A Comparative Study of Immunogenicity, Antibody Persistence, and Safety of Three Different COVID-19 Boosters between Individuals with Comorbidities and the Normal Population
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
- (1)
- BBIP-CorV primed/PastoCovac Plus boosted (BP);
- (2)
- BBIP-CorV primed/PastoCovac boosted (BPa);
- (3)
- BBIP-CorV primed/BBIP-CorV boosted (BB).
2.2. Antibodies Response
2.3. Safety Assessment
2.4. Statistical Analysis
3. Results
3.1. Study Population
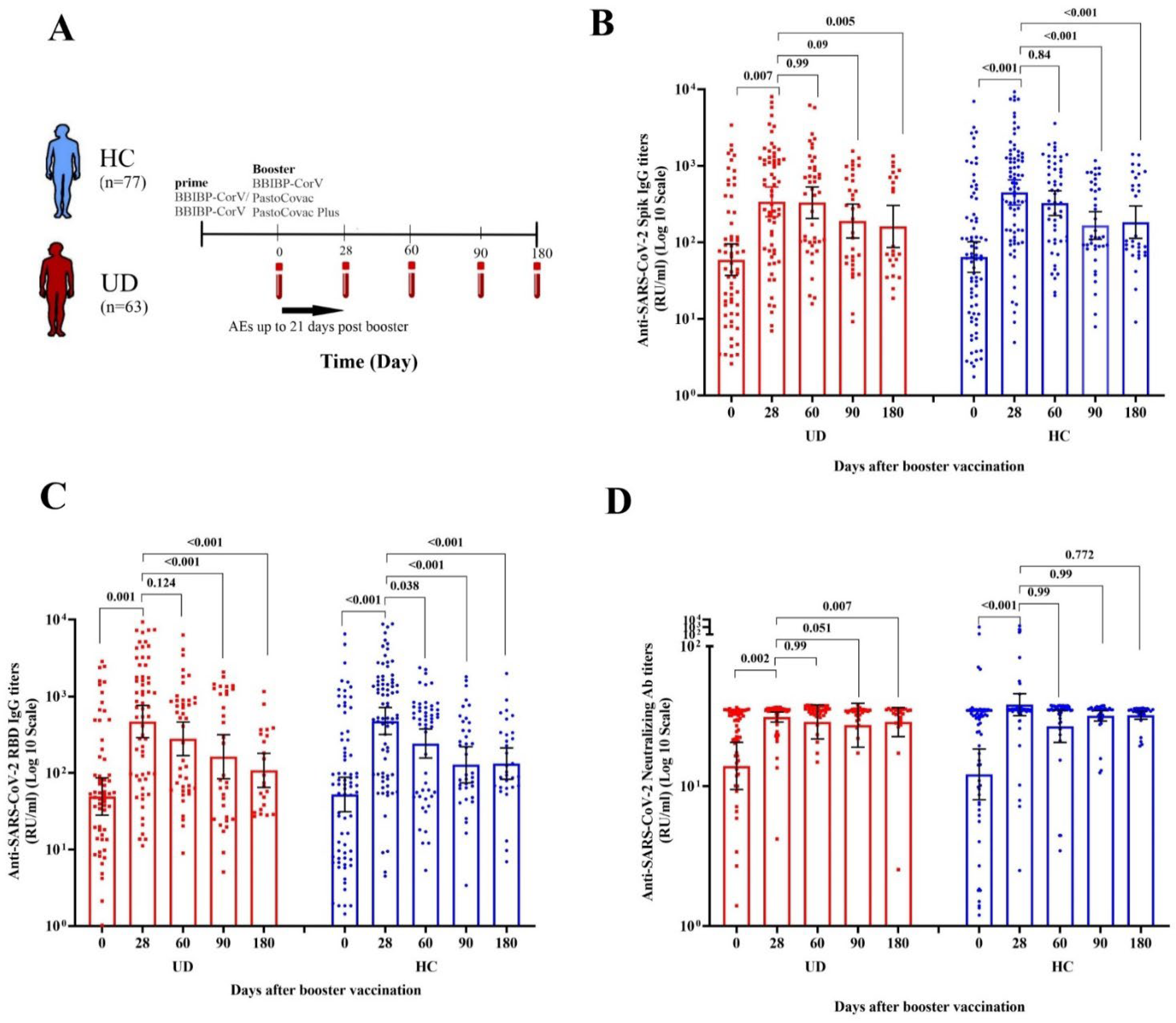
3.2. Comparison of COVID 19 Booster Simmunogenicity and Antibody Persistency between UD and HC Groups
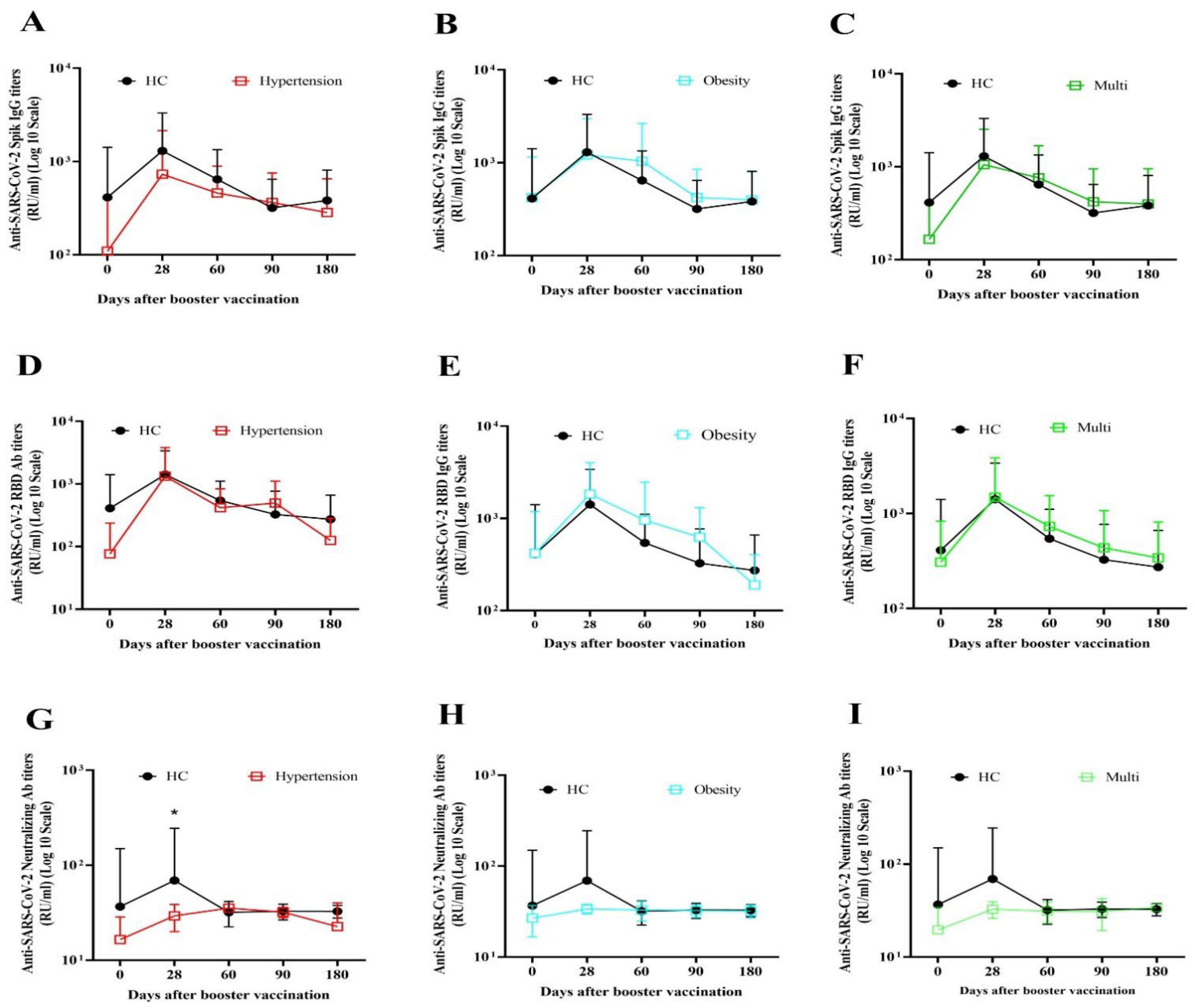
3.2.1. Immunogenicity and Antibody Persistency of Boosters among People with Underlying Diseases
3.2.2. Immunogenicity and Antibody Persistency of Boosters among Healthy People
3.3. Comparative Safety Outcomes of COVID-19 Boosters between UD and HC Groups
4. Discussion
- The humoral immune responses in people with obesity, hypertension, and diabetes mellitus were induced after three kinds of COVID-19 booster vaccines.
- There was no significant difference between the healthy individuals and those with underlying diseases regarding humoral immune responses.
- The protein subunit vaccine had a better impact on immune response induction in people with comorbidities.
- The induced antibodies were detectable 180 days after the booster shots in both healthy and comorbidity groups.
- Less adverse events were recorded after PastoCovac/Plus booster shots compared to BBIBP-CorV.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. WHO Coronavirus (COVID-19) Dashboard. 2023. Available online: https://covid19.who.int/ (accessed on 20 January 2023).
- WHO. WHO Health Emergency Dashboard. Available online: https://covid19.who.int/region/emro/country/ir (accessed on 20 January 2023).
- WHO. Statement on the Fifteenth Meeting of the IHR (2005) Emergency Committee on the COVID-19 Pandemic. 2023. Available online: https://www.who.int/news/item/05-05-2023-statement-on-the-fifteenth-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-coronavirus-disease-(covid-19)-pandemic (accessed on 11 May 2023).
- CDC. End of the Federal COVID-19 Public Health Emergency (PHE) Declaration. 2023. Available online: https://www.cdc.gov/coronavirus/2019-ncov/your-health/end-of-phe.html (accessed on 5 May 2023).
- Yin, T.; Li, Y.; Ying, Y.; Luo, Z. Prevalence of comorbidity in Chinese patients with COVID-19: Systematic review and meta-analysis of risk factors. BMC Infect. Dis. 2021, 21, 200. [Google Scholar] [CrossRef] [PubMed]
- Emami, A.; Javanmardi, F.; Pirbonyeh, N.; Akbari, A. Prevalence of underlying diseases in hospitalized patients with COVID-19: A systematic review and meta-analysis. Arch. Acad. Emerg. Med. 2020, 8, e35. [Google Scholar] [PubMed]
- Huynh, G.; Nguyen, T.V.; Nguyen, D.D.; Lam, Q.M.; Pham, T.N.; Nguyen, H.T.N. Knowledge about COVID-19, beliefs and vaccination acceptance against COVID-19 among high-risk people in Ho Chi Minh City, Vietnam. Infect. Drug Resist. 2021, 14, 1773–1780. [Google Scholar] [CrossRef]
- Wang, H.; Zhang, Y.; Huang, B.; Deng, W.; Quan, Y.; Wang, W.; Xu, W.; Zhao, Y.; Li, N.; Zhang, J. Development of an inactivated vaccine candidate, BBIBP-CorV, with potent protection against SARS-CoV-2. Cell 2020, 182, 713–721.e719. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, M.; Balena, A.; Tuccinardi, D.; Tozzi, R.; Risi, R.; Masi, D.; Caputi, A.; Rossetti, R.; Spoltore, M.E.; Filippi, V. Central obesity, smoking habit, and hypertension are associated with lower antibody titres in response to COVID-19 mRNA vaccine. Diabetes/Metab. Res. Rev. 2022, 38, e3465. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Q.; Zhang, Y.; Kang, J.; Chen, Z.; Peng, M.; Chen, M.; Zhang, G.; Xiang, D.; Xiao, S.; Li, H. Weakened humoral and cellular immune response to the inactivated COVID-19 vaccines in Chinese individuals with obesity/overweight. Genes Dis. 2022, 10, 608–617. [Google Scholar] [CrossRef] [PubMed]
- Malavazos, A.E.; Basilico, S.; Iacobellis, G.; Milani, V.; Cardani, R.; Boniardi, F.; Dubini, C.; Prandoni, I.; Capitanio, G.; Renna, L.V. Antibody responses to BNT162b2 mRNA vaccine: Infection-naïve individuals with abdominal obesity warrant attention. Obesity 2022, 30, 606–613. [Google Scholar] [CrossRef]
- Dicker, D.; Golan, R.; Baker, J.L.; Busetto, L.; Frühbeck, G.; Goossens, G.H.; Halford, J.C.; Holm, J.-C.; Woodward, E.; Farpour-Lambert, N.J. Vaccinating people with obesity for COVID-19: EASO call for action. Obes. Facts 2021, 14, 334. [Google Scholar] [CrossRef]
- Sauré, D.; O’Ryan, M.; Torres, J.P.; Zuniga, M.; Santelices, E.; Basso, L.J. Dynamic IgG seropositivity after rollout of CoronaVac and BNT162b2 COVID-19 vaccines in Chile: A sentinel surveillance study. Lancet Infect. Dis. 2022, 22, 56–63. [Google Scholar] [CrossRef]
- Singh, A.K.; Phatak, S.R.; Singh, R.; Bhattacharjee, K.; Singh, N.K.; Gupta, A.; Sharma, A. Antibody response after first and second-dose of ChAdOx1-nCOV (CovishieldTM®) and BBV-152 (CovaxinTM®) among health care workers in India: The final results of cross-sectional coronavirus vaccine-induced antibody titre (COVAT) study. Vaccine 2021, 39, 6492–6509. [Google Scholar] [CrossRef]
- Karamese, M.; Tutuncu, E.E. The effectiveness of inactivated SARS-CoV-2 vaccine (CoronaVac) on antibody response in participants aged 65 years and older. J. Med. Virol. 2022, 94, 173–177. [Google Scholar] [CrossRef] [PubMed]
- Ali, H.; Alterki, A.; Sindhu, S.; Alahmad, B.; Hammad, M.; Al-Sabah, S.; Alghounaim, M.; Jamal, M.H.; Aldei, A.; Mairza, M.J. Robust antibody levels in both diabetic and non-diabetic individuals after BNT162b2 mRNA COVID-19 vaccination. Front. Immunol. 2021, 12, 752233. [Google Scholar] [CrossRef] [PubMed]
- Soegiarto, G.; Wulandari, L.; Purnomosari, D.; Fahmita, K.D.; Gautama, H.I.; Hadmoko, S.T.; Prasetyo, M.E.; Mahdi, B.A.; Arafah, N.; Prasetyaningtyas, D. Hypertension is associated with antibody response and breakthrough infection in health care workers following vaccination with inactivated SARS-CoV-2. Vaccine 2022, 40, 4046–4056. [Google Scholar] [CrossRef]
- Pellini, R.; Venuti, A.; Pimpinelli, F.; Abril, E.; Blandino, G.; Campo, F.; Conti, L.; De Virgilio, A.; De Marco, F.; Di Domenico, E.G. Initial observations on age, gender, BMI and hypertension in antibody responses to SARS-CoV-2 BNT162b2 vaccine. EClinicalMedicine 2021, 36, 100928. [Google Scholar] [CrossRef]
- Ai, J.; Zhang, H.; Zhang, Q.; Zhang, Y.; Lin, K.; Fu, Z.; Song, J.; Zhao, Y.; Fan, M.; Wang, H. Recombinant protein subunit vaccine booster following two-dose inactivated vaccines dramatically enhanced anti-RBD responses and neutralizing titers against SARS-CoV-2 and Variants of Concern. Cell Res. 2022, 32, 103–106. [Google Scholar] [CrossRef]
- Cao, Y.; Hao, X.; Wang, X.; Wu, Q.; Song, R.; Zhao, D.; Song, W.; Wang, Y.; Yisimayi, A.; Wang, W. Humoral immunogenicity and reactogenicity of CoronaVac or ZF2001 booster after two doses of inactivated vaccine. Cell Res. 2022, 32, 107–109. [Google Scholar] [CrossRef]
- Toback, S.; Marchese, A.M.; Warren, B.; Ayman, S.; Zarkovic, S.; ElTantawy, I.; Mallory, R.M.; Rousculp, M.; Almarzooqi, F.; Piechowski-Jozwiak, B. Safety and Immunogenicity of the NVX-CoV2373 Vaccine as a Booster in Adults Previously Vaccinated with the BBIBP-CorV Vaccine: An Interim Analysis. medRxiv 2023. [Google Scholar] [CrossRef]
- Toledo-Romaní, M.E.; García-Carmenate, M.; Valenzuela-Silva, C.; Baldoquín-Rodríguez, W.; Martínez-Pérez, M.; Rodríguez-González, M.; Paredes-Moreno, B.; Mendoza-Hernández, I.; Romero, R.G.-M.; Samón-Tabio, O. Safety and efficacy of the two doses conjugated protein-based SOBERANA-02 COVID-19 vaccine and of a heterologous three-dose combination with SOBERANA-Plus: A double-blind, randomised, placebo-controlled phase 3 clinical trial. Lancet Reg. Health–Am. 2023, 18, 100423. [Google Scholar] [CrossRef]
- Toledo-Romani, M.E.; García-Carmenate, M.; Verdecia-Sánchez, L.; Pérez-Rodríguez, S.; Rodriguez-González, M.; Valenzuela-Silva, C.; Paredes-Moreno, B.; Sanchez-Ramirez, B.; González-Mugica, R.; Hernández-Garcia, T. Safety and immunogenicity of anti-SARS CoV-2 conjugate vaccine SOBERANA 02 in a two-dose or three-dose heterologous scheme in adults: Phase IIb Clinical Trial. medRxiv 2022. [Google Scholar] [CrossRef]
- Sadat Larijani, M.; Sorouri, R.; Eybpoosh, S.; Doroud, D.; Moradi, L.; Ahmadinezhad, M.; Bavand, A.; Ashrafian, F.; Tajmehrabi Namini, P.; Zali, M. Assessment of long-term adverse events regarding different COVID-19 vaccine regimens within an 18-month follow-up study. Pathog. Dis. 2023, 81, ftad010. [Google Scholar] [CrossRef]
- Puga-Gómez, R.; Ricardo-Delgado, Y.; Rojas-Iriarte, C.; Céspedes-Henriquez, L.; Piedra-Bello, M.; Vega-Mendoza, D.; Pestana Pérez, N.; Paredes-Moreno, B.; Rodríguez-González, M.; Valenzuela-Silva, C. Open label phase I/II clinical trial and predicted efficacy of SARS-CoV-2 RBD protein vaccines SOBERANA 02 and SOBERANA Plus in children. medRxiv 2022. [Google Scholar] [CrossRef]
- Mafinezhad, S.; Bayani, G.; Ehteshammanesh, H.; Langari, M.; Shokrollahi, N.; Bozorgnia, Y.; Namdar Ahmadabad, H. Evaluation of the side effects of Sinopharm and PastoCovac COVID-19 vaccines in children aged 5-12 years in Iran. Int. J. Pediatr. 2023, 11, 17572–17582. [Google Scholar]
- CDC. Diabetes Tests. 2023. Available online: https://www.cdc.gov/diabetes/basics/getting-tested.html#:~:text=A%20fasting%20blood%20sugar%20level,higher%20indicates%20you%20have%20diabetes (accessed on 28 February 2023).
- CDC. High Blood Pressure Symptoms and Causes. 2021. Available online: https://www.cdc.gov/bloodpressure/about.htm (accessed on 18 May 2021).
- Muangnoicharoen, S.; Wiangcharoen, R.; Nanthapisal, S.; Kamolratakul, S.; Lawpoolsri Niyom, S.; Jongkaewwattana, A.; Thitithanyanont, A.; Luvira, V.; Chinwangso, P.; Thanthamnu, N. Single Ad26. COV2. S Booster Dose Following Two Doses of BBIBP-CorV Vaccine Against SARS-CoV-2 Infection in Adults: Day 28 Results of a Phase 1/2 Open-Label Trial. Vaccine 2023, 41, 4648–4657. [Google Scholar] [CrossRef] [PubMed]
- Amellal, H.; Assaid, N.; Akarid, K.; Maaroufi, A.; Ezzikouri, S.; Sarih, M.H. Mix-and-match COVID-19 vaccines trigger high antibody response after the third dose vaccine in Moroccan health care workers. Vaccine X 2023, 14, 100288. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Chen, H.; Lv, J.; Huang, T.; Zhang, R.; Zhang, D.; Luo, L.; Wei, S.; Liu, X.; Zhang, S. Evaluation of Immunogenicity and Safety of Vero Cell-Derived Inactivated COVID-19 Vaccine in Older Patients with Hypertension and Diabetes Mellitus. Vaccines 2022, 10, 1020. [Google Scholar] [CrossRef]
- Li, C.; Bi, H.; Fu, Z.; Li, A.; Wan, N.; Hu, J.; Yang, F.; Zhou, T.-C.; Liang, Y.; Su, W. Retrospective study of the immunogenicity and safety of the CoronaVac SARS-CoV-2 vaccine in people with underlying medical conditions. Commun. Med. 2022, 2, 151. [Google Scholar] [CrossRef]
- Huang, R.; Liu, X.; Xie, F.; Li, J.; Tang, Z.; Wu, Y.; Zhou, P.; Zhang, D. Safety and immunogenicity of inactivated SARS-CoV-2 vaccine (BBIBP-CorV) in hypertensive and/or diabetic people aged over 60 years: A prospective open-label study. Diabetes Ther. 2023, 14, 139–151. [Google Scholar] [CrossRef]
- Pellini, R.; Venuti, A.; Pimpinelli, F.; Abril, E.; Blandino, G.; Campo, F.; Conti, L.; De Virgilio, A.; De Marco, F.; Di Domenico, E.G. Obesity may hamper SARS-CoV-2 vaccine immunogenicity. medRXiv 2021. [Google Scholar] [CrossRef]
- Rifai, A.; Wahono, C.S.; Pratama, M.Z.; Handono, K.; Susianti, H.; Iskandar, A.; Diyah, N.; Santoningsih, D.; Samsu, N.; Gunawan, A. Association between the effectiveness and immunogenicity of inactivated SARS-CoV-2 vaccine (CoronaVac) with the presence of hypertension among health care workers. Clin. Exp. Hypertens. 2022, 44, 233–239. [Google Scholar] [CrossRef]
- Toledo-Romani, M.E.; Garcia-Carmenate, M.; Silva, C.V.; Baldoquin-Rodriguez, W.; Pérez, M.M.; Gonzalez, M.R.; Moreno, B.P.; Hernández, I.M.; Romero, R.G.-M.; Tabio, O.S. Efficacy and safety of SOBERANA 02, a COVID-19 conjugate vaccine in heterologous three-dose combination. medRxiv 2021. [Google Scholar] [CrossRef]
- Pellini, R.; Venuti, A.; Pimpinelli, F.; Abril, E.; Blandino, G.; Campo, F.; Conti, L.; De Virgilio, A.; De Marco, F.; Di Domenico, E.G. Early onset of SARS-CoV-2 antibodies after first dose of BNT162b2: Correlation with age, gender and BMI. Vaccines 2021, 9, 685. [Google Scholar] [CrossRef]
- Míguez, H.M.; García, I.M.; Gómez, M.O.; Merino, I.M.G.; Cano, E.L.; De La Torre, A. Immunogenicity, effectiveness and safety of COVID-19 vaccine in older adults living in nursing homes: A real-life study. Rev. Española De Geriatría Y Gerontol. 2023, 58, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Bruel, T.; Pinaud, L.; Tondeur, L.; Planas, D.; Staropoli, I.; Porrot, F.; Guivel-Benhassine, F.; Attia, M.; Pelleau, S.; Woudenberg, T. Neutralising antibody responses to SARS-CoV-2 omicron among elderly nursing home residents following a booster dose of BNT162b2 vaccine: A community-based, prospective, longitudinal cohort study. EClinicalMedicine 2022, 51, 101576. [Google Scholar] [CrossRef]
- Shapiro, J.R.; Sitaras, I.; Park, H.S.; Aytenfisu, T.Y.; Caputo, C.; Li, M.; Lee, J.; Johnston, T.S.; Li, H.; Wouters, C. Association of Frailty, Age, and Biological Sex With Severe Acute Respiratory Syndrome Coronavirus 2 Messenger RNA Vaccine–Induced Immunity in Older Adults. Clin. Infect. Dis. 2022, 75, S61–S71. [Google Scholar] [CrossRef] [PubMed]
- Gaborit, B.; Fernandes, S.; Loubet, P.; Ninove, L.; Dutour, A.; Cariou, B.; Coupaye, M.; Clement, K.; Czernichow, S.; Carette, C. Early humoral response to COVID-19 vaccination in patients living with obesity and diabetes in France. The COVPOP OBEDIAB study with results from the ANRS0001S COV-POPART cohort. Metabolism 2023, 142, 155412. [Google Scholar] [CrossRef] [PubMed]
- Fathi, M.; Vakili, K.; Sayehmiri, F.; Mohamadkhani, A.; Hajiesmaeili, M.; Rezaei-Tavirani, M.; Eilami, O. The prognostic value of comorbidity for the severity of COVID-19: A systematic review and meta-analysis study. PLoS ONE 2021, 16, e0246190. [Google Scholar] [CrossRef]
- Channappanavar, R.; Fett, C.; Mack, M.; Ten Eyck, P.P.; Meyerholz, D.K.; Perlman, S. Sex-based differences in susceptibility to severe acute respiratory syndrome coronavirus infection. J. Immunol. 2017, 198, 4046–4053. [Google Scholar] [CrossRef]
- Badawi, A.; Ryoo, S.G. Prevalence of comorbidities in the Middle East respiratory syndrome coronavirus (MERS-CoV): A systematic review and meta-analysis. Int. J. Infect. Dis. 2016, 49, 129–133. [Google Scholar] [CrossRef]
- Naaber, P.; Tserel, L.; Kangro, K.; Sepp, E.; Jürjenson, V.; Adamson, A.; Haljasmägi, L.; Rumm, P.; Maruste, R.; Kärner, J. Declined antibody responses to COVID-19 mRNA vaccine within first three months. medRxiv 2021. [Google Scholar] [CrossRef]
- Bignucolo, A.; Scarabel, L.; Mezzalira, S.; Polesel, J.; Cecchin, E.; Toffoli, G. Sex disparities in efficacy in COVID-19 vaccines: A systematic review and meta-analysis. Vaccines 2021, 9, 825. [Google Scholar] [CrossRef]
- Erdem, M.G.; Unlu, O.; Buber, S.; Demirci, M.; Kocazeybek, B.S. Could Prior COVID-19 Affect the Neutralizing Antibody after the Third BNT162b2 Booster Dose: A Longitudinal Study. Vaccines 2023, 11, 560. [Google Scholar] [CrossRef] [PubMed]
- Salimian, J.; Ahmadi, A.; Amani, J.; Olad, G.; Halabian, R.; Saffaei, A.; Arabfard, M.; Nasiri, M.; Nazarian, S.; Abolghasemi, H. Safety and immunogenicity of a recombinant receptor-binding domain-based protein subunit vaccine (Noora vaccine™) against COVID-19 in adults: A randomized, double-blind, placebo-controlled, Phase 1 trial. J. Med. Virol. 2023, 95, 2. [Google Scholar] [CrossRef] [PubMed]
- Heidary, M.; Kaviar, V.H.; Shirani, M.; Ghanavati, R.; Motahar, M.; Sholeh, M.; Ghahramanpour, H.; Khoshnood, S. A comprehensive review of the protein subunit vaccines against COVID-19. Front. Microbiol. 2022, 13, 927306. [Google Scholar] [CrossRef] [PubMed]
- Kaabi, N.A.; Yang, Y.K.; Zhang, J.; Xu, K.; Liang, Y.; Kang, Y.; Su, J.G.; Yang, T.; Hussein, S.; ElDein, M.S. Immunogenicity and safety of NVSI-06-07 as a heterologous booster after priming with BBIBP-CorV: A phase 2 trial. Signal Transduct. Target. Ther. 2022, 7, 172. [Google Scholar] [CrossRef]
- Ramezani, A.; Sorouri, R.; Haji Maghsoudi, S.; Dahmardeh, S.; Doroud, D.; Sadat Larijani, M.; Eybpoosh, S.; Mostafavi, E.; Olyaeemanesh, A.; Salehi-Vaziri, M. PastoCovac and PastoCovac Plus as protein subunit COVID-19 vaccines led to great humoral immune responses in BBIP-CorV immunized individuals. Sci. Rep. 2023, 13, 8065. [Google Scholar] [CrossRef]
- Han, S.; Yang, Y.; Wang, T.; Song, R.; Hu, D.; Peng, M.; Lin, Z.; Deng, Q.; Ren, H.; Ming, J. Safety and immunogenicity of the third (booster) dose of inactivated and recombinant protein SARS-CoV-2 vaccine for patients with endocrine-related cancer. Front. Public Health 2023, 11, 1086872. [Google Scholar] [CrossRef]
- Li, C.; Li, A.; Bi, H.; Hu, J.; Yang, F.; Zhou, T.; Liang, Y.; Su, W.; Shi, T.; Yang, M. Immunogenicity and safety of the CoronaVac inactivated SARS-CoV-2 vaccine in people with underlying medical conditions: A retrospective study. medRxiv 2022. [Google Scholar] [CrossRef]

| Total N (%) | HC N (%) | UD N (%) | |
|---|---|---|---|
| Gender | |||
| Female | 74 (52.9%) | 41 (53.2%) | 33 (52.4%) |
| Male | 66 (47.1%) | 36(46.8%) | 30 (47.6%) |
| Age | |||
| ≤40 | 57 (40.7%) | 38 (49.4%) | 19 (30.2%) |
| >40 | 83 (59.3%) | 39 (50.6%) | 44 (69.8%) |
| COVID-19 History | |||
| No | 113 (80.7) | 59 (76.9) | 54 (85.7) |
| Yes | 27 (19.3) | 18 (23.4) | 9 (14.3) |
| Booster | |||
| BP | 54 (38.6%) | 28 (36.4%) | 26 (41.3%) |
| BPa | 44 (31.4%) | 27 (35.1%) | 17 (27.0) |
| BB | 42 (30.0) | 22 (28.6%) | 20 (31.7%) |
| HC | UD | p Value | |
|---|---|---|---|
| Anti-SARS-CoV-2 Spike Antibody (Geometric Mean, 95% CI) | |||
| Antibody titers | |||
| Day 0 | 64.26 (40.53−101.88) | 59.22 (36.87−95.12) | 0.86 |
| Day 28 | 449.52 (301.75−656.59) | 339.09 (216.83−530.28) | 0.38 |
| Day 60 | 325.87 (224.88−472.21) | 330.00 (205.34−530.34) | 0.97 |
| Day 90 | 166.11 (109.63−251.69) | 189.99 (113.92−316.86) | 0.79 |
| Day 180 | 183.41 (112.74−298.35) | 161.22 (85.65−303.49) | 0.39 |
| Mean Fold rise | |||
| Day 28 | 7.00 (5.01−9.76) | 5.72 (3.92−8.37) | 0.31 |
| Day 60 | 3.88 (2.33−6.46) | 4.27 (2.35−7.77) | 0.75 |
| Day 90 | 1.67 (0.95−2.94) | 2.88 (1.29−6.45) | 0.25 |
| Day 180 | 1.54 (0.69−3.41) | 1.61 (0.56−4.65) | 0.98 |
| Neutralizing Antibody (Geometric Mean, 95% CI) | |||
| Antibody titers | |||
| Day 0 | 12.16 (8.01−18.47) | 13.97 (9.47−20.62) | 0.78 |
| Day 28 | 38.31 (31.95−45.95) | 31.27 (28.79−33.96) | 0.054 |
| Day 60 | 26.84 (20.61−34.96) | 28.85 (21.82−38.15) | 0.90 |
| Day 90 | 31.91 (29.31−34.74) | 27.32 (19.04−39.22) | 0.10 |
| Day 180 | 32.22 (30.14−34.45) | 28.79 (22.66−36.57) | 0.34 |
| Mean Fold rise | |||
| Day 28 | 9.14 (5.98−13.96) | 9.52 (5.24−19.30) | 0.55 |
| Day 60 | 3.51 (2.01−6.12) | 4.10 (2.04−8.23) | 0.95 |
| Day 90 | 1.78 (1.22−2.60) | 1.55 (0.87−2.78) | 0.32 |
| Day 180 | 1.52 (1.17−1.97) | 1.66 (0.80−3.45) | 0.83 |
| Anti-SARS-CoV-2 RBD Antibody (Geometric Mean, 95% CI) | |||
| Antibody titers | |||
| Day 0 | 52.38 (31.24−87.83) | 49.12 (28.07−85.95) | 0.88 |
| Day 28 | 478.74 (319.48−717.38) | 470.89 (290.65−762.90) | 0.98 |
| Day 60 | 242.97 (156.99−376.03) | 279.99 (169.23−463.24) | 0.34 |
| Day 90 | 128.02 (74.30−220.57) | 163.21 (84.18−316.43) | 0.77 |
| Day 180 | 132.60 (82.72−212.55) | 107.96 (64.67−180.24) | 0.34 |
| Mean Fold rise | |||
| Day 28 | 3.15 (2.13−4.66) | 2.23 (1.52−3.27) | 0.27 |
| Day 60 | 1.61 (1.03−2.49) | 1.78 (1.19−2.66) | 0.54 |
| Day 90 | 1.31 (0.66−2.61) | 3.70 (1.27−10.78) | 0.39 |
| Day 180 | 1.05 (0.44−2.54) | 1.29 (0.37−4.45) | 0.11 |
| Day 28 | Day 60 | Day 90 | Day 180 | |||||
|---|---|---|---|---|---|---|---|---|
| Median (IQR) | P | Median (IQR) | P | Median (IQR) | P | Median (IQR) | P | |
| Anti-SARS-CoV-2 Spike Antibody Median Fold Rise (IQR) | ||||||||
| Age | ||||||||
| ≤40 | 1.61 (6.07) | 0.02 | 2.73 (9.32) | 0.55 | 1.37 (4.77) | 0.22 | 0.92 (3.30) | 0.36 |
| >40 | 7.69 (14.26) | 4.12 (25.18) | 3.90 (14.19) | 2.77 (17.39) | ||||
| Gender | ||||||||
| Female | 3.45 (11.14) | 0.3 | 1.90 (5.53) | 0.08 | 1.33 (11.02) | 0.13 | 0.86 (9.89) | 0.33 |
| Male | 5.80 (18.23) | 6.84 (30.94) | 5.02 (11.19) | 3.49 (14.48) | ||||
| COVID-19 History | ||||||||
| No | 4.58 (12.96) | 0.62 | 4.04 (17.82) | 0.19 | 3.86 (11.04) | 0.63 | 1.86 (14.40) | 0.66 |
| Yes | 4.30 (11.63) | 1.14 (25.51) | 2.37 (12.60) | 0.75 (18.53) | ||||
| Types of UD | ||||||||
| Hypertension | 9.39 (34.58) | 0.21 | 4.12 (19.25) | 0.91 | 5.26 (86) | 0.54 | 19.53 () | 0.25 |
| Obesity | 3.92 (10.58) | 2.45 (25.18) | 3.86 (12.44) | 0.92 (14.43) | ||||
| Multi | 4.48 (14.03) | 3.56 (6.34) | 1.55 (4.73) | 0.98 (2.28) | ||||
| Booster | ||||||||
| BP | 11.01 (36.75) | <0.001 | 6.07 (31.60) | 0.33 | 5.62 (110.79) | 0.53 | 1.43 (64.41) | 0.83 |
| BPa | 11.34 (20.25) | 6.05 (28.82) | 4.42 (11.83) | 3.50 (14.96) | ||||
| BB | 1.55 (1.19) | 2.18 (2.53) | 1.45 (2.86) | 1.14 (1.95) | ||||
| Anti-SARS-CoV-2 Neutralizing Antibody Median Fold Rise (IQR) | ||||||||
| Age | ||||||||
| ≤40 | 1.05 (0.52) | 0.19 | 1.05 (0.43) | 0.28 | 1 (0.46) | 0.69 | 0.96 (0.16) | 0.36 |
| >40 | 1.18 (1.81) | 1.11 (0.85) | 1.12 (0.69) | 1.03 (0.67) | ||||
| Gender | ||||||||
| Female | 1.09 (1.16) | 0.4 | 1.05 (0.13) | 0.03 | 1 (0.19) | 0.17 | 0.99 (0.20) | 0.92 |
| Male | 1.14 (1.54) | 1.23 (1.39) | 1.46 (0.68) | 1.01 (11.86) | ||||
| COVID-19 History | ||||||||
| No | 1.12 (1.38) | 0.11 | 1.10 (0.96) | 0.61 | 1.10 (0.71) | 0.3 | 0.98 (0.58) | 0.84 |
| Yes | 1.02 (0.15) | 1.08 (0.16) | 0.99 (0.15) | 1.10 (0.23) | ||||
| Types of UD | ||||||||
| Hypertension | 1.60 (2.03) | 0.04 | 1.18 (1.03) | 0.57 | 1.57 (170.96) | 0.73 | 0.96 () | 0.94 |
| Obesity | 1.09 (0.39) | 1.08 (0.19) | 1.10 (0.54) | 1.01 (0.37) | ||||
| Multi | 1.50 (8.13) | 1.13 (4.80) | 0.99 (2.77) | 1.01 (11.47) | ||||
| Booster | ||||||||
| BP | 1.61 (3.04) | 0.01 | 1.05 (1.18) | 0.1 | 1.50 (2.19) | 0.29 | 1.03 (60.69) | 0.42 |
| BPa | 1.11 (0.61) | 1.20 (0.90) | 1.11 (0.63) | 1.01 (0.59) | ||||
| BB | 1.03 (0.14) | 1.03 (0.18) | 1 (0.10) | 0.96 (0.10) | ||||
| Anti-SARS-CoV-2 RBD Antibody Median Fold Rise (IQR) | ||||||||
| Age | ||||||||
| ≤40 | 2.28(32.18) | 0.73 | 1.36(11.32) | 0.35 | 0.35(9.53) | 0.05 | 0.35(0.17) | 0.12 |
| >40 | 5.10(29.58) | 4.22(18.20) | 8.73(20.61) | 1.18(11.28) | ||||
| Gender | ||||||||
| Female | 2.29 (30.07) | 0.07 | 1.28 (4.23) | 0.02 | 0.82 (19.25) | 0.24 | 0.039 (2.54) | 0.47 |
| Male | 10.75 (36.62) | 9.70 (46.30) | 9.39 (21.23) | 0.72 (20.92) | ||||
| COVID-19 History | ||||||||
| No | 4.69 (34.15) | 0.78 | 3.19 (17.45) | 0.35 | 1.43 (22.66) | 0.53 | 0.52 (4.61) | 0.96 |
| Yes | 6.38 (27.27) | 0.98 (15.66) | 1.10 (19.35) | 0.66 (5.26) | ||||
| Types of UD | ||||||||
| Hypertension | 6.38 (38.46) | 0.66 | 2.17 (21.07) | 0.92 | 11.56 (192.97) | 0.32 | 37.53 () | 0.18 |
| Obesity | 5.10 (29.81) | 1.80 (17.13) | 1.62 (19.23) | 0.40 (2.99) | ||||
| Multi | 4.63 (17.70) | 1.95 (9.35) | 0.65 (13.25) | 0.38 (2.58) | ||||
| Booster | ||||||||
| BP | 15.26 (121.92) | <0.001 | 4.74 (20.33) | 0.03 | 11.57 (151.55) | 0.03 | 0.54 (34.19) | 0.72 |
| BPa | 13.85 (23.06) | 9.83 (45.09) | 8.73 (19.05) | 0.95 (5.66) | ||||
| BB | 1.26 (0.57) | 1.05 (0.94) | 0.34 (0.67) | 0.39 (0.55) | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ashrafian, F.; Bagheri Amiri, F.; Bavand, A.; Zali, M.; Sadat Larijani, M.; Ramezani, A. A Comparative Study of Immunogenicity, Antibody Persistence, and Safety of Three Different COVID-19 Boosters between Individuals with Comorbidities and the Normal Population. Vaccines 2023, 11, 1376. https://doi.org/10.3390/vaccines11081376
Ashrafian F, Bagheri Amiri F, Bavand A, Zali M, Sadat Larijani M, Ramezani A. A Comparative Study of Immunogenicity, Antibody Persistence, and Safety of Three Different COVID-19 Boosters between Individuals with Comorbidities and the Normal Population. Vaccines. 2023; 11(8):1376. https://doi.org/10.3390/vaccines11081376
Chicago/Turabian StyleAshrafian, Fatemeh, Fahimeh Bagheri Amiri, Anahita Bavand, Mahsan Zali, Mona Sadat Larijani, and Amitis Ramezani. 2023. "A Comparative Study of Immunogenicity, Antibody Persistence, and Safety of Three Different COVID-19 Boosters between Individuals with Comorbidities and the Normal Population" Vaccines 11, no. 8: 1376. https://doi.org/10.3390/vaccines11081376
APA StyleAshrafian, F., Bagheri Amiri, F., Bavand, A., Zali, M., Sadat Larijani, M., & Ramezani, A. (2023). A Comparative Study of Immunogenicity, Antibody Persistence, and Safety of Three Different COVID-19 Boosters between Individuals with Comorbidities and the Normal Population. Vaccines, 11(8), 1376. https://doi.org/10.3390/vaccines11081376






