Are People Willing to Take Regular COVID-19 Vaccines? Prevalence and Determinants of Hesitancy for Regular COVID-19 Vaccination: A Random Population-Based Survey in Hong Kong
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Sample, and Ethical Considerations
2.2. Data Collection
2.3. Measures
2.4. Data Analysis
3. Results
3.1. Participant Characteristics
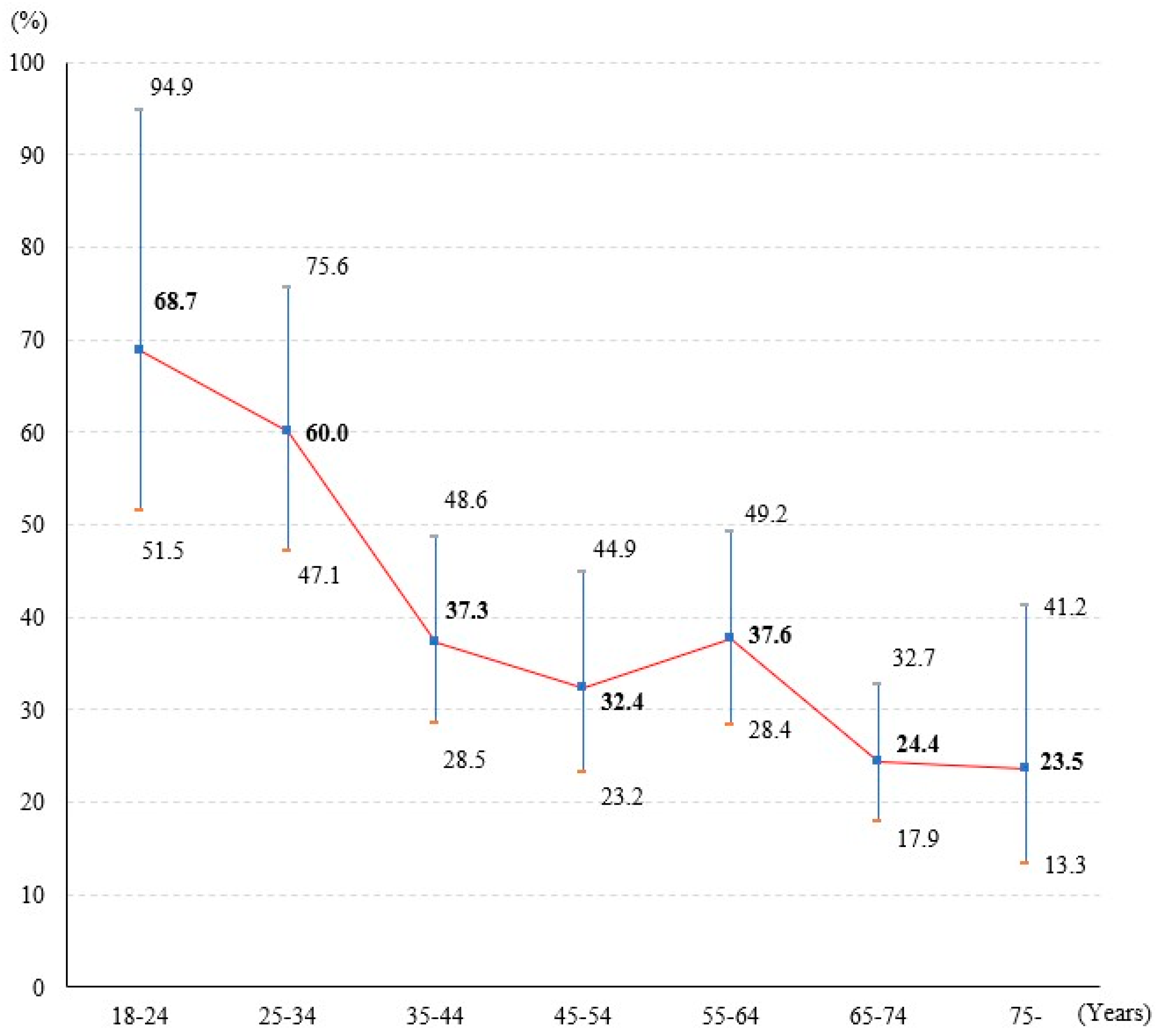
3.2. Hesitancy of Regular COVID-19 Vaccination
3.3. Determinants of Hesitancy for Regular COVID-19 Vaccination
3.3.1. Bivariate Analysis
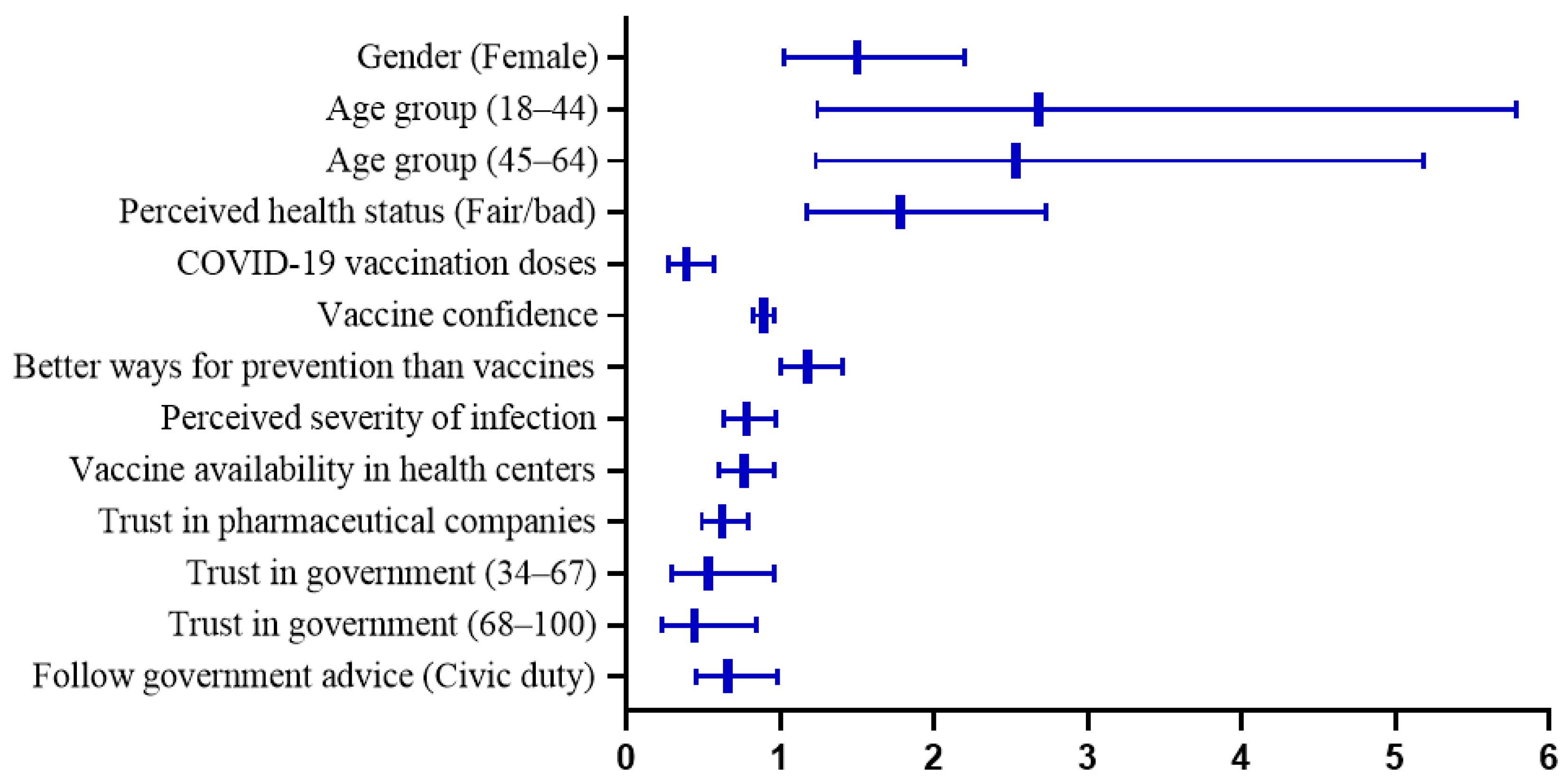
3.3.2. Multivariate Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mogharab, V.; Ostovar, M.; Ruszkowski, J.; Hussain, S.Z.M.; Shrestha, R.; Yaqoob, U.; Aryanpoor, P.; Nikkhoo, A.M.; Heidari, P.; Jahromi, A.R.; et al. Global burden of the COVID-19 associated patient-related delay in emergency healthcare: A panel of systematic review and meta-analyses. Glob. Health 2022, 18, 58. [Google Scholar] [CrossRef] [PubMed]
- Rahmani, K.; Shavaleh, R.; Forouhi, M.; Disfani, H.F.; Kamandi, M.; Oskooi, R.K.; Foogerdi, M.; Soltani, M.; Rahchamani, M.; Mohaddespour, M.; et al. The effectiveness of COVID-19 vaccines in reducing the incidence, hospitalization, and mortality from COVID-19: A systematic review and meta-analysis. Front. Public Health 2022, 10, 873596. [Google Scholar] [CrossRef]
- Huang, C.; Yang, L.J.; Pan, J.; Xu, X.M.; Peng, R. Correlation between vaccine coverage and the COVID-19 pandemic throughout the world: Based on real-world data. J. Med. Virol. 2022, 94, 2181–2187. [Google Scholar] [CrossRef] [PubMed]
- Our World in Data. Coronavirus (COVID-19) Vaccinations. Available online: https://ourworldindata.org/covid-vaccinations (accessed on 6 July 2023).
- Weitzer, J.; Birmann, B.M.; Steffelbauer, I.; Bertau, M.; Zenk, L.; Caniglia, G.; Laubichler, M.D.; Steiner, G.; Schernhammer, E.S. Willingness to receive an annual COVID-19 booster vaccine in the German-speaking D-A-CH region in Europe: A cross-sectional study. Lancet Reg. Health Eur. 2022, 18, 100414. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Tracking SARS-CoV-2 Variants. Available online: https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/ (accessed on 23 December 2022).
- The Government of the Hong Kong Special Administrative Region. Statistics on 5th Wave of COVID-19. Available online: https://www.covidvaccine.gov.hk/pdf/5th_wave_statistics.pdf (accessed on 28 December 2022).
- The Government of the Hong Kong Special Administrative Region. Vaccine Pass. Available online: https://www.coronavirus.gov.hk/eng/vaccine-pass.html (accessed on 24 December 2022).
- The Government of the Hong Kong Special Administrative Region. Hong Kong Vaccination Dashboard. Available online: https://www.covidvaccine.gov.hk/zh-HK/dashboard (accessed on 6 July 2023).
- World Health Organization. Ten Threats to Global Health in 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 27 December 2022).
- Rzymski, P.; Poniedzialek, B.; Fal, A. Willingness to Receive the Booster COVID-19 Vaccine Dose in Poland. Vaccines 2021, 9, 1286. [Google Scholar] [CrossRef]
- Pal, S.; Shekhar, R.; Kottewar, S.; Upadhyay, S.; Singh, M.; Pathak, D.; Kapuria, D.; Barrett, E.; Sheikh, A. COVID-19 Vaccine Hesitancy and Attitude toward Booster Doses among US Healthcare Workers. Vaccines 2021, 9, 1358. [Google Scholar] [CrossRef]
- Tung, T.H.; Lin, X.Q.; Chen, Y.; Zhang, M.X.; Zhu, J.S. Willingness to receive a booster dose of inactivated coronavirus disease 2019 vaccine in Taizhou, China. Expert Rev. Vaccines 2022, 21, 261–267. [Google Scholar] [CrossRef]
- Abdelmoneim, S.A.; Sallam, M.; Hafez, D.M.; Elrewany, E.; Mousli, H.M.; Hammad, E.M.; Elkhadry, S.W.; Adam, M.F.; Ghobashy, A.A.; Naguib, M.; et al. COVID-19 Vaccine Booster Dose Acceptance: Systematic Review and Meta-Analysis. Trop. Med. Infect. Dis. 2022, 7, 298. [Google Scholar] [CrossRef]
- Toro-Ascuy, D.; Cifuentes-Munoz, N.; Avaria, A.; Pereira-Montecinos, C.; Cruzat, G.; Peralta-Arancibia, K.; Zorondo-Rodriguez, F.; Fuenzalida, L.F. Factors Influencing the Acceptance of COVID-19 Vaccines in a Country with a High Vaccination Rate. Vaccines 2022, 10, 681. [Google Scholar] [CrossRef]
- Williams, L.; Gallant, A.; Brown, L.; Corrigan, K.; Crowe, K.; Hendry, E. Barriers and facilitators to the future uptake of regular COVID-19 booster vaccinations among young adults in the UK. Hum. Vaccines Immunother. 2022, 18, 2129238. [Google Scholar] [CrossRef]
- Abuhammad, S.; Khabour, O.F.; Alzoubi, K.H.; Hamaideh, S.; Alzoubi, B.A.; Telfah, W.S.; El-Zubi, F.K. The public’s attitude to and acceptance of periodic doses of the COVID-19 vaccine: A survey from Jordan. PLoS ONE 2022, 17, e0271625. [Google Scholar] [CrossRef]
- Schmid, P.; Rauber, D.; Betsch, C.; Lidolt, G.; Denker, M.L. Barriers of Influenza Vaccination Intention and Behavior—A Systematic Review of Influenza Vaccine Hesitancy, 2005–2016. PLoS ONE 2017, 12, e0170550. [Google Scholar] [CrossRef]
- MacDonald, N.E.; The SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Fuller, A.; Hancox, J.; Vedhara, K.; Card, T.; Mallen, C.; Van-Tam, J.S.N.; Abhishek, A. Barriers and facilitators to vaccination uptake against COVID-19, influenza, and pneumococcal pneumonia in immunosuppressed adults with immune-mediated inflammatory diseases: A qualitative interview study during the COVID-19 pandemic. PLoS ONE 2022, 17, e0267769. [Google Scholar] [CrossRef] [PubMed]
- Riad, A.; Pokorna, A.; Antalova, N.; Krobot, M.; Zviadadze, N.; Serdiuk, I.; Koscik, M.; Klugar, M. Prevalence and Drivers of COVID-19 Vaccine Hesitancy among Czech University Students: National Cross-Sectional Study. Vaccines 2021, 9, 948. [Google Scholar] [CrossRef] [PubMed]
- Harapan, H.; Anwar, S.; Yufika, A.; Sharun, K.; Gachabayov, M.; Fahriani, M.; Husnah, M.; Raad, R.; Abdalla, R.Y.A.; Adam, R.Y.; et al. Vaccine hesitancy among communities in ten countries in Asia, Africa, and South America during the COVID-19 pandemic. Pathog. Glob. Health 2022, 116, 236–243. [Google Scholar] [CrossRef] [PubMed]
- Xiao, J.; Cheung, J.K.; Wu, P.; Ni, M.Y.; Cowling, B.J.; Liao, Q. Temporal changes in factors associated with COVID-19 vaccine hesitancy and uptake among adults in Hong Kong: Serial cross-sectional surveys. Lancet Reg. Health West Pac. 2022, 23, 100441. [Google Scholar] [CrossRef]
- Wong, M.C.S.; Wong, E.L.Y.; Huang, J.; Cheung, A.W.L.; Law, K.; Chong, M.K.C.; Ng, R.W.Y.; Lai, C.K.C.; Boon, S.S.; Lau, J.T.F.; et al. Acceptance of the COVID-19 vaccine based on the health belief model: A population-based survey in Hong Kong. Vaccine 2021, 39, 1148–1156. [Google Scholar] [CrossRef]
- Huang, J.; Choi, P.; Pang, T.W.Y.; Chen, X.; Wang, J.; Ding, H.; Jin, Y.; Zheng, Z.J.; Wong, M.C.S. Factors associated with participation in colorectal cancer screening: A population-based study of 7200 individuals. Eur. J. Cancer Care 2021, 30, e13369. [Google Scholar] [CrossRef]
- Tu, S.; Sun, F.Y.; Chantler, T.; Zhang, X.; Jit, M.; Han, K.; Rodewald, L.; Du, F.; Yu, H.; Hou, Z.; et al. Caregiver and service provider vaccine confidence following the Changchun Changsheng vaccine incident in China: A cross-sectional mixed methods study. Vaccine 2020, 38, 6882–6888. [Google Scholar] [CrossRef]
- Kateeb, E.; Danadneh, M.; Pokorna, A.; Klugarova, J.; Abdulqader, H.; Klugar, M.; Riad, A. Predictors of Willingness to Receive COVID-19 Vaccine: Cross-Sectional Study of Palestinian Dental Students. Vaccines 2021, 9, 954. [Google Scholar] [CrossRef] [PubMed]
- Riad, A.; Abdulqader, H.; Morgado, M.; Domnori, S.; Koscik, M.; Mendes, J.J.; Klugar, M.; Kateeb, E.; Iads-Score, O.B.O. Global Prevalence and Drivers of Dental Students’ COVID-19 Vaccine Hesitancy. Vaccines 2021, 9, 566. [Google Scholar] [CrossRef] [PubMed]
- SPSS Inc. IBM SPSS Statistics 28.0.1 Documentation. Available online: https://www.ibm.com/support/pages/ibm-spss-statistics-2801-documentation (accessed on 10 September 2022).
- R Core Team. Index of /src/base/R-4. Available online: https://cran.r-project.org/src/base/R-4/ (accessed on 5 November 2022).
- Census and Statistics Department. Table 1B: Population by Sex and Age. Available online: https://www.censtatd.gov.hk/tc/web_table.html?id=1B (accessed on 6 December 2022).
- Tsang, S.J. Predicting COVID-19 vaccine hesitancy in Hong Kong: Vaccine knowledge, risks from coronavirus, and risks and benefits of vaccination. Vaccine X 2022, 11, 100164. [Google Scholar] [CrossRef] [PubMed]
- Veli, N.M.C.; Woolf, K.; Nazareth, J.; Pan, D.; Al-Oraibi, A.; Baggaley, R.F.; Bryant, L.; Nellums, L.B.; Gray, L.J.; Khunti, K.; et al. Hesitancy for receiving regular SARS-CoV-2 vaccination in UK healthcare workers: A cross-sectional analysis from the UK-REACH study. BMC Med. 2022, 20, 386. [Google Scholar] [CrossRef]
- Kumari, A.; Ranjan, P.; Chopra, S.; Kaur, D.; Kaur, T.; Kalanidhi, K.B.; Goel, A.; Singh, A.; Baitha, U.; Prakash, B.; et al. What Indians Think of the COVID-19 vaccine: A qualitative study comprising focus group discussions and thematic analysis. Diabetes Metab. Synd. 2021, 15, 679–682. [Google Scholar] [CrossRef]
- Department of Health and Social Care. Joint Committee on Vaccination and Immunisation: Interim Advice on Priority Groups for COVID-19 Vaccination. Available online: https://www.gov.uk/government/publications/priority-groups-for-coronavirus-covid-19-vaccination-advice-from-the-jcvi/interim-advice-on-priority-groups-for-covid-19-vaccination (accessed on 29 December 2020).
- Zhang, D.; Zhou, W.; Poon, P.K.; Kwok, K.O.; Chui, T.W.; Hung, P.H.Y.; Ting, B.Y.T.; Chan, D.C.; Wong, S.Y. Vaccine Resistance and Hesitancy among Older Adults Who Live Alone or Only with an Older Partner in Community in the Early Stage of the Fifth Wave of COVID-19 in Hong Kong. Vaccines 2022, 10, 118. [Google Scholar] [CrossRef]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- World Bank. Life Expectancy at Birth, Total (Years). Available online: https://data.worldbank.org/indicator/SP.DYN.LE00.IN (accessed on 10 June 2023).
- Aw, J.; Seah, S.S.Y.; Seng, B.J.J.; Low, L.L. COVID-19-Related Vaccine Hesitancy among Community Hospitals’ Healthcare Workers in Singapore. Vaccines 2022, 10, 537. [Google Scholar] [CrossRef]
- Xu, B.; Zhu, Y. A systematic review and meta-analysis of the factors associating the willingness of Chinese community residents to receive COVID-19 vaccine. Ann. Palliat. Med. 2022, 11, 3483–3493. [Google Scholar] [CrossRef]
- Fu, W.; Sivajohan, B.; McClymont, E.; Albert, A.; Elwood, C.; Ogilvie, G.; Money, D. Systematic review of the safety, immunogenicity, and effectiveness of COVID-19 vaccines in pregnant and lactating individuals and their infants. Int. J. Gynaecol. Obstet. 2022, 156, 406–417. [Google Scholar] [CrossRef]
- Wei, S.Q.; Bilodeau-Bertrand, M.; Liu, S.; Auger, N. The impact of COVID-19 on pregnancy outcomes: A systematic review and meta-analysis. Can. Med Assoc. J. 2021, 193, E540–E548. [Google Scholar] [CrossRef] [PubMed]
- Kirbis, A. The Impact of Socioeconomic Status, Perceived Threat and Healthism on Vaccine Hesitancy. Sustainability 2023, 15, 6107. [Google Scholar] [CrossRef]
- Jennings, W.; Stoker, G.; Bunting, H.; Valgarethsson, V.O.; Gaskell, J.; Devine, D.; McKay, L.; Mills, M.C. Lack of Trust, Conspiracy Beliefs, and Social Media Use Predict COVID-19 Vaccine Hesitancy. Vaccines 2021, 9, 593. [Google Scholar] [CrossRef] [PubMed]
- Abid, M.A.; Buzdar, M.A.; Junejo, S.; Karim, N. Acceptance of COVID-19 Vaccine Among Undergraduate Students. Pak. Armed Forces Med. J. 2023, 73, 595–597. [Google Scholar] [CrossRef]
- Paul, E.; Fancourt, D. Predictors of uncertainty and unwillingness to receive the COVID-19 booster vaccine: An observational study of 22,139 fully vaccinated adults in the UK. Lancet Reg. Health Eur. 2022, 14, 100317. [Google Scholar] [CrossRef] [PubMed]
- Kadoya, Y.; Watanapongvanich, S.; Yuktadatta, P.; Putthinun, P.; Lartey, S.T.; Khan, M.S.R. Willing or Hesitant? A Socioeconomic Study on the Potential Acceptance of COVID-19 Vaccine in Japan. Int. J. Environ. Res. Public Health 2021, 18, 4864. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Li, Q.; Silver Tarimo, C.; Wang, M.; Gu, J.; Wei, W.; Ma, M.; Zhao, L.; Mu, Z.; Miao, Y. COVID-19 Vaccine Hesitancy Among Chinese Population: A Large-Scale National Study. Front. Immunol. 2021, 12, 781161. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.L.; Liu, X.H. Information factors and theoretical explanation of health information avoidance. Psychol. Sci. 2023, 46, 238. [Google Scholar] [CrossRef]
- Alzahrani, S.H.; Baig, M.; Alrabia, M.W.; Algethami, M.R.; Alhamdan, M.M.; Alhakamy, N.A.; Asfour, H.Z.; Ahmad, T. Attitudes toward the SARS-CoV-2 Vaccine: Results from the Saudi Residents’ Intention to Get Vaccinated against COVID-19 (SRIGVAC) Study. Vaccines 2021, 9, 798. [Google Scholar] [CrossRef]
- Huang, Y.Z.; Kuan, C.C. Vaccination to reduce severe COVID-19 and mortality in COVID-19 patients: A systematic review and meta-analysis. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 1770–1776. [Google Scholar] [CrossRef]
- Team, C.-F. Variation in the COVID-19 infection-fatality ratio by age, time, and geography during the pre-vaccine era: A systematic analysis. Lancet 2022, 399, 1469–1488. [Google Scholar] [CrossRef]
- Ye, X.; Ye, W.; Yu, J.; Gao, Y.; Ren, Z.; Chen, L.; Dong, A.; Yi, Q.; Zhan, C.; Lin, Y.; et al. The landscape of COVID-19 vaccination among healthcare workers at the first round of COVID-19 vaccination in China: Willingness, acceptance and self-reported adverse effects. Hum. Vaccin. Immunother. 2021, 17, 4846–4856. [Google Scholar] [CrossRef] [PubMed]
- Kwok, K.O.; Li, K.K.; Wei, W.I.; Tang, A.; Wong, S.Y.S.; Lee, S.S. Editor’s Choice: Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: A survey. Int. J. Nurs. Stud. 2021, 114, 103854. [Google Scholar] [CrossRef] [PubMed]
- Esmaeilzadeh, A.; Maleki, A.J.; Moradi, A.; Siahmansouri, A.; Yavari, M.J.; Karami, P.; Elahi, R. Major severe acute respiratory coronavirus-2 (SARS-CoV-2) vaccine-associated adverse effects; benefits outweigh the risks. Expert. Rev. Vaccines 2022, 21, 1377–1394. [Google Scholar] [CrossRef]
- Hwang, J.K.; Zhang, T.; Wang, A.Z.; Li, Z. COVID-19 vaccines for patients with cancer: Benefits likely outweigh risks. J. Hematol. Oncol. 2021, 14, 38. [Google Scholar] [CrossRef] [PubMed]
- Carmody, E.R.; Zander, D.; Klein, E.J.; Mulligan, M.J.; Caplan, A.L. Knowledge and Attitudes Toward Covid-19 and Vaccines Among a New York Haredi-Orthodox Jewish Community. J. Community Health 2021, 46, 1161–1169. [Google Scholar] [CrossRef]
- Wilson, W.W.; Hatfield, K.M.; Tressler, S.; Bicking Kinsey, C.; Parra, G.; Zell, R.; Denson, A.; Williams, C.; Spicer, K.B.; Kamal-Ahmed, I.; et al. Characteristics of nursing home residents and healthcare personnel with repeated severe acute respiratory coronavirus virus 2 (SARS-CoV-2) tests positive ≥90 days after initial infection: Four US jurisdictions, July 2020–March 2021. Infect. Control. Hosp. Epidemiol. 2022, 44, 809–812. [Google Scholar] [CrossRef]
- Rennert, L.; Ma, Z.; McMahan, C.S.; Dean, D. Effectiveness and protection duration of Covid-19 vaccines and previous infection against any SARS-CoV-2 infection in young adults. Nat. Commun. 2022, 13, 3946. [Google Scholar] [CrossRef]
- Sudre, C.H.; Murray, B.; Varsavsky, T.; Graham, M.S.; Penfold, R.S.; Bowyer, R.C.; Pujol, J.C.; Klaser, K.; Antonelli, M.; Canas, L.S.; et al. Attributes and predictors of long COVID. Nat. Med. 2021, 27, 626–631. [Google Scholar] [CrossRef]
- Ned Pagliarulo, J.G.; Dubnow, S.; Fidler, B. Coronavirus Vaccines Are Rolling out Quickly. Here’s Where the Pipeline Stands. Available online: https://www.biopharmadive.com/news/coronavirus-vaccine-pipeline-types/579122/ (accessed on 1 January 2023).
- Hu, M.; Jia, H.; Xie, Y. Passport to a Mighty Nation: Exploring Sociocultural Foundation of Chinese Public’s Attitude to COVID-19 Vaccine Certificates. Int. J. Environ. Res. Public Health 2021, 18, 10439. [Google Scholar] [CrossRef]
| n | % | n | % | ||
|---|---|---|---|---|---|
| Gender | Education level | ||||
| Male | 571 | 47.1 | Primary or below | 226 | 18.8 |
| Female | 642 | 52.9 | Secondary | 558 | 46.2 |
| College or above | 422 | 35.0 | |||
| Age group | Employment | ||||
| 18–24 | 85 | 8.1 | Unemployed | 587 | 48.6 |
| 25–34 | 144 | 13.7 | Employed | 620 | 51.4 |
| 35–44 | 193 | 18.5 | Health condition | ||
| 45–54 | 164 | 15.7 | Good | 730 | 60.3 |
| 55–64 | 176 | 16.9 | Fair | 407 | 33.6 |
| 65–74 | 190 | 18.2 | bad | 73 | 6.1 |
| ≥75 | 93 | 8.9 | Chronic illness | ||
| Age | No | 834 | 68.8 | ||
| M (P25, P75) | 50 (36, 65) | Yes | 379 | 31.2 | |
| Factors | Regular Vaccination | χ2/Z | p | ||
|---|---|---|---|---|---|
| No/Not Sure | Yes | ||||
| Sociodemographics | |||||
| Gender | Male | 240 (42.2) | 329 (57.8) | 0.311 | 0.577 |
| Female | 281 (43.8) | 361 (56.2) | |||
| Age | 18–44 | 218 (51.7) | 204 (48.3) | 41.661 | <0.001 |
| 45–64 | 127 (37.5) | 212 (62.5) | |||
| ≥65 | 79 (27.9) | 204 (72.1) | |||
| Education level | Primary or below | 71 (31.4) | 155 (68.6) | 28.537 | <0.001 |
| Secondary | 227 (40.8) | 329 (59.2) | |||
| College or above | 221 (52.4) | 201 (47.6) | |||
| Employment | Unemployed | 237 (40.4) | 349 (59.6) | 2.820 | 0.093 |
| Employed | 280 (45.2) | 339 (54.8) | |||
| Health conditions | |||||
| Perceived health status | Good | 208 (38.5) | 448 (61.5) | 14.900 | <0.001 |
| Fair/bad | 239 (49.7) | 242 (50.3) | |||
| Chronic illness | No | 383 (46.0) | 450 (54.0) | 9.728 | 0.002 |
| Yes | 138 (36.4) | 241 (63.6) | |||
| Experiences | |||||
| SARS-CoV-2 infection | No | 342 (41.1) | 491 (58.9) | 8.179 | 0.017 |
| Yes | 152 (45.4) | 183 (54.6) | |||
| Probably | 26 (61.9) | 16 (38.1) | |||
| COVID-19 vaccination doses | Zero | 64 (86.5) | 10 (13.5) | 173.685 | <0.001 |
| One | 42 (67.7) | 20 (32.3) | |||
| Two | 264 (54.8) | 218 (45.2) | |||
| Three | 151 (25.5) | 441 (74.5) | |||
| COVID-19 vaccination side effects | None | 197 (33.7) | 388 (66.3) | 25.939 | <0.001 |
| Mild to moderate | 228 (45.2) | 276 (54.8) | |||
| Moderate to severe | 26 (65.0) | 14 (35.0) | |||
| Flu vaccination | No | 301 (48.9) | 314 (51.1) | 60.632 | <0.001 |
| Yes | 212 (36.4) | 370 (63.6) | |||
| Attitudes | |||||
| Vaccine confidence | 13 (10, 16) | 16 (14, 18) | −15.177 | <0.001 | |
| Better ways for prevention than vaccines | 4 (3, 4) | 3 (2, 4) | 9.665 | <0.001 | |
| Perceived knowledge sufficiency | 3 (3, 4) | 4 (3, 4) | −10.915 | <0.001 | |
| Perceived severity of infection | 2 (2, 3) | 3 (2, 3) | −2.098 | 0.036 | |
| Vaccine availability in health centers | 4 (3, 4) | 4 (4, 5) | −8.618 | <0.001 | |
| Trust in pharmaceutical companies | 3 (2, 4) | 4 (3, 4) | −11.824 | <0.001 | |
| Trust in government | 0–33 | 181 (76.7) | 55 (23.3) | 204.240 | <0.001 |
| 34–67 | 223 (46.9) | 252 (53.1) | |||
| 68–100 | 103 (21.4) | 378 (78.6) | |||
| Follow government advice | Personal choice | 339 (69.9) | 146 (30.1) | 63.675 | <0.001 |
| Civic duty | 302 (46.2) | 352 (53.8) | |||
| Attitude toward new vaccine | First to get | 14 (2.7) | 105 (82.3) | 86.725 | <0.001 |
| Wait and see | 441 (44.0) | 561 (56.0) | |||
| Refuse | 59 (78.7) | 16 (21.3) | |||
| Factors | OR | 95% CI | p | |
|---|---|---|---|---|
| Sociodemographics | ||||
| Gender | Male | Reference | ||
| Female | 1.50 | 1.02–2.20 | 0.040 | |
| Age | ≥65 | Reference | ||
| 45–64 | 2.53 | 1.23–5.18 | 0.011 | |
| 18–44 | 2.68 | 1.24–5.79 | 0.012 | |
| Education level | Primary or below | Reference | ||
| Secondary | 1.41 | 0.70–2.82 | 0.332 | |
| College or above | 1.56 | 0.72–3.37 | 0.258 | |
| Employment | Unemployed | Reference | ||
| Employed | 0.84 | 0.55–1.29 | 0.424 | |
| Health conditions | ||||
| Perceived health status | Good | Reference | ||
| Fair/bad | 1.78 | 1.17–2.73 | 0.008 | |
| Chronic illness | No | Reference | ||
| Yes | 1.21 | 0.73–2.01 | 0.468 | |
| Experiences | ||||
| COVID-19 vaccination doses | 0.39 | 0.27–0.57 | <0.001 | |
| COVID-19 vaccination side effects | None | Reference | ||
| Mild to moderate | 1.07 | 0.72–1.59 | 0.748 | |
| Moderate to severe | 1.63 | 0.40–6.59 | 0.492 | |
| SARS-CoV-2 infection | No | Reference | ||
| Yes | 0.69 | 0.43–1.10 | 0.118 | |
| Flu vaccination | No | Reference | ||
| Yes | 0.76 | 0.52–1.12 | 0.171 | |
| Attitudes | ||||
| Vaccine confidence | 0.89 | 0.82–0.96 | 0.003 | |
| Better ways for prevention than vaccines | 1.18 | 1.00–1.40 | 0.048 | |
| Perceived knowledge sufficiency | 1.05 | 0.82–1.34 | 0.704 | |
| Perceived severity of infection | 0.78 | 0.63–0.97 | 0.026 | |
| Vaccine availability in health centers | 0.76 | 0.60–0.96 | 0.023 | |
| Trust in pharmaceutical companies | 0.62 | 0.49–0.79 | <0.001 | |
| Trust in government | 0–33 | Reference | ||
| 34–67 | 0.53 | 0.29–0.96 | 0.035 | |
| 68–100 | 0.44 | 0.23–0.84 | 0.013 | |
| Follow government advice | Personal choice | Reference | ||
| Civic duty | 0.66 | 0.45–0.98 | 0.040 | |
| Attitude toward a new vaccine | First to get | Reference | ||
| Wait and see | 1.28 | 0.59–2.78 | 0.536 | |
| Refuse | 1.86 | 0.46–7.53 | 0.385 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Y.; Li, M.; Yang, L.; Bressington, D.; Leung, S.-F.; Xie, Y.-J.; Qin, J.; Molasiotis, A.; Leung, A.Y.M. Are People Willing to Take Regular COVID-19 Vaccines? Prevalence and Determinants of Hesitancy for Regular COVID-19 Vaccination: A Random Population-Based Survey in Hong Kong. Vaccines 2023, 11, 1388. https://doi.org/10.3390/vaccines11081388
Li Y, Li M, Yang L, Bressington D, Leung S-F, Xie Y-J, Qin J, Molasiotis A, Leung AYM. Are People Willing to Take Regular COVID-19 Vaccines? Prevalence and Determinants of Hesitancy for Regular COVID-19 Vaccination: A Random Population-Based Survey in Hong Kong. Vaccines. 2023; 11(8):1388. https://doi.org/10.3390/vaccines11081388
Chicago/Turabian StyleLi, Yan, Mengqi Li, Lin Yang, Daniel Bressington, Sau-Fong Leung, Yao-Jie Xie, Jing Qin, Alex Molasiotis, and Angela Y. M. Leung. 2023. "Are People Willing to Take Regular COVID-19 Vaccines? Prevalence and Determinants of Hesitancy for Regular COVID-19 Vaccination: A Random Population-Based Survey in Hong Kong" Vaccines 11, no. 8: 1388. https://doi.org/10.3390/vaccines11081388
APA StyleLi, Y., Li, M., Yang, L., Bressington, D., Leung, S.-F., Xie, Y.-J., Qin, J., Molasiotis, A., & Leung, A. Y. M. (2023). Are People Willing to Take Regular COVID-19 Vaccines? Prevalence and Determinants of Hesitancy for Regular COVID-19 Vaccination: A Random Population-Based Survey in Hong Kong. Vaccines, 11(8), 1388. https://doi.org/10.3390/vaccines11081388











