past and the future. J. Med. Virol. 2023, 95, e28701. [Google Scholar] [CrossRef]
- Overton, E.T.; Lawrence, S.J.; Stapleton, J.T.; Weidenthaler, H.; Schmidt, D.; Koenen, B.; Silbernagl, G.; Nopora, K.; Chaplin, P. A randomized phase II trial to compare safety and immunogenicity of the MVA-BN smallpox vaccine at various doses in adults with a history of AIDS. Vaccine 2020, 38, 2600–2607. [Google Scholar] [CrossRef] [PubMed]
- Walsh, S.R.; Wilck, M.B.; Dominguez, D.J.; Zablowsky, E.; Bajimaya, S.; Gagne, L.S.; Verrill, K.A.; Kleinjan, J.A.; Patel, A.; Zhang, Y.; et al. Safety and immunogenicity of modified vaccinia Ankara in hematopoietic stem cell transplant recipients: A randomized, controlled trial. J. Infect. Dis. 2013, 207, 1888–1897. [Google Scholar] [CrossRef]
- Jezek, Z.; Khodakevich, L.N.; Wickett, J.F. Smallpox and its post-eradication surveillance. Bull. World Health Organ. 1987, 65, 425–434. [Google Scholar] [PubMed]
- Simpson, K.; Heymann, D.; Brown, C.S.; Edmunds, W.J.; Elsgaard, J.; Fine, P.; Hochrein, H.; Hoff, N.A.; Green, A.; Ihekweazu, C.; et al. Human monkeypox—After 40 years, an unintended consequence of smallpox eradication. Vaccine 2020, 38, 5077–5081. [Google Scholar] [CrossRef]
- Papukashvili, D.; Rcheulishvili, N.; Liu, C.; Wang, X.; He, Y.; Wang, P.G. Strategy of developing nucleic acid-based universal monkeypox vaccine candidates. Front. Immunol. 2022, 13, 1050309. [Google Scholar] [CrossRef] [PubMed]
- Koldehoff, M.; Horn, P.A.; Lindemann, M. Cellular Immune Response after Vaccination with an Adjuvanted, Recombinant Zoster Vaccine in Allogeneic Hematopoietic Stem Cell Transplant Recipients. Vaccines 2022, 10, 809. [Google Scholar] [CrossRef]
- Schwarzkopf, S.; Krawczyk, A.; Knop, D.; Klump, H.; Heinold, A.; Heinemann, F.M.; Thummler, L.; Temme, C.; Breyer, M.; Witzke, O.; et al. Cellular Immunity in COVID-19 Convalescents with PCR-Confirmed Infection but with Undetectable SARS-CoV-2-Specific IgG. Emerg. Infect. Dis. 2021, 27, 122–129. [Google Scholar] [CrossRef]
- Thummler, L.; Gackler, A.; Bormann, M.; Ciesek, S.; Widera, M.; Rohn, H.; Fisenkci, N.; Otte, M.; Alt, M.; Dittmer, U.; et al. Cellular and Humoral Immunity against Different SARS-CoV-2 Variants Is Detectable but Reduced in Vaccinated Kidney Transplant Patients. Vaccines 2022, 10, 1348. [Google Scholar] [CrossRef]
- Matusali, G.; Petruccioli, E.; Cimini, E.; Colavita, F.; Bettini, A.; Tartaglia, E.; Sbarra, S.; Meschi, S.; Lapa, D.; Francalancia, M.; et al. Evaluation of Cross-Immunity to the Mpox Virus Due to Historic Smallpox Vaccination. Vaccines 2023, 11, 1541. [Google Scholar] [CrossRef]
- Dubois, M.E.; Slifka, M.K. Retrospective analysis of monkeypox infection. Emerg. Infect. Dis. 2008, 14, 592–599. [Google Scholar] [CrossRef] [PubMed]
- Sejvar, J.J.; Chowdary, Y.; Schomogyi, M.; Stevens, J.; Patel, J.; Karem, K.; Fischer, M.; Kuehnert, M.J.; Zaki, S.R.; Paddock, C.D.; et al. Human monkeypox infection: A family cluster in the midwestern United States. J. Infect. Dis. 2004, 190, 1833–1840. [Google Scholar] [CrossRef] [PubMed]
- Hammarlund, E.; Lewis, M.W.; Carter, S.V.; Amanna, I.; Hansen, S.G.; Strelow, L.I.; Wong, S.W.; Yoshihara, P.; Hanifin, J.M.; Slifka, M.K. Multiple diagnostic techniques identify previously vaccinated individuals with protective immunity against monkeypox. Nat. Med. 2005, 11, 1005–1011. [Google Scholar] [CrossRef] [PubMed]
- Karem, K.L.; Reynolds, M.; Hughes, C.; Braden, Z.; Nigam, P.; Crotty, S.; Glidewell, J.; Ahmed, R.; Amara, R.; Damon, I.K. Monkeypox-induced immunity and failure of childhood smallpox vaccination to provide complete protection. Clin. Vaccine Immunol. 2007, 14, 1318–1327. [Google Scholar] [CrossRef] [PubMed]
- Ligon, B.L. Monkeypox: A review of the history and emergence in the Western hemisphere. Semin. Pediatr. Infect. Dis. 2004, 15, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Ladhani, S.N.; Dowell, A.C.; Jones, S.; Hicks, B.; Rowe, C.; Begum, J.; Wailblinger, D.; Wright, J.; Owens, S.; Pickering, A.; et al. Early evaluation of the safety, reactogenicity, and immune response after a single dose of modified vaccinia Ankara-Bavaria Nordic vaccine against mpox in children: A national outbreak response. Lancet Infect. Dis. 2023, 23, 1042–1050. [Google Scholar] [CrossRef] [PubMed]
- Grifoni, A.; Zhang, Y.; Tarke, A.; Sidney, J.; Rubiro, P.; Reina-Campos, M.; Filaci, G.; Dan, J.M.; Scheuermann, R.H.; Sette, A. Defining antigen targets to dissect vaccinia virus and monkeypox virus-specific T cell responses in humans. Cell Host Microbe 2022, 30, 1662–1670.e4. [Google Scholar] [CrossRef] [PubMed]
- Rai, M.A.; Shi, V.; Kennedy, B.D.; Justement, J.S.; Manning, M.R.; Praiss, L.; Kang, E.J.; Gittens, K.; Kardava, L.; Blazkova, J.; et al. Impact of Monkeypox Virus Infection on Immune Parameters in a Woman with Human Immunodeficiency Virus Receiving Clinically Effective Antiretroviral Therapy. J. Infect. Dis. 2023, 228, 270–275. [Google Scholar] [CrossRef]
- Agrati, C.; Cossarizza, A.; Mazzotta, V.; Grassi, G.; Casetti, R.; De Biasi, S.; Pinnetti, C.; Gili, S.; Mondi, A.; Cristofanelli, F.; et al. Immunological signature in human cases of monkeypox infection in 2022 outbreak: An observational study. Lancet Infect. Dis. 2023, 23, 320–330. [Google Scholar] [CrossRef]
- Panchanathan, V.; Chaudhri, G.; Karupiah, G. Correlates of protective immunity in poxvirus infection: Where does antibody stand? Immunol. Cell Biol. 2008, 86, 80–86. [Google Scholar] [CrossRef] [PubMed]
- Earl, P.L.; Americo, J.L.; Wyatt, L.S.; Eller, L.A.; Montefiori, D.C.; Byrum, R.; Piatak, M.; Lifson, J.D.; Amara, R.R.; Robinson, H.L.; et al. Recombinant modified vaccinia virus Ankara provides durable protection against disease caused by an immunodeficiency virus as well as long-term immunity to an orthopoxvirus in a non-human primate. Virology 2007, 366, 84–97. [Google Scholar] [CrossRef] [PubMed]
- Nigam, P.; Earl, P.L.; Americo, J.L.; Sharma, S.; Wyatt, L.S.; Edghill-Spano, Y.; Chennareddi, L.S.; Silvera, P.; Moss, B.; Robinson, H.L.; et al. DNA/MVA HIV-1/AIDS vaccine elicits long-lived vaccinia virus-specific immunity and confers protection against a lethal monkeypox challenge. Virology 2007, 366, 73–83. [Google Scholar] [CrossRef] [PubMed]
- Sammartino, J.C.; Cassaniti, I.; Ferrari, A.; Piralla, A.; Bergami, F.; Arena, F.A.; Paolucci, S.; Rovida, F.; Lilleri, D.; Percivalle, E.; et al. Characterization of immune response against monkeypox virus in cohorts of infected patients, historic and newly vaccinated subjects. J. Med. Virol. 2023, 95, e28778. [Google Scholar] [CrossRef] [PubMed]
- Moschese, D.; Giacomelli, A.; Mileto, D.; Sacco Mpox Study Group. Ongoing sporadic monkeypox cases: Neutralising antibody detection in asymptomatic individuals. Lancet Microbe 2023, 4, e765. [Google Scholar] [CrossRef] [PubMed]
- Zeggagh, J.; Ferraris, O.; Salmona, M.; Tarantola, A.; Molina, J.M.; Delaugerre, C. Second clinical episode of hMPX virus in a man having sex with men. Lancet 2023, 401, 1610. [Google Scholar] [CrossRef]
- Xu, M.; Liu, C.; Du, Z.; Bai, Y.; Wang, Z.; Gao, C. Real-world effectiveness of monkeypox vaccines: A systematic review. J. Travel Med. 2023, 30, taad048. [Google Scholar] [CrossRef]
- Montero Morales, L.; Barbas Del Buey, J.F.; Alonso Garcia, M.; Cenamor Largo, N.; Nieto Julia, A.; Vazquez Torres, M.C.; Jimenez Bueno, S.; Aragon Pena, A.; Gil Montalban, E.; Inigo Martinez, J.; et al. Post-exposure vaccine effectiveness and contact management in the mpox outbreak, Madrid, Spain, May to August 2022. Eurosurveillance 2023, 28, 2200883. [Google Scholar] [CrossRef]
- Dalton, A.F.; Diallo, A.O.; Chard, A.N.; Moulia, D.L.; Deputy, N.P.; Fothergill, A.; Kracalik, I.; Wegner, C.W.; Markus, T.M.; Pathela, P.; et al. Estimated Effectiveness of JYNNEOS Vaccine in Preventing Mpox: A Multijurisdictional Case-Control Study—United States, 19 August 2022–31 March 2023. MMWR Morb. Mortal. Wkly. Rep. 2023, 72, 553–558. [Google Scholar] [CrossRef]
- Deputy, N.P.; Deckert, J.; Chard, A.N.; Sandberg, N.; Moulia, D.L.; Barkley, E.; Dalton, A.F.; Sweet, C.; Cohn, A.C.; Little, D.R.; et al. Vaccine Effectiveness of JYNNEOS against Mpox Disease in the United States. N. Engl. J. Med. 2023, 388, 2434–2443. [Google Scholar] [CrossRef]
- Weerasinghe, M.N.; Ooi, C.; Kotsiou, G.; Cornelisse, V.J.; Painter, A. Breakthrough mpox despite two-dose vaccination. Med. J. Aust. 2023, 219, 295–296. [Google Scholar] [CrossRef]
- Hazra, A.; Zucker, J.; Bell, E.; Flores, J.; Gordon, L.; Mitja, O.; Suner, C.; Lemaignen, A.; Jamard, S.; Nozza, S.; et al. Mpox in people with past infection or a complete vaccination course: A global case series. Lancet Infect. Dis. 2023, 24, 57–64. [Google Scholar] [CrossRef]
- Payne, A.B.; Ray, L.C.; Kugeler, K.J.; Fothergill, A.; White, E.B.; Canning, M.; Farrar, J.L.; Feldstein, L.R.; Gundlapalli, A.V.; Houck, K.; et al. Incidence of Monkeypox Among Unvaccinated Persons Compared with Persons Receiving ≥ 1 JYNNEOS Vaccine Dose—32 U.S. Jurisdictions, July 31–3 September 2022. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 1278–1282. [Google Scholar] [CrossRef]
- Taha, A.M.; Rodriguez-Morales, A.J.; Sah, R. Mpox breakthrough infections: Concerns and actions. Lancet Infect. Dis. 2023, 23, 1216–1218. [Google Scholar] [CrossRef]
- Jamard, S.; Handala, L.; Faussat, C.; Vincent, N.; Stefic, K.; Gaudy-Graffin, C.; Maakaroun-Vermesse, Z.; Lemaignen, A. Resurgence of symptomatic Mpox among vaccinated patients: First clues from a new-onset local cluster. Infect. Dis. Now. 2023, 53, 104714. [Google Scholar] [CrossRef]
- Mohapatra, R.K.; Mishra, S.; Rabaan, A.A.; Mohanty, A.; Padhi, B.K.; Sah, R. Monkeypox breakthrough infections and side-effects: Clarion call for nex-gen novel vaccine. New Microbes New Infect. 2023, 52, 101084. [Google Scholar] [CrossRef]
- Thy, M.; Peiffer-Smadja, N.; Mailhe, M.; Kramer, L.; Ferre, V.M.; Houhou, N.; Tarhini, H.; Bertin, C.; Beaumont, A.L.; Gare, M.; et al. Breakthrough Infections after Postexposure Vaccination against Mpox. N. Engl. J. Med. 2022, 387, 2477–2479. [Google Scholar] [CrossRef] [PubMed]
- Gigante, C.M.; Korber, B.; Seabolt, M.H.; Wilkins, K.; Davidson, W.; Rao, A.K.; Zhao, H.; Smith, T.G.; Hughes, C.M.; Minhaj, F.; et al. Multiple lineages of monkeypox virus detected in the United States, 2021–2022. Science 2022, 378, 560–565. [Google Scholar] [CrossRef] [PubMed]
- Zaeck, L.M.; Lamers, M.M.; Verstrepen, B.E.; Bestebroer, T.M.; van Royen, M.E.; Gotz, H.; Shamier, M.C.; van Leeuwen, L.P.M.; Schmitz, K.S.; Alblas, K.; et al. Low levels of monkeypox virus-neutralizing antibodies after MVA-BN vaccination in healthy individuals. Nat. Med. 2023, 29, 270–278. [Google Scholar] [CrossRef] [PubMed]
- Koch, T.; Dahlke, C.; Fathi, A.; Kupke, A.; Krahling, V.; Okba, N.M.A.; Halwe, S.; Rohde, C.; Eickmann, M.; Volz, A.; et al. Safety and immunogenicity of a modified vaccinia virus Ankara vector vaccine candidate for Middle East respiratory syndrome: An open-label, phase 1 trial. Lancet Infect. Dis. 2020, 20, 827–838. [Google Scholar] [CrossRef] [PubMed]
- Lindemann, M.; Klisanin, V.; Thummler, L.; Fisenkci, N.; Tsachakis-Muck, N.; Ditschkowski, M.; Schwarzkopf, S.; Klump, H.; Reinhardt, H.C.; Horn, P.A.; et al. Humoral and Cellular Vaccination Responses against SARS-CoV-2 in Hematopoietic Stem Cell Transplant Recipients. Vaccines 2021, 9, 1075. [Google Scholar] [CrossRef] [PubMed]
- CDC. Mpox. Get Both Doses of the Mpox Vaccine. Available online: https://www.cdc.gov/poxvirus/mpox/index.html (accessed on 17 November 2023).
- PAHO. Monkeypox Multi-Country Outbreak Response—Region of the Americas, Report n. 7. Available online: https://www.paho.org/en/file/124030/download?token=E_4G2q8f (accessed on 17 November 2023).
- Scheffer, M.; Paiva, V.S.F.; Barberia, L.G.; Russo, G. Monkeypox in Brazil between stigma, politics, and structural shortcomings: Have we not been here before? Lancet Reg. Health Am. 2023, 17, 100394. [Google Scholar] [CrossRef] [PubMed]
- PAHO. Mpox Cases—Region of the Americas. Available online: https://shiny.pahobra.org/mpox/ (accessed on 17 November 2023).

| Variable 1 | Vaccinated (n = 33) | Infected (n = 10) |
|---|---|---|
| Age (years) | 44 (24–63) | 39 (25–59) |
| Interval second vaccination or infection—testing (days) | 115 (51–247) | 314 (278–366) *** |
| Absolute cell counts (cells/μL) | ||
| CD3+ | 1710 (911–3290) | 1895 (1560–2560) |
| CD4+ | 753 (335–1770) | 950 (659–1490) |
| CD8+ | 821 (351–2150) | 794 (540–1270) |
| Relative cell counts [%] | ||
| CD3+ | 75.8 (41.3–84.2) | 73.1 (59.8–83.0) |
| CD4+ | 34.1 (20.6–59.2) | 34.9 (27.3–53.9) |
| CD8+ | 35.0 (9.3–55.4) | 30.8 (20.7–39.6) |
| CD4/CD8 ratio | 1.0 (0.4–29) | 1.0 (0.7–2.6) |
| Statins (with/without) | 3/30 | 1/9 |
| Immunosuppressive therapy (with/without) | 1/32 | 0/10 |
| ELISpot | Parameter | r | p |
|---|---|---|---|
| IFN-γ (1 μg/mL per peptide) | CD8+ T cells [%] | 0.56 | 0.09 |
| CD4/CD8 ratio | −0.63 | <0.05 * | |
| IFN-γ (2 μg/mL per peptide) | CD8+ T cells [%] | 0.57 | 0.09 |
| CD4/CD8 ratio | −0.57 | 0.08 | |
| IL-2 (1 μg/mL per peptide) | CD8+ T cells [%] | 0.73 | 0.02 * |
| CD4/CD8 ratio | −0.55 | 0.10 | |
| IL-2 (2 μg/mL per peptide) | CD8+ T cells [%] | 0.69 | 0.03 * |
| CD4/CD8 ratio | −0.65 | 0.04 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stefanie, S.; Koldehoff, M.; Schenk-Westkamp, P.; Horn, P.A.; Esser, S.; Lindemann, M. T Cell Responses against Orthopoxviruses in HIV-Positive Patients. Vaccines 2024, 12, 131. https://doi.org/10.3390/vaccines12020131
Stefanie S, Koldehoff M, Schenk-Westkamp P, Horn PA, Esser S, Lindemann M. T Cell Responses against Orthopoxviruses in HIV-Positive Patients. Vaccines. 2024; 12(2):131. https://doi.org/10.3390/vaccines12020131
Chicago/Turabian StyleStefanie, Sammet, Michael Koldehoff, Pia Schenk-Westkamp, Peter A. Horn, Stefan Esser, and Monika Lindemann. 2024. "T Cell Responses against Orthopoxviruses in HIV-Positive Patients" Vaccines 12, no. 2: 131. https://doi.org/10.3390/vaccines12020131
APA StyleStefanie, S., Koldehoff, M., Schenk-Westkamp, P., Horn, P. A., Esser, S., & Lindemann, M. (2024). T Cell Responses against Orthopoxviruses in HIV-Positive Patients. Vaccines, 12(2), 131. https://doi.org/10.3390/vaccines12020131





