Leveraging Data from a Provincial Electronic Immunization Registry to Analyze Immunization Coverage, Timeliness, and Defaulters Among 8.8 Million Children from the 2018 to 2023 Birth Cohorts in Sindh Province, Pakistan
Abstract
1. Introduction
2. Materials and Methods
2.1. Population
2.2. External Natural Shocks Impacting Immunization in Sindh
2.3. Data Source
2.4. Vaccination Schedule
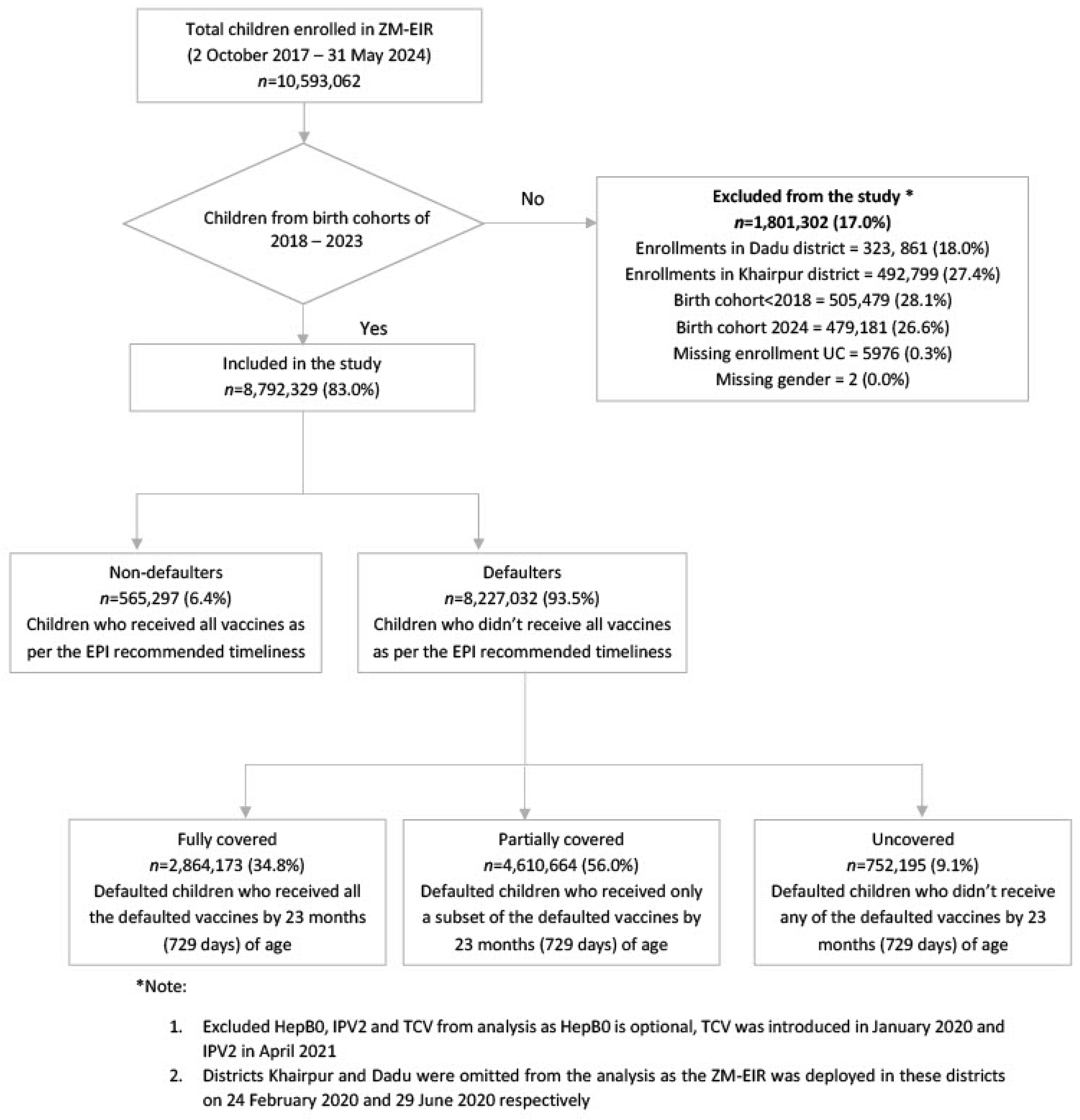
2.5. Study Design and Procedure
2.6. Outcome and Measures
2.7. Statistical Analysis
3. Results
3.1. Overview of Immunization Coverage and Timeliness
3.2. Trends in Coverage and Predictors of Immunization Defaulters
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Li, X.; Mukandavire, C.; Cucunubá, Z.M.; Londono, S.E.; Abbas, K.; Clapham, H.E.; Jit, M.; Johnson, H.L.; Papadopoulos, T.; Vynnycky, E.; et al. Estimating the Health Impact of Vaccination against Ten Pathogens in 98 Low-Income and Middle-Income Countries from 2000 to 2030: A Modelling Study. Lancet 2021, 397, 398–408. [Google Scholar] [CrossRef] [PubMed]
- Global Immunization Efforts Have Saved at Least 154 Million Lives over the Past 50 Years. Available online: https://www.who.int/news/item/24-04-2024-global-immunization-efforts-have-saved-at-least-154-million-lives-over-the-past-50-years (accessed on 26 July 2024).
- Essential Programme on Immunization. Available online: https://www.who.int/teams/immunization-vaccines-and-biologicals/essential-programme-on-immunization (accessed on 29 July 2024).
- Feikin, D.R.; Flannery, B.; Hamel, M.J.; Stack, M.; Hansen, P.M. Vaccines for Children in Low- and Middle-Income Countries. In Reproductive, Maternal, Newborn, and Child Health: Disease Control Priorities, Third Edition (Volume 2); Black, R.E., Laxminarayan, R., Temmerman, M., Walker, N., Eds.; The International Bank for Reconstruction and Development/The World Bank: Washington, DC, USA, 2016; ISBN 978-1-4648-0348-2. [Google Scholar]
- Immunization Agenda 2030. Available online: https://www.who.int/teams/immunization-vaccines-and-biologicals/strategies/ia2030 (accessed on 12 August 2024).
- Phase 5 (2021–2025). Available online: https://www.gavi.org/our-alliance/strategy/phase-5-2021-2025 (accessed on 12 August 2024).
- Dadari, I.; Belt, R.V.; Iyengar, A.; Ray, A.; Hossain, I.; Ali, D.; Danielsson, N.; Sodha, S.V. Achieving the IA2030 Coverage and Equity Goals through a Renewed Focus on Urban Immunization. Vaccines 2023, 11, 809. [Google Scholar] [CrossRef] [PubMed]
- Ota, M.O.C.; Badur, S.; Romano-Mazzotti, L.; Friedland, L.R. Impact of COVID-19 Pandemic on Routine Immunization. Ann. Med. 2021, 53, 2286–2297. [Google Scholar] [CrossRef] [PubMed]
- Immunization Coverage. Available online: https://www.who.int/news-room/fact-sheets/detail/immunization-coverage (accessed on 29 July 2024).
- EPI. Health Department of Sindh. Available online: https://sindhhealth.gov.pk/EPI (accessed on 30 July 2024).
- EMHJ. A Review of EPI Progress in Pakistan towards Achieving Coverage Targets: Present Situation and the Way Forward. Available online: http://www.emro.who.int/emhj-volume-16-2010/volume-16-supplement/article-04.html (accessed on 12 August 2024).
- GPEI-Pakistan. Global Polio Eradication Initiative. Available online: https://polioeradication.org/about-polio/where-we-work/ (accessed on 14 November 2024).
- Mbaeyi, C.; Baig, S.; Safdar, R.M.; Khan, Z.; Young, H.; Jorba, J.; Wadood, Z.M.; Jafari, H.; Alam, M.M.; Franka, R. Progress Toward Poliomyelitis Eradication—Pakistan, January 2022–June 2023. Morb. Mortal. Wkly. Rep. 2023, 72, 880–885. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Population Studies-NIPS/Pakistan and ICF. Pakistan Demographic and Health Survey: 2017–2018. Available online: https://dhsprogram.com/publications/publication-fr354-dhs-final-reports.cfm (accessed on 11 October 2024).
- Ali, I.; Hamid, S. Implications of COVID-19 and “Super Floods” for Routine Vaccination in Pakistan: The Reemergence of Vaccine Preventable-Diseases Such as Polio and Measles. Hum. Vaccines Immunother. 2022, 18, 2154099. [Google Scholar] [CrossRef] [PubMed]
- Joachim, G.E.; Wagner, A.L.; Naseem, M.; Boulton, M.L. Trends in Childhood Vaccination in Pakistan and Associated Factors; 2006–2018. Vaccine 2024, 42, 795–800. [Google Scholar] [CrossRef] [PubMed]
- Ashraf, M.F.; Daim, S.U.R.; Fayyaz, H.; Ashraf, M.A.; Ashraf, M. Navigating Pakistan’s Immunization Landscape: Progress and Pitfalls. IJID Reg. 2024, 12, 100382. [Google Scholar] [CrossRef] [PubMed]
- Shahid, S.; Ahmed, S.; Qazi, M.F.; Ali, R.; Ali, S.A.; Zaidi, A.K.M.; Iqbal, N.T.; Jehan, F.; Imran Nisar, M. Differential Coverage for Vaccines in the Expanded Program on Immunization (EPI) among Children in Rural Pakistan. Vaccine 2023, 41, 2680–2689. [Google Scholar] [CrossRef] [PubMed]
- Butt, M.; Mohammed, R.; Butt, E.; Butt, S.; Xiang, J. Why Have Immunization Efforts in Pakistan Failed to Achieve Global Standards of Vaccination Uptake and Infectious Disease Control? Risk Manag. Healthc. Policy 2020, 13, 111–124. [Google Scholar] [CrossRef] [PubMed]
- Chandir, S.; Siddiqi, D.A.; Mehmood, M.; Setayesh, H.; Siddique, M.; Mirza, A.; Soundardjee, R.; Dharma, V.K.; Shah, M.T.; Abdullah, S.; et al. Impact of COVID-19 Pandemic Response on Uptake of Routine Immunizations in Sindh, Pakistan: An Analysis of Provincial Electronic Immunization Registry Data. Vaccine 2020, 38, 7146–7155. [Google Scholar] [CrossRef] [PubMed]
- Sindh: Pakistan Bureau of Statistics. 2023. Available online: https://www.pbs.gov.pk/sites/default/files/population/2023/Sindh.pdf (accessed on 7 July 2024).
- Economy—Government of Sindh. Available online: https://www.sindh.gov.pk/economy (accessed on 30 July 2024).
- Local Govts—Local Government Department. Available online: https://lgdsindh.gov.pk/wp/local-govts/ (accessed on 7 July 2024).
- Factsheet: Strengthening Social Protection Delivery System in Sindh. Available online: https://www.worldbank.org/en/news/factsheet/2022/12/19/factsheet-strengthening-social-protection-delivery-system-in-sindh (accessed on 30 July 2024).
- Government of Pakistan. Pakistan Economic Survey: 2020–2021; Finance Division, Government of Pakistan: Islamabad, Pakistan, 2021. [Google Scholar]
- UNICEF. Sindh 2018–2019: Child Mortality. Multiple Indicator Cluster Survey; Bureau of Statistics, Planning and Developnment Board, Government of Sindh: Islamabad, Pakistan; UNICEF: New York, NY, USA, 2021. [Google Scholar]
- Original Research: Prevalence, Geographical Distribution and Factors Associated with Pentavalent Vaccine Zero Dose Status among Children in Sindh, Pakistan: Analysis of Data from the 2017 and 2018 Birth Cohorts Enrolled in the Provincial Electronic Immunisation Registry—PMC. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9119190/ (accessed on 12 August 2024).
- Pakistan COVID—Coronavirus Statistics—Worldometer. Available online: https://www.worldometers.info/coronavirus/country/pakistan/ (accessed on 31 July 2024).
- Pakistan’s Response to COVID-19: Overcoming National and International Hypes to Fight the Pandemic—PMC. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8136406/ (accessed on 31 July 2024).
- Coronavirus Disease (COVID-19) Pandemic. Available online: https://www.who.int/europe/emergencies/situations/covid-19 (accessed on 31 July 2024).
- Provincial Disaster Management Authority, Rehabilitation Department, Government of Sindh. Admin Flood 2022 in Sindh. PDMA_SINDH 2023. Available online: https://pdma.gos.pk/2023/02/07/flood-2022-in-sindh/ (accessed on 12 August 2024).
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef] [PubMed]
- Bago, B.; Terefe, W.; Sebagadis, G. Individual and Community Level Factors Associated with Defaulting of Immunization among 12–59 Months Children in Ethiopia: Multilevel Modeling Analysis Using 2011Ethiopia Demographic and Health Survey. Curr. Pediatr. Res. 2018, 22, 95–110. [Google Scholar]
- Khan, I.; Ameen, A.; Anwar, R.; Rahman, A.U.; Ali, M.W.; Khan, H.; Omair, M.; Alam, M.B. Comprehensive Outreach: Reach Every Child Initiative Expanded Program on Immunization Khyber Pakhtunkhwa, Pakistan. J. Health Rehabil. Res. 2024, 4, 188–193. [Google Scholar] [CrossRef]
- Childhood Immunization Bounces Back to Pre-COVID-19 Levels in Five South Asian Countries. Available online: https://www.unicef.org/pakistan/press-releases/childhood-immunization-bounces-back-pre-covid-19-levels-five-south-asian-countries (accessed on 13 August 2024).
- “Pakistan Can”: How One Country Repaired Its Routine Immunisation Safety Net. Available online: https://www.gavi.org/vaccineswork/pakistan-can-how-one-country-repaired-its-routine-immunisation-safety-net (accessed on 19 September 2024).
- Jamison, A.F.; McCormick, B.J.J.; Hussain, E.; Thomas, E.D.; Azam, S.I.; Hansen, C.L.; Rasmussen, Z.A. Determinants of Vaccine Coverage and Timeliness in a Northern Pakistani Village. PLoS ONE 2022, 17, e0263712. [Google Scholar] [CrossRef] [PubMed]
- Noh, J.-W.; Kim, Y.; Akram, N.; Yoo, K.B.; Cheon, J.; Lee, L.J.; Kwon, Y.D.; Stekelenburg, J. Determinants of Timeliness in Early Childhood Vaccination among Mothers with Vaccination Cards in Sindh Province, Pakistan: A Secondary Analysis of Cross-Sectional Survey Data. BMJ Open 2019, 9, e028922. [Google Scholar] [CrossRef] [PubMed]
- BMC Pediatrics. BCG Vaccination in Southern Rural Mozambique: An Overview of Coverage and Its Determinants Based on Data from the Demographic and Health Surveillance System in the District of Manhiça. 2018. Available online: https://bmcpediatr.biomedcentral.com/articles/10.1186/s12887-018-1003-4 (accessed on 20 September 2024).
- Trends and Determinants of Vaccination Among Children Aged 06–59 Months in Bangladesh: Country Representative Survey from 1993 to 2014. BMC Public Health. 2021. Available online: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-021-11576-0 (accessed on 20 September 2024).
- Vaccination and Immunization Statistics. Available online: https://data.unicef.org/topic/child-health/immunization/ (accessed on 20 September 2024).
- Schoeps, A.; Ouédraogo, N.; Kagoné, M.; Sié, A.; Müller, O.; Becher, H. Socio-Demographic Determinants of Timely Adherence to BCG, Penta3, Measles, and Complete Vaccination Schedule in Burkina Faso. Vaccine 2013, 32, 96–102. [Google Scholar] [CrossRef] [PubMed]
- At Least 80 Million Children Under One at Risk of Diseases Such as Diphtheria, Measles and Polio as COVID-19 Disrupts Routine Vaccination Efforts, Warn Gavi, WHO and UNICEF. Available online: https://www.who.int/news/item/22-05-2020-at-least-80-million-children-under-one-at-risk-of-diseases-such-as-diphtheria-measles-and-polio-as-covid-19-disrupts-routine-vaccination-efforts-warn-gavi-who-and-unicef (accessed on 26 July 2024).
- Noh, J.W.; Kim, Y.M.; Akram, N.; Yoo, K.B.; Park, J.; Cheon, J.; Kwon, Y.D.; Stekelenburg, J. Factors Affecting Complete and Timely Childhood Immunization Coverage in Sindh, Pakistan; A Secondary Analysis of Cross-Sectional Survey Data. PLoS ONE 2018, 13, e0206766. Available online: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0206766 (accessed on 14 November 2024). [CrossRef] [PubMed]
- Bekele, G.; Darega, J.; Mulu, E.; Tsegaw, M. Determinants of Immunization Defaulters among Children Aged 12–23 Months in Ambo Town, Oromia, Ethiopia: A Case–Control Study. Hum. Vaccines Immunother. 2024, 20, 2338952. [Google Scholar] [CrossRef] [PubMed]
- Krishna, D.; Mohd Zulkefli, N.A.; Md Said, S.; Mahmud, A. Sociodemographic and Health Care Factors in Determining Immunization Defaulters among Preschool Children in Petaling District, Selangor: A Cross-Sectional Study in Malaysia. BMC Public Health 2019, 19, 1275. [Google Scholar] [CrossRef] [PubMed]




| 2018 (n = 1,025,904) | 2019 (n = 1,349,301) | 2020 (n = 1,427,321) | 2021 (n = 1,456,235) | 2022 (n = 1,781,011) | 2023 b (n = 1,752,557) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | n | % | |
| BCG | 838,759 | 81.8 | 1,115,125 | 82.6 | 1,241,736 | 87.0 | 1,264,245 | 86.8 | 1,608,041 | 90.3 | 1,598,400 | 91.2 |
| Penta-1 | 795,965 | 77.6 | 1,091,995 | 80.9 | 1,230,126 | 86.2 | 1,274,994 | 87.6 | 1,626,996 | 91.4 | 1,555,632 | 88.8 |
| OPV-1 | 793,680 | 77.4 | 1,090,271 | 80.8 | 1,230,836 | 86.2 | 1,275,553 | 87.6 | 1,627,170 | 91.4 | 1,555,720 | 88.8 |
| PCV-1 | 795,716 | 77.6 | 1,091,409 | 80.9 | 1,229,525 | 86.1 | 1,274,610 | 87.5 | 1,626,875 | 91.4 | 1,555,427 | 88.8 |
| Rota-1 | 726,949 | 70.9 | 1,071,660 | 79.4 | 1,212,780 | 85.0 | 1,262,421 | 86.7 | 1,619,480 | 90.9 | 1,554,627 | 88.7 |
| Penta-2 | 707,046 | 68.9 | 1,005,418 | 74.5 | 1,151,892 | 80.7 | 1,211,603 | 83.2 | 1,519,045 | 85.3 | 1,352,710 | 77.2 |
| OPV-2 | 706,414 | 68.9 | 1,004,673 | 74.5 | 1,152,511 | 80.8 | 1,211,894 | 83.2 | 1,518,881 | 85.3 | 1,352,609 | 77.2 |
| PCV-2 | 707,029 | 68.9 | 1,005,008 | 74.5 | 1,151,566 | 80.7 | 1,211,381 | 83.2 | 1,518,937 | 85.3 | 1,352,683 | 77.2 |
| Rota-2 | 631,306 | 61.5 | 971,064 | 72.0 | 1,120,812 | 78.5 | 1,189,101 | 81.7 | 1,507,849 | 84.7 | 1,351,851 | 77.1 |
| Penta-3 | 662,556 | 64.6 | 962,962 | 71.4 | 1,143,243 | 80.1 | 1,234,864 | 84.8 | 1,521,773 | 85.4 | 1,219,269 | 69.6 |
| OPV-3 | 662,497 | 64.6 | 963,027 | 71.4 | 1,143,648 | 80.1 | 1,234,633 | 84.8 | 1,521,354 | 85.4 | 1,219,021 | 69.6 |
| PCV-3 | 662,883 | 64.6 | 962,774 | 71.4 | 1,142,820 | 80.1 | 1,234,380 | 84.8 | 1,521,468 | 85.4 | 1,219,208 | 69.6 |
| IPV-1 | 701,996 | 68.4 | 1,001,399 | 74.2 | 1,179,686 | 82.7 | 1,269,917 | 87.2 | 1,565,805 | 87.9 | 1,287,079 | 73.4 |
| Measles-1 | 679,936 | 66.3 | 972,423 | 72.1 | 1,163,588 | 81.5 | 1,264,048 | 86.8 | 1,505,384 | 84.5 | 744,064 | 42.5 |
| Measles-2 | 494,924 | 48.2 | 775,845 | 57.5 | 938,988 | 65.8 | 1,083,596 | 74.4 | 1,154,170 | 64.8 | 85,543 | 4.9 |
| FIC-M1 (without PCV) | 486,961 | 47.5 | 710,973 | 52.7 | 907,318 | 63.6 | 988,424 | 67.9 | 1,258,668 | 70.7 | 622,340 | 35.5 |
| FIC-M1 (with PCV) | 486,651 | 47.4 | 710,110 | 52.6 | 906,145 | 63.5 | 987,617 | 67.8 | 1,257,876 | 70.6 | 622,050 | 35.5 |
| FIC-M1 (with Rota) | 436,596 | 42.6 | 687,068 | 50.9 | 881,595 | 61.8 | 968,413 | 66.5 | 1,247,209 | 70.0 | 620,977 | 35.4 |
| FIC-M2 (without PCV) | 344,085 | 33.5 | 561,749 | 41.6 | 740,764 | 51.9 | 860,908 | 59.1 | 992,417 | 55.7 | 77,370 | 4.4 |
| FIC-M2 (with PCV) | 343,927 | 33.5 | 561,164 | 41.6 | 739,867 | 51.8 | 860,253 | 59.1 | 991,914 | 55.7 | 77,348 | 4.4 |
| FIC-M2 (with Rota) | 308,873 | 30.1 | 543,478 | 40.3 | 720,467 | 50.5 | 844,300 | 58.0 | 984,348 | 55.3 | 77,146 | 4.4 |
| Non-Defaulters | Defaulters | Defaulters | Total | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fully Covered | Partially Covered | Uncovered | ||||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |
| Total | 565,297 | 6.4 | 8,227,032 | 93.6 | 2,864,173 | 34.8 | 4,610,664 | 56.0 | 752,195 | 9.1 | 8,792,329 | 100.0 |
| Sex | ||||||||||||
| Male | 293,744 | 6.4 | 4,302,970 | 93.6 | 1,497,302 | 34.8 | 2,410,968 | 56.0 | 394,700 | 9.2 | 4,596,714 | 100.0 |
| Female | 271,553 | 6.5 | 3,924,062 | 93.5 | 1,366,871 | 34.8 | 2,199,696 | 56.1 | 357,495 | 9.1 | 4,195,615 | 100.0 |
| Residential Area | ||||||||||||
| Remote Rural | 8871 | 2.0 | 442,770 | 98.0 | 143,483 | 32.4 | 285,962 | 64.6 | 13,325 | 3.0 | 451,641 | 100.0 |
| Non-remote Rural | 115,976 | 3.5 | 3,230,403 | 96.5 | 1,212,758 | 37.5 | 1,857,466 | 57.5 | 160,179 | 5.0 | 3,346,379 | 100.0 |
| Urban | 440,450 | 8.8 | 4,553,859 | 91.2 | 1,507,932 | 33.1 | 2,467,236 | 54.2 | 578,691 | 12.7 | 4,994,309 | 100.0 |
| Residential sub-area | ||||||||||||
| Urban non-slum | 124,847 | 3.3 | 3,673,173 | 96.7 | 1,356,241 | 36.9 | 2,143,428 | 58.4 | 173,504 | 4.7 | 3,798,020 | 100.0 |
| Urban slum | 440,450 | 8.8 | 4,553,859 | 91.2 | 1,507,932 | 33.1 | 2,467,236 | 54.2 | 578,691 | 12.7 | 4,994,309 | 100.0 |
| Place of birth a | ||||||||||||
| Hospital | 142,040 | 11.1 | 1,134,712 | 88.9 | 414,501 | 36.5 | 560,463 | 49.4 | 159,748 | 14.1 | 1,276,752 | 100.0 |
| Maternity Home | 11,875 | 7.8 | 141,012 | 92.2 | 50,402 | 35.7 | 76,329 | 54.1 | 14,281 | 10.1 | 152,887 | 100.0 |
| Home | 25,053 | 3.6 | 666,940 | 96.4 | 224,563 | 33.7 | 392,954 | 58.9 | 49,423 | 7.4 | 691,993 | 100.0 |
| Enrollment Event b | ||||||||||||
| Fixed Site | 420,099 | 9.1 | 4,186,423 | 90.9 | 1,561,953 | 37.3 | 2,046,380 | 48.9 | 578,090 | 13.8 | 4,606,522 | 100.0 |
| Outreach | 117,102 | 4.2 | 2,645,010 | 95.8 | 882,113 | 33.4 | 1,643,140 | 62.1 | 119,757 | 4.5 | 2,762,112 | 100.0 |
| Enhanced outreach activities | 25,716 | 1.9 | 1,321,517 | 98.1 | 407,552 | 30.8 | 863,216 | 65.3 | 50,749 | 3.8 | 1,347,233 | 100.0 |
| Mobile Immunization Vans | 2380 | 3.1 | 74,080 | 96.9 | 12,553 | 16.9 | 57,928 | 78.2 | 3599 | 4.9 | 76,460 | 100.0 |
| Mother’s Education c (years) | ||||||||||||
| 0 | 17,964 | 2.9 | 591,010 | 97.1 | 202,282 | 34.2 | 337,458 | 57.1 | 51,270 | 8.7 | 608,974 | 100.0 |
| 1–5 | 29,659 | 4.7 | 600,493 | 95.3 | 229,640 | 38.2 | 308,233 | 51.3 | 62,620 | 10.4 | 630,152 | 100.0 |
| 6–8 | 6006 | 6.7 | 83,604 | 93.3 | 29,936 | 35.8 | 41,759 | 49.9 | 11,909 | 14.2 | 89,610 | 100.0 |
| 9–10 | 8546 | 10.3 | 74,757 | 89.7 | 25,145 | 33.6 | 35,087 | 46.9 | 14,525 | 19.4 | 83,303 | 100.0 |
| ≥11 | 8797 | 13.7 | 55,370 | 86.3 | 18,961 | 34.2 | 23,390 | 42.2 | 13,019 | 23.5 | 64,167 | 100.0 |
| Birth year | ||||||||||||
| 2018 | 44,430 | 4.3 | 981,474 | 95.7 | 232,144 | 23.7 | 582,696 | 59.4 | 166,634 | 17.0 | 1,025,904 | 100.0 |
| 2019 | 56,217 | 4.2 | 1,293,084 | 95.8 | 379,744 | 29.4 | 757,944 | 58.6 | 155,396 | 12.0 | 1,349,301 | 100.0 |
| 2020 | 54,663 | 3.8 | 1,372,658 | 96.2 | 492,752 | 35.9 | 770,140 | 56.1 | 109,766 | 8.0 | 1,427,321 | 100.0 |
| 2021 | 50,869 | 3.5 | 1,405,366 | 96.5 | 505,144 | 35.9 | 822,617 | 58.5 | 77,605 | 5.5 | 1,456,235 | 100.0 |
| 2022 | 103,792 | 5.8 | 1,677,219 | 94.2 | 643,981 | 38.4 | 931,103 | 55.5 | 102,135 | 6.1 | 1,781,011 | 100.0 |
| 2023 | 255,326 | 14.6 | 1,497,231 | 85.4 | 610,408 | 40.8 | 746,164 | 49.8 | 140,659 | 9.4 | 1,752,557 | 100.0 |
| Enrollment Age (months) | ||||||||||||
| 0–1 | 532,968 | 10.9 | 4,362,788 | 89.1 | 2,594,212 | 59.5 | 1,235,934 | 28.3 | 532,642 | 12.2 | 4,895,756 | 100.0 |
| 2–3 | 19,603 | 1.0 | 1,887,342 | 99.0 | 138,447 | 7.3 | 1,620,037 | 85.8 | 128,858 | 6.8 | 1,906,945 | 100.0 |
| 4–6 | 3075 | 0.4 | 841,770 | 99.6 | 55,853 | 6.6 | 766,891 | 91.1 | 19,026 | 2.3 | 844,845 | 100.0 |
| 7–9 | 3046 | 0.7 | 438,778 | 99.3 | 24,174 | 5.5 | 394,109 | 89.8 | 20,495 | 4.7 | 441,824 | 100.0 |
| 10–12 | 909 | 0.3 | 340,091 | 99.7 | 20,387 | 6.0 | 313,312 | 92.1 | 6392 | 1.9 | 341,000 | 100.0 |
| 13–15 | 4440 | 3.3 | 128,620 | 96.7 | 8445 | 6.6 | 97,502 | 75.8 | 22,673 | 17.6 | 133,060 | 100.0 |
| 16–18 | 1242 | 1.0 | 126,459 | 99.0 | 14,942 | 11.8 | 106,817 | 84.5 | 4700 | 3.7 | 127,701 | 100.0 |
| 19–21 | 5 | 0.0 | 51,786 | 100.0 | 5499 | 10.6 | 46,248 | 89.3 | 39 | 0.1 | 51,791 | 100.0 |
| ≥22 | 9 | 0.0 | 49,398 | 100.0 | 2214 | 4.5 | 29,814 | 60.4 | 17,370 | 35.2 | 49,407 | 100.0 |
| Age at Vaccination (in months) | Median | IQR e | Median | IQR e | Median | IQR e | Median | IQR e | Median | IQR e | Median | IQR e |
| BCG/OPV-0 | 0.23 | 0.10–0.43 | 0.72 | 0.23–2.04 | 0.43 | 0.20–0.89 | 1.94 | 0.53–3.98 | 0.16 | 0.03–0.39 | 0.66 | 0.23–2.00 |
| Penta-1/OPV-1/PCV-1 | 1.51 | 1.45–1.64 | 2.27 | 1.71–3.81 | 2.04 | 1.61–2.83 | 2.79 | 1.91–5.06 | 1.58 | 1.48–1.78 | 2.14 | 1.64–3.58 |
| Penta-2/OPV-2/PCV-2 | 2.60 | 2.47–2.76 | 4.21 | 3.09–6.64 | 3.75 | 2.99–5.26 | 4.96 | 3.45–8.18 | 2.63 | 2.50–2.83 | 4.01 | 2.96–6.34 |
| Penta-3/OPV-3/PCV-3 | 3.68 | 3.48–3.88 | 6.51 | 4.67–9.99 | 5.82 | 4.54–8.32 | 7.56 | 5.16–11.57 | 3.72 | 3.55–3.91 | 6.15 | 4.37–9.60 |
| Measles-1 | 9.14 | 9.01–9.34 | 10.42 | 9.44–12.59 | 10.16 | 9.34–11.64 | 10.91 | 9.66–13.77 | 9.17 | 9.04–9.40 | 10.26 | 9.34–12.36 |
| Measles-2 | 15.15 | 15.02–15.39 | 16.60 | 15.48–18.44 | 16.50 | 15.45–18.21 | 16.83 | 15.71–18.84 | 15.12 | 15.02–15.38 | 16.40 | 15.35–18.21 |
| n | % | n | % | n | % | n | % | n | % | n | % | |
| Provision of Contact Number | ||||||||||||
| Provided | 380,714 | 12.0 | 2,792,813 | 88.0 | 1,042,478 | 37.3 | 1,399,011 | 50.1 | 351,324 | 12.6 | 3,173,527 | 100.0 |
| Not provided | 184,583 | 3.3 | 5,434,219 | 96.7 | 1,821,695 | 33.5 | 3,211,653 | 59.1 | 400,871 | 7.4 | 5,618,802 | 100.0 |
| Provision of CNIC Numbers | ||||||||||||
| Provided | 109,662 | 14.8 | 629,818 | 85.2 | 250,918 | 39.8 | 283,780 | 45.1 | 95,120 | 15.1 | 739,480 | 100.0 |
| Not provided | 455,635 | 5.7 | 7,597,214 | 94.3 | 2,613,255 | 34.4 | 4,326,884 | 57.0 | 657,075 | 8.6 | 8,052,849 | 100.0 |
| SMS Reminders d | ||||||||||||
| Opted | 195,718 | 3.4 | 5,546,850 | 96.6 | 1,888,981 | 34.1 | 3,250,315 | 58.6 | 407,554 | 7.3 | 5,742,568 | 100.0 |
| Not opted | 363,425 | 12.6 | 2,518,556 | 87.4 | 953,553 | 37.9 | 1,259,358 | 50.0 | 305,645 | 12.1 | 2,881,981 | 100.0 |
| 6 Months | 12 Months | 18 Months | 23 Months | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Non-Defaulter (n = 524,646) | Defaulter (n = 8,136.916) | % Difference | Non-Defaulter (n = 370,589) | Defaulter (n = 7,359,264) | % Difference | Non-Defaulter (n = 298,756) | Defaulter (n = 6,587,052) | % Difference | Non-Defaulter (n = 239,457) | Defaulter (n = 5,713,459) | % Difference | |||||||||
| n | % | n | % | % | n | % | n | % | % | n | % | n | % | % | n | % | n | % | % | |
| BCG | 509,465 | 97.1 | 6,413,184 | 78.8 | 18.3 | 357,525 | 96.5 | 6,246,032 | 84.9 | 11.6 | 286,365 | 95.9 | 5,621,463 | 85.3 | 10.5 | 227,772 | 95.1 | 4,850,521 | 84.9 | 10.2 |
| Penta-1 | 496,998 | 94.7 | 6,083,630 | 74.8 | 20.0 | 358,238 | 96.7 | 6,238,134 | 84.8 | 11.9 | 286,964 | 96.1 | 5,717,622 | 86.8 | 9.3 | 228,181 | 95.3 | 4,973,359 | 87.0 | 8.2 |
| OPV-1 | 496,914 | 94.7 | 6,083,289 | 74.8 | 20.0 | 358,224 | 96.7 | 6,238,586 | 84.8 | 11.9 | 286,961 | 96.1 | 5,717,445 | 86.8 | 9.3 | 228,177 | 95.3 | 4,972,580 | 87.0 | 8.3 |
| PCV-1 | 497,005 | 94.7 | 6,082,373 | 74.8 | 20.0 | 358,241 | 96.7 | 6,236,830 | 84.7 | 11.9 | 286,966 | 96.1 | 5,716,358 | 86.8 | 9.3 | 228,182 | 95.3 | 4,972,040 | 87.0 | 8.3 |
| Rota-1 | 496,778 | 94.7 | 6,052,002 | 74.4 | 20.3 | 357,790 | 96.5 | 6,177,910 | 83.9 | 12.6 | 286,524 | 95.9 | 5,645,399 | 85.7 | 10.2 | 227,757 | 95.1 | 4,895,953 | 85.7 | 9.4 |
| Penta-2 | 486,546 | 92.7 | 4,573,545 | 56.2 | 36.5 | 356,106 | 96.1 | 5,461,257 | 74.2 | 21.9 | 284,963 | 95.4 | 5,215,593 | 79.2 | 16.2 | 226,318 | 94.5 | 4,595,966 | 80.4 | 14.1 |
| OPV-2 | 486,467 | 92.7 | 4,573,404 | 56.2 | 36.5 | 356,109 | 96.1 | 5,461,734 | 74.2 | 21.9 | 284,971 | 95.4 | 5,216,056 | 79.2 | 16.2 | 226,331 | 94.5 | 4,596,043 | 80.4 | 14.1 |
| PCV-2 | 486,560 | 92.7 | 4,573,617 | 56.2 | 36.5 | 356,115 | 96.1 | 5,461,147 | 74.2 | 21.9 | 284,970 | 95.4 | 5,215,220 | 79.2 | 16.2 | 226,323 | 94.5 | 4,595,460 | 80.4 | 14.1 |
| Rota-2 | 478,787 | 91.3 | 4,364,763 | 53.6 | 37.6 | 350,337 | 94.5 | 5,156,110 | 70.1 | 24.5 | 280,085 | 93.8 | 4,888,073 | 74.2 | 19.5 | 222,177 | 92.8 | 4,277,523 | 74.9 | 17.9 |
| Penta-3 | 476,787 | 90.9 | 2,798,437 | 34.4 | 56.5 | 353,051 | 95.3 | 4,749,004 | 64.5 | 30.7 | 282,117 | 94.4 | 4,840,118 | 73.5 | 21.0 | 223,696 | 93.4 | 4,379,560 | 76.7 | 16.8 |
| OPV-3 | 476,572 | 90.8 | 2,796,202 | 34.4 | 56.5 | 352,965 | 95.2 | 4,748,636 | 64.5 | 30.7 | 282,097 | 94.4 | 4,840,010 | 73.5 | 20.9 | 223,699 | 93.4 | 4,379,322 | 76.6 | 16.8 |
| PCV-3 | 476,789 | 90.9 | 2,797,519 | 34.4 | 56.5 | 353,053 | 95.3 | 4,748,864 | 64.5 | 30.7 | 282,118 | 94.4 | 4,839,417 | 73.5 | 21.0 | 223,703 | 93.4 | 4,378,584 | 76.6 | 16.8 |
| IPV-1 | 476,449 | 90.8 | 3,222,400 | 39.6 | 51.2 | 356,352 | 96.2 | 5,165,548 | 70.2 | 26.0 | 285,615 | 95.6 | 5,171,670 | 78.5 | 17.1 | 226,618 | 94.6 | 4,652,844 | 81.4 | 13.2 |
| Measles-1 | - | - | - | 354,290 | 95.6 | 4,063,989 | 55.2 | 40.4 | 298,691 | 100.0 | 4,924,282 | 74.8 | 25.2 | 239,400 | 100.0 | 4,647,012 | 81.3 | 18.6 | ||
| Measles-2 | - | - | - | - | 292,492 | 97.9 | 2,870,850 | 43.6 | 54.3 | 239,371 | 100.0 | 3,562,158 | 62.3 | 37.6 | ||||||
| FIC-M1 (without PCV) | - | - | - | - | - | 337,735 | 91.1 | 3,217,929 | 43.7 | 47.4 | 275,289 | 92.1 | 3,882,806 | 58.9 | 33.2 | 217,526 | 90.8 | 3,597,523 | 63.0 | 27.9 |
| FIC-M1 (with PCV) | - | - | - | - | - | 337,704 | 91.1 | 3,215,861 | 43.7 | 47.4 | 275,259 | 92.1 | 3,880,353 | 58.9 | 33.2 | 217,501 | 90.8 | 3,595,095 | 62.9 | 27.9 |
| FIC-M1 (with Rota) | - | - | - | - | - | 332,609 | 89.8 | 3,056,236 | 41.5 | 48.2 | 270,695 | 90.6 | 3,658,846 | 55.5 | 35.1 | 213,654 | 89.2 | 3,365,367 | 58.9 | 30.3 |
| FIC-M2 (without PCV) | - | - | - | - | - | - | - | - | - | - | 269,404 | 90.2 | 2,419,314 | 36.7 | 53.4 | 217,499 | 90.8 | 2,896,691 | 50.7 | 40.1 |
| FIC-M2 (with PCV) | - | - | - | - | - | - | - | - | - | - | 269,375 | 90.2 | 2,418,189 | 36.7 | 53.5 | 217,474 | 90.8 | 2,895,013 | 50.7 | 40.1 |
| FIC-M2 (with Rota) | - | - | - | - | - | - | - | - | - | - | 264,908 | 88.7 | 2,298,038 | 34.9 | 53.8 | 213,627 | 89.2 | 2,725,456 | 47.7 | 41.5 |
| Periods | Defaulters | Coverage Status | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Total Due | Fully Covered Defaulters | Partially Covered Defaulters | Uncovered Defaulters | ||||||
| n | n | % | n | % | n | % | n | % | |
| Pre-1st lockdown (1 January 2018–22 March 2020) | 1,001,803 | 958,287 | 95.66 | 225,115 | 23.49 | 569,603 | 59.44 | 163,569 | 17.07 |
| 1st national lockdown (23 March–9 May 2020) | 794,645 | 767,891 | 96.63 | 236,656 | 30.82 | 452,945 | 58.99 | 78,290 | 10.20 |
| Post-1st lockdown (10 May–18 June 2020) | 292,520 | 282,137 | 96.45 | 84,522 | 29.96 | 166,588 | 59.05 | 31,027 | 11.00 |
| Smart lockdown (19 June–9 August 2020) | 675,805 | 649,408 | 96.09 | 190,539 | 29.34 | 397,387 | 61.19 | 61,482 | 9.47 |
| Post-smart lockdown (10 August 2020–8 May 2021) | 1,002,850 | 957,190 | 95.45 | 360,810 | 37.69 | 502,943 | 52.54 | 93,437 | 9.76 |
| 2nd lockdown (9–16 May 2021) | 120,872 | 117,801 | 97.46 | 39,569 | 33.59 | 71,451 | 60.65 | 6781 | 5.76 |
| Restrictions (17 May–6 June 2021) | 326,215 | 315,687 | 96.77 | 107,242 | 33.97 | 188,637 | 59.75 | 19,808 | 6.27 |
| Post-restrictions (7 June–31 July 2021) | 182,397 | 175,743 | 96.35 | 65,128 | 37.06 | 100,712 | 57.31 | 9903 | 5.63 |
| 3rd lockdown (1–8 August 2021) | 120,094 | 114,856 | 95.64 | 44,079 | 38.38 | 64,200 | 55.90 | 6577 | 5.73 |
| Post-3rd lockdown 9 August 2021–30 June 2022) | 822,703 | 787,918 | 95.77 | 307,842 | 39.07 | 437,818 | 55.57 | 42,258 | 5.36 |
| Floods (1 July–31 August 2022) | 1,044,658 | 995,875 | 95.33 | 331,506 | 33.29 | 607,684 | 61.02 | 56,685 | 5.69 |
| Post-flood (1 September–31 December 2022) | 652,128 | 604,522 | 92.70 | 258,841 | 42.82 | 304,120 | 50.31 | 41,561 | 6.88 |
| Pandemic last duration (1 January–5 May 2023) | 582,728 | 533,155 | 91.49 | 223,676 | 41.95 | 274,073 | 51.41 | 35,406 | 6.64 |
| Post-pandemic (6 May 2023–19 March 2024) | 1,172,884 | 966,562 | 82.41 | 388,648 | 40.21 | 472,503 | 48.88 | 105,411 | 10.91 |
| Total | 8,792,302 | 8,227,032 | 93.57 | 2,864,173 | 34.81 | 4,610,664 | 56.04 | 752,195 | 9.14 |
| Predictor | Multivariable Analysis | |||||||
|---|---|---|---|---|---|---|---|---|
| Uncovered Defaulters vs. Immunized Children (n = 8,792,392) | Uncovered Defaulters vs. Immunized Children (n = 1,434,185) | |||||||
| OR | SE | Confidence Interval | OR | SE | Confidence Interval | |||
| Sex | ||||||||
| Female | 0.99 *** | 0.002 | 0.99 | 1.00 | 0.99 ** | 0.006 | 0.98 | 1.00 |
| Male | Ref | Ref | ||||||
| Place of Birth | ||||||||
| Maternity Home | 0.72 *** | 0.007 | 0.71 | 0.73 | 0.81 *** | 0.010 | 0.79 | 0.83 |
| Home | 0.54 *** | 0.003 | 0.53 | 0.54 | 0.83 *** | 0.006 | 0.82 | 0.84 |
| Hospital | Ref | Ref | ||||||
| Residential area | ||||||||
| Remote Rural | 0.60 *** | 0.006 | 0.59 | 0.62 | 0.80 *** | 0.014 | 0.78 | 0.83 |
| Urban | 2.61 *** | 0.008 | 2.59 | 2.62 | 1.54 *** | 0.011 | 1.52 | 1.56 |
| Non-Remote Rural | Ref | Ref | ||||||
| Enrollment modality | ||||||||
| Fixed | 3.17 *** | 0.010 | 3.15 | 3.19 | 2.11 *** | 0.018 | 2.08 | 2.15 |
| EOA | 0.86 *** | 0.005 | 0.85 | 0.87 | 0.69 *** | 0.013 | 0.67 | 0.72 |
| Van | 1.09 *** | 0.019 | 1.05 | 1.13 | 1.41 ** | 0.162 | 1.13 | 1.77 |
| Outreach | Ref | Ref | ||||||
| Mother’s Education (in years) | ||||||||
| 0 | 0.36 *** | 0.004 | 0.35 | 0.37 | 0.72 *** | 0.009 | 0.71 | 0.74 |
| 1–5 | 0.43 *** | 0.005 | 0.42 | 0.44 | 0.69 *** | 0.008 | 0.68 | 0.71 |
| 6–8 | 0.60 *** | 0.008 | 0.59 | 0.62 | 0.72 *** | 0.011 | 0.70 | 0.74 |
| 9–10 | 0.83 *** | 0.011 | 0.81 | 0.85 | 0.78 *** | 0.011 | 0.76 | 0.81 |
| ≥11 | Ref | Ref | ||||||
| Enrollment Age (months) | ||||||||
| 0–1 | 0.59 *** | 0.005 | 0.58 | 0.60 | 0.83 *** | 0.051 | 0.74 | 0.94 |
| 2–3 | 0.35 *** | 0.003 | 0.34 | 0.35 | 0.46 *** | 0.028 | 0.40 | 0.51 |
| 4–6 | 0.11 *** | 0.001 | 0.11 | 0.11 | 0.13 *** | 0.009 | 0.12 | 0.15 |
| 7–9 | 0.23 *** | 0.003 | 0.23 | 0.24 | 0.27 *** | 0.017 | 0.23 | 0.30 |
| 10–12 | 0.09 *** | 0.001 | 0.09 | 0.09 | 0.09 *** | 0.007 | 0.08 | 0.10 |
| 13–15 | 0.99 | 0.011 | 0.97 | 1.01 | 0.04 *** | 0.006 | 0.03 | 0.06 |
| 16–18 | 0.18 *** | 0.003 | 0.18 | 0.19 | 0.01 *** | 0.004 | 0.01 | 0.03 |
| >18 | Ref | Ref | ||||||
| Provision of Contact Number | ||||||||
| Not provided | 0.62 *** | 0.001 | 0.61 | 0.62 | 0.85 *** | 0.007 | 0.84 | 0.87 |
| Provided | Ref | Ref | ||||||
| Provision of CNIC Numbers | ||||||||
| Not provided | 0.60 *** | 0.002 | 0.60 | 0.61 | 1.03 ** | 0.008 | 1.01 | 1.04 |
| Provided | Ref | Ref | ||||||
| SMS Reminders | ||||||||
| Not opted | 0.64 *** | 0.002 | 0.64 | 0.65 | 1.27 *** | 0.012 | 1.25 | 1.29 |
| Opted | Ref | Ref | ||||||
| Birth Year | ||||||||
| 2019 | 0.67 *** | 0.003 | 0.67 | 0.68 | 0.57 *** | 0.005 | 0.57 | 0.58 |
| 2020 | 0.43 *** | 0.002 | 0.43 | 0.43 | 0.40 *** | 0.004 | 0.39 | 0.41 |
| 2021 | 0.29 *** | 0.001 | 0.29 | 0.29 | 0.25 *** | 0.003 | 0.24 | 0.25 |
| 2022 | 0.31 *** | 0.001 | 0.31 | 0.32 | 0.25 *** | 0.003 | 0.24 | 0.25 |
| 2023 | 0.45 *** | 0.002 | 0.45 | 0.45 | 0.34 *** | 0.005 | 0.33 | 0.34 |
| 2018 | Ref | Ref | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miraj, F.; Iftikhar, S.; Siddique, M.; Dharma, V.K.; Shah, M.T.; Siddiqi, D.A.; Chandir, S. Leveraging Data from a Provincial Electronic Immunization Registry to Analyze Immunization Coverage, Timeliness, and Defaulters Among 8.8 Million Children from the 2018 to 2023 Birth Cohorts in Sindh Province, Pakistan. Vaccines 2024, 12, 1327. https://doi.org/10.3390/vaccines12121327
Miraj F, Iftikhar S, Siddique M, Dharma VK, Shah MT, Siddiqi DA, Chandir S. Leveraging Data from a Provincial Electronic Immunization Registry to Analyze Immunization Coverage, Timeliness, and Defaulters Among 8.8 Million Children from the 2018 to 2023 Birth Cohorts in Sindh Province, Pakistan. Vaccines. 2024; 12(12):1327. https://doi.org/10.3390/vaccines12121327
Chicago/Turabian StyleMiraj, Fatima, Sundus Iftikhar, Muhammad Siddique, Vijay Kumar Dharma, Mubarak Taighoon Shah, Danya Arif Siddiqi, and Subhash Chandir. 2024. "Leveraging Data from a Provincial Electronic Immunization Registry to Analyze Immunization Coverage, Timeliness, and Defaulters Among 8.8 Million Children from the 2018 to 2023 Birth Cohorts in Sindh Province, Pakistan" Vaccines 12, no. 12: 1327. https://doi.org/10.3390/vaccines12121327
APA StyleMiraj, F., Iftikhar, S., Siddique, M., Dharma, V. K., Shah, M. T., Siddiqi, D. A., & Chandir, S. (2024). Leveraging Data from a Provincial Electronic Immunization Registry to Analyze Immunization Coverage, Timeliness, and Defaulters Among 8.8 Million Children from the 2018 to 2023 Birth Cohorts in Sindh Province, Pakistan. Vaccines, 12(12), 1327. https://doi.org/10.3390/vaccines12121327






