Development and Assessment of a Six-Item Index to Gauge Motivation to Receive COVID-19 Vaccination
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Data Collection
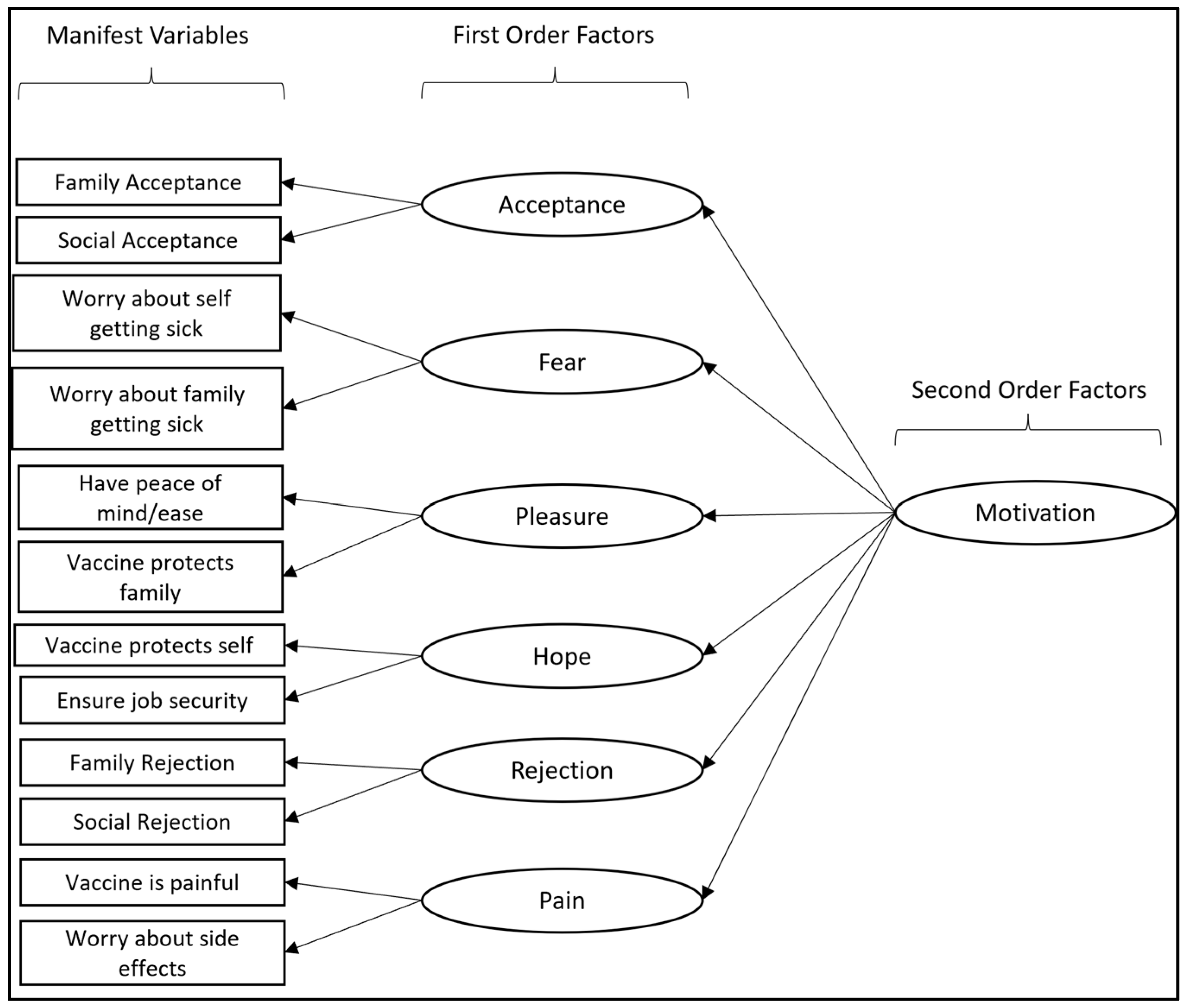
2.2. Motivation Index Development
2.3. Data Analysis
3. Results
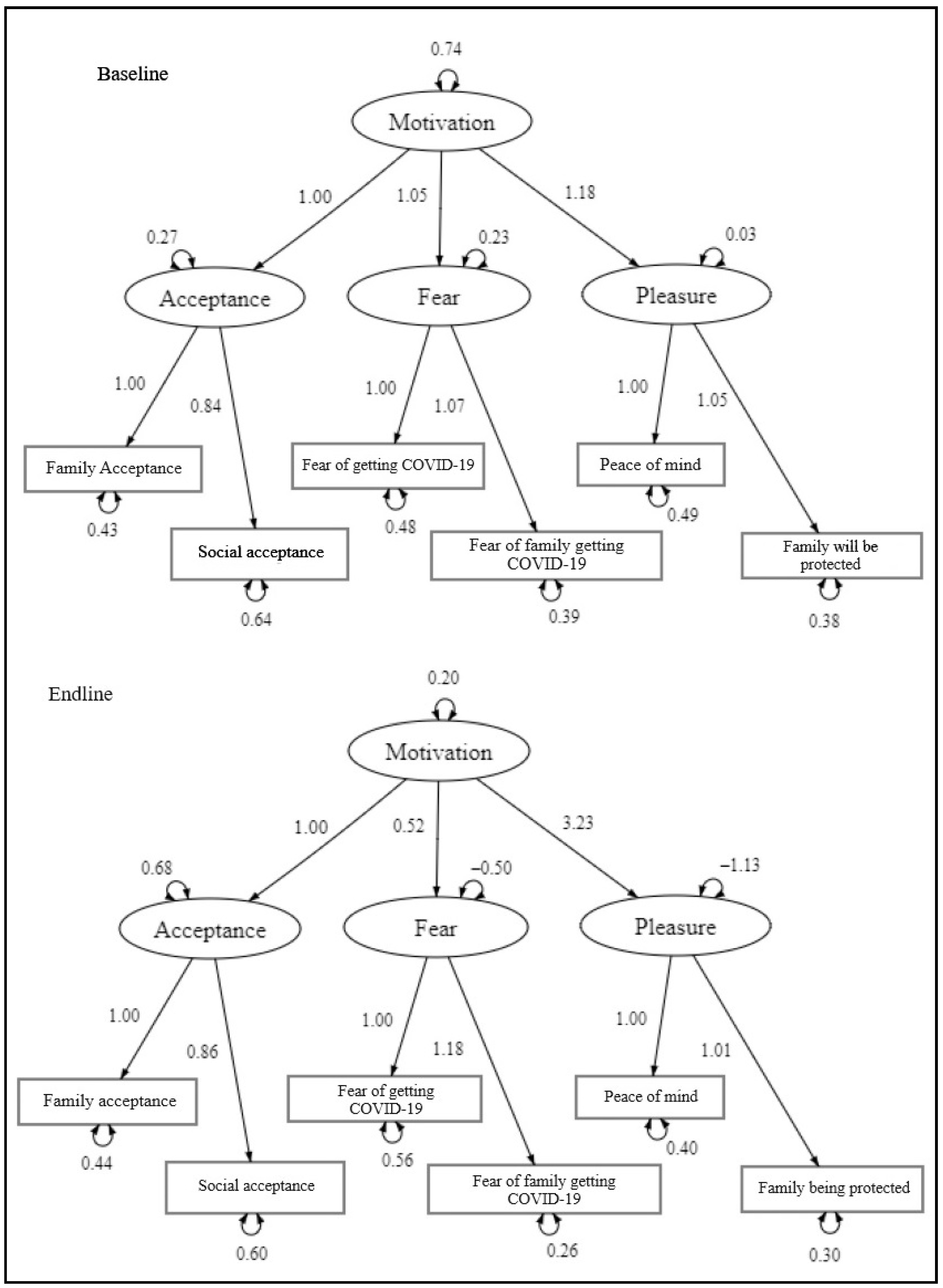
Assessment of Motivation Index
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/?mapFilter=vaccinations (accessed on 27 September 2023).
- Watson, O.J.; Barnsley, G.; Toor, J.; Hogan, A.B.; Winskill, P.; Ghani, A.C. Global impact of the first year of COVID-19 vaccination: A mathematical modelling study. Lancet Infect. Dis. 2022, 22, 1293–1302. [Google Scholar] [CrossRef] [PubMed]
- Sato, R. Vaccine hesitancy against COVID-19 vaccine over time in Nigeria. Vaccine 2023, 41, 2749–2753. [Google Scholar] [CrossRef] [PubMed]
- Fridman, A.; Gershon, R.; Gneezy, A. COVID-19 and vaccine hesitancy: A longitudinal study. PLoS ONE 2021, 16, e0250123. [Google Scholar] [CrossRef] [PubMed]
- Parthasarathi, A.; Puvvada, R.K.; Basappa, S.; Krishna, M.T.; Mahesh, P.A. Global intention of the general public to undergo COVID-19 vaccination: Time trends and risk factors for vaccine refusal, a Systematic Review and Meta-analysis. Wellcome Open Res. 2022, 7, 17. [Google Scholar] [CrossRef]
- Roy, D.N.; Biswas, M.; Islam, E.; Azam, S. Potential factors influencing COVID-19 vaccine acceptance and hesitancy: A systematic review. PLoS ONE 2022, 17, e0265496. [Google Scholar] [CrossRef] [PubMed]
- Faye, S.L.B.; Krumkamp, R.; Doumbia, S.; Tounkara, M.; Strauss, R.; Ouedraogo, H.G.; Sagna, T.; Barry, A.M.; Mbawah, A.K.; Doumbia, C.O.; et al. Factors influencing hesitancy towards adult and child COVID-19 vaccines in rural and urban West Africa: A cross-sectional study. BMJ Open 2022, 12, e059138. [Google Scholar] [CrossRef] [PubMed]
- Gerretsen, P.; Kim, J.; Caravaggio, F.; Quilty, L.; Sanches, M.; Wells, S.; Brown, E.E.; Agic, B.; Pollock, B.G.; Graff-Guerrero, A. Individual determinants of COVID-19 vaccine hesitancy. PLoS ONE 2021, 16, e0258462. [Google Scholar] [CrossRef] [PubMed]
- Ackah, B.B.B.; Woo, M.; Stallwood, L.; Fazal, Z.A.; Okpani, A.; Ukah, U.V.; Adu, P.A. COVID-19 vaccine hesitancy in Africa: A scoping review. Glob. Health Res. Policy 2022, 7, 21. [Google Scholar] [CrossRef]
- Zewude, B.; Habtegiorgis, T. Willingness to Take COVID-19 Vaccine Among People Most at Risk of Exposure in Southern Ethiopia. Pragmatic Obs. Res. 2021, 12, 37–47. [Google Scholar] [CrossRef]
- Mohammed, R.; Nguse, T.M.; Habte, B.M.; Fentie, A.M.; Gebretekle, G.B. COVID-19 vaccine hesitancy among Ethiopian healthcare workers. PLoS ONE 2021, 16, e0261125. [Google Scholar] [CrossRef]
- Iliyasu, Z.; Umar, A.A.; Abdullahi, H.M.; Kwaku, A.A.; Amole, T.G.; Tsiga-Ahmed, F.I.; Garba, R.M.; Salihu, H.M.; Aliyu, M.H. “They have produced a vaccine, but we doubt if COVID-19 exists”: Correlates of COVID-19 vaccine acceptability among adults in Kano, Nigeria. Hum. Vaccines Immunother. 2021, 17, 4057–4064. [Google Scholar] [CrossRef] [PubMed]
- Adebisi, Y.A.; Alaran, A.J.; Bolarinwa, O.A.; Akande-Sholabi, W.; Iii, D.E.L.-P. When it is available, will we take it? Social media users’ perception of hypothetical COVID-19 vaccine in Nigeria. Pan Afr. Med. J. 2021, 38, 230. [Google Scholar] [CrossRef] [PubMed]
- Carcelen, A.C.; Prosperi, C.; Mutembo, S.; Chongwe, G.; Mwansa, F.D.; Ndubani, P.; Simulundu, E.; Chilumba, I.; Musukwa, G.; Thuma, P.; et al. COVID-19 vaccine hesitancy in Zambia: A glimpse at the possible challenges ahead for COVID-19 vaccination rollout in sub-Saharan Africa. Hum. Vaccines Immunother. 2021, 18, 1–6. [Google Scholar] [CrossRef]
- Wang, Y.; Liu, Y. Multilevel determinants of COVID-19 vaccination hesitancy in the United States: A rapid systematic review. Prev. Med. Rep. 2021, 25, 101673. [Google Scholar] [CrossRef] [PubMed]
- Eze, U.A.; Ndoh, K.I.; Ibisola, B.A.; Onwuliri, C.D.; Osiyemi, A.; Ude, N.; Chime, A.; Ogbor, E.O.; Alao, A.O.; Abdullahi, A. Determinants for Acceptance of COVID-19 Vaccine in Nigeria. Cureus 2021, 13, e19801. [Google Scholar] [CrossRef]
- Glanz, K.; Rimer, B.K.; Lewis, F.M. Theory, Research, and Practice in Health Behavior and Health Education. In Health Behavior and Health Education: Theory, Research, and Practice, 3rd ed.; Glanz, K., Rimer, B.K., Lewis, F.M., Eds.; Jossey-Bass: San Francisco, CA, USA, 2008; pp. 22–39. [Google Scholar]
- Painter, J.E.; Borba, C.P.C.; Hynes, M.; Mays, D.; Glanz, K. The Use of Theory in Health Behavior Research from 2000 to 2005: A Systematic Review. Ann. Behav. Med. 2008, 35, 358–362. [Google Scholar] [CrossRef] [PubMed]
- Boateng, G.O.; Neilands, T.B.; Frongillo, E.A.; Melgar-Quiñonez, H.R.; Young, S.L. Best Practices for Developing and Validating Scales for Health, Social, and Behavioral Research: A Primer. Front. Public Health 2018, 6, 149. [Google Scholar] [CrossRef]
- Pedersen, B.; Thanel, K.; Kouakou, A.Y.; Zo, J.R.; Ouattara, M.L.; Gbeke, D.; Thompson, G.; Agha, S. Identifying Drivers of COVID-19 Vaccine Uptake among Residents of Yopougon Est, Abidjan, Côte d’Ivoire. Vaccines 2022, 10, 2101. [Google Scholar] [CrossRef]
- Fogg, B. A behavior model for persuasive design. In Proceedings of the 4th International Conference on Persuasive Technology, Claremont, CA, USA, 26–29 April 2009; Volume 350, pp. 1–7. [Google Scholar] [CrossRef]
- Yuasa, T.; Harada, F.; Shimakawa, H. Proposal to Improve Exercise Using the Fogg Behavior Model. In Proceedings of the 2022 IEEE Asia-Pacific Conference on Computer Science and Data Engineering (CSDE), Gold Coast, Australia, 18–20 December 2022; IEEE: Piscataway, NJ, USA, 2022; pp. 1–4. [Google Scholar] [CrossRef]
- Zhou, Y.; Qin, Q.; Tang, B.; Tian, W. A Study on the Fogg Behavior Model in Designing Educational Apps for Children. In Proceedings of the International Conference on Human-Computer Interaction, Copenhagen, Denmark, 23–28 July 2023; pp. 249–261. [Google Scholar] [CrossRef]
- Akmal, M.; Niwanputri, G.S. Spoonful: Mobile Application for Reducing Household Food Waste using Fogg Behavior Model (FBM). In Proceedings of the 2021 International Conference on Data and Software Engineering (ICoDSE), Bandung, Indonesia, 3–4 November 2021; IEEE: Piscataway, NJ, USA, 2021; pp. 1–6. [Google Scholar] [CrossRef]
- Meekers, D.; Onuoha, C.; Olutola, O. Applying the Fogg Behavior Model to improve contraceptive social marketing during the COVID-19 lockdown in Nigeria: A case study. Gates Open Res. 2020, 4, 141. [Google Scholar] [CrossRef]
- Katirayi, L.; Tchendjou, P.; Tchounga, B.; Mbunka, M.; Wicks, M.; Conserve, D.F. Changing attitudes towards HIV testing and treatment among three generations of men in Cameroon: A qualitative analysis using the Fogg Behavior Model. BMC Public Health 2023, 23, 501. [Google Scholar] [CrossRef]
- Evans, W.D.; Bingenheimer, J.B.; Long, M.; Ndiaye, K.; Donati, D.; Rao, N.M.; Akaba, S.; Hoglin, B. Development and Evaluation of an Index to Measure the Ability to Get Vaccinated for COVID-19. Vaccines 2023, 11, 342. [Google Scholar] [CrossRef]
- Agha, S.; Chine, A.; Lalika, M.; Pandey, S.; Seth, A.; Wiyeh, A.; Seng, A.; Rao, N.; Badshah, A. Drivers of COVID-19 Vaccine Uptake amongst Healthcare Workers (HCWs) in Nigeria. Vaccines 2021, 9, 1162. [Google Scholar] [CrossRef]
- McArdle, J.J. Current Directions in Structural Factor Analysis. Curr. Dir. Psychol. Sci. 1996, 5, 11–18. [Google Scholar] [CrossRef]
- Bollen, K.A. Structural Equations with Latent Variables; Wiley: Hoboken, NJ, USA, 1989. [Google Scholar] [CrossRef]
- Gamst, G.; Meyers, L.S.; Burke, H.M.; Guarino, A.J. Scale Development and Validation. In Public Health Research Methods; Guest, G., Namey, E.E., Eds.; SAGE: Thousand Oaks, CA, USA, 2014; pp. 379–409. [Google Scholar]
- Levine, T.R. Confirmatory Factor Analysis and Scale Validation in Communication Research. Commun. Res. Rep. 2005, 22, 335–338. [Google Scholar] [CrossRef]
- Cronbach, L.J. Coefficient alpha and internal structure of tests. Psychometrika 1951, 16, 297–334. [Google Scholar] [CrossRef]
- R: The R Project for Statistical Computing. Available online: https://www.r-project.org/ (accessed on 26 September 2023).
- Thompson, G.; Yao Kouakou, A.; Nicholes, S.; Ouattara, M.L.; Dorgeles, G.; Mujinga, M.; Thanel, K.; Martinez, A.; Agha, S.; Pedersen, B. Quantitative Model of Factors that Drive COVID-19 Vaccination Uptake: Testing the Fogg Behavioral Model Motivation, Ability and Prompt Constructs and Their Interaction. 2023. Unpublished manuscript, last modified 29 September 2023. Microsoft Word file.
- Byrne, B.M. Structural Equation Modeling with AMOS; Routledge: London, UK, 2016. [Google Scholar] [CrossRef]
| Items |
|---|
| Acceptance |
| 1. My family wants me to get vaccinated against COVID-19. |
| 2. Getting vaccinated against COVID-19 would make me feel more accepted by the people around me. |
| Rejection |
| 3. My family would be angry with me if I got vaccinated against COVID-19. |
| 4. Most of the people I know would think poorly of me if I were to get a COVID-19 vaccine. |
| Hope |
| 5. Getting vaccinated against COVID-19 would protect me from getting sick. |
| 6. Getting vaccinated against COVID-19 would allow me to keep my job. |
| Fear |
| 7. I worry about getting ill from COVID-19. |
| 8. I worry about COVID-19 infecting someone in my family. |
| Pleasure |
| 9. I would feel more at ease everyday if I were vaccinated against COVID-19. |
| 10. It would make me feel good knowing that I am protecting my family by getting vaccinated against COVID-19. |
| Pain |
| 11. I worry that the COVID-19 vaccine will make me sick. |
| 12. I worry that the needlestick for the COVID-19 vaccine will be painful. |
| Variable | nbaseline | % | nendline | % | ntotal |
|---|---|---|---|---|---|
| Location | |||||
| Yopougon Est, Abidjan, CI | 601 | 54.53% | 560 | 52.79% | 1161 |
| Kinshasa, DRC | 512 | 45.47% | 500 | 47.21% | 1012 |
| Age | |||||
| 18–24 years | 266 | 23.90% | 213 | 20.09% | 479 |
| 25–29 years | 223 | 20.04% | 213 | 20.09% | 436 |
| 30–34 years | 175 | 15.72% | 140 | 13.21% | 315 |
| 35–39 years | 139 | 12.49% | 147 | 13.87% | 286 |
| 40–44 years | 130 | 11.68% | 137 | 12.92% | 267 |
| 45–54 years | 157 | 14.11% | 125 | 11.79% | 282 |
| 55+ years | 21 | 1.89% | 85 | 8.02% | 106 |
| Sex | |||||
| Female | 555 | 49.87% | 477 | 45.00% | 1032 |
| Male | 558 | 50.13% | 583 | 55.00% | 1141 |
| Education | |||||
| No formal education | 55 | 4.94% | 63 | 5.95% | 118 |
| Secondary, no diploma | 94 | 8.45% | 60 | 5.67% | 154 |
| Secondary | 150 | 13.48% | 162 | 15.30% | 312 |
| Technical training | 179 | 16.08% | 181 | 17.09% | 360 |
| Professional qualification | 21 | 1.89% | 36 | 3.40% | 57 |
| Current student, e.g., university | 82 | 7.37% | 91 | 8.59% | 173 |
| Tertiary | 431 | 38.72% | 412 | 38.90% | 843 |
| Skip/Do not know | 101 | 9.07% | 54 | 5.10% | 155 |
| Employment | |||||
| Unemployed | 88 | 7.91% | 76 | 7.18% | 164 |
| Student | 159 | 14.29% | 149 | 14.07% | 308 |
| Retired | 19 | 1.71% | 31 | 2.93% | 50 |
| Stay-at-home parent | 53 | 4.76% | 45 | 4.25% | 98 |
| Business owner | 53 | 4.76% | 63 | 5.95% | 116 |
| Independent/self-employed | 169 | 15.18% | 206 | 19.45% | 375 |
| Part-time | 118 | 10.60% | 165 | 15.58% | 283 |
| Full-time | 275 | 24.71% | 263 | 24.83% | 538 |
| Skip/Do not know | 179 | 16.08% | 61 | 5.76% | 240 |
| Marital Status | |||||
| Single | 178 | 15.99% | 184 | 17.37% | 362 |
| Boyfriend/girlfriend | 292 | 26.24% | 283 | 26.72% | 575 |
| Partnered | 252 | 22.64% | 225 | 21.25% | 477 |
| Married | 251 | 22.55% | 304 | 28.71% | 555 |
| Skip/Do not know | 140 | 12.58% | 63 | 5.95% | 203 |
| Religious Affiliation | |||||
| Catholic | 304 | 27.31% | 281 | 26.53% | 585 |
| Evangelical | 231 | 20.75% | 206 | 19.45% | 437 |
| Methodist | 121 | 10.87% | 122 | 11.52% | 243 |
| Protestant | 175 | 15.72% | 144 | 13.60% | 319 |
| Christian (Other) | 75 | 6.74% | 92 | 8.69% | 167 |
| Muslim | 153 | 13.75% | 137 | 12.94% | 290 |
| Traditional African Religion | 33 | 2.96% | 29 | 2.74% | 62 |
| Other | 12 | 1.08% | 17 | 1.61% | 29 |
| Skip/Do not know | 9 | 0.81% | 31 | 2.93% | 40 |
| Vaccination Status | |||||
| Not vaccinated | 679 | 61.00% | 427 | 40.28% | 1106 |
| Vaccinated | 434 | 39.00% | 633 | 59.72% | 1067 |
| Second Order CFA for Motivation | Baseline | Endline | |||
|---|---|---|---|---|---|
| λ 1 | Std | λ 1 | Std | ||
| First Order Loadings | |||||
| Factors | Items | ||||
| Acceptance | 1. My family wants me to get vaccinated against COVID-19. | 1.00 | 0.84 | 1.00 | 0.82 |
| 2. Getting vaccinated against COVID-19 would make me feel more accepted by the people around me. | 0.84 | 0.72 | 0.86 | 0.72 | |
| Fear | 7. I worry about getting ill from COVID-19. | 1.00 | 0.83 | 1.00 | 0.71 |
| 8. I worry about COVID-19 infecting someone in my family. | 1.69 | 0.87 | 1.18 | 0.86 | |
| Pleasure | 9. I would feel more at ease everyday if I were vaccinated against COVID-19. | 1.00 | 0.83 | 1.00 | 0.84 |
| 10. It would make me feel good knowing that I am protecting my family by getting vaccinated against COVID-19. | 1.05 | 0.87 | 1.01 | 0.87 | |
| Second Order Loadings | |||||
| Motivation | Acceptance | 1.00 | 0.86 | 1.00 | 0.47 |
| Fear | 1.06 | 0.89 | 0.52 | 0.31 | |
| Pleasure | 1.18 | 0.99 | 3.23 | 1.50 | |
| Timepoint | Cronbach’s Alpha | CLI | TLI | RMSEA | SRMS | χ2 | df | p 1 |
|---|---|---|---|---|---|---|---|---|
| Baseline | 0.89 | 0.990 | 0.975 | 0.074 | 0.018 | 42.823 | 6 | *** |
| Endline | 0.77 | 0.996 | 0.989 | 0.040 | 0.011 | 16.126 | 6 | * |
| Items |
|---|
| Acceptance |
| 1. My family wants me to get vaccinated against COVID-19. |
| 2. Getting vaccinated against COVID-19 would make me feel more accepted by the people around me. |
| Fear |
| 3. I worry about getting ill from COVID-19. |
| 4. I worry about COVID-19 infecting someone in my family. |
| Pleasure |
| 5. I would feel more at ease everyday if I were vaccinated against COVID-19. |
| 6. It would make me feel good knowing that I am protecting my family by getting vaccinated against COVID-19. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pedersen, B.; Thompson, G.; Kouakou, A.Y.; Mujinga, M.; Nicholes, S.; Martinez, A.; Agha, S.; Thanel, K.; Ouattara, M.L.; Gbeke, D.; et al. Development and Assessment of a Six-Item Index to Gauge Motivation to Receive COVID-19 Vaccination. Vaccines 2024, 12, 6. https://doi.org/10.3390/vaccines12010006
Pedersen B, Thompson G, Kouakou AY, Mujinga M, Nicholes S, Martinez A, Agha S, Thanel K, Ouattara ML, Gbeke D, et al. Development and Assessment of a Six-Item Index to Gauge Motivation to Receive COVID-19 Vaccination. Vaccines. 2024; 12(1):6. https://doi.org/10.3390/vaccines12010006
Chicago/Turabian StylePedersen, Brian, Gretchen Thompson, Albert Yao Kouakou, Marie Mujinga, Samuel Nicholes, Andres Martinez, Sohail Agha, Katherine Thanel, Mariame Louise Ouattara, Dorgeles Gbeke, and et al. 2024. "Development and Assessment of a Six-Item Index to Gauge Motivation to Receive COVID-19 Vaccination" Vaccines 12, no. 1: 6. https://doi.org/10.3390/vaccines12010006
APA StylePedersen, B., Thompson, G., Kouakou, A. Y., Mujinga, M., Nicholes, S., Martinez, A., Agha, S., Thanel, K., Ouattara, M. L., Gbeke, D., & Burke, H. M. (2024). Development and Assessment of a Six-Item Index to Gauge Motivation to Receive COVID-19 Vaccination. Vaccines, 12(1), 6. https://doi.org/10.3390/vaccines12010006






