Vaccination Communication Strategies and Uptake in Africa: A Systematic Review
Abstract
1. Introduction
2. Methodology
2.1. Eligibility Criteria
2.2. Search Strategy
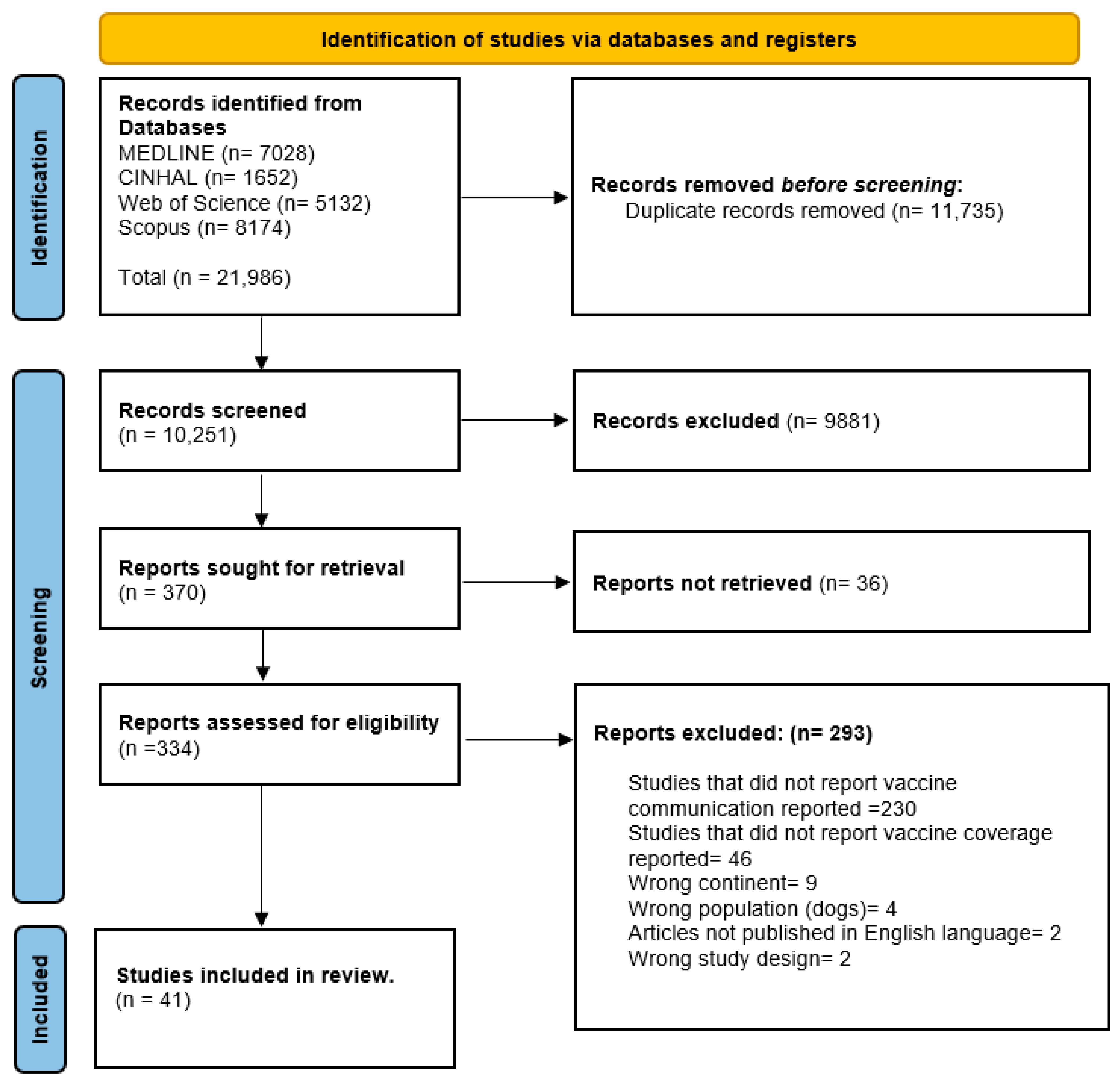
2.3. Study Selection
2.4. Study Appraisal
2.5. Data Extraction
2.6. Analysis and Narrative Synthesis
3. Results
3.1. Results of the Search
3.2. Study Characteristics
| Author | Country of Study | Study Design/ Study Duration | Vaccine Administered | Target Group/ Sample Size | Setting | Vaccination Communication Method | Vaccination Uptake | Quality Assessment |
|---|---|---|---|---|---|---|---|---|
| Abd Elaziz et al. 2010 [40] | Egypt | Quasi-experimental 2 months | Measles and rubella (MR) vaccine | Medical students (n = 341) | School | Campaign using posters | Vaccine uptake: 65% | Strong |
| Addi et al. 2021 [41] | Morocco | Cross-sectional (DNR) | COVID-19 vaccine | General population (n = NR) | Community | Official Ministry of Health website mass media | Vaccine coverage: 8.94% | Weak |
| Admassie et al. 2009 [42] | Ethiopia | Quasi-experimental 4 months | DPT 3-doses Polio 3-doses BCG Measles | Households (n = 3095) | Community | Training of health extension workers House visits | Fully vaccinated with BCG, polio, measles, and DPT vaccines is significantly larger in the treatment villages | Moderate |
| Akande et al. 2005 [43] | Ghana | Cross-sectional 1 month | Polio vaccine | Children aged 0–59 months (n = 3737) | Community | House visits Announcements by radio and gong-gong Mobile van Health worker’s education | Vaccination uptake: 98.8% | Moderate |
| Amani et al. 2023 [44] | Central African Republic | Cross-sectional 5 months | COVID-19 vaccine | General population (n = 5,570,659) | Community | Capacity building and training of CHW Health education by trained CHWs | Vaccination coverage change: 9% to 29% | Moderate |
| Amani et al. 2021 [45] | Cameroon | Cross-sectional (Evaluation) 1 month | Oral cholera vaccine (OCV) | General population (n = 537,274) | Health centre | House visits by social mobilisers Messages circulated through press, radio, sports, television, megaphones, banners, and posters | The overall vaccination coverage was 99.9% | Strong |
| Amare et al. 2021 [46] | Ethiopia | Quasi-experimental 7 months | Penta-3 Polio 3 vaccines | Health workers (n = 90) | Health centre | Capacity building of health workers | 17.4% increase for Penta 3 vaccine in IG over CG | Moderate |
| Andrianarivelo et al. 2001 [47] | Madagascar | Quasi-experiment (DNR) | Oral polio vaccine (OPV) | Children up to 59 months (n = 929) | Community | Mass immunisation campaigns | Vaccination coverage after two mass campaigns:
| Moderate |
| Appiah et al. 2022 [48] | Ethiopia | RCT 3 months | Penta 3 vaccine | Mothers of children (n = 638) | Community | Radio Campaign: IG: 10 + 10 + 30 (10 min radio drama on infant vaccination, 10 min discussion by CHW, 30 min phone-in from listeners) CG: No intervention | CG = 324; IG = 314 Vaccine coverage change IG: 89.8%, 95% CI: 85.9–92.9%) CG: (65.1%, 95% CI: 59.7–70.3%). | Strong |
| Ateudjieu et al. 2022 [37] | Cameroon | Cross-sectional 2 months | Oral cholera vaccine | General population (n = 9212) | Community | Training workshops for healthcare workers | First round = 4372, second round = 4840 Vaccination coverage - First round: 81.0% - Second round: 88.8% (single dose change 4.3%, second dose change 80.1%) | Strong |
| Bangure et al. 2015 [49] | Zimbabwe | RCT 7 months | Childhood immunisation | Women (n= 304) | Health centre | IG: Automated text reminders were sent at 6, 10, and 14 weeks CG: Routine health education | IG = 152, CG = 152 Immunisation coverage - At 6 weeks: IG (97%) vs. CG (82%), (p < 0.001). - At 14 weeks: IG (95%), CG (75%) | Moderate |
| Basheer et al. 2021 [50] | Nigeria | Quasi-experiment 4 months | Childhood immunisation | Mothers of children 12–23 months of age (n = 420) | Community | Training of primary HCWs to improve interpersonal communication skills | IG = 210, C = 210 Routine childhood immunisation uptake (IG vs. CG) - Fully immunised: 53.8% vs. 9.5% - Partially immunised: 16.6% vs. 32.8% - Un-immunised: 29.5% vs. 57.6% p < 0.001. | Moderate |
| Botha et al. 2015 [51] | South Africa | Quasi-experiment (DNR) | HPV vaccine | Girls (n = 2046) | School | Advocacy for school stakeholders and teachers Health education targeted at caregivers and schoolgirls Written information leaflets | - At least one dose of HPV vaccine: 99.2% - Received 3 doses: 87.8% - Sufficient vaccination: 91.6% of the vaccinated cohort | Moderate |
| Brown et al. 2016 [39] | Nigeria | RCT (DNR) | Childhood immunisation | Children aged 0–12 months paired with their mothers (n = 595) | Health centre | Cell phone call reminder Primary healthcare immunization Providers’ training intervention | Immunisation completion: - IG (3 arms): cell phone reminder (98.6%), PHC providers’ training intervention (70%), combined cell phone reminders and training of PHC providers (97.3%) - CG: 57.3% | Moderate |
| Crippin et al. 2022 [52] | Mali | Quasi-experiment 7 months | HPV vaccine | Women (n = 500) | Community and health centre | Community educational sessions by community health workers and a storytelling cloth | Willingness of women to want their children to be vaccinated: 87% | Moderate |
| Dougherty et al. 2020 [29] | Nigeria | Quasi-experiment 12 months | BCG Polio vaccine Hep B vaccine | Children aged 0–23 months and their mothers (n = 2639) | Community | Training of traditional barbers (direct and interpersonal communication) | Received yellow card: IG (16.6%) | Moderate |
| Dreyer et al. 2015 [32] | South Africa | Quasi-experiment (DNR) | HPV vaccine | Primary school girls; parents and female guardians (n = 3465) | School | Health education with presentation and leaflets | Vaccination uptake - First dose: 99.3% - Second-doses: 95.9% (974/1016) - Third-dose: 91.6% (1859/2030). - Overall completion: 90.5% | Moderate |
| Durrheim et al. 2001 [53] | South Africa | Commentary (DNR) | Polio vaccine Measles vaccine | Children (n = NR) | Community | Mass immunisation campaigns | - Decrease in second-round national OPV coverage by: 1995 (11.7%), 1996 (12.8%), 1997 (3.5%) - Polio mass campaign coverage declined by 7.7% between 1995 and 1997 (chi-square for trend = 7465.3, df =1, p < 0.001) - Measles Campaign: 1996 (91.1%) and the 2000 campaign (91.0%) | Weak |
| Egbon et al. 2022 [54] | Nigeria | Cross-sectional 5 months | HPV vaccine | School girls 9–19 years old (n = 100) | School | Community mobilisation and advocacy | Vaccination completion: under-14 years (60%, 42/70), ≥15 years 83% (25/30) | Strong |
| Ekhaguere et al. 2019 [28] | Nigeria | RCT 12 months | Penta 1, 2, 3 vaccine | Mothers of children (n = 600) | Health centre | Automate reminders using phone calls and text messages | IG (n = 300), CG (n = 300) Completion of 12-month immunisation series: IG (74%) vs. CG (66%); (RR: 1.12, 95%CI: 1.01–1.25; p = 0.03) Received Penta-3 within 1 week of the expected date: IG (84%) vs. CG (78%); (RR: 1.09, 95%CI: 1.01–1.17, p = 0.04) Received measles immunisation within 1 week of the expected date: IG (73%) vs. CG (65%); (RR: 1.33, 95%CI: 1.02–1.26, p = 0.02) | Strong |
| Gibson et al. 2017 [31] | Kenya | RCT 12 months | Pentavalent and Measles vaccine | Caregivers of infants aged 0–34 days (n = 2018) | Community | IG1 = SMS only (Financial incentives) IG2 = SMS + 75 KES IG3 = SMS + 200 KES | IG1 (n = 476), IG2 (n = 562), IG3 (n = 491), CG (n = 489) - Full immunisation among children 12 months of age: - IG (3 arms): SMS only (86%), SMS + 75 KES (86%), SMS + 200 KES (90%) - CG: 82% - Coverage at 12 months and timely vaccination: - IG (3 arms): SMS only (48%), SMS + 75 KES (60%), SMS + 200 KES (62%) - CG: 41% | Moderate |
| Jones and Kawesa-Newell, 2021 [55] | Malawi | Quasi-experiment (DNR) | HPV vaccine | School girls (n = NR) | School | Mini magazine | Vaccine uptake change - Cohort 1: 83% vs. 70%, p = 0.0028 - Cohort 2: 82% vs. 62%, p = 0.0002 | Moderate |
| Kaduru et al. 2023 [33] | Nigeria | Quasi-experiment 5 months | Childhood immunisation | Caregivers (women) (n = 216) | Community | Community drama/theatre | Fully immunised: Baseline (46%), midline (55%), post-intervention (84%) | Strong |
| Levine et al. 2021 [56] | Ghana | RCT 5 months | Polio vaccine BCG vaccine | Mothers who delivered a live-born, surviving infant; primary caregivers (n = NR) | Community | IG1 = Voice call reminders IG2 = Community health volunteers and financial incentives (training of community health volunteers) | Vaccination coverage - First dose of Polio and BCG: higher in all arms than during the baseline period - Vaccinated on time with both vaccines: voice call reminder (37.8%), CHV and incentives arms (54.5%) - Increase from pre-intervention to post-intervention: voice call reminder (12.8% points), CHV and incentives arms (42.0% points) | Moderate |
| Meiring et al. 2019 [57] | Malawi | Quasi-experiment 3 months | Typhoid conjugate vaccine | Community members (n = NR) | School | Community mobilisation and advocacy Announcements and jingle for invitation for vaccination with a mobile van | School-based vaccine campaign increased community participation, exceeding recruitment targets (average, >200 children/day) | |
| Mekonnen et al. 2021 [30] | Ethiopia | RCT 12 months | Penta 3 Measles | Mothers and infant (n = 434) | Health centre | IG = Text message reminders CG = Routine verbal reminders | IG = 217, CG = 217 - On-time vaccination: IG (63.3%), CG (39.9%) - Penta 2 coverage: IG (98.1%), CG (95.3%) - Penta 3 coverage: IG (95.8%), CG 185 (86.9%) - Measles vaccine coverage: IG (91.5%), CG (79.3%) | Strong |
| Mohammed et al. 2023 [58] | Ghana | Cross-sectional (DNR) | COVID-19 vaccine | HCWs (n = 424) | Health centre | Media | First dose of COVID-19 vaccine uptake: 73.6% | Moderate |
| Mphuru et al. 2022 [59] | Tanzania | Qualitative 2 months | HPV vaccine | 14-year-old girls (n = 10) | Community and Health centre | Health education in schools Community advocacy and sensitisation Mass media using posters, brochures, fliers, TV, radio, social media | - First dose (HPV1) coverage: 78% - Second dose (HPV2) coverage: 49%. | Strong |
| Msunyaro et al. 2023 [60] | Tanzania | Quasi-experiment 8 months | COVID-19 vaccine | Community members (n = 1,351,320) | Community | Community engagement; house visits, village meetings by community champions | Increase during the campaign: 10% to 22% | Moderate |
| Obi-Jeff et al. 2022 [34] | Nigeria | Qualitative (DNR) | Routine childhood immunisation (BCG, OPV, DPT, Hep B, Measles, Yellow fever vaccines) | Program stakeholders (policymakers, program managers, development partners) and HCW (n = 144) | Community | Automated text messages using immunisation reminders system | Many noted that personalised reminders reminded caregivers, especially those who were busy and forgot their child’s vaccination dates and prompted them to go for vaccination | Moderate |
| Odunyemi et al. 2018 [61] | Nigeria | Quasi-experiment (DNR) | HPV vaccine | Married civil servants’ women (n = 146) | Community | IG = Health education by nurses CG = No intervention | IG = 69, CG = 77 Mothers were ready to accept HPV vaccination for their adolescent daughters - Baseline: IG (73.9%), CG% (83.1%) - 3-months: IG (93.8%), CG% (60.8%) | Strong |
| Oku et al. 2017 [62] | Nigeria | Qualitative 2 months | Childhood immunisation | Caregivers and Healthcare workers (n = 84) | Community | Health workers education Mass media (radio and jingles) Town announcers in church Home visits | All caregivers: -Expressed messages received in the clinic were useful -Received information about managing vaccination side effects | Moderate |
| Ozohu-Suleiman et al. 2010 [63] | Nigeria | Cross-sectional (DNR) | Polio vaccine | Community members, including caregivers (n = 2253) | Community | Mass immunisation campaigns using interpersonal sources | - Immunisation campaign acceptance: 5.1% - Immunisation campaign resistance: 44.9% | Moderate |
| Sato and Takasaki, 2021 [64] | Nigeria | RCT 2 months | Tetanus toxoid vaccine | Pregnant women/women with children (n = 1600) | Community | Graphical illustrations using flipcharts | IG = 782 Decreased vaccine take-up by 3.7–6.1% | Strong |
| Sato and Titus, 2021 [65] | Nigeria | Quasi-experiment 10 months | Childhood immunisation | Women with children (n = 515) | Community | IG = One-time tailored information on their children’s current vaccination status and the next schedule for vaccination CG = Generic information on the vaccination schedule | IG = 198, CG = 317 Immunisation uptake: IG (38.4%), CG (46.6%) | Strong |
| Ugwuoke et al. 2021 [38] | Nigeria | Quasi-experiment (DNR) | COVID-19 vaccine | Victims of conflicts in IDPS (n = 470) | Community | IG = Graphical illustrations using visual illustrations on the importance of COVID-19 vaccination and counselling CG = No intervention | IG = 235, CG = 235 Intention toward COVID-19 vaccination (pre vs. post-test) (mean, SD): IG (1.1, 0.21) vs. (3.8, 0.98), CG (1.2, 0.11 vs. 1.3, vs. 0.23) | Moderate |
| Vermandere et al. 2015 [35] | Kenya | Qualitative 2 months | HPV vaccine | Teachers and parents of girls (n = 7) | School | Training of teachers by HCWs Health education to create awareness for girls and fathers | Teachers = 4, Fathers = 3 Despite high baseline acceptance, reported uptake at follow up was low | Moderate |
| Wamai et al. 2012 [66] | Cameroon | Cross-sectional 2 months | HPV vaccine | Parents of girls aged between 9–13 years old (n = 337) | Community | Sensitisation campaigns conducted through local media using both radio and television | Overall to vaccinate daughters: 49.9% Strong willingness to vaccinate: 27.0% | Strong |
| Warigon et al. 2016 [67] | Nigeria | Quasi-experiment (DNR) | Polio vaccine | Children (n = 5991) | Community | Advocacy for religious leader support Local drama Media, radio, newspapers. and TV | Received vaccination: 85.5% | Moderate |
| Yau et al. 2023 [68] | Nigeria | Quasi-experiment (DNR) | Routine childhood immunisation (BCG, OPV, DPT, Hep B, Measles, Yellow fever) vaccines | Newborns (0–14 days old) and mothers (n = 435) | Health centre | IG = Color-coded bracelets CG = No bracelets, but they received standard information provided at routine immunisation services | IG = 256, CG = 179 Completed their vaccination schedule at the fifth contact: IG (62%), CG (41%), p < 0.0001 | Moderate |
| Yego et al. 2023 [36] | Kenya | RCT (DNR) | COVID-19 vaccine | High-risk patients either due to age (>60 years old) and/or have a documented medical history of hypertension or diabetes (n = 8514) | Health centre | IG1 = Phone call + Gain messages IG2 = Phone call + Loss messages IG3 = Phone call + Social norms messages IG4 = SMS + Gain messages IG5 = SMS + Loss messages IG6 = SMS + Social norms messages CG = No intervention | IG1 = 1216, IG2 = 1216, IG3 = 1216, IG4 = 1216, IG5 = 1216, IG6 = 1217 CG = 1217 1716 (47%) participants in the phone call channel received intervention Vaccination status of those who received the intervention: 83% (1524) - Completed vaccine doses: 89% (1267) - Partially vaccinated: 11% (157) had been | Strong |
3.3. Study Findings
3.3.1. Vaccination Communication Methods
3.3.2. Vaccination Communication Sources and Purposes
3.4. Vaccination Coverage and Uptake
3.5. Barriers and Facilitators to Vaccine Uptake
| Author, Year | Facilitators | Barriers |
|---|---|---|
| Abd Elaziz et al. 2010 [40] | More health education | Insufficient information, fear of getting infection, past infection, unconcerned, afraid of injections, vaccinated in private, fear of side effects, others |
| Addi et al. 2021 [41] | Vaccination campaign is free for all citizens and foreigners | Fake news in social media, low level of education and economic status, and insufficiency in population awareness programs |
| Amani et al. 2023 [44] | Task shifting provided equitable vaccine access | |
| Andrianarivelo et al. 2001 [47] | OPV doses during the mass vaccination campaign improved their immune status | |
| Appiah et al. 2022 [48] | Lack of communication and knowledge about the importance of vaccinations | |
| Ateudjieu et al. 2022 [37] | Absenteeism (49.4%), Lack of awareness (18.2%) | |
| Bangure et al. 2015 [49] | Overall increase likely attributed to use of SMS reminders | |
| Crippin et al. 2022 [52] | Seeking consent from husband or partner first | |
| Dougherty et al. 2020 [29] | Parents trusted traditional barbers; messages shared consistently throughout the community reinforced their beliefs that the advice benefited child health | Low levels of literacy among community leaders and barbers |
| Egbon et al. 2022 [54] | Remote area, hard-to-reach locations, high operational costs, infrastructure health workforce, vaccine delivery included operational costs exacerbated by a lack of adequate health workforce and infrastructure | |
| Ekhaguere et al. 2019 [28] | Long wait times (55%), transportation cost (34%), distance to the clinic (4%), forgetfulness (2.2%), clinic not conducive for mother and child (2%) | |
| Gibson et al. 2017 [31] | SMS reminders plus monetary incentives were modestly effective | |
| Jones and Kawesa-Newell, 2021 [55] | Girls interest in reading the Zathu mini magazine as they were already familiar with the characters and believed the Zathu brand to be trustworthy and reliable | |
| Levine et al. 2021 [56] | - Vaccination provided by a community-level health system infrastructure - Incentives to both CHV and caregivers | Timely vaccination and complete birth registration are not remunerated and formally cadred |
| Mohammed et al. 2023 [58] | COVID-19 vaccine, vaccine-free (82.7%), sufficient efficacy and safety (75.6%), protects against the virus (70.8%), social responsibility (61.9%), benefits outweigh the dangers (72.1%), does not harm people (62.2%), seeing others taking it (62.2%) | Vaccine rapid development and approval (41.0%), immediate side effects (39.2%), unforeseen future effects (37.5%), health workers refusing to take the COVID-19 vaccine (24.5%) |
| Mphuru et al. 2022 [59] | Misinformation, religious radio station airing HPV vaccine causes infertility | |
| Msunyaro et al. 2023 [60] | Vaccine safety concerns Frequent changes in COVID-19 vaccine types confusing | |
| Obi-Jeff et al. 2022 [34] | - Perceived importance in reminding and educating community members on the importance of immunisation - Satisfaction with the message content, especially the health facility day and operation time accuracy | Lack of mobile phones and the inability to read text messages as barriers to intervention participation |
| Odunyemi et al. 2018 [61] | Lack of information deterred vaccinating daughters (85.5%), under age for vaccination, unaware of the venue of vaccination, cost of vaccine | |
| Oku et al. 2017 [62] | - Barriers affecting public: clinic environment, long waiting times, health worker attitudes - Barriers affecting health workers: poor communication skills, poor motivation, and attitudes of community members, including vaccine resistance | |
| Ozohu-Suleiman et al. 2010 [63] | Fears of polio vaccine contamination with anti-fertility hormone and HIV virus aimed at depopulating Muslims around the world | |
| Vermandere et al. 2015 [35] | Protecting girls fertility | Bad experiences or rumours about other vaccines (polio and asthma especially) indicating possible danger of vaccines; new vaccine was potentially hidden experiment; fear vaccine harm girls fertility; fear vaccination will enhance sexual activity among children |
| Wamai et al. 2012 [66] | Knowledge of HPV | Concerns about vaccine effectiveness (31.8%) and side effects/safety (18.4%) |
| Warigon et al. 2016 [67] | Negative campaigns against polio vaccine in the media; negative campaigns initiated by scholars and religious leaders through various media platforms persuading audiences who were largely nonliterate vaccines were contaminated | |
| Yego et al. 2023 [36] | No communication access via phone calls due to incorrect number and change in SIM |
3.6. Vaccine Accessibility and Availability
4. Discussion
4.1. Implication of Findings
4.2. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Fenollar, F.; Mediannikov, O. Emerging infectious diseases in Africa in the 21st century. New Microbes New Infect. 2018, 26, S10–S18. (In English) [Google Scholar] [CrossRef] [PubMed]
- WHO. In Africa, 63% Jump in Diseases Spread from Animals to People Seen in Last Decade. Available online: https://www.afro.who.int/news/africa-63-jump-diseases-spread-animals-people-seen-last-decade#:~:text=There%20has%20been%20a%2063,in%20the%20WHO%20African%20region (accessed on 22 July 2024).
- WHO. Vaccines and Immunization. World Health Organization. Available online: https://www.who.int/health-topics/vaccines-and-immunization#tab=tab_1 (accessed on 22 July 2024).
- WHO. Africa Needs to Vaccinate 33 Million Children to Put Progress Back on Track. Available online: https://www.un.org/africarenewal/magazine/april-2023/africa-needs-vaccinate-33-million-children-put-progress-back-track (accessed on 22 July 2024).
- UNICEF. New UNICEF Report Shows 12.7 Million Children in Africa Missed Out on One or More Vaccinations over Three Years. UNICEF. Available online: https://www.unicef.org/esa/press-releases/new-unicef-report-shows-127-million-children-africa-missed-out-one-or-more (accessed on 22 July 2024).
- Mavundza, E.J.; Cooper, S.; Wiysonge, C.S. A Systematic Review of Factors That Influence Parents’ Views and Practices around Routine Childhood Vaccination in Africa: A Qualitative Evidence Synthesis. Vaccines 2023, 11, 563. [Google Scholar] [CrossRef] [PubMed]
- Oketch, S.Y.; Ochomo, E.O.; Orwa, J.A.; Mayieka, L.M.; Abdullahi, L.H. Communication strategies to improve human papillomavirus (HPV) immunisation uptake among adolescents in sub-Saharan Africa: A systematic review and meta-analysis. BMJ Open 2023, 13, e067164. [Google Scholar] [CrossRef] [PubMed]
- Bradshaw, A.; Mamo, L.T.; Akuagwuagwu, M. Executive Summary. Tony Blair Institute for Global Change. 2022. Available online: https://institute.global/insights/public-services/solve-delivery-challenges-today-futureproof-africas-vaccine-infrastructure (accessed on 18 November 2024).
- Janusz, C.B.; Frye, M.; Mutua, M.K.; Wagner, A.L.; Banerjee, M.; Boulton, M.L. Vaccine Delay and Its Association with Undervaccination in Children in Sub-Saharan Africa. Am. J. Prev. Med. 2021, 60, S53–S64. [Google Scholar] [CrossRef]
- Mbonigaba, E.; Nderu, D.; Chen, S.; Denkinger, C.; Geldsetzer, P.; McMahon, S.; Bärnighausen, T. Childhood vaccine uptake in Africa: Threats, challenges, and opportunities. J. Glob. Health Rep. 2021, 5, e2021080. [Google Scholar] [CrossRef]
- Ackah, B.B.B.; Woo, M.; Stallwood, L.; Fazal, Z.A.; Okpani, A.; Ukah, U.V.; Adu, P.A. COVID-19 vaccine hesitancy in Africa: A scoping review. Glob. Health Res. Policy 2022, 7, 21. [Google Scholar] [CrossRef]
- Razai, M.S.; Oakeshott, P.; Esmail, A.; Wiysonge, C.S.; Viswanath, K.; Mills, M.C. COVID-19 vaccine hesitancy: The five Cs to tackle behavioural and sociodemographic factors. J. R. Soc. Med. 2021, 114, 295–298. [Google Scholar] [CrossRef]
- Miretu, D.G.; Asfaw, Z.A.; Addis, S.G. Impact of COVID-19 pandemic on vaccination coverage among children aged 15 to 23 months at Dessie town, Northeast Ethiopia, 2020. Hum. Vaccines Immunother. 2021, 17, 2427–2436. [Google Scholar] [CrossRef]
- Betsch, C.; Schmid, P.; Heinemeier, D.; Korn, L.; Holtmann, C.; Böhm, R. Beyond confidence: Development of a measure assessing the 5C psychological antecedents of vaccination. PLoS ONE 2018, 13, e0208601. [Google Scholar] [CrossRef]
- Khosa, L.A.; Meyer, J.C.; Motshwane, F.M.M.; Dochez, C.; Burnett, R.J. Vaccine hesitancy drives low human papillomavirus vaccination coverage in girls attending public schools in South Africa. Front. Public Health 2022, 10, 860809. [Google Scholar] [CrossRef]
- Adeyanju, G.C.; Sprengholz, P.; Betsch, C.; Essoh, T.-A. Caregivers’ willingness to vaccinate their children against childhood diseases and human papillomavirus: A cross-sectional study on vaccine hesitancy in Malawi. Vaccines 2021, 9, 1231. [Google Scholar] [CrossRef] [PubMed]
- Adeyanju, G.C.; Betsch, C. Vaccination Decision-Making among Mothers of Children Under-5 in Nigeria: A qualitative study. Hum. Vaccines Immunother. 2024, 20, 2355709. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- O’Leary, S.T.; Opel, D.J.; Cataldi, J.R.; Hackell, J.M. Strategies for improving vaccine communication and uptake. Pediatrics 2024, 153, e2023065483. [Google Scholar] [CrossRef] [PubMed]
- Oku, A.; Oyo-Ita, A.; Glenton, C.; Fretheim, A.; Ames, H.; Muloliwa, A.; Kaufman, J.; Hill, S.; Cliff, J.; Cartier, Y.; et al. Communication strategies to promote the uptake of childhood vaccination in Nigeria: A systematic map. Glob. Health Action 2016, 9, 30337. [Google Scholar] [CrossRef]
- GAVI. Cameroon Increases Reach to Zero-Dose Children Through Microplanning and Communication. Available online: https://zdlh.gavi.org/sites/default/files/2023-09/Cameroon%20Increases%20Reach%20to%20Zero-Dose%20Children%20through%20Microplanning%20and%20Communication.pdf (accessed on 30 July 2024).
- Chandeying, N.; Thongseiratch, T. Clinician Communication Training to Increase Human Papillomavirus Vaccination Uptake: A Systematic Review and Meta-Analysis. Vaccines 2024, 12, 611. [Google Scholar] [CrossRef]
- Ekezie, W.; Bosah, G. Vaccination Communication Strategies and Uptake in Africa: A Systematic Review. PROSPERO 2020 CRD42020196073. Available online: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020196073 (accessed on 30 July 2024).
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- JBI. Critical Appraisal Tools. Available online: https://jbi.global/critical-appraisal-tools (accessed on 30 July 2024).
- Campbell, M.; McKenzie, J.E.; Sowden, A.; Katikireddi, S.V.; Brennan, S.E.; Ellis, S.; Hartmann-Boyce, J.; Ryan, R.; Shepperd, S.; Thomas, J. Synthesis without meta-analysis (SWiM) in systematic reviews: Reporting guideline. BMJ 2020, 368, l6890. [Google Scholar] [CrossRef]
- Ekhaguere, O.A.; Oluwafemi, R.O.; Badejoko, B.; Oyeneyin, L.O.; Butali, A.; Lowenthal, E.D.; Steenhoff, A.P. Automated phone call and text reminders for childhood immunisations (PRIMM): A randomised controlled trial in Nigeria. BMJ Glob. Health 2019, 4, e001232. [Google Scholar] [CrossRef]
- Dougherty, L.; Abdulkarim, M.; Ahmed, A.; Cherima, Y.; Ladan, A.; Abdu, S.; Kilgori, B.; Olayinka, F.; Garr, S.; Gilroy, K.E. Engaging traditional barbers to identify and refer newborns for routine immunization services in Sokoto, Nigeria: A mixed methods evaluation. Int. J. Public Health 2020, 65, 1785–1795. [Google Scholar] [CrossRef] [PubMed]
- Mekonnen, Z.A.; Gelaye, K.A.; Were, M.; Tilahun, B. Effect of Mobile Phone Text Message Reminders on the Completion and Timely Receipt of Routine Childhood Vaccinations: Superiority Randomized Controlled Trial in Northwest Ethiopia. JMIR Mhealth Uhealth 2021, 9, e27603. [Google Scholar] [CrossRef] [PubMed]
- Gibson, D.G.; Ochieng, B.; Kagucia, E.W.; Were, J.; Hayford, K.; Moulton, L.H.; Levine, O.S.; Odhiambo, F.; O’Brien, K.L.; Feikin, D.R. Mobile phone-delivered reminders and incentives to improve childhood immunisation coverage and timeliness in Kenya (M-SIMU): A cluster randomised controlled trial. Lancet Glob. Health 2017, 5, e428–e438. [Google Scholar] [CrossRef] [PubMed]
- Dreyer, G.; Botha, M.H.; Snyman, L.C.; Visser, C.; Burden, R.; Laubscher, N.; Grond, B.; Richter, K.; Becker, P.J.; Harvey, J.; et al. Combining cervical cancer screening for mothers with schoolgirl vaccination during human papillomavirus (HPV) vaccine implementation in South Africa: Results from the VACCS1 and VACCS2 trials. Int. J. Gynecol. Cancer 2022, 32, 592–598. [Google Scholar] [CrossRef]
- Kaduru, C.C.; Mbagwu, G.C.; Aadum, D.K.; Eshikhena, G.; Idim, G.A.; Ibe, U.F.; Sabenus, T.; Jenson, F.G.; Egbe, E.; Aworabhi-Oki, N.; et al. Using community theater to improve demand for vaccination services in the Niger Delta Region of Nigeria. BMC Proc. 2023, 17 (Suppl. 7), 6. [Google Scholar] [CrossRef]
- Obi-Jeff, C.; Garcia, C.; Adewumi, F.; Bamiduro, T.; David, W.; Labrique, A.; Wonodi, C. Implementing SMS reminders for routine immunization in Northern Nigeria: A qualitative evaluation using the RE-AIM framework. BMC Public Health 2022, 22, 2370. [Google Scholar] [CrossRef]
- Vermandere, H.; Naanyu, V.; Degomme, O.; Michielsen, K. Implementation of an HPV vaccination program in Eldoret, Kenya: Results from a qualitative assessment by key stakeholders. BMC Public Health 2015, 15, 875. [Google Scholar] [CrossRef]
- Yego, J.; Korom, R.; Eriksson, E.; Njavika, S.; Sane, O.; Kanorio, P.; Rotich, O.; Wambui, S.; Mureithi, E. A Comparison of Strategies to Improve Uptake of COVID-19 Vaccine among High-Risk Adults in Nairobi, Kenya in 2022. Vaccines 2023, 11, 209. [Google Scholar] [CrossRef]
- Ateudjieu, J.; Yakum, M.N.; Goura, A.P.; Tembei Ayok, M.; Guenou, E.; Kangmo Sielinou, C.B.; Kiadjieu, F.F.; Tsafack, M.; Douanla Koutio, I.M.; Tchio-Nighie, K.H.; et al. An innovative approach in monitoring oral cholera vaccination campaign: Integration of a between-round survey. BMC Public Health 2022, 22, 238. [Google Scholar] [CrossRef]
- Ugwuoke, J.C.; Talabi, F.O.; Adelabu, O.; Sanusi, B.O.; Gever, V.C.; Onuora, C. Expanding the boundaries of vaccine discourse: Impact of visual illustrations communication intervention on intention towards COVID-19 vaccination among victims of insecurity in Nigeria. Hum. Vaccines Immunother. 2021, 17, 3450–3456. [Google Scholar] [CrossRef]
- Brown, V.B.; Oluwatosin, O.A.; Akinyemi, J.O.; Adeyemo, A.A. Effects of Community Health Nurse-Led Intervention on Childhood Routine Immunization Completion in Primary Health Care Centers in Ibadan, Nigeria. J. Community Health 2016, 41, 265–273. [Google Scholar] [CrossRef] [PubMed]
- Abd Elaziz, K.M.; Sabbour, S.M.; Dewedar, S.A. A measles and rubella (MR) catch-up vaccination campaign in an Egyptian University: Vaccine uptake and knowledge and attitudes of students. Vaccine 2010, 28, 7563–7568. [Google Scholar] [CrossRef] [PubMed]
- Addi, R.A.; Benksim, A.; Cherkaoui, M. The vaccination against COVID-19 in Morocco: A success story in progress. Signa Vitae 2021, 17, 250–255. [Google Scholar] [CrossRef]
- Admassie, A.; Abebaw, D.; Woldemichael, A.D. Impact evaluation of the Ethiopian Health Services Extension Programme. J. Dev. Eff. 2009, 1, 430–449. [Google Scholar] [CrossRef]
- Akande, T.M.; Eshetu, M.; Bonsu, G. Rapid assessment as an evaluation tool for polio national immunisation days in Brong Ahafo region, Ghana. Ann. Afr. Med. 2005, 4, 172–176. [Google Scholar]
- Amani, A.; Atuhebwe, P.; Mboussou, F.F.; Ngoy, N.; M’Boufoungou, N.E.; Osei-Sarpong, F.; Traore, C.; Mihigo, R.; Chaiban, T. A rapid increase in coverage of COVID-19 vaccination, Central African Republic. Bull. World Health Organ. 2023, 101, 431–436. [Google Scholar] [CrossRef]
- Amani, A.; Tatang, C.A.; Bayiha, C.N.; Woung, M.; Ngo Bama, S.; Nangmo, A.; Mbang, M.A.; Epee Douba, E. A reactive vaccination campaign with single dose oral cholera vaccine (OCV) during a cholera outbreak in Cameroon. Vaccine 2021, 39, 1290–1296. [Google Scholar] [CrossRef]
- Amare, A.T.; Toni, A.T.; Mekonnen, Z.A.; Endehabtu, B.F.; Tilahun, B.C. Effectiveness and Feasibility of Using Local Medical Universities for Capacity Building to Improve the Immunization Program in Ethiopia: Quasi-Experimental Study. J. Multidiscip. Healthc. 2021, 14, 9–19. [Google Scholar] [CrossRef]
- Andrianarivelo, M.R.; Boisier, P.; Rabarijaona, L.; Ratsitorahina, M.; Migliani, R.; Zeller, H. Mass vaccination campaigns to eradicate poliomyelitis in Madagascar: Oral poliovirus vaccine increased immunity of children who missed routine programme. Trop. Med. Int. Health 2001, 6, 1032–1039. [Google Scholar] [CrossRef]
- Appiah, B.; Gebretsadik, L.A.; Mamo, A.; Kmush, B.; Asefa, Y.; France, C.R.; Samman, E.; Alemayehu, T.; Abafogi, M.; Ahmed, M.K.; et al. A 10+10+30 radio campaign is associated with increased infant vaccination and decreased morbidity in Jimma Zone, Ethiopia: A prospective, quasi-experimental trial. PLOS Glob. Public Health 2022, 2, e0001002. [Google Scholar] [CrossRef]
- Bangure, D.; Chirundu, D.; Gombe, N.; Marufu, T.; Mandozana, G.; Tshimanga, M.; Takundwa, L. Effectiveness of short message services reminder on childhood immunization programme in Kadoma, Zimbabwe—A randomized controlled trial, 2013. BMC Public Health 2015, 15, 137. [Google Scholar] [CrossRef] [PubMed]
- Basheer, A.S.; Kumar, R.; Viwattanakulvanid, P.; Yaha, M.S.; Somrongthong, R. Effect of interpersonal communication training program on child’s immunization among mothers living in Kebbi state of Nigeria. JAMC 2021, 33, 139–144. [Google Scholar] [PubMed]
- Botha, M.H.; van der Merwe, F.H.; Snyman, L.C.; Dreyer, G. The vaccine and cervical cancer screen (VACCS) project: Acceptance of human papillomavirus vaccination in a school-based programme in two provinces of South Africa. S. Afr. Med. J. 2015, 105, 40–43. [Google Scholar] [CrossRef] [PubMed]
- Crippin, T.; Tounkara, K.; Squibb, E.; Beseme, S.; Barry, K.; Sangare, K.; Coulibaly, S.; Fane, P.; Bagayoko, A.; Koita, O.A.; et al. A story-telling cloth approach to motivating cervical cancer screening in Mali. Front. Public Health 2022, 10, 1051536. [Google Scholar] [CrossRef] [PubMed]
- Durrheim, D.N.; Ogunbanjo, G.A.; Webb, E.; Lee, C.K. Mass Immunisation Campaigns in South Africa- The case for judicious timing and spacing. SAMJ 2001, 91, 829–830. [Google Scholar]
- Egbon, M.; Ojo, T.; Aliyu, A.; Bagudu, Z.S. Challenges and lessons from a school-based human papillomavirus (HPV) vaccination program for adolescent girls in a rural Nigerian community. BMC Public Health 2022, 22, 1611. [Google Scholar] [CrossRef]
- Jones, A.; Kawesa-Newell, N. Using branded behaviour change communication to create demand for the HPV vaccine among girls in Malawi: An evaluation of Girl Effect’s Zathu mini magazine. Vaccine 2022, 40 (Suppl. 1), A107–A115. [Google Scholar] [CrossRef]
- Levine, G.; Salifu, A.; Mohammed, I.; Fink, G. Mobile nudges and financial incentives to improve coverage of timely neonatal vaccination in rural areas (GEVaP trial): A 3-armed cluster randomized controlled trial in Northern Ghana. PLoS ONE 2021, 16, e0247485. [Google Scholar] [CrossRef]
- Meiring, J.E.; Sambakunsi, R.; Moyo, E.; Misiri, T.; Mwakiseghile, F.; Patel, P.; Patel, P.; Ndaferankhande, J.; Laurens, M.; Gooding, K.; et al. Community Engagement Before Initiation of Typhoid Conjugate Vaccine Trial in Schools in Two Urban Townships in Blantyre, Malawi: Experience and Lessons. Clin. Infect. Dis. 2019, 68, S146–S153. [Google Scholar] [CrossRef]
- Mohammed, A.S.; Asumah, M.N.; Padhi, B.K.; Sinha, A.; Mohammed, I.; Jamil, S.; Boasiako, O.A.; Leman, N.; Kabir, R. Predictors of SARS-CoV-2 Vaccine Uptake among Health Professionals: A Cross-Sectional Study in Ghana. Vaccines 2023, 11, 190. [Google Scholar] [CrossRef]
- Mphuru, A.; Li, A.J.; Kyesi, F.; Mwengee, W.; Mazige, F.; Nshunju, R.; Shayo, B.; Giattas, M.R.; Loharikar, A.; Lyimo, D. National introduction of human papillomavirus (HPV) vaccine in Tanzania: Programmatic decision-making and implementation. Vaccine 2022, 40 (Suppl. 1), A2–A9. [Google Scholar] [CrossRef] [PubMed]
- Msunyaro, E.; Rangi, J.; Haonga, T.; Kileo, N.; Mlembwa, J.; Nyawade, S.; Machekanyanga, Z.; Kalinga, A.; John, W.; Bukuku, M.A.; et al. Contribution of community champions to accelerate the uptake of COVID-19 vaccination in Rukwa region, Tanzania, February—October 2022. Pan Afr. Med. J. 2023, 45 (Suppl. 1), 5. [Google Scholar] [CrossRef] [PubMed]
- Odunyemi, F.T.; Ndikom, C.M.; Oluwatosin, O.A. Effect of Nursing Intervention on Mothers’ Knowledge of Cervical Cancer and Acceptance of Human Papillomavirus Vaccination for their Adolescent Daughters in Abuja— - Nigeria. Asia Pac. J. Oncol. Nurs. 2018, 5, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Oku, A.; Oyo-Ita, A.; Glenton, C.; Fretheim, A.; Ames, H.; Muloliwa, A.; Kaufman, J.; Hill, S.; Cliff, J.; Cartier, Y.; et al. Perceptions and experiences of childhood vaccination communication strategies among caregivers and health workers in Nigeria: A qualitative study. PLoS ONE 2017, 12, e0186733. [Google Scholar] [CrossRef]
- Ozohu-Suleiman, Y. Media and interpersonal persuasions in the polio eradication campaign in northern Nigeria. J. Public Health Afr. 2010, 1, e2. [Google Scholar] [CrossRef]
- Sato, R.; Takasaki, Y. Backfire effect of salient information on vaccine take-up experimental evidence from scared-straight intervention in rural northern Nigeria. Hum. Vaccines Immunother. 2021, 17, 1703–1713. [Google Scholar] [CrossRef]
- Sato, R.; Titus, T. Effect of tailored information of vaccination schedule on vaccine uptake in northern Nigeria. Hum. Vaccines Immunother. 2021, 17, 3818–3822. [Google Scholar] [CrossRef]
- Wamai, R.G.; Ayissi, C.A.; Oduwo, G.O.; Perlman, S.; Welty, E.; Manga, S.; Ogembo, J.G. Assessing the effectiveness of a community-based sensitization strategy in creating awareness about HPV, cervical cancer and HPV vaccine among parents in North West Cameroon. J. Community Health 2012, 37, 917–926. [Google Scholar] [CrossRef]
- Warigon, C.; Mkanda, P.; Banda, R.; Zakari, F.; Damisa, E.; Idowu, A.; Bawa, S.; Gali, E.; Tegegne, S.G.; Hammanyero, K.; et al. The Journalists Initiatives on Immunisation Against Polio and Improved Acceptance of the Polio Vaccine in Northern Nigeria 2007–2015. J. Infect. Dis. 2016, 213 (Suppl. 3), S86–S90. [Google Scholar] [CrossRef]
- Yau, I.B.; Zubair Mustapha, M.; Nwaze, E.; Nobila, O.; Maigoro, A.; Abdullah, A.; Gamawa, A.; Meissner, P.; Albrecht, J.; Muller, O. Improving the timeliness and completeness of childhood vaccination through color-coded bracelets: A pilot study among Fulani tribe populations in Nigeria. J. Public Health Afr. 2023, 14, 2079. [Google Scholar] [CrossRef]
- Zammit, N.; Gueder, A.E.; Brahem, A.; Ayouni, I.; Ghammam, R.; Fredj, S.B.; Sridi, C.; Chouchene, A.; Kalboussi, H.; Maalel, O.E.; et al. Studying SARS-CoV-2 vaccine hesitancy among health professionals in Tunisia. BMC Health Serv. Res. 2022, 22, 489. [Google Scholar] [CrossRef] [PubMed]
- Lubanga, A.F.; Bwanali, A.N.; Kangoma, M.; Matola, Y.; Moyo, C.; Kaonga, B.; Ssebibubbu, S.; Makole, T.J.; Kambili, F.; Chumbi, G.D. Addressing the re-emergence and resurgence of vaccine-preventable diseases in Africa: A health equity perspective. Hum. Vaccines Immunother. 2024, 20, 2375081. [Google Scholar] [CrossRef] [PubMed]
- Ekezie, W.; Awwad, S.; Krauchenberg, A.; Karara, N.; Dembiński, Ł.; Grossman, Z.; Del Torso, S.; Dornbusch, H.J.; Neves, A.; Copley, S. Access to vaccination among disadvantaged, isolated and difficult-to-reach communities in the WHO European region: A systematic review. Vaccines 2022, 10, 1038. [Google Scholar] [CrossRef] [PubMed]
- Ekezie, W.; Bosah, G. Demographic representation of COVID-19 social media and information engagement in Nigeria. Popul. Med. 2021, 3, 18. [Google Scholar] [CrossRef]
- Hoy; Alexander, C.; Kanagavel, R.; Cameron; Morales, C. Intra-Household Dynamics and Attitudes Toward Vaccines: Experimental and Survey Evidence from Zambia. Policy Research Working Paper; no. WPS 10136; COVID-19 (Coronavirus); Impact Evaluation Series Washington, D.C.: World Bank Group. Available online: http://documents.worldbank.org/curated/en/099239408032215339/IDU00eb25fa7060d9046af09f400895c23d855f9 (accessed on 18 November 2024).
- West, R.L.; Hurst, N.; Sharma, S.; Henry, B.; Vitale-Rogers, S.; Mutahi, W.; Salt, F.; Gardner, C.; Turley, G.; Ezeanochie, N. Communication strategies to promote vaccination behaviours in sub-Saharan Africa. BMC Glob. Public Health 2023, 1, 10. [Google Scholar] [CrossRef]
- ECDC. Effective Communication Around the Benefit and Risk Balance of Vaccination in the EU/EEA; European Centre for Disease Prevention and Control: Stockholm, Sweden, 2024; Available online: https://www.ecdc.europa.eu/en/publications-data/effective-communication-around-benefit-and-risk-balance-vaccination-eueea (accessed on 22 May 2024).
- Udochi-Nwachukwu, A.P.; Dada, S.O.; Nyashanu, M. The Use of Indigenous Communication Media for Children’s Vaccination and Immunization Promotion in Rural Communities of Abia State, Nigeria. J. Public Health Prim. Care 2023, 4, 162–167. [Google Scholar] [CrossRef]
- Odone, A.; Ferrari, A.; Spagnoli, F.; Visciarelli, S.; Shefer, A.; Pasquarella, C.; Signorelli, C. Effectiveness of interventions that apply new media to improve vaccine uptake and vaccine coverage: A systematic review. Hum. Vaccines Immunother. 2015, 11, 72–82. [Google Scholar] [CrossRef]
- Szilagyi, P.; Vann, J.; Bordley, C.; Chelminski, A.; Kraus, R.; Margolis, P.; Rodewald, L. Interventions aimed at improving immunization rates. Cochrane Database Syst. Rev. 2002, 4, CD003941. [Google Scholar]
- Frascella, B.; Oradini-Alacreu, A.; Balzarini, F.; Signorelli, C.; Lopalco, P.L.; Odone, A. Effectiveness of email-based reminders to increase vaccine uptake: A systematic review. Vaccine 2020, 38, 433–443. [Google Scholar] [CrossRef]
- Louw, G.E.; Hohlfeld, A.S.-J.; Kalan, R.; Engel, M.E. Mobile Phone Text Message Reminders to Improve Vaccination Uptake: A Systematic Review and Meta-Analysis. Vaccines 2024, 12, 1151. [Google Scholar] [CrossRef]
- Reñosa, M.D.C.; Landicho, J.; Wachinger, J.; Dalglish, S.L.; Bärnighausen, K.; Bärnighausen, T.; McMahon, S.A. Nudging toward vaccination: A systematic review. BMJ Glob. Health 2021, 6, e006237. [Google Scholar] [CrossRef] [PubMed]
- Asgedom, Y.S.; Kebede, T.M.; Seifu, B.L.; Mare, K.U.; Asmare, Z.A.; Asebe, H.A.; Kase, B.F.; Shibeshi, A.H.; Tebeje, T.M.; Sabo, K.G. Human papillomavirus vaccination uptake and determinant factors among adolescent schoolgirls in sub-Saharan Africa: A systematic review and meta-analysis. Hum. Vaccines Immunother. 2024, 20, 2326295. [Google Scholar] [CrossRef] [PubMed]
- Kabakama, S.; Gallagher, K.E.; Howard, N.; Mounier-Jack, S.; Burchett, H.E.D.; Griffiths, U.K.; Feletto, M.; LaMontagne, D.S.; Watson-Jones, D. Social mobilisation, consent and acceptability: A review of human papillomavirus vaccination procedures in low and middle-income countries. BMC Public Health 2016, 16, 834. [Google Scholar] [CrossRef] [PubMed]
- WHO. Principles and Considerations for Adding a Vaccine to a National Immunization Programme: From Decision to Implementation and Monitoring; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- EU. Ten Actions Towards Vaccination for All; Eurpoean Union World Health Orgaization: Geneva, Switzerland, 2019. [Google Scholar]
- Godongwana, M.; Myburgh, N.; Adedini, S.A.; Cutland, C.; Radebe, N. Knowledge and attitudes towards maternal immunization: Perspectives from pregnant and non-pregnant mothers, their partners, mothers, healthcare providers, community and leaders in a selected urban setting in South Africa. Heliyon 2021, 7, e05926. [Google Scholar] [CrossRef]
- Oyo-Ita, A.; Wiysonge, C.S.; Oringanje, C.; Nwachukwu, C.E.; Oduwole, O.; Meremikwu, M.M. Interventions for improving coverage of childhood immunisation in low- and middle-income countries. Cochrane Database Syst. Rev. 2016, 7, Cd008145. [Google Scholar] [CrossRef]
- Moran, K.R.; Del Valle, S.Y. A meta-analysis of the association between gender and protective behaviors in response to respiratory epidemics and pandemics. PLoS ONE 2016, 11, e0164541. [Google Scholar] [CrossRef]
- Cooper, S.; Schmidt, B.-M.; Sambala, E.Z.; Swartz, A.; Colvin, C.J.; Leon, N.; Wiysonge, C.S. Factors that influence parents’ and informal caregivers’ views and practices regarding routine childhood vaccination: A qualitative evidence synthesis. Cochrane Database Syst. Rev. 2021, 10, CD013265. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ekezie, W.; Igein, B.; Varughese, J.; Butt, A.; Ukoha-Kalu, B.O.; Ikhile, I.; Bosah, G. Vaccination Communication Strategies and Uptake in Africa: A Systematic Review. Vaccines 2024, 12, 1333. https://doi.org/10.3390/vaccines12121333
Ekezie W, Igein B, Varughese J, Butt A, Ukoha-Kalu BO, Ikhile I, Bosah G. Vaccination Communication Strategies and Uptake in Africa: A Systematic Review. Vaccines. 2024; 12(12):1333. https://doi.org/10.3390/vaccines12121333
Chicago/Turabian StyleEkezie, Winifred, Beauty Igein, Jomon Varughese, Ayesha Butt, Blessing Onyinye Ukoha-Kalu, Ifunanya Ikhile, and Genevieve Bosah. 2024. "Vaccination Communication Strategies and Uptake in Africa: A Systematic Review" Vaccines 12, no. 12: 1333. https://doi.org/10.3390/vaccines12121333
APA StyleEkezie, W., Igein, B., Varughese, J., Butt, A., Ukoha-Kalu, B. O., Ikhile, I., & Bosah, G. (2024). Vaccination Communication Strategies and Uptake in Africa: A Systematic Review. Vaccines, 12(12), 1333. https://doi.org/10.3390/vaccines12121333







