Bridging the Vaccination Equity Gap: A Community-Driven Approach to Reduce Vaccine Inequities in Polio High-Risk Areas of Pakistan
Abstract
1. Introduction
2. Methods
2.1. Data Source
2.2. Outcome Indicators
2.3. Ethics Statement
2.4. Statistical Analysis
3. Results
3.1. Overall Equity by Wealth Quintiles
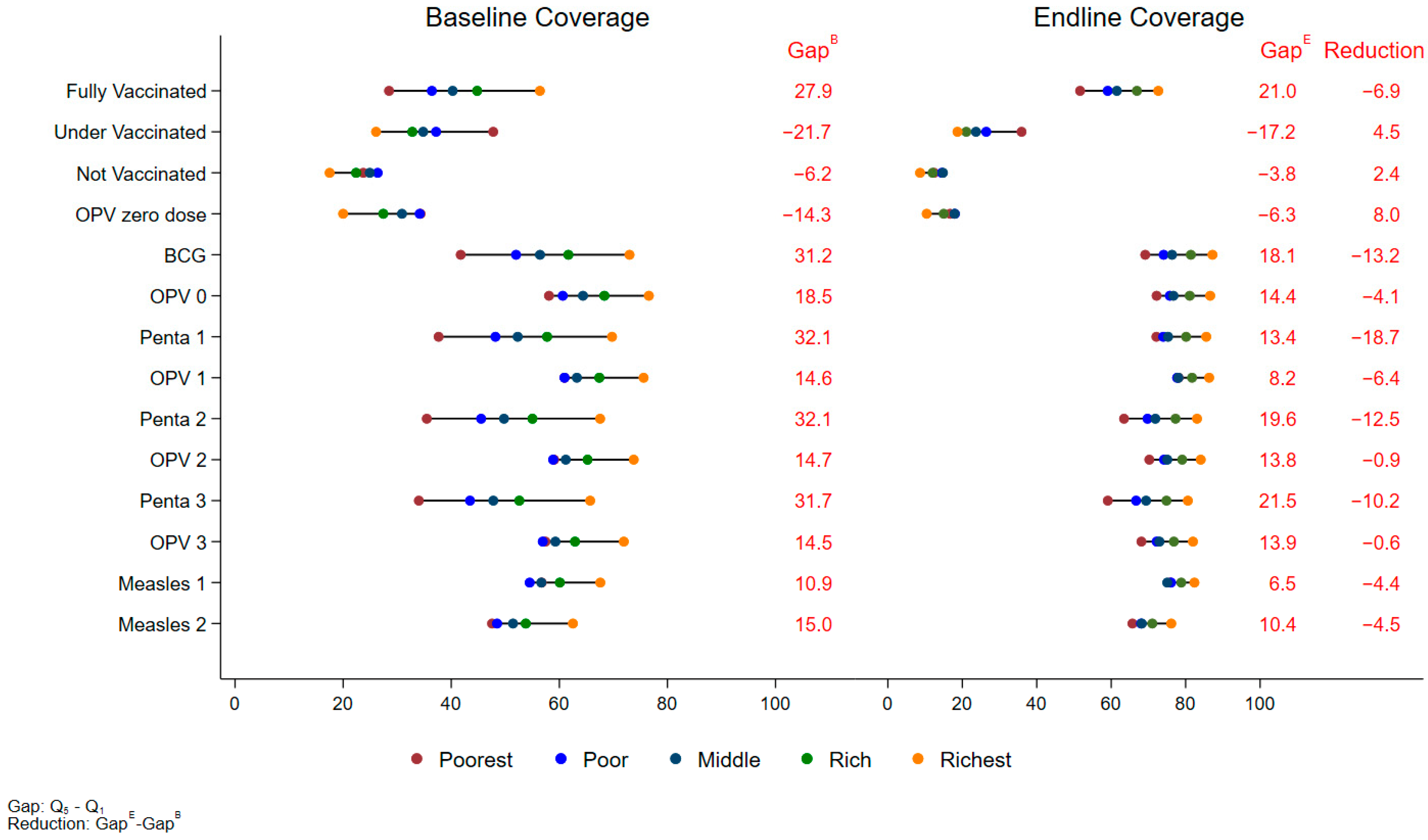
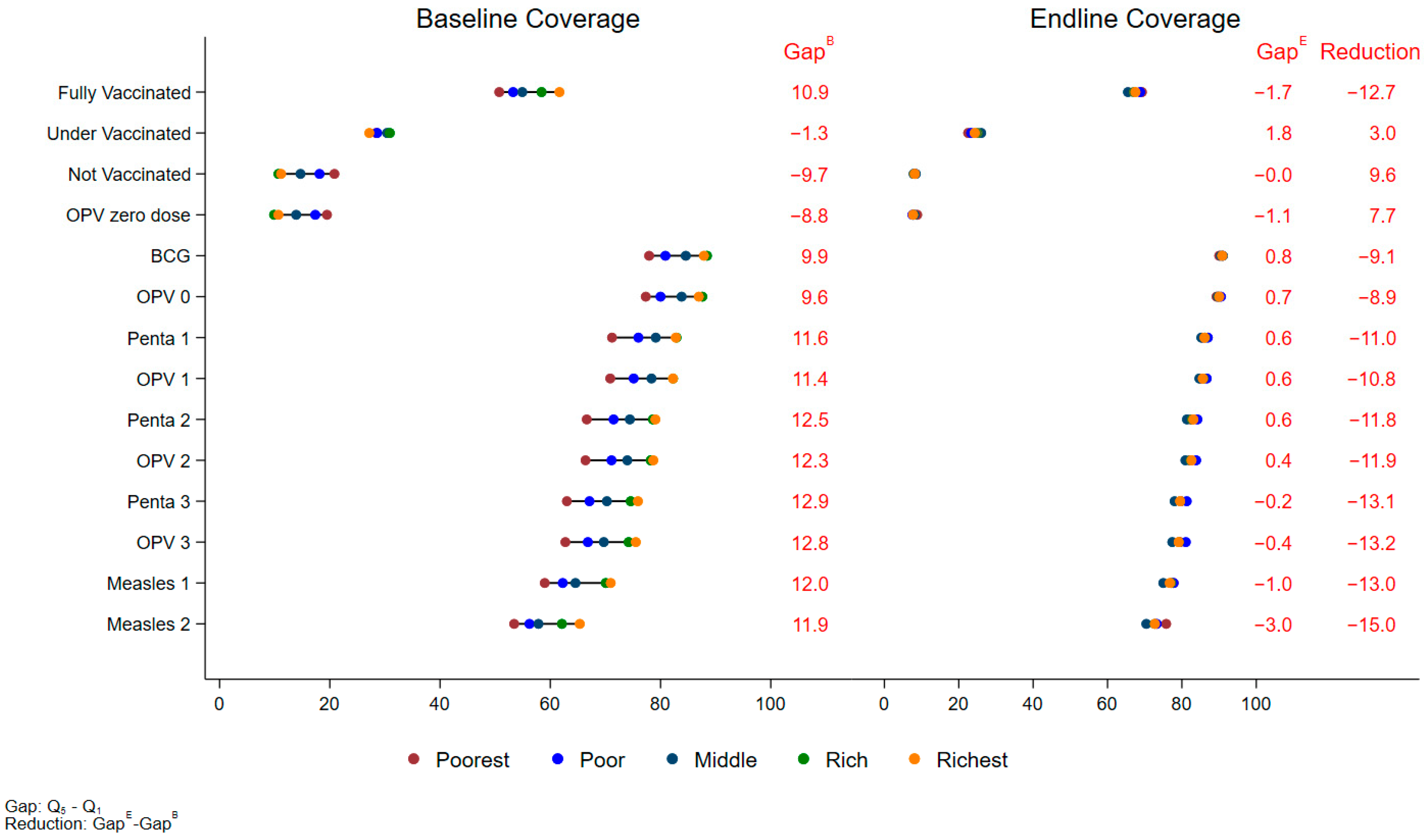
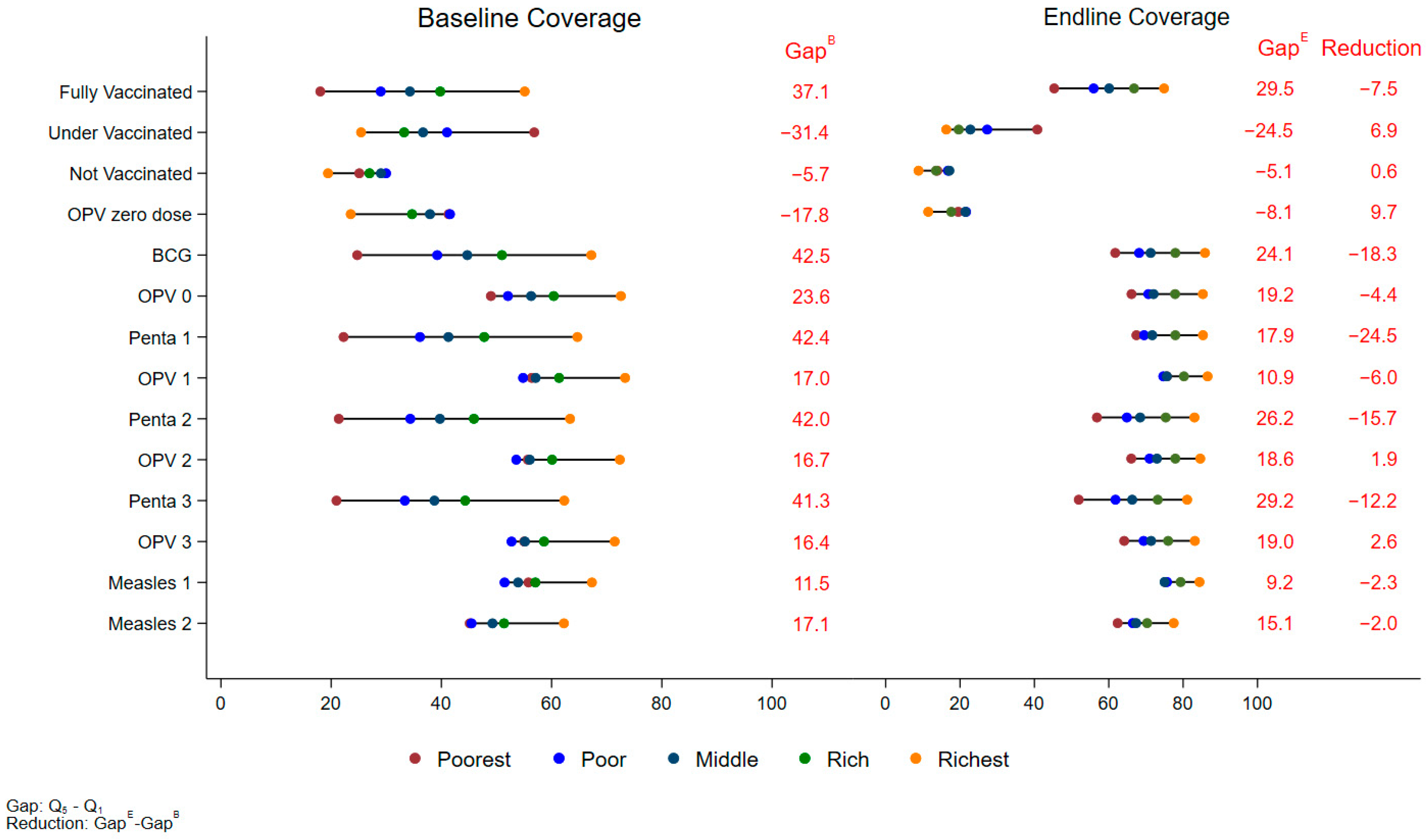
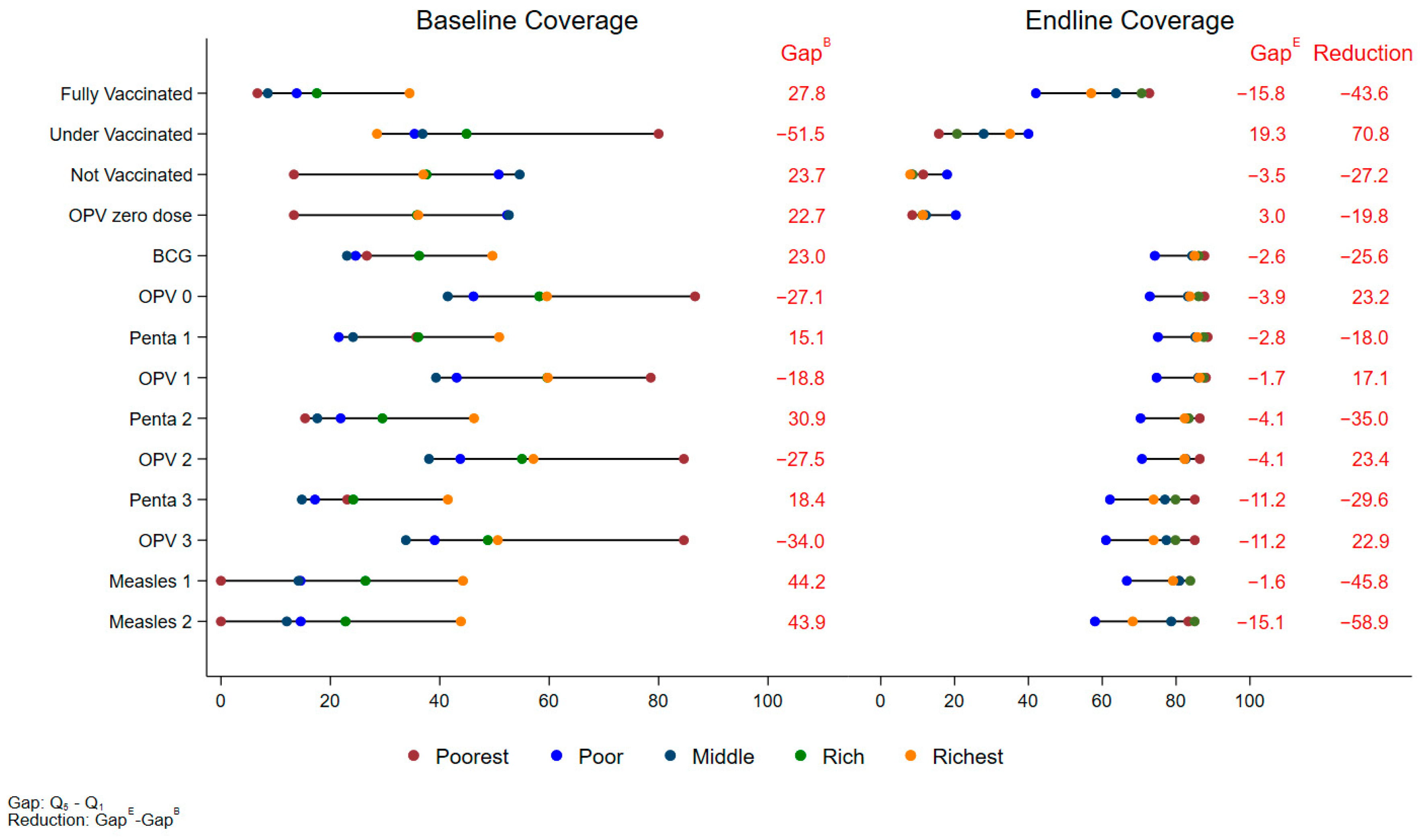
3.2. Regional Equity by Wealth Quintiles
3.3. Prevalence of Fully Vaccinated Children Across Equity Parameters
3.4. Prevalence of Under-Vaccinated Children Across Equity Parameters
3.5. Prevalence of Unvaccinated Children Across Equity Parameters
3.6. Prevalence of Zero-Dose Children Across Equity Parameters
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Vaccines and Immunization. Available online: https://www.who.int/health-topics/vaccines-and-immunization#tab=tab_1 (accessed on 8 October 2024).
- Shattock, A.J.; Johnson, H.C.; Sim, S.Y.; Carter, A.; Lambach, P.; Hutubessy, R.C.; Thompson, K.M.; Badizadegan, K.; Lambert, B.; Ferrari, M.J.; et al. Contribution of vaccination to improved survival and health: Modelling 50 years of the Expanded Programme on Immunization. Lancet 2024, 403, 2307–2316. [Google Scholar] [CrossRef]
- UNICEF. WUENIC Pakistan 2023. 2024. Available online: https://www.unicef.org/pakistan/media/6001/file/WUENIC%20Pakistan%202023.pdf.pdf (accessed on 8 October 2024).
- Global Dashboard for Vaccine Equity Data Futures Exchange. Available online: https://data.undp.org/insights/vaccine-equity (accessed on 21 November 2024).
- World Health Organization. Immunization Coverage. Available online: https://www.who.int/news-room/fact-sheets/detail/immunization-coverage (accessed on 4 October 2024).
- Butt, M.; Mohammed, R.; Butt, E.; Butt, S.; Xiang, J. Why Have Immunization Efforts in Pakistan Failed to Achieve Global Standards of Vaccination Uptake and Infectious Disease Control? Risk Manag. Health Policy 2020, 13, 111–124. [Google Scholar] [CrossRef]
- Bobo, F.T.; Asante, A.; Woldie, M.; Dawson, A.; Hayen, A. Child vaccination in sub-Saharan Africa: Increasing coverage addresses inequalities. Vaccine 2022, 40, 141–150. [Google Scholar] [CrossRef]
- Cata-Preta, B.O.; Santos, T.M.; Mengistu, T.; Hogan, D.R.; Barros, A.J.; Victora, C.G. Zero-dose children and the immunisation cascade: Understanding immunisation pathways in low and middle-income countries. Vaccine 2021, 39, 4564–4570. [Google Scholar] [CrossRef]
- Restrepo-Méndez, M.C.; Barros, A.J.; Wong, K.L.; Johnson, H.L.; Pariyo, G.; França, G.V.; Wehrmeister, F.C.; Victora, C.G. Inequalities in full immunization coverage: Trends in low-and middle-income countries. Bull. World Health Organ. 2016, 94, 794–805B. [Google Scholar] [CrossRef]
- Shahid, S.; Ahmed, S.; Qazi, M.F.; Ali, R.; Ali, S.A.; Zaidi, A.K.; Iqbal, N.T.; Jehan, F.; Nisar, M.I. Differential coverage for vaccines in the expanded program on immunization (EPI) among children in rural Pakistan. Vaccine 2023, 41, 2680–2689. [Google Scholar] [CrossRef]
- Umer, M.F.; Zofeen, S.; Hu, W.; Qi, X.; Zhuang, G. Spatiotemporal clustering analysis of Expanded Program on Immunization (EPI) vaccination coverage in Pakistan. Sci. Rep. 2020, 10, 10980. [Google Scholar] [CrossRef]
- Habib, M.A.; Soofi, S.B.; Hussain, Z.; Ahmed, I.; Tahir, R.; Anwar, S.; Nauman, A.A.; Sharif, M.; Islam, M.; Cousens, S.; et al. A Holistic Strategy of Mother and Child Health Care to Improve the Coverage of Routine and Polio Immunization in Pakistan: Results from a Demonstration Project. Vaccines 2024, 12, 89. [Google Scholar] [CrossRef] [PubMed]
- Filmer, D.; Pritchett, L.H. Estimating wealth effects without expenditure data—Or tears: An application to educational enrollments in states of India. Demography 2001, 38, 115–132. [Google Scholar]
- Arsenault, C.; Harper, S.; Nandi, A.; Rodríguez, J.M.M.; Hansen, P.M.; Johri, M. Monitoring equity in vaccination coverage: A systematic analysis of demographic and health surveys from 45 Gavi-supported countries. Vaccine 2017, 35, 951–959. [Google Scholar] [CrossRef]
- Siddiqui, F.A.; Padhani, Z.A.; Salam, R.A.; Aliani, R.; Lassi, Z.S.; Das, J.K.; Bhutta, Z.A. Interventions to Improve Immunization Coverage Among Children and Adolescents: A Meta-analysis. Pediatrics 2022, 149 (Suppl. 5), e2021053852D. [Google Scholar] [CrossRef]
- UNICEF. Gender Disparities in Immunization Coverage: What We Know; UNICEF Report; UNICEF: New York, NY, USA, 2021. [Google Scholar]
- Naseer, F.; Sultan, R.S. Barriers to Access and Utilization of Maternal Health Care Services in District Quetta, Baluchistan. Pak. JL Anal. Wisdom 2023, 2, 623. [Google Scholar]
- Joachim, G.E.; Wagner, A.L.; Naseem, M.; Boulton, M.L. Trends in childhood vaccination in Pakistan and associated factors; 2006–2018. Vaccine 2004, 42, 795–800. [Google Scholar] [CrossRef]
- Rammohan, A.; Awofeso, N. District-level variations in childhood immunizations in India: The role of socio-economic factors and health infrastructure. Soc. Sci. Med. 2015, 145, 163–172. [Google Scholar] [CrossRef] [PubMed]
- Arooj, S.; Ali, S.; Baber, N.; Abbasi, A.; Ali, M. Socioeconomic factors effecting polio vaccination in Pakistan. Health 2013, 5, 892–897. [Google Scholar] [CrossRef]
- Hajizadeh, M. Socioeconomic inequalities in child vaccination in low/middle-income countries: What accounts for the differences? J. Epidemiol. Community Health 2018, 72, 719–725. [Google Scholar] [CrossRef]
- Gandhi, G. Charting the evolution of approaches employed by the Global Alliance for Vaccines and Immunizations (GAVI) to address inequities in access to immunization: A systematic qualitative review of GAVI policies, strategies and resource allocation mechanisms through an equity lens (1999–2014). BMC Public Health 2015, 15, 1198. [Google Scholar]
- WHO. Global Routine Immunization Strategies and Practices (GRISP): A Companion Document to the Global Vaccine Action Plan (GVAP); WHO: Geneva, Switzerland, 2016. [Google Scholar]


| Characteristics | BL % (95% CI) | EL % (95% CI) | EL-BL % (95% CI) |
|---|---|---|---|
| Gender | |||
| Male | 54.9% (54.6%, 55.2%) | 55.9% (55.6%, 56.2%) | 1.0% (0.6%, 1.4%) |
| Female | 45.1% (44.8%, 45.4%) | 44.1% (43.8%, 44.4%) | −1.0% (−1.4%, −0.6%) |
| Age (months) | |||
| 0–23 | 36.6% (36.3%, 37.0%) | 37.8% (37.3%, 38.3%) | 1.2% (0.6%, 1.8%) |
| 24–59 | 63.4% (63.0%, 63.7%) | 62.2% (61.7%, 62.7%) | −1.2% (−1.8%, −0.6%) |
| Wealth quintile | |||
| Poorest | 19.0% (18.1%, 19.9%) | 20.5% (19.7%, 21.4%) | 1.5% (0.5%, 2.5%) |
| Poor | 19.4% (18.8%, 20.0%) | 20.1% (19.5%, 20.7%) | 0.7% (−0.1%, 1.5%) |
| Middle | 19.9% (19.3%, 20.4%) | 19.9% (19.3%, 20.5%) | 0.1% (−0.7%, 0.8%) |
| Rich | 20.3% (19.7%, 21.0%) | 19.6% (19.0%, 20.2%) | −0.7% (−1.5%, 0.1%) |
| Richest | 21.4% (20.4%, 22.3%) | 19.8% (19.0%, 20.6%) | −1.5% (−2.6%, −0.5%) |
| Mother education | |||
| Literate | 44.5% (43.6%, 45.5%) | 50.8% (49.8%, 51.8%) | 6.3% (5.1%, 7.5%) |
| Illiterate | 55.5% (54.5%, 56.4%) | 49.2% (48.2%, 50.2%) | −6.3% (−7.5%, −5.1%) |
| Family Size | |||
| ≤6 | 36.6% (35.8%, 37.4%) | 38.9% (38.0%, 39.7%) | 2.3% (1.3%, 3.2%) |
| >6 | 63.4% (62.6%, 64.2%) | 61.1% (60.3%, 62.0%) | −2.3% (−3.2%, −1.3%) |
| Improved water | 80.7% (79.7%, 81.8%) | 86.4% (85.5%, 87.2%) | 5.6% (4.5%, 6.8%) |
| Improved toilet facility | 65.1% (63.9%, 66.4%) | 67.3% (66.2%, 68.5%) | 2.2% (0.8%, 3.6%) |
| Equity Parameters | BL % (95% CI) | EL % (95% CI) | EL-BL % (95% CI) | p-Values |
|---|---|---|---|---|
| Overall | 41.6% (40.6%, 42.7%) | 62.3% (61.2%, 63.3%) | 20.6% (19.3%, 22.0%) | <0.001 |
| Gender | ||||
| Male | 41.7% (40.5%, 42.8%) | 63.2% (62.1%, 64.3%) | 21.5% (20.1%, 22.9%) | <0.001 |
| Female | 41.6% (40.5%, 42.7%) | 61.1% (60.0%, 62.2%) | 19.5% (18.1%, 20.9%) | <0.001 |
| Age (months) | ||||
| 0–23 | 40.1% (39.0%, 41.2%) | 63.5% (62.4%, 64.6%) | 23.4% (22.0%, 24.8%) | <0.001 |
| 24–59 | 42.5% (41.4%, 43.7%) | 61.5% (60.3%, 62.7%) | 19.0% (17.5%, 20.5%) | <0.001 |
| Wealth quintile | ||||
| Poorest | 28.5% (26.7%, 30.3%) | 51.6% (49.5%, 53.8%) | 23.1% (20.5%, 25.8%) | <0.001 |
| Poor | 36.4% (34.8%, 38.0%) | 59.1% (57.4%, 60.8%) | 22.7% (20.4%, 24.9%) | <0.001 |
| Middle | 40.3% (38.8%, 41.8%) | 61.5% (59.9%, 63.1%) | 21.3% (19.2%, 23.3%) | <0.001 |
| Rich | 44.8% (43.2%, 46.4%) | 66.9% (65.4%, 68.4%) | 22.1% (20.1%, 24.2%) | <0.001 |
| Richest | 56.4% (54.6%, 58.2%) | 72.7% (71.1%, 74.2%) | 16.2% (14.0%, 18.4%) | <0.001 |
| Mother education | ||||
| Literate | 50.6% (49.2%, 52.0%) | 69.3% (68.0%, 70.5%) | 18.7% (17.0%, 20.3%) | <0.001 |
| Illiterate | 34.5% (33.3%, 35.6%) | 55.0% (53.7%, 56.3%) | 20.5% (19.0%, 22.1%) | <0.001 |
| Family Size | ||||
| ≤6 | 50.8% (49.5%, 52.0%) | 66.9% (65.7%, 68.0%) | 16.1% (14.5%, 17.6%) | <0.001 |
| >6 | 36.4% (35.2%, 37.6%) | 59.3% (58.0%, 60.7%) | 23.0% (21.3%, 24.6%) | <0.001 |
| Equity Parameters | BL % (95% CI) | EL % (95% CI) | EL-BL % (95% CI) | p-Values |
|---|---|---|---|---|
| Overall | 35.5% (34.5%, 36.5%) | 25.2% (24.4%, 26.1%) | −10.2% (−11.4%, −9.1%) | <0.001 |
| Gender | ||||
| Male | 35.5% (34.4%, 36.6%) | 24.9% (24.0%, 25.8%) | −10.5% (−11.8%, −9.3%) | <0.001 |
| Female | 35.5% (34.4%, 36.5%) | 25.6% (24.7%, 26.5%) | −9.8% (−11.0%, −8.6%) | <0.001 |
| Age (months) | ||||
| 0–23 | 36.0% (35.0%, 37.0%) | 26.0% (25.2%, 26.9%) | −10.0% (−11.2%, −8.8%) | <0.001 |
| 24–59 | 35.1% (34.0%, 36.3%) | 24.8% (23.8%, 25.8%) | −10.4% (−11.7%, −9.0%) | <0.001 |
| Wealth quintile | ||||
| Poorest | 47.8% (45.6%, 50.0%) | 35.9% (33.8%, 38.0%) | −11.8% (−14.6%, −9.1%) | <0.001 |
| Poor | 37.2% (35.6%, 38.8%) | 26.4% (25.0%, 27.8%) | −10.8% (−12.7%, −8.8%) | <0.001 |
| Middle | 34.8% (33.3%, 36.3%) | 23.7% (22.5%, 24.9%) | −11.1% (−13.0%, −9.3%) | <0.001 |
| Rich | 32.8% (31.4%, 34.2%) | 21.1% (20.0%, 22.1%) | −11.7% (−13.5%, −10.0%) | <0.001 |
| Richest | 26.1% (24.7%, 27.5%) | 18.7% (17.5%, 19.9%) | −7.4% (−9.2%, −5.6%) | <0.001 |
| Mother education | ||||
| Literate | 31.7% (30.5%, 32.9%) | 22.3% (21.2%, 23.3%) | −9.5% (−10.9%, −8.0%) | <0.001 |
| Illiterate | 38.5% (37.2%, 39.7%) | 28.3% (27.3%, 29.4%) | −10.1% (−11.6%, −8.7%) | <0.001 |
| Family Size | ||||
| ≤6 | 31.8% (30.7%, 33.0%) | 22.8% (21.9%, 23.8%) | −9.0% (−10.3%, −7.6%) | <0.001 |
| >6 | 37.6% (36.3%, 38.8%) | 26.8% (25.7%, 27.9%) | −10.8% (−12.3%, −9.3%) | <0.001 |
| Equity Parameters | BL % (95% CI) | EL % (95% CI) | EL-BL % (95% CI) | p-Values |
|---|---|---|---|---|
| Overall | 22.9% (21.9%, 23.8%) | 12.5% (11.7%, 13.2%) | −10.4% (−11.5%, −9.3%) | <0.001 |
| Gender | ||||
| Male | 22.9% (21.9%, 23.9%) | 11.9% (11.1%, 12.6%) | −11.0% (−12.1%, −9.8%) | <0.001 |
| Female | 22.9% (22.0%, 23.9%) | 13.3% (12.5%, 14.1%) | −9.7% (−10.8%, −8.5%) | <0.001 |
| Age | ||||
| 0–23 | 23.9% (22.9%, 24.9%) | 10.5% (9.8%, 11.1%) | −13.4% (−14.5%, −12.3%) | <0.001 |
| 24–59 | 22.3% (21.3%, 23.3%) | 13.7% (12.9%, 14.6%) | −8.6% (−9.8%, −7.4%) | <0.001 |
| Wealth quintile | ||||
| Poorest | 23.7% (21.9%, 25.6%) | 12.4% (11.1%, 13.8%) | −11.3% (−13.6%, −9.1%) | <0.001 |
| Poor | 26.4% (24.8%, 27.9%) | 14.5% (13.3%, 15.7%) | −11.9% (−13.8%, −10.0%) | <0.001 |
| Middle | 24.9% (23.5%, 26.4%) | 14.8% (13.6%, 16.0%) | −10.1% (−11.9%, −8.4%) | <0.001 |
| Rich | 22.4% (21.0%, 23.8%) | 12.0% (10.9%, 13.1%) | −10.4% (−12.0%, −8.7%) | <0.001 |
| Richest | 17.5% (15.9%, 19.1%) | 8.6% (7.7%, 9.6%) | −8.9% (−10.6%, −7.1%) | <0.001 |
| Mother education | ||||
| Literate | 17.7% (16.6%, 18.8%) | 8.5% (7.7%, 9.2%) | −9.2% (−10.5%, −8.0%) | <0.001 |
| Illiterate | 27.1% (25.9%, 28.2%) | 16.7% (15.6%, 17.7%) | −10.4% (−11.8%, −9.0%) | <0.001 |
| Family Size | ||||
| ≤6 | 17.4% (16.4%, 18.4%) | 10.3% (9.6%, 11.0%) | −7.1% (−8.2%, −6.0%) | <0.001 |
| >6 | 26.1% (24.9%, 27.2%) | 13.9% (13.0%, 14.8%) | −12.2% (−13.5%, −10.8%) | <0.001 |
| Equity Parameters | BL % (95% CI) | EL % (95% CI) | EL-BL % (95% CI) | p-Values |
|---|---|---|---|---|
| Overall | 29.2% (28.0%, 30.3%) | 15.6% (14.8%, 16.5%) | −13.5% (−14.8%, −12.2%) | <0.001 |
| Gender | ||||
| Male | 29.7% (28.5%, 30.9%) | 15.2% (14.3%, 16.0%) | −14.5% (−15.9%, −13.1%) | <0.001 |
| Female | 28.5% (27.4%, 29.6%) | 16.2% (15.3%, 17.1%) | −12.3% (−13.6%, −10.9%) | <0.001 |
| Age | ||||
| 0–23 | 26.3% (25.2%, 27.4%) | 10.2% (9.5%, 10.9%) | −16.1% (−17.3%, −14.9%) | <0.001 |
| 24–59 | 30.8% (29.6%, 32.0%) | 18.9% (17.9%, 20.0%) | −11.9% (−13.3%, −10.4%) | <0.001 |
| Wealth quintile | ||||
| Poorest | 34.3% (31.8%, 36.8%) | 16.7% (15.2%, 18.2%) | −17.6% (−20.5%, −14.7%) | <0.001 |
| Poor | 34.2% (32.3%, 36.0%) | 18.0% (16.6%, 19.4%) | −16.2% (−18.4%, −13.9%) | <0.001 |
| Middle | 30.9% (29.2%, 32.5%) | 17.9% (16.6%, 19.3%) | −13.0% (−15.0%, −11.0%) | <0.001 |
| Rich | 27.4% (25.8%, 29.0%) | 15.0% (13.8%, 16.2%) | −12.4% (−14.2%, −10.6%) | <0.001 |
| Richest | 20.0% (18.4%, 21.7%) | 10.4% (9.4%, 11.5%) | −9.6% (−11.5%, −7.7%) | <0.001 |
| Mother education | ||||
| Literate | 24.5% (23.2%, 25.9%) | 11.6% (10.7%, 12.4%) | −13.0% (−14.5%, −11.4%) | <0.001 |
| Illiterate | 32.9% (31.5%, 34.2%) | 19.8% (18.7%, 21.0%) | −13.0% (−14.6%, −11.4%) | <0.001 |
| Family Size | ||||
| ≤6 | 19.5% (18.4%, 20.5%) | 12.7% (11.8%, 13.5%) | −6.8% (−8.0%, −5.5%) | <0.001 |
| >6 | 34.7% (33.4%, 36.1%) | 17.5% (16.5%, 18.5%) | −17.2% (−18.9%, −15.6%) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chauhadry, I.A.; Soofi, S.B.; Sajid, M.; Ali, R.; Khan, A.; Naqvi, S.K.; Hussain, I.; Umer, M.; Bhutta, Z.A. Bridging the Vaccination Equity Gap: A Community-Driven Approach to Reduce Vaccine Inequities in Polio High-Risk Areas of Pakistan. Vaccines 2024, 12, 1340. https://doi.org/10.3390/vaccines12121340
Chauhadry IA, Soofi SB, Sajid M, Ali R, Khan A, Naqvi SK, Hussain I, Umer M, Bhutta ZA. Bridging the Vaccination Equity Gap: A Community-Driven Approach to Reduce Vaccine Inequities in Polio High-Risk Areas of Pakistan. Vaccines. 2024; 12(12):1340. https://doi.org/10.3390/vaccines12121340
Chicago/Turabian StyleChauhadry, Imran A., Sajid Bashir Soofi, Muhammad Sajid, Rafey Ali, Ahmad Khan, Syeda Kanza Naqvi, Imtiaz Hussain, Muhammad Umer, and Zulfiqar A. Bhutta. 2024. "Bridging the Vaccination Equity Gap: A Community-Driven Approach to Reduce Vaccine Inequities in Polio High-Risk Areas of Pakistan" Vaccines 12, no. 12: 1340. https://doi.org/10.3390/vaccines12121340
APA StyleChauhadry, I. A., Soofi, S. B., Sajid, M., Ali, R., Khan, A., Naqvi, S. K., Hussain, I., Umer, M., & Bhutta, Z. A. (2024). Bridging the Vaccination Equity Gap: A Community-Driven Approach to Reduce Vaccine Inequities in Polio High-Risk Areas of Pakistan. Vaccines, 12(12), 1340. https://doi.org/10.3390/vaccines12121340







